Currently, 33 million people are estimated to be at risk of malnutrition in Europe( Reference Ljungqvist and de Man 1 ). Of the patients hospitalised throughout Europe, 25 % suffer from disease-related malnutrition( Reference Roller, Eglseer and Eisenberger 2 ). In contrast, obesity has been reported to affect 10–30 % of the adult population( 3 ). Obesity leads to diseases such as hypertension, diabetes and cardiovascular illnesses( 4 ). Interdisciplinary cooperation is vital to cover the wide range of these nutritional diseases and guarantee that patients are provided with holistic care( Reference White, Guenter and Jensen 5 ). To ensure high-quality nutritional care in many care settings, however, it is essential to improve the accessibility of information related to the individual’s nutritional status, nutritional assessment and nutrition therapy, allowing it to be read by all professionals involved in the care pathway( Reference Tappenden, Quatrara and Parkhurst 6 ). The transfer of information from the hospital to the community setting is especially important in that it ensures the efficacy and effectiveness of nutritional interventions( Reference Tappenden, Quatrara and Parkhurst 6 ).
This dimension of patient care is also included in the guidelines on definitions and terminology of clinical nutrition published by the European Society for Clinical Nutrition and Metabolism (ESPEN) in 2016( Reference Cederholm, Barazzoni and Austin 7 ). ESPEN recommends including information on the result of the nutritional risk screening, the diagnosis, assessment of associated factors, nutritional requirements and the nutrition care plan, including the individual goals listed in the patient documentation. This information should be included in the documentation provided to physicians, dieticians and nurses. The person who is responsible for further treatment in the ambulatory setting should be clearly defined. Information about the food preferences, need for support during meals or oral care should also be included in this documentation( Reference Cederholm, Barazzoni and Austin 7 ).
Although published recommendations are available, goal-oriented communication and documentation are still not being sufficiently addressed in the daily clinical practice( Reference Kripalani, Lefevre and Phillips 8 ). Studies have shown that relevant nutritional information is often lost and is not passed on when the patient is transferred to another care setting( Reference Kripalani, Lefevre and Phillips 8 , Reference Belleli, Naccarella and Pirotta 9 ). In a review of deficits in communication and information transfer between inpatient and outpatient settings, fifty-five observational studies and eighteen controlled studies were analysed. The results show that communication between staff members working in hospital and primary care settings is rather poor. Discharge summaries are often not transferred to the primary care physician and, if they are available, they are often incomplete( Reference Kripalani, Lefevre and Phillips 8 ). No studies could be identified that dealt with the transfer of nutritional information for patients between the hospital and outpatient setting. Incomplete information sharing may reduce the quality of care and the ability of the primary care physicians and therapists to continue providing appropriate nutritional care or making informed decisions( Reference Kripalani, Lefevre and Phillips 8 , Reference Belleli, Naccarella and Pirotta 9 ).
The aim of the current study was to develop a nutritional documentation tool that could be used by healthcare professionals and facilitate the transfer of nutritional patient information between different institutions and care settings. The tool is intended to be used for the transfer of nutritional information for adult patients. The development of the tool was based on information in the literature and experts’ opinions. The information tool was developed in such a way that it is easy to understand and can be introduced into medical record systems around the world.
Methods
Literature review
A comprehensive literature review was performed to develop the content that would be included in the nutritional documentation tool. During the literature search, we identified existing tools and recommendations from expert groups regarding the documentation and transfer of nutritional information. The search was carried out between February 2016 and December 2017. The result of the search included publications that were indexed in the scientific and medical databases MEDLINE (PubMed), Embase and the Cochrane Library. In addition, a literature search was conducted using the search engines Google Scholar and Google as well as a manual search in the bibliographies of the publications identified. We included all types of study designs, set no publication date limitation and included articles written in either the English or German language. The following keywords were used during the search: nutritional documentation, patient discharge, discharge letter, discharge report, standardised terminology and nutritional care process. The titles and abstracts were reviewed by one author. Based on the literature review, a list of content that could potentially be included in the nutritional documentation tool was developed, and details were added by the research team for the subsequent Delphi survey.
Delphi survey
The authors used a modified Delphi technique for consensus building among experts( Reference Keeney, McKenna and Felicity 10 ). The experts were selected for the Delphi panel according to their areas of scientific expertise as well as their clinical experience in the field of nutritional medicine. An attempt was made to collect the broadest range of expert opinions possible, which could then be used to develop the new nutritional documentation tool. For this purpose, the authors used a convenience sample and invited experts from different associations, such as ESPEN and educational institutions for clinical nutrition. To include different perspectives, members of different professions were included, such as dieticians, physicians, nurses and nutritionists. The potential participants of the Delphi survey came from sixteen European countries (one each from Belgium, Denmark, Slovenia, France, Czech Republic, the Netherlands, Greece and Israel; two each from Switzerland, Spain, Sweden, Portugal, Italy and Germany; and three from the UK and five from Austria).
Before the delivery of the Delphi questionnaires, seven persons who were not involved in the study evaluated the understandability and comprehensibility of the questionnaire. The survey was conducted in English language. We sent out the first Delphi questionnaire on 1 June 2016 and asked the participants to respond within 3 weeks. The second Delphi questionnaire was sent out on 1 July 2016 with the same response deadline. We used the online survey platform LimeSurvey™( 11 ). The survey was conducted anonymously to comply with the request made by the Ethics Committee from the Medical University Graz, Austria.
In the Delphi survey rounds, experts were asked to rate each item for its clinical and scientific relevance, not including economic aspects of care (answers of yes or no were possible; quantitative answers). Experts could additionally add comments to each item (qualitative answers). After each Delphi round, the research team met to discuss the results of the survey round. This team consisted of two clinicians (physicians with nutritional backgrounds) and two dietitians from the University Hospital Graz, Austria. During these meetings, all results were summarised and the comments were examined with reference to the scientific literature.
Items that exceeded the cut-off value of 60 % positive replies were included in the nutritional documentation tool. In the literature, an agreement between the participants of 75 % is widely used to demonstrate consensus( Reference Diamond, Grant and Feldman 12 ). After intensive discussions among members of the team, an cut-off value of 60 % agreement was set for the current study. We used this lower agreement cut-off value because we wanted to develop a nutritional documentation tool that was as comprehensive as possible. We assumed that some items would need to be omitted after the subsequent evaluation of the tool by physicians working in clinical practice. The evaluation of an item was repeated if 50–60 % of the raters provided positive replies (i.e. no clear cut-off was reached), and most replies for an item were positive, but many qualitative remarks were provided by the experts or if a new item had been suggested by one of the experts. For these three reasons, these items were sent out in the second round to receive feedback from the experts, until a final consensus was reached for all items.
Evaluation of the nutritional documentation tool
The evaluation of the newly developed tool was conducted with physicians because they are central figures who direct care planning in Austria. Physicians are the first people who deal with transfer letters, such as the nutritional documentation form, when patients are transferred within one institution, to another institution or to the ambulatory setting.
To evaluate the usability of the new nutritional documentation tool, an independent person employed at the Medical Association of Styria (Ärztekammer Steiermark) randomly assigned primary physicians who were working in primary care in the province of Styria (Austria) and were listed in the official doctors’ registry. All of the primary physicians assigned were invited by email to participate in the usability test of the new documentation tool.
In addition, physicians who were working in hospitals and had been randomly selected from the doctors’ registry of the Styrian Hospital Corporation (Steiermärkische Krankenanstalten Gesellschaft m.b.H. KAGes) were contacted via telephone and invited to evaluate the new nutritional documentation tool for its usability during their daily practice in hospital.
If the doctors agreed to participate, they were provided access to the tool via the online survey service platform LimeSurvey™( 11 ). They were asked to assess each item in terms of its usability and relevance in daily practice by choosing one of the dichotomous answers (yes or no). Space for additional comments was not provided as part of this evaluation survey.
Data analysis
The statistical analyses of the quantitative data were performed using SPSS version 21.0 for Windows (SPSS).
During the quantitative analysis of the answers collected from the rounds of the Delphi survey as well as the answers collected from the evaluation of the nutritional documentation tool, a cut-off value of 60 % – in terms of agreement of all respondents – was set. This meant that the content suggestions were considered to be relevant for inclusion in the nutritional documentation tool if 60 % of the experts or clinical and primary care physicians assessed the item as important. If an expert or physician did not provide an answer for an item, this person was not included in the analysis of that respective item.
In the analysis of the evaluation of the nutritional documentation tool by clinical and primary care physicians, the differences among the answers provided by these physicians were calculated by applying Fisher’s exact test. The significance level was determined at P≤0·05.
Ethics statement
For this study, the ethical approval of the responsible medical ethical committee was obtained (28–386 ex 15/16). Participation in the Delphi survey as well as in the evaluation of the newly developed nutritional documentation tool was voluntary.
Results
Literature review
The literature review results did not allow us to identify any studies that addressed the needs of primary care physicians in terms of helping them manage continuing nutritional care in the post-acute setting. Few studies were identified that dealt with the topic of nutritional documentation. The contents of the main studies obtained are shown in Table 1. Rachman-Elbaum et al. ( Reference Rachman-Elbaum, Porat-Katz and Kachal 13 ) described a standardised nutritional documentation tool that was explicitly developed for a geriatric population( Reference Rachman-Elbaum, Porat-Katz and Kachal 13 ). The tool was initially based on the nutrition care process (NCP), which was published by the American Dietetic Association( Reference Lacey and Pritchett 14 ), but this reflects the specific needs and medical care relevant to local patient populations and specific governmental healthcare policies( Reference Rachman-Elbaum, Porat-Katz and Kachal 13 ).
Table 1 Overview of the most important studies for the development of the Delphi survey among experts
Lacey & Pritchett( Reference Lacey and Pritchett 14 ) outlined a general nutritional care pathway and also touched upon the documentation and content that needed to be included in a tool. The content of this publication was, therefore, also included in the development of the survey template.
The ESPEN guideline on definitions and terminology of clinical nutrition( Reference Cederholm, Barazzoni and Austin 7 ) recommends that care records provide information about nutritional risk screening, assessment of risk factors, diagnosis, nutritional requirements, nutritional therapy, goals and outcomes of nutrition therapy. This guideline also suggests that clear references to the time points of goals should be set, how responsibilities should be shared and which information should be provided in the transfer records regarding the patients’ need for assistance while eating and drinking( Reference Cederholm, Barazzoni and Austin 7 ).
The initiatives created by the European Innovation Partnership on Active and Healthy Ageing confirmed the importance of this recommendation for nutritional documentation( Reference Illario, Maione and Rusciano 15 ) and were, therefore, also included during the development of the template.
Based on these recommendations and examples extracted from the literature, the first round of Delphi survey was developed, which included thirty items split into three domains:
(1) Nutritional assessment
(2) Nutrition diagnosis/nutrition intervention
(3) Artificial nutrition
Within each of these three domains, attempts were made to create a standardised documentation tool to facilitate communication among members of all disciplines involved( Reference Hakel-Smith, Lewis and Eskridge 16 ).
Delphi survey
Participants
Initially, twenty-eight raters from across Europe were invited to participate in the first round of the Delphi survey.
Fifteen experts responded and completed the first round of the Delphi survey (response rate 54 %; four physicians, one dietitian and ten professors in the field of nutrition medicine). The second round of the Delphi survey was completed by twelve experts (three physicians, one dietitian and eight professors in the field of nutrition medicine).
Due to the homogenous responses and the high level of agreement among the experts, only two rounds of the Delphi survey were necessary to achieve a consensus. An overview of the experts who participated in the Delphi survey as well as the number of experts who completed the Delphi survey is shown in Fig. 1.
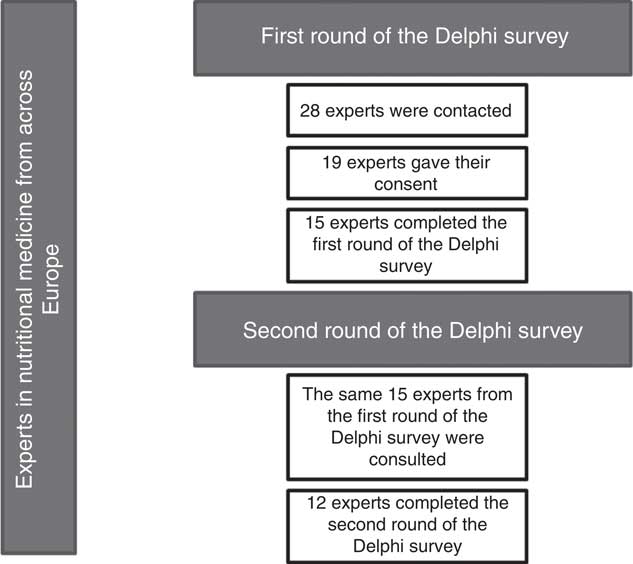
Fig. 1 Experts from across Europe: the number of persons who gave their consent and the number of persons who completed the Delphi procedure.
Results: first round of the Delphi survey
All items in the domains ‘Nutritional Assessment’ and ‘Nutrition Diagnosis/Nutrition Intervention’ were considered as relevant by the experts during the first round of the Delphi survey (consensus rate >60 %; Table 2).
Table 2 Results: first round of the Delphi survey
The Delphi experts did not consider information on the nutritional content of fat and carbohydrates as part of oral nutritional supplements as important enough to be included in the nutritional documentation tool (Table 2).
The following voluntary comments were provided by the experts and, therefore, were included in the second round of the Delphi survey: ‘weight loss during the last three months in percent (%) and kilogram (kg)’ and ‘waist to hip ratio’, information on the micronutrients ‘phosphorus’ and ‘potassium’. Moreover, the experts suggested separating the item ‘enteral and parenteral nutrition’ into the individual items ‘enteral nutrition’ and ‘parenteral nutrition’ and that information on macro- and micronutrients should be introduced for both entities. The experts also suggested that the total amount of daily fluid intake should also be introduced as part of the description of parenteral nutrition in this round of the Delphi survey.
Results: second round of the Delphi survey
For the second round of the Delphi survey, only items for which no consensus had been reached and for which comments that were assessed as relevant were sent out again. An agreement of 50 % was reached among raters for the items ‘phosphorus and potassium in oral nutritional supplements’ and ‘fat, carbohydrates, vitamins, minerals and trace elements in enteral nutrition’. These items were eventually removed from the documentation tool.
A high level of agreement among the experts was reached for all other items, and these were maintained in the documentation tool.
Table 3 shows all the identified items that should be included in the nutritional documentation as part of medical healthcare records. These were subsequently sent out to physicians for further validation in the daily clinical practice.
Table 3 Final list of content included in the developed nutritional documentation tool for use across care settingsFootnote *
* The table also outlines the physicians’ feedback on the usability of the new instrument in the daily practice of ambulatory and inpatient care.
† Items were removed from the documentation tool.
Evaluation of the nutritional documentation tool
In total, eighty-three physicians were asked to participate in the evaluation of the newly developed nutritional documentation tool. A total of twenty-five clinical physicians and twenty-three primary care physicians completed the evaluation survey (response rate of 58 %). This sample represents about 1 % of the registered physicians in Styria and about 0·1 % of all physicians registered in Austria.
Table 3 shows the ratings for usability obtained for the nutrition documentation tool based on the feedback received from primary care physicians and clinical physicians. A significant difference was noted among the opinions of these physicians for the item ‘weight loss during the last 3 months in percent’ (P=0·037). Overall, the item was not assessed as relevant for inclusion in the nutritional documentation tool (<60 % of rating), and it was subsequently removed from the tool. However, the item ‘weight loss given in kilograms’ was assessed positively by both groups of doctors and was maintained in the final version of the documentation tool.
Similar results were obtained for the item ‘malnutrition screening score’. In all, 79·9 % of clinical physicians felt that the malnutrition risk score needed to be documented, but only 59·1 % of primary care physicians felt the same way. Overall, more than 60 % of the doctors agreed that the malnutrition risk score should be documented. The impact of risk scoring for malnutrition has been proven to be effective, as demonstrated in the literature( Reference Roller, Eglseer and Eisenberger 2 , Reference Tappenden, Quatrara and Parkhurst 6 , Reference Eglseer, Halfens and Lohrmann 17 ) and, therefore, this item was maintained in the final version of the nutritional documentation tool.
Moreover, the item ‘food preferences’ was not considered relevant for nutritional documentation by either group and was also removed from the tool.
All other items were considered relevant by both groups and were maintained in the final tool. Table 3 shows the results of the evaluation of the nutritional documentation tool.
Discussion
Information must be transferred in a goal-oriented and patient-centred way from the hospital to the primary care setting, so that the primary care physician can make accurate decisions. However, the process of medical information transfer is not standardised in the daily practice, and few standardisation processes are referenced in the literature. For this reason, key data are often lost during the discharge and transfer of patients( Reference Kattel, Manning and Erwin 18 ). This study addressed the gap between the standardised transfer of clinical nutrition information as suggested by ESPEN and the reality of what occurs in the daily practice( Reference Cederholm, Barazzoni and Austin 7 ).
Based upon the results of a comprehensive literature review on the transfer of nutritional information, the authors developed a template that included items that were primarily related to the nutritional assessment, nutritional diagnosis, nutritional interventions, artificial nutrition and care needs of patients of all ages who were transferred between care settings. The authors used a modified Delphi technique( Reference Keeney, McKenna and Felicity 10 ) to build an expert consensus for core elements that should be included in a nutrition documentation tool in patient records to support transfer processes. Given this basic information, the primary care physician has the opportunity to continue the nutritional care that has begun in the hospital setting.
During the entire consensus-building process, none of the experts questioned the assignment of the three domains that had initially been suggested by the research team, which consisted of two physicians and two dietitians who work at the University Hospital Graz, Austria. This may be due to the fact that this scheme is well known within the community and reflects the NCP as developed by the American Dietetic Association( Reference Lacey and Pritchett 14 ). Experts are used to working within this well-known framework. The experts, clinical physicians and the primary care physicians who were asked to validate the usability of the documentation tool indicated that the framework was easy to follow and did not express any concerns about the use of this structure.
During the first round of the Delphi survey, a rather weak consensus was identified among experts on the role of dieticians in primary care (60 % of raters). This point requires further study. It has been shown in the literature that the dietitians’ skills and knowledge have a strong impact on the patient outcome with respect to the diversity in care and nutritional needs and settings( Reference Mitchell, Ball and Ross 19 ). Today, and especially in the context of an interdisciplinary team, the contributions of dietitians are considered hallmarks for high-quality patient care( Reference Cederholm, Barazzoni and Austin 7 ).
During the first round of the Delphi survey, one rater also suggested including detailed information on weight loss in the documentation that would be transferred between care settings. In the second round of the Delphi survey, the inclusion of this item was proposed, and all raters in the Delphi process agreed on that weight loss should be included in the medical records. This recommendation, which was provided during the rounds of the Delphi survey, is in agreement with the recommendations given by the International Societies of ESPEN( Reference Cederholm, Barazzoni and Austin 7 ) and American Society for Parenteral and Enteral Nutrition (ASPEN)( Reference Mueller, Compher and Ellen 20 ). It also reflects the guidelines of nutrition societies that advocate the general inclusion of weight loss into nutritional screening and assessment tools( Reference Mueller, Compher and Ellen 20 , Reference Kondrup, Allison and Elia 21 ). However, a high level of consensus was noted among experts in terms of expressing the percentage of weight that has been lost during the stay in the hospital or care setting (91·7 % of experts) as compared to expressing the weight loss in kilograms (75 % of experts). The fact that many of the experts work in academic settings may have influenced this feedback. However, because the experts’ personal data were anonymised during the process, and specific statements cannot be correlated with individuals, this remains speculative.
Another weak consensus was found for the inclusion of information on the content of fat and carbohydrate content in any compounds that had been prescribed in the first round of the Delphi survey (33·3 % for inclusion of the fat and carbohydrate content in nutritional supplements; 60 % for inclusion in the enteral and parenteral products prescribed). The documentation of fat and carbohydrate content is particularly important in certain patient populations (e.g. those with diabetes). Once this item had been included in the second round of the Delphi survey, the results showed that the participants of the Delphi survey rated the information on fat and carbohydrate content in enteral nutrition as irrelevant for the nutritional documentation tool (50 % of all raters in round two). Interestingly, the inclusion of the content of fat and carbohydrate in parenteral nutrition was rated positively by the majority of experts. Given the fact that these products are mainly used for patients with complex care needs or during intensive care( Reference Gomes, Schuetz and Bounoure 22 , Reference Singer, Berger and Van Den Berghe 23 ), the impact of the information on further care planning in primary care remains unclear. Although clinical nutrition experts generally have the expertise and knowledge to prescribe and monitor clinical and ‘high-quality’ nutrition in complex patients, it is not expected that this is part of the daily practice of any medical doctor involved in the patient care process( Reference Han, Auer and Cornuz 24 ). Once these domains have been implemented in the routine, it will be necessary to analyse and monitor them for their usability and impact in the daily practice.
During the validation of the new nutritional documentation tool in the daily clinical practice, the mismatch identified for some of the items was similar to the mismatch observed in the results obtained from experts during the Delphi process. The primary care physicians clearly preferred to document weight loss in kilograms of body weight. Furthermore, primary care physicians were clearly in favour of documenting cultural anamneses, which is surprising when considering the weak consensus among the experts regarding food preferences observed during the tool development. However, primary care physicians generally interact closely with the patients and their relatives. The primary care physicians are often the first contact person for healthcare, especially with respect to people with a migration background( Reference Bungartz, Joos and Steinhäuser 25 ). Food and nutrition are topics related to health and disease but also have strong social and cultural backgrounds( Reference Katz, Frates and Bonnet 26 ). Studies have shown that culturally tailored, behavioural and nutritional interventions are more effective than the usual, non-customised interventions( Reference Hawthorne, Robles and Edwards 27 , Reference Eyles and Mhurchu 28 ). To detect possible cultural or social barriers that can be overcome to promote lifestyle changes( Reference Kjøllesdal, Hjellset and Ra 29 ), these interventions may, therefore, also be viewed in the light of public health change management. Primary care physicians, who are central figures in these health promotion activities, should be informed about the changes that need to be made and the possible barriers that practically hinder these interventions.
Another key issue that was identified during the validation of the new nutritional documentation tool was that clinical physicians and primary care physicians had different views on the impact of performing and documenting malnutrition risk screenings between care settings. According to the current literature, few primary care physicians use a malnutrition screening tool( Reference Gaboreau, Imbert and Jacquet 30 ). This is surprising, as more than 70 % of primary care physicians have indicated that they consider annual malnutrition screening in older patients to be useful( Reference Gaboreau, Imbert and Jacquet 30 ). This evidence could be underlined by the results of our study. Given the fact that the majority of patients admitted to hospital wards are at risk of malnutrition( Reference Hiesmayr, Schindler and Pernicka 31 , Reference Morris, Stewart and Riley 32 ), the detection of this risk in primary care is essential in that it allows staff to offer tailored interventions at early stages and reduce risks of related diseases, syndromes, reduced quality of life and future readmission to hospital( Reference Goates, Du and Braunschweig 33 ).
Primary care physicians considered the provision of information about the procedures or screenings that had been conducted, information about advice that had been given to the patients and the caregivers and information about the patient’s specific follow-up needs as highly important, allowing them to provide effective follow-up care. Therefore, tools that allow caregivers to communicate effectively between care settings are of utmost importance for the continuity of adequate care( Reference Kripalani, Lefevre and Phillips 8 ). As part of this study, we developed and presented a standardised and carefully evaluated nutritional documentation tool that can be integrated into medical records and facilitates improved communication between care settings. The information transfer between different wards in a hospital has been shown in a study on data recording in care settings to be non-linear in terms of how the members of various professions gather the information( Reference Benham-Hutchins and Effken 34 ). Implementing nutritional information into records could further improve the efficiency of interdisciplinary collaboration in the field of clinical nutrition in the hospital setting as well as the discharge process to primary care over the long-term. The tool developed in our study has the potential to contribute to improvements in both communication and collaboration.
The major limitation of the work presented was fact that the raters chosen for the modified Delphi survey were selected by convenience sampling. This may have led to potential selection bias, and the results of this study should be interpreted with care in terms of their application to larger populations. The validation for the usability of the instrument was solely performed in Austria. We reached only about 1 % of all physicians registered in Styria and about 0·1 % of all physicians registered throughout Austria. This small sample size limits our ability to generalise our results to other populations. Therefore, authors encourage others to evaluate the usability of the nutritional documentation tool locally. If other healthcare professionals, such as dietitians, carry out other studies to evaluate the nutritional documentation tool, this could provide additional support for its use in new settings.
However, the raters were invited on the basis of their clinical and academic expertise in the field of clinical nutrition. They came from many countries in Europe and, therefore, were considered as a representative group of internationally well-known experts. For this reason, the results of this study can serve as a basic framework for the creation of standardised nutritional documentation tools in general.
The strength of the data presented is the homogeneity and consistency of the feedback received about the new tool. These data reflect a strong degree of consensus among European experts working in the field of nutrition and among physicians working with patients in different care settings. The tool presented in this publication was incorporated into the hospital software at the University Hospital Graz in 2017. This step can easily be taken by any other care provider in Europe.
Conclusion
The current tool was developed on the basis of available evidence (obtained from a literature review) and expert opinions and was evaluated by clinical physicians and primary care physicians for its usability in the daily practice in a care setting in Austria. The results of the study show that there is a lack of nutritional documentation tools described in the literature and that multi-professional experts in clinical nutrition from different European countries have similar opinions about the content of such a tool. The expectations of physicians were similar to those expressed by members of the expert panel. The current version of this instrument can easily be implemented in different care settings throughout Europe and, thus, serves as framework for further developments. However, this newly developed tool requires additional testing regarding its usability in clinical practice in different settings and by different health professionals.
Acknowledgements
The authors acknowledge and thank all the experts that participated in the Delphi survey as well as all the primary care physicians and clinical physicians that participated in the usability survey. The authors also thank members of the local hospital management and especially the dietitians who assisted with the implementation of the documentation tool. This paper was written as part of the Master’s programme Applied Nutrition Medicine at the Medical University Graz and the FH Joanneum.
This research received no specific grants from funding agencies, commercial agencies or organisations in the not-for-profit sector.
R. E. R.-W. and S. B. designed and conducted the study and wrote the manuscript. D. E. wrote and reviewed the paper. A. E. and G. H. W. reviewed the manuscript and helped with the set-up of nutritional documentation tool.
The authors have no conflicts of interest to declare.
Supplementary material
For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S0007114518003781








Target article
Development of a nutritional documentation tool: a Delphi study
Related commentaries (1)
Invited commentary in response to: Development of a nutritional documentation tool: a Delphi study