First-episode psychosis (FEP) refers to individuals who are early in the course of a psychotic illness or treatment. Reference Breitborde, Srihari and Woods1 Such psychotic illnesses include schizophrenia, which is a leading cause of global disability-adjusted life-years. Reference He, Liu, Li, Guo, Gao and Bai2 Psychosis refers to the presence of ‘positive symptoms’ such as hallucinations and delusions, and ‘negative symptoms’ such as affective flattening, alogia, apathy, asociality and associated cognitive dysfunction. Reference Fulford, Niendam, Floyd, Carter, Mathalon and Vinogradov3 Negative symptom burden predicts prospective long-term functioning, Reference Austin, Mors, Secher, Hjorthøj, Albert and Bertelsen4 and there is often little improvement in negative symptoms over time. Reference Austin, Mors, Budtz-Jørgensen, Secher, Hjorthøj and Bertelsen5 Cognitive impairment is present in over 80% of those with a diagnosis of schizophrenia. Reference Saha, Chant, Welham and McGrath6 Unfortunately, mainstay current pharmacological and psychological treatment for psychosis show little improvement in negative symptoms and cognitive function. Reference Young and Geyer7
Psychosis and ethnicity
Ethnicity and migration independently predict incidence of psychotic disorders, with recent meta-analytic evidence revealing a relative risk for non-affective psychotic disorders among migrants of 2.13 (95% CI 1.99–2.27), and for affective psychotic disorders it is even higher (2.94, 95% CI 2.28–3.79), even when socioeconomic confounders have been taken into account. Reference Selten, Van Der Ven and Termorshuizen8 British South Asians have an apparent increased incidence of psychosis compared with the White British population in the UK; research examining ethnic inequalities in the incidence of schizophrenia in England found that South Asian groups have a relative risk of 2.27 (95% CI 1.63–3.16) compared with White British populations. Reference Halvorsrud, Nazroo, Otis, Brown Hajdukova and Bhui9 Concerningly, in the UK, some tentative evidence suggests an overrepresentation of ethnic minorities with more severe mental illness. Reference Rees, Stokes, Stansfield, Oliver, Kneale and Thomas10
Cultural background can influence idioms of distress, evaluation of symptoms, engagement with services and outcomes from interventions. Reference Desai and Chaturvedi11,Reference Bhikha, Farooq, Chaudhry and Husain12 Psychosocial interventions form part of the management plan for patients with FEP. 13 Considering psychosocial interventions for ethnic minorities, there is evidence of greater drop-out for ethnic minority groups compared with ethnic majority groups. Reference de Haan, Boon, de Jong and Vermeiren14 However, qualitative evidence has described how cognitive–behavioural therapy, for example, can be an acceptable treatment if culturally adapted by including culturally based patient health beliefs, attributions concerning psychosis, attention to help seeking pathways and technical adjustments. Reference Rathod, Kingdon, Phiri and Gobbi15 This has been demonstrated in a randomised controlled trial. Reference Rathod, Phiri, Harris, Underwood, Thagadur and Padmanabi16 Considering specifically the adaptation of psychosocial interventions for psychosis, there is evidence of increased efficacy of adapted interventions for patients with schizophrenia. Reference Degnan, Baker, Edge, Nottidge, Noke and Press17
Cognitive remediation
One such psychosocial intervention for FEP is cognitive remediation, a behavioural training-based intervention that aims to improve cognitive processes with the goal of durability and generalisation. Reference Bowie, Bell, Fiszdon, Johannesen, Lindenmayer and McGurk18 Cognitive remediation is delivered by a trained therapist and involves the practise of cognitive exercises, with particular attention to the development of cognitive strategies, and procedures to facilitate transfer of cognitive gains to everyday functioning. Reference Bowie, Bell, Fiszdon, Johannesen, Lindenmayer and McGurk18 It has been demonstrated to provide significant benefits in relation to functioning, cognition and those negative symptoms in schizophrenia, Reference Revell, Neill, Harte, Khan and Drake19 and has been found to be effective and acceptable for people diagnosed with schizophrenia, Reference Vita, Barlati, Ceraso, Deste, Nibbio and Wykes20 with durable effects. Reference van Duin, de Winter, Oud, Kroon, Veling and van Weeghel21 Computerised delivery of interventions among patients with schizophrenia have been found to be effective and well received, Reference Alvarez-Jimenez, Alcazar-Corcoles, Gonzalez-Blanch, Bendall, McGorry and Gleeson22 but still need to be delivered with a trained therapist. Reference Bowie, Bell, Fiszdon, Johannesen, Lindenmayer and McGurk18 One such example of computerised cognitive remediation is the computerised interactive remediation of cognition training for schizophrenia (CIRCuiTS) Reference Reeder and Wykes23 which focuses on metacognition. CIRCuiTS was delivered via internet or CD. Reference Reeder and Wykes23 CIRCuiTS is delivered by a therapist, supplemented by independent sessions and is highly acceptable by both patients and clinicians, and feasible for patients with schizophrenia. Reference Reeder, Huddy, Cella, Taylor, Greenwood and Landau24–Reference Drake, Day, Picucci, Warburton, Larkin and Husain26
Given that British South Asian groups have a greater incidence of psychotic illness, Reference Halvorsrud, Nazroo, Otis, Brown Hajdukova and Bhui9 while holding culturally distinct illness beliefs, often following alternative pathways to accessing care, and having specific cultural, religious and linguistic needs, Reference Bhikha, Farooq, Chaudhry, Naeem and Husain27 this group presents an opportunity to examine the benefit of culturally adapting cognitive remediation to improve outcomes for FEP. This is vitally important to address ethnic inequalities in pathways to care. This is demonstrated by the fact that South Asian patients, compared with White patients, have elevated rates of civil detention and repeated admissions. Reference Halvorsrud, Nazroo, Otis, Brown Hajdukova and Bhui9 Specific to early intervention services, there is evidence that British South Asians are more likely to present later to services, Reference Beattie, Ritchie, Cardno and Mahmood28 miss out-patient appointments Reference Agius, Talwar, Murphy and Zaman29 and are three times more likely to drop out of treatment. Reference Patel, Cardno and Isherwood30,Reference Ouellet-Plamondon, Rousseau, Nicole and Abdel-Baki31 Further, British South Asians, like other ethnic minority groups, are often underrepresented in clinical trials for most psychological interventions, Reference Hussain-Gambles, Atkin and Leese32 with some tentative evidence that outcomes of standard psychosocial interventions are poorer for ethnic minorities compared with their White peers, as they are underpinned by Western values and norms. Reference Degnan, Baker, Edge, Nottidge, Noke and Press17,Reference Bhugra, Leff, Mallett, Der, Corridan and Rudge33 Culturally adapted interventions have been shown to be more efficacious compared with usual treatment, Reference Degnan, Baker, Edge, Nottidge, Noke and Press17,Reference Shehadeh, Heim, Chowdhary, Maercker and Albanese34 and align with National Institute for Health and Care Excellence guidance for schizophrenia, which advocates for ensuring that clinicians and interventions address differing explanatory models, health beliefs and expectations that vary across cultures. 13
We aim to investigate how to culturally adapt computerised cognitive remediation, and then explore the feasibility of delivering culturally adapted cognitive remediation (caCR) to British South Asians with FEP, but many aspects of this need consideration in terms of feasibility before conducting a randomised controlled trial. Reference Hallingberg, Turley, Segrott, Wight, Craig and Moore35,Reference Skivington, Matthews, Simpson, Craig, Baird and Blazeby36 Previous research has explored culturally adapting cognitive–behavioural therapy for psychosis, Reference Rathod, Phiri, Harris, Underwood, Thagadur and Padmanabi16 but this is the first study to assess the feasibility of culturally adapted computerised cognitive remediation. We used two different samples to address this aim, sample 1 (S1) were involved in qualitative interviews to determine how to culturally adapt cognitive remediation, and sample 2 (S2) were involved in exploring the feasibility of the intervention. Assessing feasibility would include exploration of acceptability of the intervention for participants, and if participants are retained in the study.
Method
Study design and sample
We employed initial formative qualitative interviews to explore how best to culturally adapt computerised cognitive remediation, followed by a single-group, non-blinded, non-randomised feasibility study with culturally adapted cognitive remediation as the intervention. With respect to the qualitative interviews, we adopted an interpretative approach, Reference Ritchie, Spencer and O’Connor37 and our sample was generated via purposive sampling of people with FEP from three NHS early intervention services within Lancashire Care NHS Foundation Trust and Manchester Mental Health and Social Care NHS Trust, and non-statutory services in the North-West of England. Early intervention services are constituted by a multidisciplinary team whose objective is to provide support to individuals experiencing a first episode of psychosis. The teams are composed of professionals from a variety of disciplines, including nursing, social work, occupational therapy and psychology. The provision of treatments is consistent across teams where participants were recruited. A total of ten participants were involved in the qualitative interviews. For the feasibility study, our sample was generated via purposive sampling. Researchers contacted community psychiatric nurses (CPNs) and case managers, psychiatrists and clinical psychologists within the Lancashire and Manchester early intervention services, who then made referrals to the research team. A total of ten participants were referred to the research team, and all were eligible for the study and provided written informed consent. Thus, we describe the methods for our two interlinked studies, involving ten participants in each sample (S1 and S2).
Inclusion criteria
For both the qualitative and feasibility studies, inclusion criteria were age 16–35 years, of self-reported South Asian ethnicity, a DSM-IV diagnosis of non-affective psychosis confirmed with the Structured Clinical Interview for DSM IV (SCID-I/P IV) Reference First and Gibbon38 and capacity to consent. We focused on 16- to 35-year-olds as computer-based therapy such as CIRCuiTS is valued by younger patients. Reference Reeder, Pile, Crawford, Cella, Rose and Wykes25
Exclusion criteria
For both studies, exclusion criteria were a DSM-IV diagnosis of substance dependence or misuse, or organic brain disease.
Procedure
Formative qualitative interviews
NHS key workers and voluntary service staff were asked to refer participants that met the inclusion criteria. All participants referred were able to, and provided, informed consent for involvement in the study. Semi-structured interviews were employed, and demographic information was collected at this stage. The interviewer led participants through a 20-min interactive demonstration of the computerised cognitive remediation package CIRCuiTS. This was followed by an interview lasting on average 1.5 h, based around a topic guide, but responsive to issues raised by respondents. The topic guide was developed based on previous literature including author N.H.’s work on culturally adapting psychological interventions, and patient advisors. The guide was informed by the domains commonly explored when assessing acceptability of interventions. Reference Sekhon, Cartwright and Francis39 Areas explored by the topic guide included the participants’ concerns with cognition, the acceptability of computerised cognitive remediation and how it could be culturally adapted.
All interviews were recorded and transcribed verbatim. Data was analysed with thematic analysis. Reference Braun and Clarke40 Thematic analysis allows for identifying and describing themes (or patterns of meaning). Reference Braun and Clarke40 Themes were derived inductively; coding and analysis was guided by our study aims on how to adapt cognitive remediation. Coding was an iterative process, developed by moving back and forth through data familiarisation, searching for themes, reviewing themes, defining and naming themes. Reference Braun and Clarke40 These themes were used in conjunction with a framework for cultural adaptation of psychosocial interventions Reference Degnan, Baker, Edge, Nottidge, Noke and Press17 to implement changes to cognitive remediation.
Participants were encouraged to indicate their preferred language that the intervention be administered, and were able to choose the location for the intervention (this could be at home, or in a public space such as a library). Patients were able to select times that worked around their schedule. One participant exhibited high levels of disorganised and bizarre thought content throughout his interview. The participant’s transcript was independently assessed by two members of the research team (C.P. and R.D.) to identify sections that were too disorganised to be analysed. This process allowed for 63% of the interview to be included in the analysis, rather than removing the entire interview.
Feasibility study
Intervention: computerised cognitive remediation
The intervention was the computerised cognitive remediation programme CIRCuiTS, which is based on paper-and-pencil therapy and was developed with patients and therapists. Reference Reeder, Pile, Crawford, Cella, Rose and Wykes25,Reference Medalia and Revheim41,Reference Wykes, Joyce, Velikonja, Watson, Aarons and Birchwood42 Participants engaged with 40 h of increasingly complex neuropsychological tasks over 12 weeks, and this took place in person. Demographic information was collected. Tasks were delivered by a trained therapist, at the participant’s own pace, typically three to four 1-h sessions per week. CIRCuiTS focuses on developing skills by means of drill, practise and strategy, in common with many other forms of cognitive remediation. The tasks prompt participants to use specific methods (drill); tasks have repeated elements even as they become more complex, so that participants use skills and routines repeatedly (practise); but as tasks become more complex, participants are forced to devise methods by themselves (strategy). Reference Bowie, Bell, Fiszdon, Johannesen, Lindenmayer and McGurk18 In initial sessions task instructions and the therapist directs participants to use particular strategies, and with increasing task difficulty, the amount of direction decreases, and sessions lengthen as the participants attention and problem-solving skills improve. Correct responses are consistently met with praise from the programme and therapist.
Cultural adaptation
We adapted computerised cognitive remediation based on results from our qualitative interviews, and using an established framework. Reference Degnan, Baker, Edge, Nottidge, Noke and Press17 Our adaptations focused on language, therapeutic alliance, teaching style, manual content, family, treatment goals, delivery and engagement, and stigma. Adaptations are presented in detail in Table 1. Confidentiality was discussed with both the participant and their family.
Table 1 Details of the specific components of cognitive remediation and how it was adapted

CPN, community psychiatric nurse.
Outcome measures
We employed a variety of outcome measures to explore perceived efficacy, acceptability and impact on mental state and neurocognition.
Cognitive remediation satisfaction
The Cognitive Remediation Satisfaction Questionnaire Reference Rose, Wykes, Farrier, Doran, Sporle and Bogner43 was used to explore participants’ attitudes toward the content of caCR, the computerisation of tasks, rapport with their therapist, self-perceived cognitive effects and any perceived adverse effects. This was considered an assessment of acceptability as domains explored match onto the different component constructs: affective attitude, burden, ethicality, intervention coherence, opportunity costs, perceived effectiveness and self-efficacy. Reference Sekhon, Cartwright and Francis39
Secondary outcomes
Mental state
We measured mental state using the following instruments: Positive and Negative Syndrome Scale (PANSS), Reference Kay, Fiszbein and Opler44 Psychotic Symptom Rating Scale (PSYRATS), Reference Haddock, McCarron, Tarrier and Faragher45 Calgary Depression Scale for Schizophrenia (CDSS), Reference Addington, Addington and Maticka-Tyndale46 Clinical Global Impressions Scale (CGI) Reference Guy47 and Global Assessment of Functioning (GAF), including the Social and Occupational Functioning Assessment Scale (SOFAS). Reference Jones, Thornicroft, Coffey and Dunn48
Neurocognition
We measured difference aspects of cognition. Visual learning and memory was assessed via the Ray Osterteith task, immediate recall and long term. Reference Osterrieth49 Verbal learning was assessed via the Logical Memory Test. Reference Hodges, Salmon and Butters50 Speed of processing, an aspect of working memory was assessed via the Trail Making Test (A and B). Reference Reitan51 Attention and working memory was measured by the N-Back continuous test. Reference Kirchner52 Executive functioning and metacognition were assessed by the Meta-cognitive Wisconsin Card Sorting Test (MC-WCST). Reference Koren, Seidman, Harrison, Lyons, Kremem and Caplan53 Finally, reasoning and problem-solving was measured by the Wechsler Adult Intelligence Scale Test of Adult Reading (WAIS-R). Reference Wechsler54
Other
We also administered the following measures: Beck Cognitive Insight Scale (BCIS), Reference Beck, Baruch, Balter, Steer and Warman55 Birchwood Insight Scale (BIS), Reference Birchwood, Smith, Drury, Healy, Macmillan and Slade56 Rosenberg Self-Esteem Scale (RSES), Reference Rosenberg57 Brief Illness Perception Questionnaire (IPQ-Brief) Reference Lobban, Barrowclough and Jones58 and quality of life via the EuroQol visual analogue scales (EQ-VAS). Reference Kind59
Procedure
All assessment measures, including demographic information, were obtained at baseline apart from satisfaction. Demographic information for S1 included gender, age, ethnicity, country of birth, immigration generation, education level, current employment, household size and whether they were on medication, and was collected before interviews with the use of a self-completed form. For S2, we collected demographic information, including gender, ethnicity, immigration generation, education level, current employment, medication, age and household size. We included more categories of antipsychotics, and age and household size as continuous variables for S2 compared with S1.
There was an initial family engagement session before caCR sessions commenced. Families were invited to meet the therapist. Family members and participants were invited to discuss how cognitive deficits affected their daily activities. A short explanation of caCR was given, and questions answered. A key caregiver was identified for weekly contact throughout the intervention, and this involved a quick check to determine if they felt things were progressing as expected. Participants then undertook 40 h of caCR over 12 weeks. Upon completion, all assessments were repeated, with the exclusion of demographic details and the SCID-I/P IV, and inclusion of the Cognitive Remediation Satisfaction Questionnaire. We primarily determined the feasibility, not efficacy of cognitive remediation. The Cognitive Remediation Satisfaction Questionnaire was completed without contact from the therapist. Questionnaires were left on the last session to be filled in by the participants (with help from family or their CPN where necessary), sealed and then posted back or collected by the research team. All other assessments were carried out by the therapist at baseline and post intervention.
Analysis
Data was analysed, and continuous pre- and post-intervention data was compared with Wilcoxon signed-rank tests.
Ethics
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human patients were approved by the Bolton Research Ethics Committee (qualitative study: reference 09/H1012/2; feasibility study: reference 08/H1009/76).
Results
Formative interviews
The participants chose to conduct the interviews in English and in their own homes. Code saturation was achieved after seven interviews, but recruitment continued to total ten participants from the NHS early intervention service. No participants from voluntary services met the SCID-I/P IV criteria. Participant demographics for S1 are presented in Table 2. All participants had experienced their first episode of psychosis within the past 18 months (reflecting the nature of early intervention service programming); eight without relapse and two relapsing once. The mean age was 23.3 years (range 16–30 years); five lived with their parent/s and siblings, three with their spouse and young children, one in council supported accommodation and one in an Islamic residential home. All stated they were Muslim and grew up within an Islamic household.
Table 2 Sample characteristics for the qualitative study (S1)

The analysis of the data revealed themes relating to the importance and need for interventions to address cognitive impairment, and then how best to culturally adapt cognitive remediation, in particular, (a) how to adapt the content of the tasks, (b) how best to deliver cognitive remediation and (c) how to make it more engaging. Quotations from interviews relating to the below themes are presented in Table 3.
Table 3 Quotations from qualitative interviews

Perspectives of cognitive remediation
All respondents expressed their frustration with the effect of cognitive impairments on their social functioning, meaningful daily activities and self-confidence. All wanted to improve their cognitive skills. Computerised cognitive remediation was well received by all participants: ‘interactive’, ‘colourful’ and ‘fun’. Respondents were able to offer advice about the delivery and content of cognitive remediation.
Content of cognitive remediation tasks
Participants suggested making the content of the tasks more culturally familiar (i.e. include capital cities from Muslim countries, Asian names, ingredients for recipes) and religiously sensitive (i.e. remove all non-Halal foods from shopping or cooking tasks).
Delivery
Most respondents preferred cognitive remediation sessions to take place in their own home, saving them time and avoiding costs for travel and childcare. Those unsure were concerned they would be distracted by younger family members during sessions. Field notes highlight the presence of family members during all interviews, often young children needing attention from the participant, or older family members who spoke little English but expressed an interest in the nature of the intervention. All participants suggested a high frequency of sessions was preferable, between twice and five times a week.
The majority of participants had their own home computer and regularly accessed the internet, but some had limited or no access and wished to improve their computer skills. All participants preferred computerised cognitive remediation to the idea of using pen and paper, but many asked for clearer instructions to the programme and a preliminary session to familiarise themselves with the computer.
All considered the support of a therapist essential during sessions. All but one preferred working one to one with the therapist rather than in a group. This individual was attracted by the social aspects of a group. Emphasis was placed on the competence and amiability of the therapist, whereas ethnicity or specific qualifications were dismissed as unimportant. Two individuals (one female, one male) preferred the therapist to be gender matched.
All participants preferred the cognitive remediation programme to be in English, but recommended that a translated version should be available. Only one bilingual participant encountered linguistic problems on one task. This required participants to respond quickly to an image on the screen by pressing the letter it began with on the keyboard. He explained that the additional cognitive process of translating what he had seen appeared to increase his reaction times.
Engagement
Participants highlighted the importance of being receptive to participants’ holding multiple or distinct illness beliefs, openness to help-seeking from multiple sources, and awareness of problems concerning confidentiality and community stigma. Respondents highlighted the importance of family: not only providing families with clear information, but recognising their willingness to help their family member. There was also a clear requirement for therapists to exhibit cultural competence and recognise the individuals’ and their families’ level of acculturation and language needs.
Feasibility study
Sample and retention
Sample characteristics for S2 are presented in Table 4 for our feasibility study. The mean age was 24, the sample was evenly divided by gender and most identified as Pakistani. A majority of the sample were second generation immigrants, and only one participant was not on antipsychotic medication. Two participants withdrew; both were full-time students. One withdrew immediately after baseline assessments: they felt they did not suffer from cognitive deficits, so caCR would not be of any benefit. The other completed four sessions of caCR, but being in their final year of university, said they did not have time to continue with sessions.
Table 4 Sample characteristics for feasibility study (S2)

Acceptability (the Cognitive Remediation Satisfaction Questionnaire)
Sessions
Overall, our participants reported that the tasks were fun and challenging. Seven (87.5%) enjoyed the attention they got during therapy, six (75%) said sessions kept their mind occupied, and seven that there were the right number of sessions per week. With one exception, all participants completed 40 h of caCR. The participant who did not complete the caCR had fluctuating, severe symptoms that made engagement intermittent and therefore prolonged the intervention. For this individual, only 20 h of caCR was completed over 6 months. Scheduling of sessions was flexible, as several participants attended college full time or had young children. The majority preferred two 1.5–2 h sessions per week. All sessions took place at the participant’s family home, with the exception of one participant, who asked for sessions to move to the local library during school holidays, to allow them to concentrate away from younger siblings. To improve participant and family engagement, the therapist tried to avoid seeming hurried and always left time at the beginning and end of sessions for informal conversation with families and participants. The majority (87.5%) were disappointed when sessions ended. Reasons given included that they would miss their therapist, found caCR beneficial and worthwhile, and enjoyed the challenge and the progressively increasing difficulty. One respondent indicated relief when sessions ended because caCR had gone on too long, but added that they would miss contact with the therapist. Further, 50% of our sample said they had improved their computer skills during sessions.
Tasks
Our sample was divided into those who did (n = 4) and did not (n = 3) find the tasks difficult, and there was no consensus on which task was the most difficult. The majority who found it difficult conveyed they enjoyed the challenge. Among our sample, seven of the eight participants felt they had improved as the therapy proceeded, and all reported this had made them feel better. For those who did not improve, one participant found it frustrating. Each participant named a different task as their favourite, and all but one said they understood the use of strategies for each task. Four participants stated they had used the tasks and strategies outside the therapy sessions. This included using lists and memory strategies in the supermarket, working out travel times for transport, planning and to-do lists, and reasoning strategies to make decisions. Three participants had never used strategies outside of caCR sessions.
Family
For seven of the families, the therapist engaged with at least one family member throughout the intervention. All participants stated family members understood why the therapist visited, and all but one said that their family was happy they were participating. The exception, whose family had limited engagement during the intervention, said he was uncertain. For three families, despite many efforts, the therapist was only able to make contact with the primary caregiver on the preliminary engagement session.
Therapeutic alliance
All participants assessed the therapist positively and identified qualities such as being a good teacher, being non-judgemental, easy to talk to and encouraging. Several participants reported the most helpful attribute of cognitive remediation sessions was having someone to talk to. The therapist and the participants were not ethnically matched. Religion (specifically Islam), spirituality and British South Asian cultural norms were frequently discussed. Families often sought some disclosure of the therapist’s own cultural background. The therapist encouraged the family to advise them on cultural norms, and spent a considerable amount of time exploring the families’ treatment expectations and goals.
General benefits and costs of caCR
Although four (50%) reported caCR had made them more aware of their limitations, none found this frustrating. Seven (87.5 %) said caCR made them feel better about themselves, boosted their confidence, improved their mood and increased their general knowledge; that they enjoyed using strategies to complete the harder levels and that it gave them an understanding of metacognition. Helpful outcomes included improvements in memory, having someone to talk to, occupying spare time, improving mood and the real-life application of strategies. The only negative outcome was the frustration when getting tasks wrong and exposing their cognitive limitations.
Specific aspects of cognition
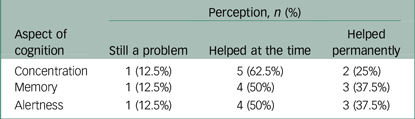
Self-perceived changes in concentration, memory and alertness are displayed in Table 5. Among our sample only one out of the eight (12.5%) participants felt that concentration, memory and alertness remained a problem after the intervention. Two out of eight (25%) participants reported permanent improvement in concentration, three out of eight reported permanent improvement in memory and three out of eight reported permanent improvement in alertness, and the rest reported that the intervention helped at the time.
Table 5 Self-perceived changes in concentration, memory and alertness
Secondary measures
Mental state
Even with this small sample, there were significant improvements (uncorrected for multiple testing) in PANSS and PYSRATS totals and GAF and SOFAS scores (Table 6). No significant difference in baseline compared with post caCR were identified for health-related quality of life (EQ-VAS), beliefs about illness (IPQ-Brief), cognitive insight (BCIS), insight (BIS), depression (CDSS) and self-esteem (RSES).
Table 6 Secondary outcomes before and after culturally adapted cognitive remediation

caCR, culturally adapted cognitive remediation; PANSS, Positive and Negative Syndrome Scale; PSYRATS, Psychotic Symptom Rating Scale; CDSS, Calgary Depression Scale for Schizophrenia; CGI, Clinical Global Impressions Scale; GAF, Global Assessment of Functioning; SOFAS, Social and Occupational Functioning Assessment Scale; BCIS, Beck Cognitive Insight Scale; BIS, Birchwood Insight Scale; RSES, Rosenberg Self-Esteem Scale; IPQ-Brief, Brief Illness Perception Questionnaire; EQ-VAS, EuroQol visual analogue scales; MC-WCST, Meta-cognitive Wisconsin Card Sorting Test; WAIS-R, Wechsler Adult Intelligence Scale Test of Adult Reading.
*P < 0.05; **P < 0.01.
Neurocognition
Global cognitive change had an effect size (Cohen’s d) of 0.40. Learning and memory showed evidence of appreciable improvement (effect sizes of 0.46 and 1.77) for visual immediate and long-term recall (Rey Osterieth task), verbal immediate and long-term recall (Logical Memory Task, effect sizes of 0.83 and 0.63, respectively), and reasoning (WAIS-R) (effect size 0.52). Improvements in speed of processing (Trail Making Test A, 0.20; Trail Making Test B, 0.33) was close to expected practice effects. Working memory and metacognition’s effect sizes were 0.
Discussion
Cultural adaptation
Computerised cognitive remediation was well received by all respondents, who recommended modifications to the content and mode of delivery. We used these findings from our thematic analysis in conjunction with another model for culturally adapting interventions. Reference Degnan, Baker, Edge, Nottidge, Noke and Press17 Our adaptations focused on language, family, communication, content, cultural norms and practises, context and delivery, therapeutic alliance and treatment goals. As mentioned, all of the sample stated they were Muslim, and this therefore influenced the adaptions made to the cognitive remediation, such as incorporating Halal foods. We did not focus on adapting cognitive remediation with respect to concepts and illness models, as this did not arise as an issue during our qualitative interviews. Participants’ recommendations largely fit within Bernal and Sáez-Santiago’s existing theoretical framework for culturally adapting psychological interventions for ethnic minorities. Reference Bernal and Sáez-Santiago60 The model recommends modifying language, culturally matching client, and therapist, using culturally familiar content and establishing common treatment goals between the patient and provider. The framework was based on research exploring the needs of Latin Americans. Notable differences between the model and this study’s results were clients’ preference for conversing in the English language and an apparent indifference to the therapist’s ethnicity. These differences are important for practise, implementation and scale-up.
Other results are consistent with adaptations made in previously published randomised controlled trials of adapted interventions for psychosis. These include incorporating cultural and religious content; Reference Mann and Chong61,Reference Patterson, Bucardo, McKibbin, Mausbach, Moore and Barrio62 acknowledging distinct illness beliefs; Reference Razali and Yahya63,Reference Shin and Lukens64 recognising the importance of family, specifically a distinct family structure or hierarchy; Reference Chien, Chan and Thompson65–Reference Kulhara, Chakrabarti, Avasthi, Sharma and Sharma67 recognising patient and family expectations and treatment goals; Reference Chien, Chan and Thompson65,Reference Kulhara, Chakrabarti, Avasthi, Sharma and Sharma67 the importance of confidentiality, given patients’ perception of stigmatisation by their community and families; Reference Chien, Chan and Thompson65 and optimising delivery, i.e. flexibility to financial, domestic or religious needs. Reference Kulhara, Chakrabarti, Avasthi, Sharma and Sharma67,Reference Bradley, Couchman, Psych, Perlesz, Nguyen, Singh and Riess68
Feasibility outcomes
Results from the satisfaction questionnaire showed that caCR was highly acceptable as an intervention to this sample of British South Asian with FEP. Levels of engagement and satisfaction were high. Enthusiasm and engagement were determined by family engagement, the challenge of the tasks and therapist contact. We identified that the family was central to optimising delivery and engagement. Other studies have identified the importance of family engagement for success of psychosocial interventions. Reference Khan, Lovell, Lunat, Masood, Shah and Tomenson69 Participants for which contact with families was limited were most likely to drop out, cancel sessions or report they had improved the least. Family members, particularly young children or siblings, were frequently at home throughout caCR appointments and would often want to sit in on sessions. During the preliminary family engagement session, family members frequently identified cognitive deficits and discussed how this affected the whole family. They were keen to have an active role: setting aside a quiet room during sessions, motivating participants to complete homework and discussing the goals of the intervention. Previous studies focusing on British South Asians have stressed the importance of a good relationship between the therapist/facilitator and the patient’s family. Reference Gater, Waheed, Husain, Tomenson, Aseem and Creed70,Reference Chaudhry, Waheed, Husain, Bhatti and Creed71 Future studies could explore this further to determine the critical ingredients in relation to family involvement.
It has been evidenced that issues with transport and childcare can be a deterrent for engaging with psychosocial interventions, Reference Gater, Waheed, Husain, Tomenson, Aseem and Creed70,Reference Crockett, Zlotnick, Davis, Payne and Washington72 therefore it is likely that the flexibility of the therapist to adjust to participants’ schedules, and being able to visit them at home, kept participants engaged. Participants enjoyed having someone to talk to, and to keep them motivated throughout sessions. All of the participants were young; many were still or had just recently stopped studying. All commented positively on how CIRCuiTS sessions reminded them of studying.
With respect to retention, two of the initial ten participants dropped out. However, baseline cognitive data and verbal feedback suggests neither participant dropped out because of severe cognitive impairment or dissatisfaction with the intervention; however, both were busy students, and this may reflect that this intervention is more of a challenge to engage with if the participant has a busy schedule. Given that patients with psychosis are often hard to engage, the attrition rate of this intervention is low, with 80% of our sample completing 12 weeks of cognitive remediation and high levels of engagement.
Strengths and limitations
One strength of this study is that we ensured purposive sampling was from three areas that support large ethnic minority communities, similar to many urban areas in the UK. Barriers to recruitment were minimised by asking language preference, choice of location and time of interview, exhibiting cultural competence and reimbursement of all costs. Our intervention was delivered in English and we recognise that not translating the intervention is a limitation. A future trial would be designed to consider preferred language and translate the intervention, similar to the approach used in ROSHNI-D study. Reference Husain, Lunat, Lovell, Sharma, Zaidi and Bokhari73 The sample varied in gender, age, source of income, previous convictions, level of education, immigrant generation, family structure, acculturation and religious beliefs. This increased our confidence that the saturation of key themes was valid in the qualitative interviews.
However, although our study offers a novel insight into how to culturally adapt cognitive remediation and the feasibility of such an intervention, there are important limitations to this study. Our study has a small sample size and as such results should be interpreted with caution. Our sample was entirely Muslim, mostly Pakistani and born in the UK, and therefore not reflective of all British South Asians. The analyses of our feasibility study were exploratory, with significance uncorrected for multiple testing. Without a control group, assessments were not blind, and we are unable to determine if improvements in mental state and cognition are better than usual cognitive remediation/routine care. Further feasibility data, including deriving eligible numbers to power a randomised controlled trial and assessment of willingness to be randomised, is needed to fully satisfy that this intervention can be employed in a trial and allow for the development of a protocol. Future feasibility work should also focus on determining if caCR is more or less effective depending on psychosis symptoms and severity.
In conclusion, this study is the first study that provides novel evidence on how to culturally adapt cognitive remediation for Muslim British South Asians with FEP in the UK. We have demonstrated this caCR is highly acceptable, with high levels of satisfaction and engagement and good retention. This study indicates that computerised cognitive remediation can be successfully culturally adapted for British South Asians with FEP, and such an intervention is acceptable. Further feasibility evaluation is needed, such as assessing agreeability for randomisation and estimation of effect sizes for future randomised controlled trials.
Data availability
The data that support the findings of this study are available from the corresponding author, J.B., upon reasonable request.
Author contributions
C.P. was involved in formulating the research question, designing the study, carrying it out and analysis. J.B. was involved with analysis and writing the article. L.R. was involved with analysis and writing the article. M.N., R.D. and N.H. were involved with formulating the research question, designing the study and carrying it out.
Funding
This report presents independent research commissioned by the National Institute for Health and Care Research (NIHR) under The HeLPER Programme Grant awarded to Nusrat Husain (RP PG-0606-1302), and was part of a larger doctoral thesis, which can be accessed online. Reference Press74 The views expressed in this paper are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Declaration of interest
None.










eLetters
No eLetters have been published for this article.