Background
People with severe mental illness, such as schizophrenia, schizoaffective disorders and bipolar disorder die 10 to 20 years earlier compared with the general population.Reference Chesney, Goodwin and Fazel1–Reference Liu, Daumit, Dua, Aquila, Charlson and Cuijpers3 The mortality rate is two to three times higher than the general population.Reference Chesney, Goodwin and Fazel1,2,Reference Fekadu, Medhin, Kebede, Alem, Cleare and Prince4 However, most evidence is from high-income countries with better health services and higher health literacy;2 the limited studies from low- and middle-income countries suggest a more serious situation. One study from rural Ethiopia reports premature mortality by 30 years for people with severe mental illness,Reference Fekadu, Medhin, Kebede, Alem, Cleare and Prince4 and three studies from China report a 1.8Reference Zhou5,Reference Zhang, Wang, Li, Yang and Zheng6 or 4.0Reference Ran, Chen, Conwell, Chan, Yip and Xiang7 times mortality rate for patients who are mentally ill, and the standardised mortality was higher than the general population across the whole lifespan.Reference Zhou5 However, evidence about mortality rates of patients with mental disorders in China is scant, especially considering the limited geographical coverage of existing data.Reference Zhou5–Reference Ran, Chen, Conwell, Chan, Yip and Xiang7
The integration of mental health into primary healthcare has been recognised as the most effective approach to closing the gap between need and demand for mental health services in low- and middle-income countries.8–Reference Kauye, Chiwandira, Wright, Common, Phiri and Mafuta10 In 2004, the Chinese government implemented the ‘686 Program’ in certain regions as a pioneering model for comprehensive management and treatment of patients with severe mental illness (SMI).Reference Ma, Liu, He, Xie, Xu and Hao11,Reference Liang, Mays and Hwang12 The programme assesses the feasibility of hospital–community integrated services,Reference Ma, Liu, He, Xie, Xu and Hao11,Reference Liang, Mays and Hwang12 and prioritises identification and treatment of patients with SMI, especially those with violent tendencies.Reference Ma, Liu, He, Xie, Xu and Hao11 In 2009, the government expanded the ‘686 Program’ by integrating mental healthcare into the primary public health service and scaling up the coverage to almost the whole country.Reference Liang, Mays and Hwang12,13 Patients with SMI are diagnosed by psychiatrists and followed up regularly by trained service providers (including psychiatrists, general practitioners or nurses in urban community healthcare centres or rural township hospitals). The programme promotes standard medication, regular physical examinations, health education, rehabilitation and referrals to psychiatrists. A performance evaluation based on 280 000 registered patients in 160 cities in China showed that, from 2006 to 2011, the proportion of patients remaining stable increased significantly from 67.0% to 90.7%, the proportion of aggressive behaviour decreased from 4.8% to 0.5%,Reference Ma, Liu, He, Xie, Xu and Hao11 and a total of 94 000 prescriptions of free medication and 12 400 sessions of free treatment had been provided.Reference Ma14 Because of limited resources and a primary concern for social stability,Reference Liu, Ma, He, Xie, Xu and Tang15 the government placed its primary focus on mental illnesses with a high possibility of violent or socially disruptive behaviours.13 Thus, six mental disorders with violence tendency – schizophrenia, schizoaffective disorder, delusional disorder, bipolar disorder, psychotic disorder due to epilepsy and disorders of intelectual development with psychosis – are included in the primary mental health services programme.
Community measures and SMI
The government has defined two measures as the performance indicators for the primary mental health programme, disease stability and high-risk behaviour. But little is known about their association with mortality despite the programme being in effect for over 10 years. And medication adherence, which is not under official surveillance but has abundant evidence proving its significance in the treatment of mental illness,Reference Chapman and Horne16 is an important process indicator in the programme, with scant research about its association with mortality based on the programme.
Aims
The World Health Organization (WHO) recommends using a multilevel intervention framework (MIF) model, informed by multilevel risk factors for excess mortality in people with SMI at the individual, health system and socio-environment levels, aiming to identify priorities for clinical practice, policy and research.Reference Liu, Daumit, Dua, Aquila, Charlson and Cuijpers3 Following the MIF model, this study aimed to:
(a) assess mortality of patients with SMI in Sichuan, China and compare this with the general population;
(b) examine how progress on three core indicators measuring community-based patients with SMI management i.e. high-risk behaviour, disease stability and medication adherence, is related to mortality; and
(c) explore other multilevel risk factors.
Method
Data source
Participants were registered patients on the National System of Basic Information Collection and Analysis for Psychoses (NSBICAP) in Sichuan from 1 January 2009 to 31 January 2014. The NSBICAP is the only mental health surveillance system in China,Reference Zhou and Xiao17 collecting information from patients with SMI on disease stability, violent or socially disruptive behaviours, treatment care (for example taking medication or admission to hospital) and survival status.Reference Zhou and Xiao17 Sichuan Province is located in southwest China, with a population of over 81 million living in 21 municipalities. There were 158 957 patients registered in the NSBICAP in January 2014, accounting for approximately 20% of the total estimated 800 000 patients with SMI in Sichuan.Reference Wen, Wang, Wang and Yang18
The recruitment of patients into the NSBICAP includes two pathways: (a) referral from psychiatric hospitals or departments in general hospitals to urban community health centres or rural township hospitals; and (b) direct identification or referral from local communities, community health centres, hospitals, village committees, or the China Disabled Persons’ Federation (a national organisation for individuals with disabilities).13 Individuals identified from the second pathway are diagnosed by psychiatrists. All participants diagnosed with one of the six specific diseases and with signed informed consent are registered in the NSBICAP, and are managed by doctors or nurses from community health centres or township hospitals.
Once registered, patients are evaluated in terms of high-risk behaviour (harm to people or damage to property), disease stability, mental symptoms and severe physical diseases, social function and adverse drug effects.13 They are then followed up at intervals based on their disease stability (stable, more or less stable, or unstable). The frequency for patients who are stable is every 3 months, and every 2 weeks for other patients. At follow-up, each patient is re-evaluated on the same aspects as above, as well as on medication adherence.
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human patients were approved by the Institutional Review Board at Sichuan University and Mental Health Center of Sichuan Province.
Community management indicators
The three indicators, high-risk behaviour, disease stability and medication adherence, were defined in order to measure community management. All indicators are defined by the Chinese government to assess community-based mental healthcare.13 These three measures were assessed at each follow-up for all registered patients and reflect the conditions from the last survey to date.
High-risk behaviour was assessed on a scale of 0 to 5 according to the degree of damage a patient enacted against people or property either verbally or physically, with level 0 indicating no damage at all, and levels 1 to 5 gradually increasing in terms of the degree of damage, as reported by relatives or hospital records from each follow-up. The detailed definition can be found elsewhereReference Liu, Liu, Wen, Wang, Yang and Tang19 and in the Supplementary material 1 available at https://doi.org/10.1192/bjo.2021.46. This factor was categorised into low risk (level 0–2) and high risk (level 3–5) for this study.
Based on the 2012 Chinese Managerial and Treatment Regulations for Severely Mentally Disordered Patients, disease stability is a comprehensive indicator encompassing assessment of risk behaviour, insight, psychotic symptoms, adverse drug reaction and physical diseases, with the back-up support of psychiatric specialists.13,Reference Ma14 At least one psychiatrist would be included in the community management team of each community health centre or township hospital. And a regular top–down on-site instruction from psychiatric specialists to doctors or nurses of community health centres or township hospitals was conducted quarterly. Insight and psychotic symptoms were initially diagnosed by psychiatric specialists following the ICD-10 standards (F20 for schizophrenia, F25 for schizoaffective disorder, F22 for delusional disorder, F31 for bipolar disorder, F06 for psychotic disorder due to epilepsy, and F70–F79 for mental retardation with mental disorders)Reference Jingwu20 and followed up regularly by trained doctors or nurses.
Adverse drug reactions for patients prescribed medicine by psychiatrists was also collected by the trained doctors or nurses at each follow-up. Physical diseases were diagnosed by licensed doctors. If patients could not continue their work or were incapable of living independently because of physical diseases, they would be considered as having severe physical diseases. Disease stability was categorised into stable and unstable. Stable was defined as high-risk behaviour at level 0 to 2, with complete insight, free of psychotic symptoms, free of serious adverse drug reaction and free of severe physical diseases. Unstable was defined if high-risk behaviour was assessed at level 3 to 5, or if patients had a poor condition in any of the remaining aspects including insight, psychotic symptoms, adverse drug reaction or physical diseases.
Self-reported medication adherence was assessed among those who were prescribed medications to treat mental illnesses (including all medication available to treat mental illnesses, such as antipsychotic and mood stabilising drugs), and was categorised into adherent (taking medicine according to prescription), taking a lower dose of medication or taking it at a reduced frequency than prescribed and refusing to take medicine.
Outcome
Death status at each follow-up was recorded in the NSBICAP, and the date of death of the patient was defined as the survey date when the patient's status was ‘died’. We calculated survival time by month from the date of enrolment in the NSBICAP to the date when a ‘died’ status was recorded, or to the last contact date for those lost to follow-up or censored by 31 January 2014.
Covariates
Based on the MIF model,Reference Liu, Daumit, Dua, Aquila, Charlson and Cuijpers3 baseline covariates were grouped into five categories. The first category was disorder-specific factors including disease diagnosis, and family history of mental disorders (yes versus no). The second category was socioeconomic position that includes education (no formal education or illiterate, primary or middle school, or high school or above), occupation (employed/student/retired, unemployed, or farmer) and family economic status (poverty versus non-poverty; dichotomised as above or below the poverty line defined by local governmentsReference Ma, Liu, He, Xie, Xu and Hao11). The third category was the cultural and societal aspects of ethnicity (Han versus minority). The fourth category was social support, meaning marital status (married versus unmarried). The final category was on health systems and context factors at the county level that consisted of area socioeconomic status (gross domestic product (GDP) per capita, the average figure in 2009, 2011, and 2013 provided by the Health Bureau of Sichuan), the average travelling time to the nearest hospital computed using the topographic data-set of the National Fundamental Geographic Information System of China in 2012,Reference Pan, Liu, Wang, Xie and Delamater21 and the number of mental health hospitals (including psychiatry departments in general hospitals) per 100 000 people. These variables covered 146 counties where participants resided during the study period. Gender and baseline age were other adjustable covariates.
Study population
The study population is shown in Fig. 1. From 1 January 2009 to 31 January 2014, the NSBICAP database registered 158 953 patients with SMI managed by primary health facilities (community health centres and township hospitals). We excluded: (a) 2103 patients with missing values in all three community indicators; (b) 2042 patients with ‘logic errors’ in the data between dates of birthday, SMI onset and enrolment; (c) 20 626 patients under age 15 years at baseline, as individuals younger than 15 years were unlikely to receive SMI diagnoses.Reference Chang, Hayes, Perera, Broadbent, Fernandes and Lee22 A total of 134 182 participants were identified for the current study: 32 392 (24.1%) patients had records for 1 year, 44 282 (33%) for 2 years, 48 978 (36.5%) for 3 years, 8308 (6.2%) for 4 years, and 222 (0.2%) for 5 years.
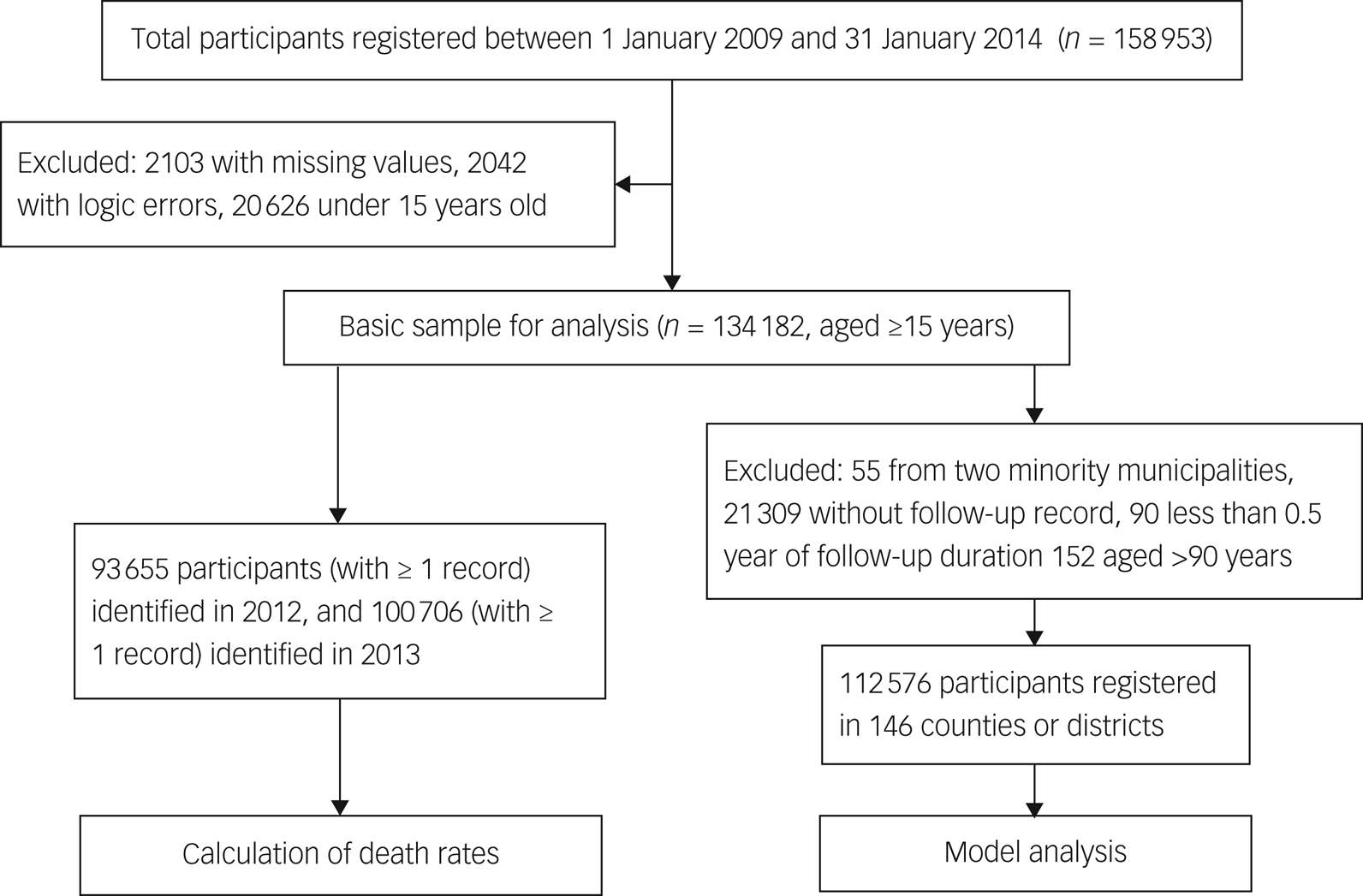
Fig. 1 Flow chart of study population.
To compare the disparity of mortality between patients with SMI and the general population, we calculated mortality rates for 93 655 individuals with at least one record in 2012 and 100 706 individuals with at least one record in 2013 (Fig. 1). We did not calculate mortality for 2009, 2010 or 2011 because the mortality rates seemed implausible compared with the general population, possibly because of the early system being unable to cope with data requirements. We did not calculate the death rate for 2014 as only data for January were available.
To examine the association between all-cause mortality and risk factors, of the 134 182 participants aged ≥15 years and registered from January 2009 to January 2014, we further excluded (a) 55 patients from two minority municipalities due to infrequent participation; (b) 21 309 patients who did not have follow-up records for high-risk behaviour, disease stability or medication adherence; (c) 90 patients whose follow-up duration was less than 0.5 month (completed months of follow-up duration were used in the multilevel survival analysis); (d) 152 patients older than 90 years (Fig. 1). Finally, we included 112 576 participants who were registered in 146 out of 183 county-level administrative regions in Sichuan Province. We also conducted a sensitivity analysis excluding those lost to follow-up to estimate the association between community management measures and mortality. To simplify it, we consider participants lost to follow-up if their last contact dates were on or before 31 July 2013 as the longest follow-up interval was 6 months. Of the 112 576 individuals, 88 625 (78.7%) were included in the sensitivity analysis.
Statistical analysis
To answer the first research question, we first calculated the 1-year crude mortality rate of patients with SMI for 2012 and 2013. The numerator was the number of all-cause deaths; the denominator was the total number of registered patients with at least one record subtracting half the number of deaths. We then calculated the age-specific standardised mortality ratio (SMR) and its 95% CI by years with an indirect method, taking the general population of Sichuan Province, obtained from the 2010 census, as the reference population.
For the second and third research questions, we first calculated death rates (defined as number of deaths divided by total follow-up duration, which was person-years) and its 95% CI for patients with different characteristics. Then we used a two-stage modelling approach: growth models in the first stage to identify change in patterns for repeated measures over time, and multilevel proportional hazard models in the second stage to estimate the association between death and the change in patterns for the community measures, as well as other risk factors. Each community management measure was examined separately. In the growth models, with repeated time points at level 1 and individuals at level 2, each patient had a specific linear slope over time. We defined community measures as ‘better’ in progression in the positive highest third of the slope, and defined measures as ‘worse’ in progression in the negative lowest third of the slope. Otherwise, the progression was labelled ‘no change’. We fitted four separate proportional hazard models for each community measure: we only regressed the progression of the measure in model 1 (minimal model), added the baseline community measure in model 2, added other individual covariates in model 3, and added county-level covariates in model 4 (full model). The effects of covariates in the framework of the MIF model were estimated in the full model. More details about the modelling approach are given in the Supplementary material 2.
We used MLwiN 2.32 to fit the growth models and multilevel models, and Stata 13.0 for the remaining analyses. All estimates were significant at a level of 0.05.
Results
Mortality rate in patients with SMI
The number of deaths among patients with SMI was 1183 in 2012 and 1396 in 2013, with a crude mortality rate of 1.231% (per 1000 persons) and 1.355%, respectively. The average age at death was 60 years (s.d. = 16) in both years. The crude mortality rate for males was 1.364% (636 deaths) in 2012 and 1.534% (765 deaths) in 2013; for females, it was 1.106% (547 deaths) and 1.187% (631 deaths), respectively.
The SMR was 6.44 (95% CI 4.94–8.26) in 2012 and 7.57 (95% CI 5.98–9.44) in 2013 for those aged 15–34 years; 3.60 (95% CI 3.08–4.18) in 2012 and 3.70 (95% CI 3.19–4.27) in 2013 among those aged 35–44 years; and overall 1.35 (1.28–1.43) in 2012 and 1.50 (1.42–1.58) in 2013 for all patients aged ≥15 years, respectively (Table 1). The SMR decreased dramatically with age, to 0.82 (95% CI 0.72–0.93) in 2012 and 0.86 (0.76–0.97) in 2013 among patients aged ≥75 years. Male patients aged 35–74 years in 2012, or aged 15–74 years in 2013, had higher standardised mortality rates than female patients, thus leading to an overall higher SMR.
Table 1 Age–gender-specific standardised mortality ratio (SMR) in patients with severe mental illness from Sichuan of China, 2012–2013a
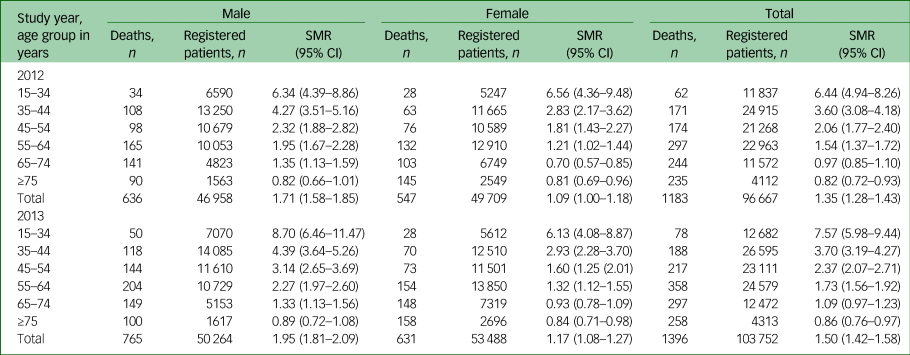
a. The SMR was calculated using mortality of general population in Sichuan Province from the sixth demographic census.
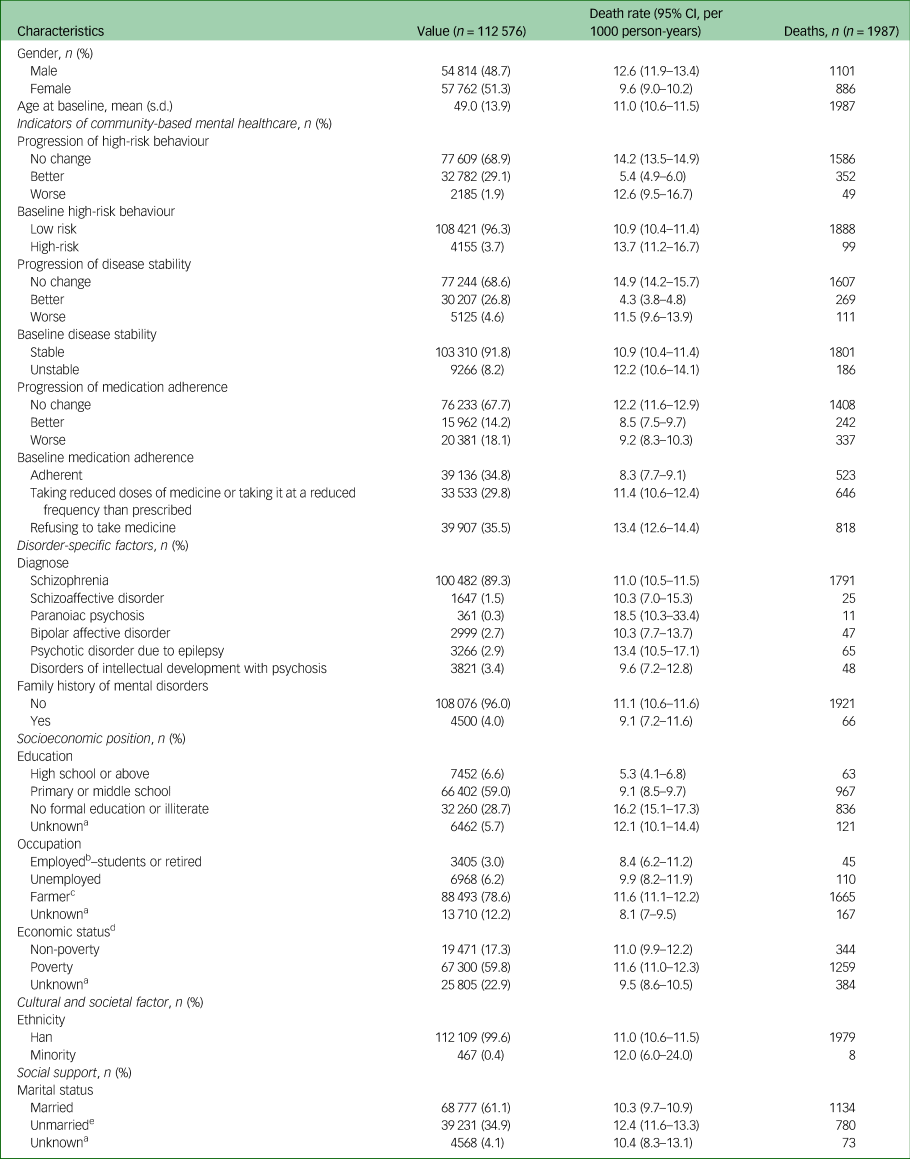
Characteristics of patients and counties in modelling analysis
Among the 112 576 patients with SMI used for model analysis (Fig. 1), 1987 (11.0 per 1000 person-years) died from 2009 to 2014. The median survival time was 20 months (interquartile (IQR) = 12–26 months). The mean baseline age for all participants was 49 years (s.d. = 14 years, Table 2). Nearly half of the participants (54 814, 48.7%) were male.
Table 2 Characteristics and death rate for patients with severe mental illness from Sichuan Province, China, 2009–2014 (n = 112 576)
a. Unknow was included in the model analysis.
b. Including professional/technical personnel, managerial personnel, industrial worker.
c. Including agriculture, forestry, animal husbandry, fishery.
d. Determined by whether they were above or below the poverty line as determined by the local government according to the local socioeconomic status.
e. Including widowed, separated, divorced and never married.
The proportions of ‘better’ for high-risk behaviour (29.1%) and disease stability (26.8%) were similar. However, for only 14.2% of patients was there an improvement in terms of medication adherence; patients’ medication adherence got worse in 18.1%; which was higher than rates of deterioration for high-risk behaviour (1.9%) and disease stability (4.6%) (Table 2). Participants with better progression for the measures of high-risk behaviour, disease stability and medication adherence showed the lowest death rates, however, those with worse progression did not have higher death rates compared with those where it was unchanged.
Those patients with an unfavourable baseline status on all three measures had higher death rates than those with a favourable status, as expected. Most patients (89%) were diagnosed with schizophrenia. The death rates were higher among males, patients with no family history of mental disorders, with lower education attainment, those working as farmers and unmarried compared with their counterparts.
Of the 146 counties, GDP per capita varied from ¥7265 to ¥78 914 (RMB, Chinese currency), the average travelling time to the nearest hospital varied from 13.8 min to 180.6 min, and the number of mental health-related hospitals from 0 to 1.01 per 100 000 population.
Association between death and risk factors
High-risk behaviour
In the full model, participants with better progression regarding high-risk behaviour showed a 54% (95% CI 47–60%) lower hazard of death than those unchanged (Table 3). People with worse progression on measures did not show a difference from the reference group. Favourable baseline status was associated with a 59% (95% CI 41–71%) lower hazard of death than the unfavourable status.
Table 3 Association between death and community-based management in hazard ratio (95% CI)
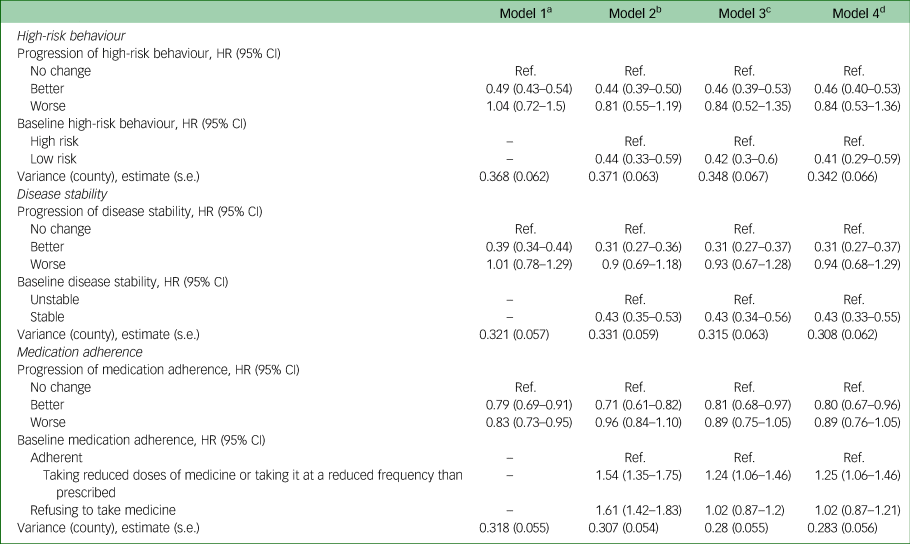
Ref., reference.
a. Without adjusting for covariates.
b. Adjusting for baseline community management indicator.
c. Adding other individual covariates, including age at baseline, gender, diagnose, family history of mental disorders, education attainment, occupation, economic status, ethnicity and marital status.
d. Adding county-level covariates, including gross domestic product per capita, average travelling time to the nearest hospital, and the number of mental health hospitals.
Disease stability
Participants who showed improvement in disease stability had a consistently lower hazard of death compared with those patients where it was unchanged, with a 69% (95% CI 63–73%) reduced hazard in the full model (Table 3). Patients with worse progression showed no difference from the reference. Stable baseline disease status was associated with a 57% (95% CI 45–67%) lower hazard of death than the unstable status.
Medication adherence
Participants with improvement in medication adherence showed a 20% (95% CI 4–33%) lower hazard of death compared with the unchanged group (Table 3). Those getting worse showed no difference from their counterparts. Compared with participants who were adherent at baseline, people taking a lower dose of their medication or taking it less frequently than prescribed had a 25% (95% CI 6–46%) higher hazard of death. Surprisingly, patients refusing to take medicine did not show a greater hazard of death in the fully adjusted model.
In the sensitivity analysis excluding those lost to follow-up, similar results can be found in Supplementary Table 1.
Other risk factors
Effects of other risk factors on risk of death were similar based on the three full models (Supplementary Table 2). Disadvantaged socioeconomic status, such as lower education level, unemployment and farmer, was associated with a 38–50% higher hazard of death. Less social support, i.e., unmarried, was associated with a 32% higher hazard compared with married status. None of the health systems and context factors had a significant impact on risk of death in all models.
Discussion
Main findings
Using a large provincial sample of community-dwelling participants with SMI in Sichuan, China, we found that the SMRs were 6.44 and 7.57 times higher than the general population in patients aged 15–34 years in 2012 and 2013, respectively, and the mortality gap diminished with age. Participants whose risk behaviour, disease stability and medication adherence improved over time had a 54%, 69% and 20% reduction in the hazard of death, respectively, even after controlling six components of the multilevel risk factor model for excess mortality in people with SMI.Reference Liu, Daumit, Dua, Aquila, Charlson and Cuijpers3 Favourable baseline status of all three community indicators was related to a reduced hazard of 25–59%. Disadvantaged socioeconomic status and less social support were associated with a 32–50% higher hazard of death.
Comparison with findings from other studies
Our findings echo numerous studies that have found that people with mental illness have higher mortality than the general population, including three studies conducted with Chinese participants.Reference Zhou5–Reference Ran, Chen, Conwell, Chan, Yip and Xiang7 Systematic reviews have reported two to three times mortality for SMI,Reference Chesney, Goodwin and Fazel1,Reference Walker, McGee and Druss23 and the mortality gap tended to diminish with increasing age,Reference Zhou5,Reference Zgueb, Jomli, Ouertani, Hechmi, Ouanes and Nacef24 consistent with our findings. Older adults experienced slightly higher SMRs from natural causes than people aged 20–39 years, while younger adults had remarkably higher SMRs from unnatural causes such as poisoning and suicide, especially among women.Reference Heiberg, Jacobsen, Nesvag, Bramness, Reichborn-Kjennerud and Naess25 The age diminution in China needs further investigation for the age-cause-specific causes of death.
The SMRs in our study (overall 1.35 and 1.5) suggest lower excess risks compared with the above findings (1.8–4.0),Reference Chesney, Goodwin and Fazel1,Reference Zhou5–Reference Ran, Chen, Conwell, Chan, Yip and Xiang7,Reference Chang, Hayes, Perera, Broadbent, Fernandes and Lee22 which could be explained by the following:
(a) In China, 22% patients with mental illness had ever sought professional care, only 12% had ever been admitted to a psychiatric hospital. The care-seeking rate for older adults was lower than younger people with a larger gap among those with severer disability.Reference Phillips, Zhang, Shi, Song, Ding and Pang26 Using data from the Sichuan NSBICAP, one study reported that fewer than 1.2% of patients who died had received any treatment before death.Reference Wen, Wang, Wang and Yang18 However, because the identification of patients included referral or direct identification from institutions, patients with severe symptoms and limitation of motion, especially older adults, might well be omitted and excluded from the system. The SMR for patients aged 15–64 was 2.26, similar to the NordicReference Wahlbeck, Westman, Nordentoft, Gissler and Laursen27 and TunisianReference Zgueb, Jomli, Ouertani, Hechmi, Ouanes and Nacef24 studies. The mortality rate for patients aged 65 and above may be underestimated because of the lower care-seeking rate discussed above.
(b) Evidence using in-patient data might overestimate mortality in people with mental disorders, as patients in hospitals are more likely to have serious conditions than patients who are community dwelling.Reference Crump, Ioannidis, Sundquist, Winkleby and Sundquist28
Our findings show a notable positive association between improvement in risk behaviour, disease stability or medication adherence and a decreased hazard of death. High-risk behaviour, including violence against others or self, often implies deterioration of symptoms and lack of insight into psychotic symptoms and thus worse adherence to treatment,Reference Arango, Calcedo Barba, Gonzalez and Calcedo Ordonez29 which would aggravate disease symptoms and increase risk of death. Stereotypes of individuals with mental illness being violent would deepen the stigma that permeates patients’ lives,Reference Webermann and Brand30 contributing to them neglecting routine health checks and refusing necessary healthcare.Reference Saxena31
Although it has a strong association with mortality, disease stability may not be an efficient measure in predicting mortality for this particular population because of its inability to distinguish mental and physical symptoms. Rigorously designed indicators tested for validity and reliability are necessary for further promotion and dissemination of mental healthcare. Numerous studies highlight the beneficial impact of medication adherence on health outcomes.Reference Sampson, Mansour, Maayan, Soares-Weiser and Adams32,Reference Garcia, Martinez-Cengotitabengoa, Lopez-Zurbano, Zorrilla, Lopez and Vieta33 Poor adherence to treatment is associated with worse symptoms of mental illness, increased risk of readmission, relapse and mortality.Reference Garcia, Martinez-Cengotitabengoa, Lopez-Zurbano, Zorrilla, Lopez and Vieta33 Using the same database, Tang and colleaguesReference Tang, Liu, Cao, Li, Wen and Wang34 reported an unchanged rate of medication adherence from 2006 to 2013, compared with risk behaviour and disease stability, which improved significantly over time. Although medication adherence may be overestimated in our study and in Tang and colleagues’ study because long-acting injectable antipsychotics were included (and the proportion was unknow), its relationship with death may not be biased. Thus, we recommend the government and health professionals to focus on process indicators in the performance assessment of mental healthcare.
As expected, lower socioeconomic status was associated with increased hazard of death resulting from disparities in health resources and health literacy.Reference Berkman, Sheridan, Donahue, Halpern and Crotty35 The literature has consistently identified that married individuals generally report better health and lower mortality compared with unmarried ones, partially benefiting from spousal emotional support.Reference Robards, Evandrou, Falkingham and Vlachantoni36 Social determinants of health, such as poverty and connectedness, most likely interact with disease characteristics, behavioural and lifestyle factors, and health services to determine the differential mortality found in people with mental disorders.Reference Walker, McGee and Druss23
Strengths and limitations
There are several strengths to our study. We are among the first to study the association between community management measures and mortality among patients with SMI under the administrative surveillance system in China. Community mental healthcare in China is responding to the international call to integrate clinical treatment with primary care, thus it is critical to assess the value of these key measures, which may prompt the development of community-based mental health services.
Second, we used a two-stage model including growth models and multilevel models, effectively linking the changes in patterns of the key indicators and the risk factors for mortality. The growth model can handle repeated measures with random missing data and irregular time intervals between measures (for example medication adherence was assessed at irregular times), ideal for our data. The multilevel model is designed to handle the hierarchical data to mitigate type I error for the estimation of predictors’ coefficients by extracting different levels’ variances.
Third, we followed the MIF model to estimate risk factors for mortality among patients with SMI, providing insight into identifying priorities of interventions under a systematic framework. Finally, we used the NSBICAP, the only mental health surveillance system in China, for comprehensive analyses for a whole province, which provides evidence for comparison with other areas with a different context.
We acknowledge several limitations, primarily the short length of follow-up because of the limited accessibility of administrative data and the lack of evaluation studies for the quality of the data-set.Reference Liang, Mays and Hwang12 We excluded data collected before 2009, and only calculated mortality for 2012 and 2013, as the early system might have resulted in lower quality data. A system review has demonstrated that studies with shorter follow-up tended to report higher mortality ratios.Reference Walker, McGee and Druss23 Further studies with longer follow-up durations should be developed to test our methods and findings.
As our study used large scale and routinely collected administrative data, the quality of data can always be debated. We conducted strict inclusion and exclusion criteria for data cleaning and analysed the logical rationality of time-related variables, and excluded those with missing records, those with logic errors, those under 15 years old at baseline, and those without follow-up records in the final analysis. This procedure might lead to a biased sample of patients with mental illness in Sichuan Province. However, it is less likely to affect the association between progress of community management measures and mortality of patients.
Furthermore, the mortality of older adults in this paper could be underestimated, although it was claimed that over 20% of the estimated patients with SMI were registered in the system by the end of 2013.Reference Wen, Wang, Wang and Yang18 As explained above, because recruitment relied largely on referral from institutions, and older adults were more unlikely to receive any professional services before death,Reference Phillips, Zhang, Shi, Song, Ding and Pang26 the representativeness of the data is debatable, and the mortality and SMR estimated in this study may not represent the actual mortality of community-based patients with SMI in Sichuan. However, this may not affect the results in the association analysis.
Another limitation is that the information about death in the NSBICAP was obtained through regular follow-up by community workers. Neither the dates nor the specific causes of death were collected by the system. In this study, we used the survey dates as a proxy of date of death when calculating survival time. The survival time for the deceased might be slightly overestimated because their actual date of deaths were supposed to be two weeks to six months (depend on their follow-up frequency) earlier than the last survey dates. As a consequence, the association between community measures and mortality may be slightly underestimated.
In addition, although the growth model has obvious advantages in dealing with irregular time points and creating a specific slope for each individual, we manually divided the patterns of change using a tertile method after trying different strategies (for example quartile, quintile, decile) per overall consideration of the fitness effects and the number of participants in each group. This approach is popular in social science but the results need more verification using different data. Finally, we have pooled all disorders together in the analysis, irrespective of their differences in terms of disease characteristics, treatment and thus their association with death.
Implications
In this large community-based mental health programme in China, we have evidenced the effectiveness of three key community measures in evaluating a community-based mental health outcome – survival – among patients with SMI. Over time the management strategy for these patients with targeting reducing high-risk behaviour, increasing stability of both mental and physical diseases, and increasing medicine adherence could lead to reduced mortality in patients. In place for over 10 years as the world-largest mental health services demonstration project,Reference Good and Good37 this programme has scant evidence evaluating its project design and the effectiveness of the indicators that are being monitored. Our findings are of great importance in filling this gap. As the integration of mental health into primary care is a major pragmatic method advocated by the World Health Organization, particularly for low- and middle-income countries with limited health resources, this study provides some innovative evidence on the rationality of a national community-management programme, and may facilitate sustained evidence-based mental healthcare programmes for other counties with limited health resources.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjo.2021.46.
Data availability
The publication of data is not permitted according to government regulations. All information that could be used to identify personal identities, including names, ID number and addresses has been concealed before we gained access to the data. However, anonymised data might be available upon request.
Acknowledgements
The publication is based on data collected by hundreds of mental health professionals in communities. We acknowledge and thank them for managing the information.
Author contributions
Y.L. conducted the literature review, analysed the data and drafted and revised the manuscript. L.L.Y., C.R., and J.X. contributed to the study design and the results interpretation, and reviewed the manuscript. H.W. and D.W. supervised the collection and the quality control of the data, and contributed to the results interpretation. M.Y. was the Grant principal investigator, designed the study, supervised data analysis, contributed to the results interpretation, and reviewed the manuscript. All authors read and approved the final version of the submission.
Funding
This work was supported by the China Medical Board (Grant number CMB 12-106). The funder had no role in study design, data collection, data analysis, data interpretation or writing of the report.
Declaration of interest
None.








eLetters
No eLetters have been published for this article.