Systemic arterial hypertension is an independent risk factor for the incidence and mortality from CHD, stroke, heart failure and chronic kidney disease(Reference Forouzanfar, Liu and Roth1,Reference Ettehad, Emdin and Kiran2) . In 2015, 10·7 million deaths and 211·8 million of disability-adjusted life years were attributed to hypertension, a major factor for the global burden of chronic non-communicable diseases(Reference Forouzanfar, Afshin and Alexander3).
The progressive increase of blood pressure (BP) levels and the ultimate hypertension development are associated with health-related behaviours, such as dietary habits(Reference Ndanuko, Tapsell and Charlton4,Reference Frisoli, Schmieder and Grodzicki5) . These outcomes may be prevented by healthy lifestyle attitudes, including regular physical activity, healthy diets, healthy weight maintenance and quitting smoking(Reference Dickinson, Mason and Nicolson6).
The Dietary Approaches to Stop Hypertension (DASH) diet was developed in the 1990s to support hypertension prevention and control(Reference Sacks, Obarzanek and Windhauser7). The DASH diet recommends high intake of fruits, vegetables, low-fat milk and dairy products, whole grains, fish, poultry and nuts, and a limited intake of sweets, added sugar, sugary beverages and fatty meats(Reference Sacks, Obarzanek and Windhauser7). Evidence derived from experimental studies underscored the ability of increased compliance to the DASH diet to lower BP(Reference Siervo, Lara and Chowdhury8–Reference Appel, Moore and Obarzanek11). Overall, these studies involved short follow-up periods, small samples and strictly controlled meals, hardly seen in real life(Reference Sacks, Obarzanek and Windhauser7,Reference Siervo, Lara and Chowdhury8) . In contrast, observational longitudinal studies investigating the relation between the DASH diet and incidence of hypertension have yielded inconsistent results, with evidence of the association of higher DASH-style diet with lower hypertension risk(Reference Bai, Zhang and Zhao12,Reference Schulze, Hoffmann and Kroke13) or absence of association(Reference Jiang, Liu and Troy14–Reference Folsom, Parker and Harnack17). Results from observational studies on the potential benefit of high adherence to the DASH diet are important because they consider individuals in their real context, where living conditions are not controlled and diet variability is much higher. In addition, these studies especially in low- and middle-income countries are scarce, where hypertension is more prevalent.
However, the relationship between the DASH diet and lower risk of cardiovascular outcome seems to be well established. Meta-analyses of cohort studies revealed a linear and inverse association between DASH diet intake and the risks of coronary artery disease, stroke and heart failure(Reference Feng, Fan and Wu18,Reference Salehi-Abargouei, Maghsoudi and Shirani19) . Recent analyses confirm the cardioprotective effects of high adherence to the DASH diet that was associated with the lower risk of specific cardiovascular events (coronary artery disease and stroke), total incident cardiovascular events and also CVD-related death(Reference Jones, Forouhi and Khaw20,Reference Djoussé, Ho and Nguyen21) .
DASH diet benefits are apparently derived from high intake of nutrients with BP-lowering capacity, such as proteins and K, and limited intake of nutrients associated with increased BP, such as saturated fats or salt(Reference Bazzano, Green and Harrison22,Reference Karanja, Obarzanek and Lin23) . Body weight loss resulting from increased adherence to the DASH diet(Reference Soltani, Shirani and Chitsazi24) may also contribute to optimal BP levels, since excess weight is related to increased BP and incidence of hypertension(Reference Semlitsch, Jeitler and Berghold25,Reference Neter, Stam and Kok26) .
Therefore, the objectives of the present study were to investigate whether high adherence to the DASH diet at baseline was associated with lower risk of incident hypertension among free-living adults participating in a multicentre Brazilian cohort.
Methods
Ethical statement
The research was approved by the National Commission for Research Ethics (CONEP) through the approval letter of no. 976/2006, by the Research Ethics Committee of the Federal University of Minas Gerais (COEP/UFMG) and by the ethics committees of the other institutions involved in the study. Additionally, the study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Study population
The Longitudinal Study of Adult Health (ELSA-Brasil) is a multicentre cohort comprising 15 105 active or retired civil services of higher education and research institutions at baseline (2008–2010), aged between 35 and 74 years, located in six Brazilian cities (Belo Horizonte, Porto Alegre, Rio de Janeiro, Salvador, São Paulo and Vitória). Study design, methods and cohort profile have been described elsewhere(Reference Aquino, Barreto and Bensenor27,Reference Schmidt, Duncan and Mill28) . The first follow-up visit to exams and interview was carried out between 2012 and 2014. Data collection included face-to-face interviews, clinical examinations and laboratory tests conducted by trained, certified professionals using standardised instruments. The research ethics committees of participating institutions approved the ELSA-Brasil study. Informed consent was obtained from all individual participants included in the study; all participants signed an informed consent form.
For the present analysis were excluded participants who fulfilled the criteria for hypertension (n 5402), used antihypertensive drugs for other reasons (265) and reported CVD (n 738) at baseline. We also excluded individuals who had changed their dietary habits in the last 6 months because we are studying dietary habits prevailing on the 12 months prior to the baseline interview. Participants who self-reported their race/skin colour as Asian (n 374), Brazilian Indigenous (n 157) and with missing information on BP values (n 14), antihypertensive drug use (n 19), change dietary habit (n 45), diet (n 18), urinary Na (n 447) and race/skin colour (n 184) were excluded. Considering that some exclusion factors overlapped, 5983 participants were thus at risk to develop hypertension in the present study. Of this total, fifty-four (0·9 %) died before the first follow-up visit and 333 (5·7 %) did not attend it. Among those examined at the first follow-up visit, BP values or antihypertensive drug use was missing for thirty-two; thus, the final sample comprised 5632 participants (Fig. 1). Compared with the study participants, those lost to follow-up were older, had lower schooling level and smoked more (P < 0·05 for all comparisons); no differences regarding sex, race, physical activity and BMI were observed (data not shown).

Fig. 1. Flow diagram for selection of the analytic study population.
Hypertension
Hypertension was defined as systolic BP ≥140 mmHg or diastolic BP ≥90 mmHg, or use of antihypertensive drugs(Reference Chor, Pinho Ribeiro and Carvalho29). Both, at baseline and follow-up visit, hypertension was ascertained on the basis of self-reported information and BP measurement. A participant was considered to have a previously diagnosed hypertension when answering ‘Yes’ to the question ‘Are any of the drugs you have taken in the past 2 weeks for hypertension (high blood pressure)?’. Those without a previous diagnosis were evaluated for undiagnosed hypertension based on their BP measurements and then ascertained as having hypertension if they reached the thresholds for systolic BP or diastolic BP.
Baseline and follow-up BP measurements were taken using a validated digital sphygmomanometer (Omron® HEM − 705 CP) in a quiet, temperature-controlled (20–24°C) environment, after 5 min of rest in the sitting position(Reference O’Brien, Mee and Atkins30). Participants were fasting and were instructed to avoid drinking alcoholic beverages and caffeine, and avoid exercising within 12 h prior to examinations. Three measurements were taken 1-min apart, and the average of the second and third values was considered for this analysis(Reference Mill, Pinto and Griep31). Antihypertensive drug use was determined according to drug registry data following analysis of packages and prescriptions and later classified according to the Anatomical Therapeutic Chemical criterion(32).
DASH diet quality score
Dietary habits on the 12 months prior to baseline interviews were measured using a semi-quantitative, 114-item FFQ, with satisfactory reliability for target nutrient assessment (intraclass correlation ranging from 0·55 to 0·83; proteins and vitamin E, respectively) and reasonable relative validity (intraclass correlation ranging from 0·20 to 0·72; Ca and Se, respectively)(Reference Molina, Benseñor and Cardoso33). Nutrients identified via FFQ were quantified as follows: number of servings consumed per occasion × serving weight/size × intake frequency × nutritional content of food serving. Data were converted into daily intake expressed in g or ml. Nutritional content of different food items was extracted from the Nutrition Data System for Research (University of Minnesota) and the Tabela Brasileira de Composição de Alimentos (Universidade Estadual de Campinas – UNICAMP)(Reference Molina, Faria and Cardoso34).
The DASH diet score based on the intake of recommended and restricted food items (in g/d) was obtained by FFQ(Reference Molina, Faria and Cardoso34). Given the low validity of the FFQ-estimated Na intake from ELSA-Brasil(Reference Pereira, Benseñor and Meléndez35,Reference Pereira, Cade and Mill36) , the daily Na intake was determined based on overnight 12-h urinary Na excretion for all study participants. The daily urinary Na excretion was obtained from the adjustment of the 12-h night Na excretion, which corresponds to nearly 47 % of the 24-h Na excretion(Reference Mil, da Silva and Baldo37). The Na excreted during 12-h period (night) was strongly correlated with the gold standard, that is, 24-h urine collection(Reference Baldo, Brant and Cunha38).
The DASH diet score was based on the recommended and restricted food items (groups 1 to 5 and 6 to 8, respectively)(39): (1) fruits; (2) vegetables; (3) nuts, seeds and legumes; (4) cereals and whole grains; (5) low-fat dairy products; (6) sugary beverages; (7) fatty, red and processed meats and (8) Na. For calculation of the DASH score, the consumption of each food group was classified into sex-specific quintiles, allocating a value from 1 to 5, so that a higher value reflected more adherence to the DASH diet recommendations, that is, greater consumption of recommended food groups and lower consumption of restricted food items. Finally, the scores were summed up to obtain the final DASH diet score, ranging from 8 to 40; the higher the score, the greater the adherence to the DASH diet. This score was then categorised into adherence to DASH (low, high). High adherence corresponded to adherence ≥75 %, that is, a DASH score from 30 to 40 points, and low adherence corresponded to adherence <75 % (<30 points). Low adherence was the reference category.
Covariates
Covariates were assessed at baseline and included: (1) socio-demographic characteristics: sex, age groups (35–44; 45–54; 55–64 or 65–74 years), self-reported race/skin colour (White, Brown or Pardo, Black), schooling level (university degree, high school, complete elementary school and incomplete elementary school) and family income per capita (grouped in quintiles: 1st quintile the highest and 5th quintile the lowest); (2) health-related behaviours: smoking (non-smoker, former smoker and smoker), alcohol consumption (non-consumption, moderate and excessive consumption), leisure time physical activity (light, moderate and vigorous) and total energy intake in MJ/d (continuous); (3) family history of hypertension (dichotomical) and diabetes (dichotomical); (4) BMI (kg/m2): BMI < 25, overweight (≥25 BMI < 30) or obese (BMI ≥ 30).
Smokers were defined as those reporting having smoked at least 100 cigarettes in their lifetime and who were still smoking at the time of the interview, and former smokers as those who quitted smoking. Alcohol consumption per week (moderate, non-consumption and excessive) was defined as summed doses of different types of alcoholic drinks consumed in g/week. Moderate alcohol consumption was defined as <210 g/week for men and <140 g/week for women, and excessive alcohol consumption was defined as ≥210 g/week for men and ≥140 g/week for women(40). Physical activity levels were based on the physical activity domain of the long version of the International Physical Activity Questionnaire and categorised according to the time spent at different intensities of physical activity (light, <600 MET-min/week; moderate, 600–3000 MET-min/week; or vigorous, ≥3000 MET-min/week)(41). Family history of hypertension was based on self-reported data. Diabetes was defined as self-reported or fasting blood glucose ≥7·0 mmol/l or 2-h oral glucose tolerance test ≥11·1 mmol/l or glycated Hb ≥6·5 %, and dyslipidaemia as low lipoprotein cholesterol ≥7·2 mmol/l or use of lipid-lowering medication. Anthropometric measurements were taken after fasting using calibrated devices and standardised techniques. Blood samples were collected after 10- to 14-h fasting and stored using standardised protocol.
Statistical analysis
Study population characteristics (baseline) according to adherence to the DASH diet score were expressed as proportions, mean values and standard deviations. The following estimates were made: (1) the total cumulative incidence of hypertension, calculated as the number of new cases of hypertension divided by the total number of participants without hypertension at baseline; (2) age-standardised (5-year intervals) cumulative incidence of hypertension based on total study population according to adherence to DASH diet score. Differences among the groups of the DASH diet adherence and cumulative incidence of hypertension were tested by Pearson’s χ 2 test.
Mean intake of DASH diets’ food items and nutrients, BMI (baseline and first follow-up visit) and inter-wave body weight variation according to adherence to the DASH diet score were described. Differences between means were tested using Student’s t test.
We calculated time to event (detection of hypertension) as the halfway point between the baseline and the first follow-up visit dates for participants whose hypertension criteria were defined by the use of antihypertensive drugs. For incident cases defined on the basis of BP measurements at the follow-up visit, time to event was determined by linear interpolation of baseline and the first follow-up visit dates as the first date that any of the BP values reached the diagnostic criteria (systolic BP ≥ 140 mmHg or diastolic BP ≥ 90 mmHg), whichever occurred first, assuming that BP levels increased at constant rates. Hazard ratios (HR) and 95 % CI were estimated using stratified Cox regression models. When the model does not satisfy the proportional hazard assumptions, the stratified Cox regression model allows control for this variable by entering it as a stratum, in order to satisfy the model assumptions. Thus, the model includes as adjusting variables only the ones that comply with the proportional hazard assumption(Reference Kleinbaum42). The stratification variable in the present study was sex. Proportional hazard assumptions per stratum were guaranteed using Schoenfeld residual analysis.
Following analysis of crude data (model 0), to account for potential confounding on the association between adherence to the DASH diet and incident hypertension, sequential adjustments were made for: age, used as continuous variable (model 1); race/skin colour, schooling level and per capita family income (model 2); smoking, alcohol consumption, leisure time physical activity and total energy intake (model 3); family history of hypertension and diabetes (model 4) and BMI – included in the last model (model 5). Although BMI may have a mediator role in the association between the DASH diet and hypertension, we considered this variable in the regression models because we would like to investigate if this association is independent of this mechanism. Significant variables (P < 0·05) and those considered as confounder on a priori bases were retained in the model.
The DASH diet index was obtained using R programming language version 3.4.1 (R Core Team 2017). Analyses were performed using STATA 14.0 (StataCorp).
Results
In the present study, a total of 780 new cases of hypertension were identified over the course of the follow-up period (3·8 (sd 0·51) years), resulting in a 13·8 % overall cumulative incidence of hypertension among ELSA-Brasil participants in 3·8 years.
Baseline participant characteristics are shown in Table 1. The mean age was 49·9 (sd 8·3) years, most participants were women, self-reported white as race/skin colour, had completed university education, reported light physical activities and had never smoked.
Table 1. Baseline characteristics according to adherence to the Dietary Approaches to Stop Hypertension (DASH) diet and incidence of hypertension, Longitudinal Study of Adult Health (ELSA-Brasil), 2008–2010 (n 5632)
(Numbers and percentages; mean values and standard deviations)

The intake of items recommended by DASH was at least 25 % higher in the group with the highest adherence to the diet. The intake of low-fat dairy products differed most between the two groups (mean intake was 2·4 times higher in the high adherence group compared with the low adherence group). In contrast, mean red/processed/fatty meat, sugary drinks and Na intake were 2·8-, 2·5- and 1·3-fold higher in the low compared with the high adherence group, respectively (Table 2).
Table 2. Food consumption components of the Dietary Approaches to Stop Hypertension (DASH) diet score according to adherence to DASH diet score, Longitudinal Study of Adult Health (ELSA-Brasil), 2008–2010
(Mean values and standard deviations)

* Participants with DASH score >75 %.
† Student’s t test.
‡ Estimated from overnight 12-h urinary Na excretion.
Age-standardised incidence of hypertension was significantly 28·6 % lower in the high (10·0 %; 95 % CI 8·0, 12·0) compared with the low (14·0 %; 95 % CI 13·0, 15·0) DASH diet adherence group (P < 0·05) (Fig. 2).

Fig. 2. Age-standardised incidence of hypertension with 95 % CI according to the level of adherence to the Dietary Approaches to Stop Hypertension (DASH) diet, Longitudinal Study of Adult Health (ELSA-Brasil), 2008–2010/2012–2014. Pearson’s χ 2: P < 0·05.
HR and respective 95 % CI for incidence of hypertension according to adherence to the DASH diet are shown in Table 3. In the crude analysis, the high adherence to the DASH diet was not statistically associated with hypertension risk (HR 0·81; 95 % CI 0·63, 1·02). However, high adherence to the DASH diet was associated with lower risk of hypertension, as compared with medium adherence following adjustment for age (HR 0·68; 95 % CI 0·59, 0·95 (model 1). The magnitude of this association decreased slightly after adjustment for race/skin colour, schooling level and family income per capita (model 2), health-related behaviours (model 3), family history of hypertension and diabetes (HR 0·74; 95 % CI 0·57, 0·95) (model 4). After adjustment for BMI, participants with high adherence to the DASH diet presented hypertension incidence 20 % lower compared with medium adherence, although it was of borderline statistical significance (HR 0·81; 95 % CI 0·63, 1·04) (P = 0·083) (model 5). Proportional hazard assumptions per stratum were guaranteed (Schoenfeld P = 0·23).
Table 3. Crude and adjusted association between adherence to Dietary Approaches to Stop Hypertension (DASH) diet score and incident hypertension, Longitudinal Study of Adult Health (ELSA-Brasil), 2008–2010/2012–2014
(Hazard ratios and 95 % confidence intervals)

Model 0, crude analysis; Model 1, Model 0 + age; Model 2, Model 1 + race /skin colour, education, family income per capita; Model 3, Model 2 + smoking, physical activity, alcohol consumption, total energy intake; Model 4, Model 3 + family story of hypertension, diabetes; Model 5, Model 4 + BMI.
In the baseline, mean BMI decreased as adherence to the DASH diet increased. Follow-up analysis revealed weight gain regardless of the level of adherence to the DASH diet; however, body weight changes were smaller in the high adherence group (Table 4).
Table 4. Indicators of adiposity and adherence to the Dietary Approaches to Stop Hypertension (DASH) diet, Longitudinal Study of Adult Health (ELSA-Brasil), 2008–2010/2012–2014
(Mean values and standard deviations)
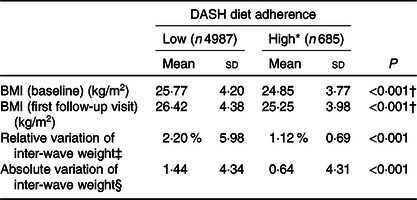
* Participants in the highest 25 % on the DASH score.
† P trend < 0·05.
‡ % = weight ((wave 2 − baseline weight)/baseline weight) × 100.
§ kg = weight (wave 2 − baseline weight).
Discussion
In this large cohort of middle-aged Brazilian adults, the high adherence to the DASH diet was statistically associated with a 26 % reduction in the risk of developing hypertension after about 4-year follow-up. This association was independent of potential confounding factors, such as socio-demographic characteristics, health-related behaviours, family history of hypertension and diabetes. The magnitude of this association reduced to 19 % after adjustment for BMI, and the statistical significance was borderline.
Antihypertensive effect of the DASH diet is thought to result from the balance and the combination of nutrients recommended in this dietary standard(Reference Karanja, Obarzanek and Lin23). These nutrients seem to act on BP via different and complementary mechanisms. Dietary proteins have lower glycaemic index compared with carbohydrates and are thought to improve insulin sensitivity, which enhances nitric oxide production by the vascular endothelium. It is also associated with higher plasma concentrations of amino acids with vasodilating properties and enhanced renal plasma flow, glomerular filtration rate and Na excretion, thereby regulating the BP(Reference Rebholz, Friedman and Powers43,Reference Vasdev and Stuckless44) . BP-lowering effects of K-rich diets are related to decreased vascular smooth muscle contraction(Reference Bazzano, Green and Harrison22). K also enhances natriuresis, improves insulin sensitivity and reduces oxidative stress(Reference Houston45). Mg is thought to act in combination with K in BP control(Reference Bazzano, Green and Harrison22), while Ca (along with K, Na and Mg) stabilises vascular cell membranes, inhibits its own entry into cells and decreases vasoconstriction(Reference Houston and Harper46).
The association observed here between high adherence to the DASH diet and lower incidence of hypertension is in line with a cohort study based on a subgroup of China Health and Nutrition Survey participants followed for 11 years(Reference Bai, Zhang and Zhao12). In the latter study, the association seen was stronger when only normal weight participants (BMI 18·5–24 kg/m2) reporting moderate or vigorous levels of daily physical activity at baselinewere accounted for(Reference Bai, Zhang and Zhao12). In contrast, 6-year follow-up of the Seguimiento Universidad de Navarra cohort failed to reveal statistically significant associations, in spite of a linear trend towards higher adherence to the DASH diet and lower risk of hypertension(Reference Toledo, Carmona-Torre and Alonso15). The Iowa Women’s Health Study revealed statistically significant association between adherence to the DASH diet and low hypertension, regardless of age and daily energy intake but not of other risk factors, including BMI(Reference Folsom, Parker and Harnack17). In the European Prospective Investigation into Cancer and Nutrition-Potsdam study, including only female participants, an independent association between the DASH diet and lower incidence of hypertension was limited to the third quartile of the final adherence score to the DASH diet(Reference Schulze, Hoffmann and Kroke13). Associations between the DASH diet and hypertension were also lacking in two other prospective observational studies(Reference Jiang, Liu and Troy14,Reference Camões, Oliveira and Pereira16) .
Findings of the present study suggest that the association between high adherence to the DASH diet and lower risk of hypertension is not independent of BMI. At baseline, BMI was smaller in participants with high adherence to the DASH diet. Because there is a consistent direct relation between body weight and BP levels both in observational studies and randomised clinical trials(Reference Neter, Stam and Kok26,Reference Stevens, Chambless and Neto47) , and the DASH diet is also associated with lower BMI(Reference Smethers and Rolls48–Reference Blumenthal, Babyak and Hinderliter52), it is likely that part of the protective effect of the DASH diet on incident hypertension is partly mediated by lower BMI. In a meta-analysis of randomised clinical trials, subjects complying to the DASH diet achieved significantly greater weight loss compared with the control group in studies with no energy restriction (−0·85 kg, 95 % CI −1·27, −0·82)(Reference Soltani, Shirani and Chitsazi24).
In the present study, similar to others(Reference Jiang, Liu and Troy14,Reference Toledo, Carmona-Torre and Alonso15) , the high-adherence DASH diet group presented higher average energy intake than the low adherence group, even though they had both lower BMI and incidence of hypertension. These apparent intriguing findings might be explained by diet quality and physical activity level. In our study, the high adherence to the DASH diet group reported greater intake of fibre, vegetable protein, white meat and PUFA. A previous study found that weight gain was more strongly associated with sugar-sweetened beverages, red and processed meat and inversely associated with the intake of vegetables, whole grains, fruits, and nuts, while low fat dairy intake was not linked to weight gain(Reference Mozaffarian, Hao and Rimm53). As the high adherence group in our study also had greater prevalence of moderate and vigorous physical activities as compared with the other group, we cannot rule out that the mean BMI of the high adherence group has greater influence of lean mass than the BMI of the low adherence group.
Current DASH diet Na intake recommendations correspond to approximately 2·3 g,(39) and related BP-lowering effects are thought to be more marked when is combined with low-Na diet(Reference Juraschek, Miller and Weaver54–Reference He and MacGregor56). As expected, mean salt intake decreased as adherence to the DASH diet increased. Estimated Na intake (based on overnight 12-h urinary Na excretion) in the high adherence group was 50 % and almost 30 % lower compared with the low and medium adherence groups, respectively (P < 0·05). Still, mean Na intake in the high adherence group (3·2 (sd 1·6) g/d) exceeded WHO (2 g/d) and DASH guideline recommendations (2·3 g/d)(39,57) . Brazilian Na intake estimates suggest 72 % of Na intake to be derived from table salt and seasonings, which may be present even in diets rich in vegetables, whole grains, lean meats, dairy products, nuts and seeds(Reference Sarno, Claro and Levy58). Thus, we cannot rule out Na intake that remained high even among DASH diet followers, contributing to the low effect of the DASH diet on incident hypertension in the present study.
High adherence to the DASH diet was more common among participants reporting moderate to vigorous physical activity, non-smokers and those drinking moderate or none alcohol amounts. Individuals with healthy dietary habits are likely to adhere to other healthy behaviours(Reference Short and Mollborn59). Studies involving lifestyle interventions have shown BP-related benefits of the DASH dietary pattern to be even more pronounced when dietary changes are part of lifestyle change programmes, particularly those aimed to promote physical activity and reduce excess body weight, inadequate Na intake and excessive alcohol consumption(Reference Blumenthal, Babyak and Hinderliter52,Reference Appel, Champagne and Harsha60) .
The present findings confirmed the role of the DASH diet on prevention of the hypertension in this cohort. However, compared with medium adherence to the DASH diet, low adherence to the DASH diet was not associated with increased risk of hypertension. Taken together; these results emphasised the combined effects of nutrients of the DASH diet on BP-lowering effects, while the absence of this dietary pattern does not seem to be a potential risk factor to hypertension.
The large study population and inclusion of different regions of Brazil (and hence different cultural and dietary contexts)(Reference Schmidt, Duncan and Mill28) are some of the strengths of the present study. In addition, the large ELSA-Brasil sample allowed the investigation of independent associations between adherence to the DASH diet and hypertension. The use of standardised BP measurement procedures and strict quality control in ELSA-Brasil(Reference Schmidt, Duncan and Mill28,Reference Mill, Pinto and Griep31) suggest impacts of measurement errors on study findings to be unlikely. However, limitations must be accounted for. First, the food intake was estimated using FFQ, and these instruments may overestimate intake, particularly when addressing more than 100 food items(Reference Willett61). Despite potentially overestimated absolute intake of DASH diet items, relative comparison between the three groups with different levels of adherence may mitigate this error. Second, although we have included many potential confounding factors, we cannot rule out the possibility of residual confounding. Third, the 3·8-year follow-up in the present study was short as compared with previous studies, but the incidence of hypertension was high and the likelihood of diet change is lower than expected in longer follow-up periods. Fourth, participants who refused to attend to the first follow-up visit had lower schooling level and smoked more; thus, these follow-up losses probably attenuated the associations observed, as these variables are associated with lower adherence to the DASH diet and higher hypertension risk. Finally, although the ELSA-Brasil participants are civil servants with higher average schooling level, we do not believe that this fact undermines our results, as many scientific evidences on risk factors for chronic diseases have come from selected occupational cohorts, such as the Nurses’ Health Study, or from very selected community-based cohorts such as the Framingham Health Study(Reference Rothman, Gallacher and Hatch62,Reference Richiardi, Pizzi and Pearce63) .
Conclusion
High adherence to the DASH diet was associated with 19 % lower risk of hypertension in about 3·8 years of follow-up. Also, our results suggest that body weight may be an important pathway behind the impact of the DASH diet on BP levels in this cohort. Our finding emphasises the relevance of this dietary strategy for hypertension prevention and hence of related CVD.
Acknowledgements
The authors thank the staff and participants of the ELSA-Brasil study for their important contributions.
This work was supported by the Brazilian Ministry of Health (Department of Science and Technology) and the Brazilian Ministry of Science, Technology and Innovation (Financiadora de Estudos e Projetos, FINEP; and Conselho Nacional de Desenvolvimento Científico e Tecnológico, CNPq), through grant nos. 01 06 0010.00 RS, 01 06 0212.00 BA, 01 06 0300.00 ES, 01 06 0278.00 MG, 01 06 0115.00 SP and 01 06 0071·00 RJ. The present study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES) – Finance Code 001. R. H. G., D. C., M. D. C. B. M., J. G. M., S. M. A. M., I. M. B. and S. M. B. are CNPq research fellow. L. F. A. received a postdoctoral scholarship from CNPq (grant no. 150248/2015-6)
S. C. F. contributed to the conception and design, data analysis and drafting the manuscript. L. G., L. F. A. contributed to the conception and design, data acquisition, data analysis and drafting the manuscript. S. M. B. contributed to the conception and design, data acquisition, data analysis and approved the final version of the manuscript. R. H. G., J. G. M., D. C., M. D. C. B. M. and S. M. A. M., and I. M. B. contributed to data acquisition, intellectual content during manuscript drafting, reviewed and commented on data analysis and approval the final version of the manuscript.
The authors declare that there are no conflicts of interest.









