The metabolic syndrome (MetS) is a cluster of conditions, including abdominal obesity, elevated blood pressure, hypertriacylglycerolaemia, hyperglycaemia and low HDL-cholesterol, which together increase the risk of CVD and type 2 diabetes( Reference Saely, Rein and Drexel 1 ). The prevalence of the MetS has rapidly increased worldwide( Reference Mozumdar and Liguori 2 , Reference Nestel, Lyu and Low 3 ), and diet plays an important role in the prevention and management of the MetS( Reference Chung, Lee and Lee 4 ). A number of studies have explored the association between dairy consumption and the risk of the MetS. However, the relationship remains controversial because of the inconsistency of the results. Some cross-sectional( Reference Kim 5 , Reference Azadbakht, Mirmiran and Esmaillzadeh 6 ) and prospective studies( Reference Lutsey, Steffen and Stevens 7 , Reference Fumeron, Lamri and Abi Khalil 8 ) have shown an inverse association, whereas others have shown no association( Reference Damiao, Castro and Cardoso 9 , Reference Lin, Chang and Tseng 10 ).
Although most studies propose the favourable effects of dairy products on the risk of developing the MetS in Western populations, there is little evidence to draw a cause–effect relationship between dairy consumption and the incidence of the MetS in the Asian population. Generally, dairy consumption is much lower in Asians, especially in Koreans because dairy foods are not a part of the traditional Korean diet and 75 % of Koreans have lactose intolerance( Reference Kim 5 , Reference Scrimshaw and Murray 11 ). Recommendation for dairy food intake is one serving per day for Korean adults( 12 ). According to the data from the Korea National Health and Nutrition Examination Survey, Korean adults consuming ≥1 serving of dairy food/d was 27 %( Reference Lee, Cho and Lee 13 ) and Korean adults consume milk (2·7 servings/week) more frequently than yogurt (1·3 servings/week) or cheese( 14 ). Furthermore, different types of dairy products with a varying nutrient composition may have contributed to these controversial results( Reference Louie, Flood and Rangan 15 , Reference Babio, Becerra-Tomas and Martinez-Gonzalez 16 ). Only one prospective study reported an inverse association between total dairy products with the risk of the MetS in Korean adults( Reference Shin, Yoon and Lee 17 ). However, the study did not examine the effect of individual dairy products on the risk of developing the MetS and the follow-up period was relatively short. Furthermore, the effect of sex on the association between dairy food intake and the risk of incident MetS has not been investigated although some evidences have suggested sex differences on the association between dietary factors and the risk of chronic diseases including the MetS( Reference Bedard, Riverin and Dodin 18 , Reference Kang and Kim 19 ). Therefore, the present study explored the sex-stratified association of individual dairy products such as milk and yogurt, with the risk of the MetS and its components in middle-aged and older Korean adults using data from the Korean Genome and Epidemiology Study (KoGES), a large community-based cohort study. We hypothesised that frequent consumption of dairy products may be associated with a reduced risk of the MetS and individual components.
Methods
Study population
This study is a prospective, community-based cohort study with data collected from the KoGES. KoGES began in 2001 and sought to assess the effects of dietary, environmental and lifestyle determinants on the incidence of chronic diseases such as diabetes mellitus, hypertension and the MetS in the general Korean population. Detailed information on the study procedure was described in a previous report( Reference Lim, Jang and Lee 20 ). In brief, 10 030 Korean adults aged 40–69 years who lived in Ansan (urban) and Ansung (rural) were recruited at baseline between 2001 and 2002. All participants completed interviewer-administered questionnaires on demographic information, lifestyle including dietary habits, their health condition, and medical history, and also anthropometric measurements were acquired and biochemical tests were conducted biennially. The study protocol was approved by the Institutional Review Board of the Korea Centers for Disease Control and Prevention, and informed written consent was obtained from all participants. The present study was based on the data from baseline through the fourth follow-up examination between 2009 and 2010.
Of the original 10 030 participants, 2977 participants had the MetS at baseline, 747 participants refused to participate in the follow-up examinations, 137 participants had CVD or cancer and 659 participants did not complete the baseline or follow-up FFQ; these participants were excluded from the study. In our data, the ninety participants had very low or high energy intake (<2092 or 20 920 kJ/d (<500 or >5000 kcal/d)). We included the participants with unusually low or high energy intake in our analysis because the exclusion of ninety subjects did not affect the results. Thus, 5510 participants (2859 men and 2651 women) were entered into the analysis during the 10-year period from 2001 to 2010, and a follow-up rate of 66 % was achieved, resulting in 30 947 person-years accrued. The average follow-up period was 67·4 months.
Dietary assessment
At baseline and the second follow-up examination, dietary intake was assessed by trained dietitians with a 103-item semi-quantitative FFQ, which has been validated( Reference Ahn, Kwon and Shim 21 ). Total dairy products included milk, yogurt and cheese. Participants were asked to report usual frequency and portion size of dairy consumption during the past year. The answer for frequency had nine options for each food (never or almost never, once per month, two to three times per month, one to two times per week, three to four times per week, five to six times per week, once per day, two times per day, three times per day). The answer for portion size had three options for each food (1/2 serving, 1 serving (standard), ≥2 servings). To enhance the accuracy of serving size, pictures of dairy products and cup models marked with 50, 100, 150 and 200 ml were used as reference materials for serving sizes. One serving was equal to 200 ml of milk, 130 ml of liquid yogurt, 150 ml of solid yogurt and 20 g of cheese( 12 ). For analysis, dairy consumption was converted to weekly frequencies and then multiplied by the reported portion sizes of each food. To estimate whether consuming more than a recommended level of dairy food group (>7 servings/week) affect the incidence of the MetS compared with consuming non-dairy food. Finally, dairy consumption was categorised into five groups (never, <1, 1≤ to <4, 4≤ to ≤7, >7 servings/week) for total dairy and milk and four groups (never, <1, 1≤ to <4, ≥4 servings/week) for yogurt because the number of subjects consuming yogurt frequently was very small. The effect of cheese consumption on the incidence of the MetS was not examined because most of the participants never or rarely consumed cheese. For subjects who acquired the MetS or were censored between baseline and the second follow-up examination, intake of dairy products was evaluated based on the FFQ at baseline; for those who acquired the MetS or were censored after the second follow-up examination, intake of dairy products was evaluated based on the average of FFQ at baseline and FFQ at the second follow-up.
Measurements
Height (cm) and body weight (kg) were measured to the nearest 0·1 cm or 0·1 kg in light clothes without shoes. BMI was calculated as weight (kg) divided by height squared (m2). Waist circumference was measured to the nearest 0·1 cm at the narrowest point between the lowest rib and iliac crest, and the average of three repeated measurements was used in the analysis. Blood pressure was measured with a Baumanometer mercury sphygmomanometer (W.A. Baum) after subjects had rested for 5 min in a sitting position. Systolic and diastolic blood pressures were measured at phases I and V Korotkoff sound, respectively, and were determined as the average of the both arm readings. The blood samples were collected after at least 8 h of fasting state and plasma was separated for biochemical measurements. The concentrations of glucose, TAG and HDL-cholesterol in plasma were measured enzymatically using an autoanalyzer (ADIVA 1650; Bayer HealthCare).
Definition of the metabolic syndrome
We used the diagnostic criteria for the MetS based on the National Cholesterol Education Program Adult Treatment Panel III definition modified by the American Heart Association and the National Heart Lung and Blood Institute( Reference Alberti, Eckel and Grundy 22 ). According to the criteria, the MetS was defined as the presence of three or more of the following: abdominal obesity (waist circumference ≥90 cm in men or ≥80 cm in women); elevated blood pressure (systolic blood pressure ≥130 mmHg or diastolic blood pressure ≥85 mmHg or on antihypertensive medication or physician’s diagnosis of hypertension); hyperglycaemia (fasting blood glucose≥5·6 mmol/l, current use of insulin, oral hypoglycaemic medication or physician’s diagnosis of diabetes mellitus); hypertriacylglycerolaemia (TAG≥1·7 mmol/l); low HDL-cholesterol (HDL-cholesterol<1·0 mmol/l in men or <1·3 mmol/l in women).
Covariates
Educational levels were categorised into three groups: ≤6 years (elementary school graduates), 7≤ to ≤12 years (high school graduates) and >12 years (college graduates or more). Average monthly household income was categorised into four groups: <1 million KRW (approximately <850 USD at 2016), 1≤ to <2 million KRW (approximately 850≤ to <1700 USD), 2≤ to <3 million KRW (approximately 1700≤ to <2500 USD) and ≥3 million KRW (approximately ≥2500 USD). Smoking status was classified as non-smoker, former smoker or current smoker. Alcohol consumption was classified into three groups: non-drinker, former drinker and current drinker. Physical activity was assessed using metabolic equivalent of task (MET) hours per day. To obtain MET, participants reported hours spent on sleep and five types of activities classified according to activity intensity including sedentary, very light, light, moderate and heavy. Total MET-hours per day were calculated by multiplying the reported hours spent by the MET values that were determined based on each type of activity( Reference Ainsworth, Haskell and Whitt 23 ). Daily nutrient intakes such as energy, Ca and fibre were obtained from the semi-quantitative FFQ, and calculated on the basis of the fifth edition of Food Composition Table developed by Rural Development Administration of Korea( 24 ).
Statistical analysis
Statistical analysis were performed with SAS version 9.3 (SAS Institute). Baseline characteristics are expressed as percentage (categorical) or as means and standard deviation (continuous). Comparisons of variables at baseline across total dairy product consumption were analysed by the χ 2 test for categorical data and by the generalised linear models with post hoc Tukey’s HSD (honestly significant difference) test for continuous data. Multivariate adjusted Cox’s proportional hazard models were conducted as a method for survival analysis to assess the hazard ratios (HR) and 95 % CI for incident MetS and its components during follow-up according to the consumption of total dairy products, milk and yogurt either in categorical form or in continuous form (dairy consumption as servings/week). We used an average of dairy products intake calculated from the two dietary measures instead of single measurement to minimise within-subject variation in diet and well represent long-term diet during follow-up( Reference Hu, Stampfer and Rimm 25 ). The proportional hazard assumption that the ratio of hazards is proportional and constant over time was confirmed graphically using log-log plots( Reference Hess 26 ) and statistically based on Schoenfeld’s residuals( Reference Schoenfeld 27 ) with no major violation of the assumption. In multivariable adjusted model, model 1 was adjusted for age, sex, BMI, residential location, educational level, household income, smoking status, alcohol intake and physical activity as covariates and model 2 was adjusted for covariates included in model 1 plus nutrient intakes such as energy and energy-adjusted Ca and fibre using the residual method because dietary Ca and fibre have been suggested to be associated with the risk of the MetS( Reference Shin, Kim and Lee 28 , Reference Moreno Franco, Leon Latre and Andres Esteban 29 ). Sex-stratified analyses were conducted to investigate the association between dairy consumption and the risks of the MetS and individual components of the MetS. To assess the statistical significance for trends of the MetS risk across categories, the median consumption values for each category were used as a continuous variable in the Cox’s proportional hazard models.
Results
Among the 5510 participants, 2103 subjects developed the MetS during the 10-year follow-up.
The baseline characteristics of the study participants according to total dairy consumption is shown in Table 1. Compared with non-dairy consumers, frequent dairy consumers (>7 servings/week) were more likely to be younger male residents of Ansan (urban area), be educated, to have higher income and were less likely to be current smokers and be physically active. Frequent dairy consumers had a lower waist circumference, systolic and diastolic blood pressures, and TAG level and a higher concentration of HDL-cholesterol compared with non-dairy consumers. In addition, frequent dairy consumers had a higher intake of non-dairy food group such as vegetables, fruits and meat as well as nutrient such as energy, energy from fat, Ca and fibre, and a lower intake of energy from carbohydrates.
Table 1 Baseline characteristics of participants according to total dairy consumption (n 5510) (Mean values and standard deviations; percentages)
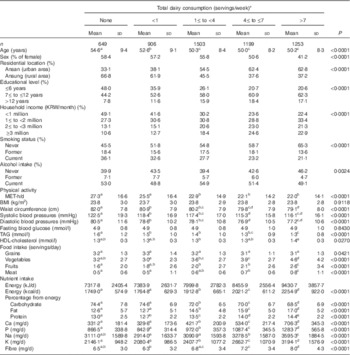
MET, metabolic equivalent of task.
a,b,c,d,e Mean values with unlike superscript letters indicates difference of variables among categories were examined by a generalised linear model (Tukey’s test of multiple comparisons).
* One serving was equal to 200 ml of milk, 130 ml of liquid yogurt, 150 ml of solid yogurt and 20 g of cheese.
The associations between total dairy consumption and incidence of the MetS and its components are summarised in Table 2. Frequent dairy consumers had a 39 % lower risk of the MetS than non-dairy consumers after adjusting for potential confounders such as age, sex, BMI, residential location, educational level, income, smoking status, alcohol intake and physical activity (HR 0·61; 95 % CI 0·52, 0·71, P for trend<0·0001). The inverse association became even stronger after further adjustment for nutrient intake such as energy, Ca and fibre (HR 0·51; 95 % CI 0·43, 0·61, P for trend<0·0001). Frequent total dairy consumption was associated with a reduced risk of individual MetS components (HR 0·51; 95 % CI 0·42, 0·63, P for trend<0·0001 for elevated blood pressure; HR 0·54; 95 % CI 0·45, 0·66, P for trend<0·0001 for hypertriacylglycerolaemia; HR 0·51; 95 % CI 0·43, 0·61, P for trend<0·0001 for hyperglycaemia) compared with that of non-dairy consumers after adjusting for all confounding factors. We analysed sex-stratified association of total dairy consumption with the risk of MetS components. Frequent total dairy consumption was associated with lower risk of incident abdominal obesity (HR 0·49; 95 % CI 0·36, 0·65, P for trend<0·0001 for men; HR 0·45; 95 % CI 0·33, 0·60, P for trend<0·0001 for women) and low HDL-cholesterol (HR 0·81; 95 % CI 0·65, 1·00, P for trend=0·0438 for men; HR 0·44; 95 % CI 0·35, 0·54, P for trend<0·0001 for women) in both sexes. Except for abdominal obesity and low HDL-cholesterol, no sex difference between total dairy consumption and the risk of other MetS components was found (range of P values<0·0001–0·0054).
Table 2 Hazard ratios (HR) for incident metabolic syndrome (MetS) and its components according to total dairy consumptionFootnote * (HR and 95 % confidence intervals)
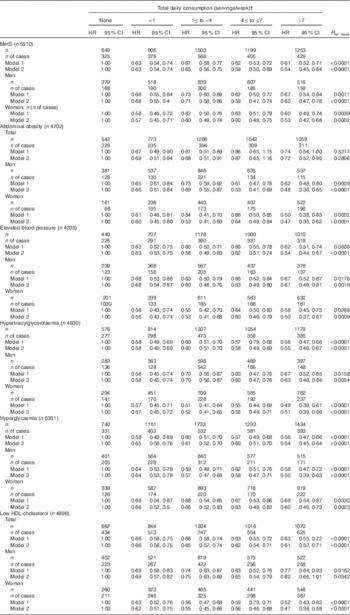
* Model 1: adjusted for age, (sex), BMI, residential location, educational level, household income, smoking status, alcohol intake and physical activity; model 2: further adjusted for nutrient intakes such as energy and energy-adjusted Ca and fibre.
† One serving was equal to 200 ml of milk, 130 ml of liquid yogurt, 150 ml of solid yogurt and 20 g of cheese.
We also observed associations between individual dairy products such as milk or yogurt and the risk of incident MetS and its components (Tables 3 and 4). Frequent milk consumers (>7 servings/week) had a 50 % reduction in the risk of developing the MetS (HR 0·50; 95 % CI 0·38, 0·66, P for trend<0·0001) and individual components of the MetS such as elevated blood pressure (HR 0·45; 95 % CI 0·32, 0·62, P for trend<0·0001) hypertriacylglycerolaemia (HR 0·51; 95 % CI 0·38, 0·69, P for trend<0·0001) and hyperglycaemia (HR 0·44; 95 % CI 0·33, 0·59, P for trend<0·0001) after adjustment for confounding factors compared with non-milk consumers. In sex-stratified analysis, frequent milk consumption was associated with a reduced risk of abdominal obesity only in men (HR 0·64; 95 % CI 0·40, 1·02, P for trend=0·0115) and of low HDL-cholesterol only in women (HR 0·56; 95 % CI 0·42, 0·76, P for trend<0·0001) compared with that of non-milk consumers.
Table 3 Hazard ratios (HR) for incident metabolic syndrome (MetS) and its components according to milk consumptionFootnote * (HR and 95 % confidence intervals)

* Model 1: adjusted for age (sex), BMI, residential location, educational level, household income, smoking status, alcohol intake and physical activity; model 2: further adjusted for nutrient intakes such as energy and energy-adjusted Ca and fibre.
† One serving was equal to 200 ml of milk.
Table 4 Hazard ratios (HR) for incident metabolic syndrome (MetS) and its components according to yogurt consumptionFootnote * (HR and 95 % confidence intervals)

* Model 1: adjusted for age, (sex), BMI, residential location, educational level, household income, smoking status, alcohol intake, and physical activity; model 2: further adjusted for nutrient intakes such as energy and energy-adjusted Ca and fibre.
† One serving was equal to 130 ml of liquid yogurt and 150 ml of solid yogurt.
Similarly, frequent yogurt consumption (≥4 servings/week) was associated with a 33 % reduction in the risk of developing the MetS (HR 0·67; 95 % CI 0·57, 0·78, P for trend<0·0001), and individual components such as abdominal obesity (HR 0·64; 95 % CI 0·50, 0·81, P for trend<0·0001), elevated blood pressure (HR 0·70; 95 % CI 0·59, 0·84, P for trend<0·0001), hypertriacylglycerolaemia (HR 0·68; 95 % CI 0·58, 0·80, P for trend<0·0001) and hyperglycaemia (HR 0·72; 95 % CI 0·62, 0·84, P for trend<0·0001) compared with non-yogurt consumers. In sex-stratified analysis, the risk of low HDL-cholesterol decreased significantly according to increasing yogurt consumption only in women (HR 0·61; 95 % CI 0·51, 0·73, P for trend<0·0001).
When dairy consumption was included in the analysis as a continuous form, total dairy consumption was associated with a reduced risk of incident MetS (HR 0·95; 95 % CI 0·90, 0·99, P for trend=0·0231), but it was not significantly associated with individual components of the MetS (range of P values 0·0667–0·9674, data not shown).
Discussion
In this community-based prospective study with a 10-year follow-up period, we found that frequent consumption of total dairy products or milk (>7 servings/week) were inversely associated a lower incidence of the MetS and all individual components of the MetS including abdominal obesity (only significant in men for milk), elevated blood pressure, hypertriacylglycerolaemia, hyperglycaemia and low HDL-cholesterol (only significant in women for milk) after adjustment for age, sex, BMI, residential location, educational level, income, smoking status, alcohol intake, physical activity and nutrient intakes such as energy, Ca and fibre. Furthermore, increased consumption of yogurt (≥4 servings/week) was associated with a lower incidence of all MetS components (only significant in women for low HDL-cholesterol) as well as the MetS. The results suggest the beneficial effects of milk and yogurt as well as total dairy products on the risk of the MetS.
Our findings are in line with those of other prospective studies indicating an inverse association between dairy consumption and the risk of the MetS. In a prospective study conducted in Australian adults aged 49 years and over, higher consumption of regular-fat dairy products was associated with a 59 % reduction in the risk of the MetS after adjustment for age, sex, smoking status, physical activity, family history of type 2 diabetes, dietary glycaemic load and nutrient intakes including energy, Ca and fibre( Reference Louie, Flood and Rangan 15 ). Fumeron et al. ( Reference Fumeron, Lamri and Abi Khalil 8 ) found that dairy consumption was negatively associated with a lower incidence of the MetS in a 9-year follow-up cohort of 3435 French adults aged 30–65 years. Likewise, a prospective study of 1868 Mediterranean participants aged 55–80 years showed that subjects in the highest tertile of low-fat dairy, low-fat milk and yogurt consumption had a lower risk of incident MetS compared with those in the lowest tertile after adjustment for risk factors during a median follow-up of 3·2 years. In addition, high consumption of whole-fat yogurt was associated with a reduced risk of all of the individual components of the MetS as well as the MetS in itself, which is similar to our results( Reference Babio, Becerra-Tomas and Martinez-Gonzalez 16 ).
In contrast, the results of some studies are not fully consistent with our findings( Reference de Oliveira, McLellan and Vaz de Arruda Silveira 30 , Reference Pereira, Jacobs and Van Horn 31 ). In a cross-sectional study of Brazilian adults aged >35 years, for example, no association between frequent dairy consumption and the prevalence of the MetS was observed( Reference de Oliveira, McLellan and Vaz de Arruda Silveira 30 ). Pereira et al. ( Reference Pereira, Jacobs and Van Horn 31 ) found an inverse relationship between dairy consumption and incidence of the MetS among overweight subjects, but not among subjects with normal weight. The discordant results from these studies may be attributable to differences in the definition of the MetS, study population and study design.
Several potential mechanisms for the favourable effect of dairy products on metabolic risk factors have been proposed. Various nutrients from dairy products including Ca and dairy protein may synergistically protect against all MetS components. Ca in milk products combine with fatty acids and bile acids in the gut, thereby increasing fecal fat excretion and/or inhibiting fat reabsorption( Reference Boon, Hul and Stegen 32 ). As a result, this can improve the ratio of HDL-cholesterol:LDL-cholesterol( Reference Reid, Mason and Horne 33 , Reference Denke, Fox and Schulte 34 ). An intervention study reported that unlike Ca from supplements, Ca from milk or yogurt reduced postprandial TAG levels in healthy male subjects aged 18–50 years old, suggesting dairy Ca reduces fat absorption( Reference Lorenzen, Nielsen and Holst 35 ). Dietary Ca also reduces blood pressure via suppression of 1,25-dihydroxyvitamin D, which increases intercellular Ca in vascular smooth muscle cells( Reference Zemel 36 ).
Dairy proteins may have antihypertensive properties as well. Casein and whey protein, the major proteins in dairy, may regulate blood pressure via inhibition of angiotensin I-converting enzyme, which converts angiotensin I to angiotensin II, a potent vasoconstrictor( Reference Choi, Sabikni and Hassan 37 ). Pal & Ellis( Reference Pal and Ellis 38 ) showed that supplements with 54 g/d of casein and whey protein for 12 weeks significantly decreased blood pressure compared with the placebo group in overweight and obese subjects. Furthermore, fasting TAG and insulin resistance were significantly decreased at week 12 in the whey protein supplemented group compared with the casein or control group( Reference Pal, Ellis and Dhaliwal 39 ). The insulinotropic effect of whey protein may be associated with specific amino acid composition, in particular branched-chain amino acids such as leucine, isoleucine and valine. A mixture of branched-chain amino acids can result in a glycaemic and insulinaemic response that is similar to those seen after whey ingestion in a healthy person( Reference Nilsson, Holst and Bjorck 40 ). Dairy protein-derived peptides may play an important role in preventing the MetS by regulating insulinaemia, blood pressure, dyslipidaemia and fat accumulation( Reference Ricci-Cabello, Herrera and Artacho 41 ). Despite beneficial effects of various components, dairy products have a high proportion of SFA, which have been shown to have harmful effects on metabolic health( Reference Bjornshave and Hermansen 42 ). However, the effect of dairy fat on metabolic risk factors is controversial( Reference Chowdhury, Warnakula and Kunutsor 43 ). Recent studies suggest that dairy fat has different effects depending on the type of dairy products and composition of macronutrients in the meal( Reference Visioli and Strata 44 ).
In our study, yogurt consumption was inversely associated with the risk of the MetS and all components including abdominal obesity, unlike milk. Although yogurt is nutritionally similar to milk, added ingredients (protein, vitamins and minerals) and fermentation may improve its nutritional value and enhance the bioavailability of some minerals such as Ca, Mg and Zn by inducing an acidic environment( Reference Wang, Livingston and Fox 45 , Reference El-Abbadi, Dao and Meydani 46 ). Recent studies showed that high consumption of yogurt was associated with a reduced risk of obesity and the MetS( Reference Martinez-Gonzalez, Sayon-Orea and Ruiz-Canela 47 , Reference Drehmer, Pereira and Schmidt 48 ). Probiotic bacteria from yogurt beneficially influence the balance of gut microbiota. Gut microbiota are considered to play an important role in the development of obesity and obesity-related low-grade inflammation( Reference Verdam, Fuentes and de Jonge 49 ). Bacteria from yogurt ferment indigestible carbohydrates and produce SCFA, which will alter cholesterol synthesis. In addition, some bacteria can bind bile acids to cholesterol and resulting in the excretion of bile acid–cholesterol complexes in the feces( Reference St-Onge, Farnworth and Jones 50 ).
Interestingly, an inverse association between dairy consumption and risk of low HDL-cholesterol was shown only in women regardless of dairy food type. Sex might play a role as an influencing factor on the association between diet and disease risk( Reference Kang and Kim 51 ). The sex difference may be associated with sex hormones. For example, oestrogen enhances fat transport and increases the levels of lipoproteins in the blood, whereas androgen has the opposite effect of oestrogen( Reference Knopp, Paramsothy and Retzlaff 52 ). Therefore, lipid levels could be differently regulated between men and women. Moreover, the lipid levels may respond more sensitive to dietary changes in women than in men( Reference Walden, Retzlaff and Buck 53 ). In this study, changes in lipid metabolism caused by sex hormones might have contributed to a greater association between dairy consumption and the risk of low HDL-cholesterol in women.
Our study has several strengths. The relatively long period of follow-up may be helpful to evaluate the relationship between dairy consumption from the habitual diet and the incidence of the MetS. Furthermore, the use of average consumption in dairy intake from baseline and follow-up FFQ could minimise the random measurement error caused by within-person variation and dietary changes during follow-up. Finally, multiple confounders that might influence the association between dairy consumption and the MetS such as lifestyle factors including nutrient intakes were adjusted for analysis.
The present study has some limitations. First, we could not clarify the effect of dairy subtypes with different fat content on the risk of developing the MetS. Second, this cohort was composed of middle-aged Korean adults, so caution should be used when generalising our findings to other age groups. Third, we have not examined the use of cholesterol medication. Finally, although we extensively adjusted for potential confounding factors of MetS risks, the residual confounding factors which were not considered in the analysis might affect the metabolic risks associated with dairy consumption.
In conclusion, frequent consumption (>7 servings/week) of total dairy products and milk was associated with a lower 10-year incidence of the MetS, abdominal obesity (only significant in men for milk), elevated blood pressure, hypertriacylglycerolaemia, and hyperglycaemia, and increased consumption (≥4 servings/week) of yogurt was associated with a lower incidence of the MetS and all individual components in the middle-aged and older Korean adults. Frequent dairy consumption (milk and yogurt) was associated with lower risk of low HDL-cholesterol only in women. Further studies should be conducted to investigate the effect of dairy subtypes with different fat contents on metabolic risk factors.
Acknowledgements
We thank Korea Centers for Disease Control and Prevention (KCDC) for providing open source data. Epidemiological data used in this study were obtained from the Korean Genome and Epidemiology Study (KoGES; 4851-302) of KCDC, Republic of Korea. This research was supported by the Basic Science Research Program of the National Research Foundation of Korea (NRF), funded by the Ministry of Education, Science, and Technology (NRF2016R1D1A1B03931307). The NRF had no role in the study design, data analysis or writing of this article.
Both authors had a significant role in the project. D. K. contributed to data analysis and writing the manuscript. J. K. contributed to designing the research and writing the manuscript; and also has primary responsibility for the final content. Both authors read and approved the final manuscript.
The authors have no conflicts of interest to declare.







