Around 5–7% of children and 2–4% of adults have attention-deficit hyperactivity disorder (ADHD).Reference Faraone and Biederman1–Reference Salari, Ghasemi, Abdoli, Rahmani, Shiri and Hashemian3 Individuals with ADHD commonly experience co-occurring difficulties, including mental illness and occupational or social challenges.Reference Anker, Bendiksen and Heir4–6 High co-occurrence also exists with other neurodevelopmental differences.5,Reference Gillberg7 Supports throughout the lifespan can mitigate challenges.8 Although non-pharmacological and environmental stratagies are the primary source of support for both children and adults,8 medication should be considered for those with persistent needs in at least one domain.8 However, there is ongoing discussion concerning appropriate use of ADHD medications.Reference Asherson, Leaver, Adamou, Arif, Askey and Butler9,Reference Connelly10 On the one hand, robust empirical evidence suggests pharmacological interventions offer effective symptom management, enabling individuals with ADHD to improve functioning.8 Medication initiations have also been shown to be associated with significant lower all-cause mortality, particularly for deaths from unnatural causes.Reference Li, Zhu, Zhang, Kuja-Halkola, D'Onofrio and Brikell11 On the other hand, critics are concerned about overmedicalisation and commercialisation of typical human traitsReference David and Deeley12 and escalating rates of prescriptions, particularly among adults, and whether such trends reflect genuine increases or diagnostic inflation.Reference Gascon, Gamache, St-Laurent and Stipanicic13 There is some apprehension that non-pharmacological supports, environmental modifications and broader holistic approaches are receiving inadequate attention.Reference Weissenberger, Ptacek, Klicperova-Baker, Erman, Schonova and Goetz14 Review of empirical data on real-world medication practice provides an objective analysis of this topic.
A key direction for medication research is to move beyond the relatively small populations typically available within clinical trials or studies based on diagnosed cohorts, and focus instead on regional or national prescription volume by using large data-sets.Reference Bennie, Malcolm, McTaggart and Mueller15 Historically, most research has also focussed on children,Reference Asherson, Leaver, Adamou, Arif, Askey and Butler9 leaving knowledge gaps in understanding patterns in adults. Variations in access to ADHD medication represent a health inequalities and public health issue. Although it is the case that a variety of personal and contextual factors influence use of ADHD medication, including personal knowledge about ADHD, patient and professional opinion about medication, and ADHD-related stigma,Reference Boudreau and Mah16 another potential concern is that unequal medication prevalence may reflect disparities in healthcare access.Reference Young, Asherson, Lloyd, Absoud, Arif and Colley17 For instance, regions with specialised mental health services may exhibit higher prescription rates, whereas those with limited services might experience lower rates, leading to inadequate or no treatment.Reference Asherson, Leaver, Adamou, Arif, Askey and Butler18 As noted, untreated ADHD can lead to adverse health outcomes and mental health challenges.Reference Anker, Bendiksen and Heir4–6 This presents a key public health concern, given the relatively high prevalence.Reference Faraone and Biederman1–Reference Salari, Ghasemi, Abdoli, Rahmani, Shiri and Hashemian3
Study background
This research was completed in Scotland, which has a publicly funded healthcare system, managed by local Health Boards, who oversee general practice, hospitals, community services, therapies, diagnostics and allied health services. General practitioners serve as gatekeepers to mental health, psychiatry specialists and community paediatrics. Long-term ADHD management can occur in primary care under ‘shared care’ arrangements, but practice variations exist in prescribing and mental health/ADHD services. Recruitment challenges persist, particularly for psychiatrists and mental health nurses and in community paediatrics. ADHD assessments should follow the National Institute for Health and Care Excellence ADHD guidelines,8 Scottish Intercollegiate Guidelines Network ‘Management of attention deficit and hyperkinetic disorders in children and young people’,19 and the recent update on ADHD by the Royal College of Psychiatrists (Scotland).20 Recommendations include considering differential diagnoses, conducting full assessments before diagnosis, psychosocial strategies as first-line supports for children and young people, giving environmental modification advice before prescribing for adults, and establishing local practice protocols between mental health teams and general practitioners. Prescription decisions should consider various factors, with agreements on processes and responsibilities for addressing concerns. Medications typically used to treat ADHD in Scotland include methylphenidate preparations, dexamfetamine preparations, atomoxetine, guanfacine and modafinil.
The analyses of medication use in Scotland presented here are part of a comprehensive programme aiming to act as a catalyst for developing improved services. The Scottish Government partnered with the authors of the current work, the National Autism Implementation Team (NAIT) and the Royal College of Psychiatrists in 2020 to establish comprehensive pathways for adult ADHD care as part of a national effort to enhance neurodevelopmental assessment, diagnosis and supports across the lifespan.21–Reference Rutherford, Johnston and Carotenuto25 The NAIT team is composed of neurodivergent and neurotypical individuals, as well as professionals from various domains, including psychiatry, education, speech and language therapy, and occupational therapy. The team collaborates with academics and patients to champion evidence-informed practices and neuro-affirming work, with a focus on multi-professional and cross-sector work, environmental modifications and partnership with neurodivergent individuals.21–Reference Rutherford, Johnston and Carotenuto25
Method
Aims
This study aimed to analyse prescribing patterns for medication typically used to treat ADHD in Scotland for adolescents and adults. Although recent analysis from Public Health Scotland26 offered initial insights into decreasing prescription rates after 15 years of age and significant regional variation in medication usage in Scotland, our study aims to further explore and substantiate these findings by using a comprehensive population data-set.
Data-set
The study used information from the Prescribing Information System (PIS).26 The PIS includes all National Health Service (NHS) prescribing relating to all medicines, and their costs, that are prescribed and dispensed in the community in Scotland. General practitioners provide most prescriptions, with other authorised prescribers such as nurses also contributing. Prescriptions written in hospitals that are dispensed in the community are also included. Prescriptions dispensed within hospital settings or hospital-based clinics are not included. Private prescriptions and direct supplies are also not included. Data include a unique identifier, the Community Health Index (CHI) number, prescriber and dispenser details for community prescribing, costs and drug information. Data on practices (e.g. NHS Boards), and prescribable items (e.g. manufacturer, formulation code, strength) are also included. NHS Scotland uses extensive computerised record keeping, with around 100 million data items loaded into the PIS per annum.26 The PIS data are refreshed monthly, and therefore provide a very robust indication of routine prescribing practice in the community.
Data processes and analysis
An extract from the PIS was made in 2021 for 2019 and 2010 data. Both extracts identified people prescribed medication from British National Formulary Section 4.4 ‘CNS stimulants and drugs used for ADHD’ (including methylphenidate preparations (immediate release and sustained release), dexamfetamine preparations (immediate release and sustained release), atomoxetine and guanfacine), but excluding modafinil because of its non-ADHD indications. The extracts included items prescribed in Scotland, with all available prescriber types included. Information is for items that have been prescribed and subsequently dispensed. The extracts reported data by unique patient identified (UPI) (the number of cases prescribed medication typically used to treat ADHD), defined daily dose (DDD) (assumed average maintenance dose per day used on its main indication in adults) and gross ingredient cost (GIC) (a measure to show the cost of items). Changes in DDD, GIC and UPI from 2010 to 2019 were analysed.
The 2019 extract additionally included age and NHS Scotland Health Board locality. Age was calculated on 30 September 2019 and all data by age is a unique count, based on a unique identifier (CHI). The following age categories were chosen: children and young people aged 10–19 years and adults aged 20–59 years. These age categories allowed comparison between paediatric and adult services. Data for people over 60 years of age were excluded because of the limited numbers recorded. The number of cases prescribed medication typically used to treat ADHD (UPIs) was compared with the National Records of Scotland mid-year population estimate by age group for NHS Board.27 The ratio of number of cases and corresponding mid-year population estimate was calculated (cases per population – treated prevalence). We set the expected prevalence of ADHD in adolescents as between 5 and 7%, and the expected prevalence of ADHD in adults as between 2 and 4%.Reference Faraone and Biederman1–Reference Salari, Ghasemi, Abdoli, Rahmani, Shiri and Hashemian3 The number of cases identified was then compared to expected prevalence and the treated proportion of expected prevalence calculated for age groups 10–19 years and 20–59 years.
Ethics
This analysis is based on an anonymised, aggregated data-set containing routinely collected data, and therefore no ethical approvals have been sought.
Results
Changes in prescribing between 2010 and 2019
An analysis of UPI, DDD and GIC (Table 1) showed prescribing patterns of medication for people with ADHD between 2010 and 2019 at NHS Board (geographical) level. Overall, there was a large increase in the volume of people receiving medication for ADHD between 2010 and 2019. For Scotland as a whole, this increase was +233.2% for the number of people dispensed a prescription (UPI), +234.9% for the DDD and +216.6% for changes in expenditure on these medicines (GIC).
Table 1 Increases in people prescribed medication, by NHS Board (2010–2019), for individuals aged ≥10 years
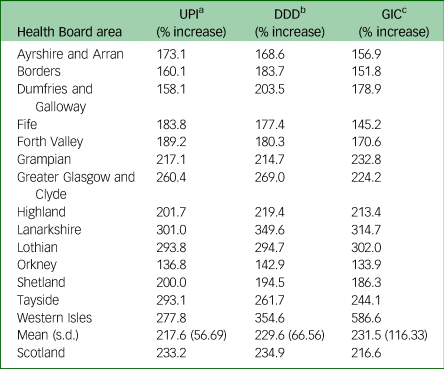
UPI, unique patient identified; DDD, defined daily dose; GIC, gross ingredient cost.
a. UPI represents the number of cases prescribed medication typically used to treat attention-deficit hyperactivity disorder.
b. DDD is the assumed average maintenance dose per day used on its main indication.
c. GIC is a measure to show the cost of items reimbursed before deduction of any dispenser discount.
A marked variation in increase between NHS Board level was also observed from these data, for each of the parameters. Between Scotland's 14 Health Board areas, increases ranged from +136.8% to +301% for UPI (mean increase +217.6%, s.d. 56.69). Increases across Health Boards for DDD ranged from +142.9% to +354.6% (mean increase +229.6%, s.d. 66.56). The increase for GIC across health boards ranged from +133.9% to +586.6% (mean increase +231.5%, s.d. 116.33).
ADHD prescribing in 2019
The 2019 extract was 15 516 people aged 10–59 years. The CHI capture rates were 94.27%. In the extract, 92.5% had a valid CHI, and 7.5% had missing data and so were excluded from the analysis, leaving a usable sample of 12 804 (10–19 years, n = 7806; 20–59 years, n = 4998).
Adolescent
Using 2019 mid-year population estimates for Scotland27 1.35% (95% CI 1.33–1.39) of the entire adolescent (10–19 years) Scottish population were receiving medication typically used to treat ADHD on the NHS (Table 2). There was variance geographically across Scotland: between 0.26 and 2.92% (Table 2) of local adolescent populations were receiving medication typically used to treat ADHD in 2019. Variance in the treated proportion of expected prevalence was between 3.62 and 58.36% of adolescents with likely ADHD at the 5% level (Table 2), and between 2.59 and 41.69% at the 7% level (Table 2). For Scotland as a whole, at the 5% level, 27.07% of children with likely ADHD were receiving medication typically used to treat ADHD, and at the 7% level, 19.34% of likely ADHD cases were receiving medication typically used to treat ADHD.
Table 2 Cases (age 10–19 years, n = 7806) per population (treated prevalence) and comparison of expected prevalence with the number of treated cases, by NHS Board (2019)
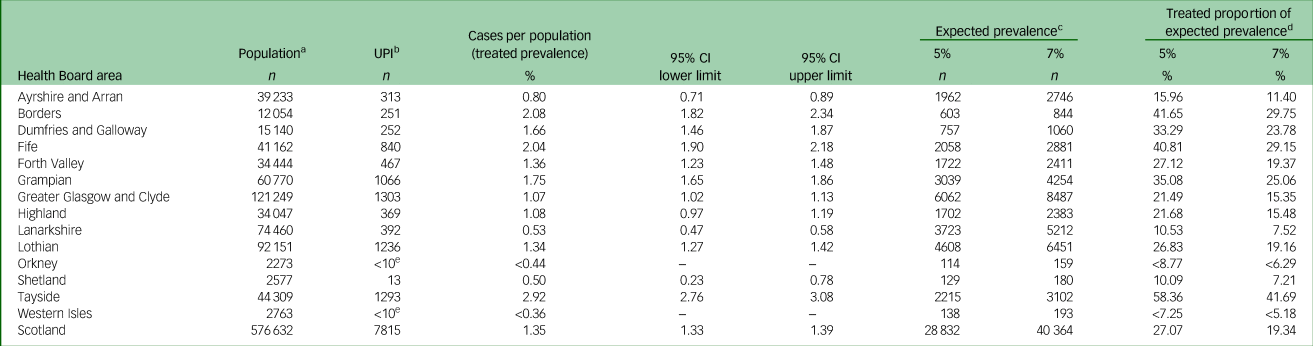
UPI, unique patient identified; ADHD, attention-deficit hyperactivity disorder.
a. National Records of Scotland mid-year population estimate by age group, for NHS Board, 2019.
b. UPI: the numbers of cases prescribed medication typically used to treat ADHD.
c. Expected prevalence of ADHD, as applied to the population.
d. Expected prevalence compared with the number of people identified as being treated for ADHD (UPI).
e. Records of fewer than ten cases have been hidden to manage disclosure risk.
Adult
The same approach was applied to the adult cohort (20–59 years) (Table 3). Using 2019 mid-year population estimates,27 0.17% (95% CI 0.17–0.18) of the entire Scottish adult population were receiving medication typically used to treat ADHD on the NHS in 2019. There was variance geographically. Across different areas of Scotland, between 0 and 0.28% (Table 3) of the local adult population were receiving medication typically used to treat ADHD in 2019. Variance in the treated proportion of expected prevalence was between 0 and 14.19% of adults with likely ADHD at the 2% level (Table 2), and between 0 and 7.10% at the 5% level (Table 2). For Scotland as a whole, at the 2% level, 8.54% of adults with likely ADHD were receiving medication typically used to treat ADHD, and at the 4% level, 4.27% of likely ADHD cases were receiving medication typically used to treat ADHD.
Table 3 Cases (age 20–59 years, n = 4998) per population (treated prevalence) and comparison of expected prevalence with the number of treated cases, by NHS Board (2019)
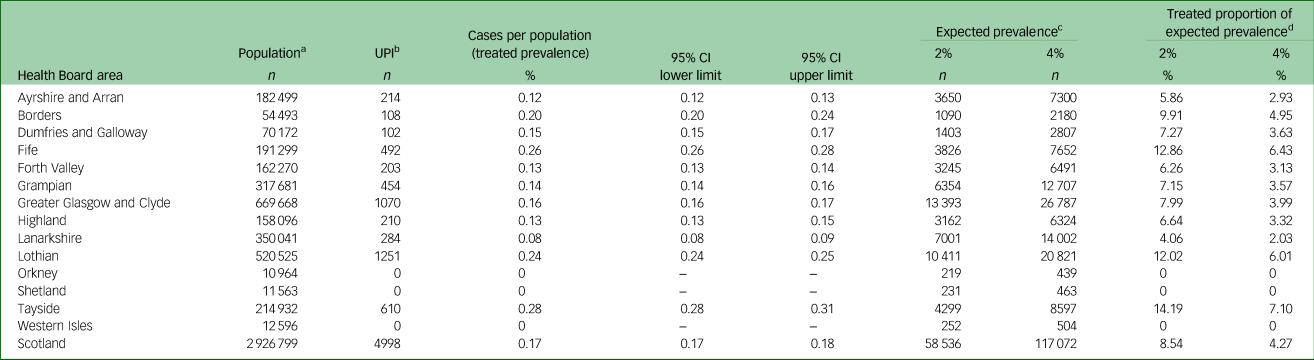
UPI, unique patient identified; ADHD, attention-deficit hyperactivity disorder.
a. National Records of Scotland mid-year population estimate by age group, for NHS Board, 2019.
b. UPI: the numbers of cases prescribed medication typically used to treat ADHD.
c. Expected prevalence of ADHD, as applied to the population.
d. Expected prevalence compared with the number of people identified as being treated for ADHD (UPI).
Discussion
The main benefit of this analysis lies in its utilisation of contemporary data from a national prescribing database, offering a reasonably accurate snapshot of current practice in a national population. The study revealed significant variation in the proportion of the population receiving active pharmacological treatment for ADHD. The number of people receiving pharmacological therapy was significantly below conservative estimates of those who might benefit from such intervention in the community. Our results illustrate that despite a noticeable increase in ADHD prescribing, levels remain lower than expected. This study is important given the concerns about rising prescriptions and fears of clinician overprescribing. These findings serve as strong evidence to the contrary. Some commentators express particular concern over the substantial rise in adult prescriptions. Alternatively, this is a predictable phenomenon, as increasing numbers of individuals initiated on medication during childhood go on to seek continued treatment as they progress into adulthood. Additionally, more adults are seeking diagnosis as ADHD becomes more accepted and understood, and awareness of missed diagnosis in childhood and how this might present in adulthood increases. This an equity and public health issue, as the perceived issues and nervousness about increases may be used as a reason for capping, limiting or even not treating individuals.
It remains evident that there was a significant increase in the number of individuals receiving medication for ADHD between 2010 and 2019. This increase was illustrated using the numbers of people dispensed a prescription (UPI, +233.2%), the DDD (+234.9%) and changes in expenditure on these medicines (GIC, +216.6%). However, the analysis also revealed variations in the number of treated cases compared with estimates of prevalence, indicating less use of medication than might be expected, given the likely size of the population who might benefit from pharmacological interventions. In Scotland, with prevalence estimated at 5–7%, between 72.93 and 80.66% of the adolescent population with likely ADHD were not prescribed medication typically used to treat ADHD in 2019. This represents less than a quarter of the estimated eligible cohort who received a prescription in 2019. For adults, the findings were even more pronounced, with between 91.46 and 95.73% of adults with likely ADHD not prescribed medication typically used to treat ADHD in 2019. This means that fewer than one in ten of the estimated eligible adult cohort were identified as having received a prescription in 2019. Variation in the treated proportion of expected prevalence was present across geographies. In some areas of Scotland, no adult was identified as having a prescription for medication typically used to treat ADHD in 2019. No area exceeded 15% in treatment of expected prevalence for adults. All areas of Scotland had some ADHD prescribing for adolescents, and in some areas, treatment approached or exceeded 50% of expected prevalence.
Our data is in keeping with other published evidence. Studies are identifying decreased ADHD treatment prevalence alongside increases in diagnosis. Recent publications from the UKReference Newlove-Delgado, Ford, Hamilton, Janssens, Stein and Ukoumunne28–Reference Newlove-Delgado, Hamilton, Ford, Stein and Ukoumunne30 found that for cases aged 10–20 years, 61.6% (95% CI 60.6–62.5%) had a prescription at some point for medication typically used to treat ADHD; however, prescribing prevalence declined between the ages of 16 and 18 years, from 37.8% (95% CI 36.6–38.9) to 23.7% (95% CI 22.7–24.6%). This research also confirmed regional variations in prescribing in the UK.Reference Price, Ford, Janssens, Williams and Newlove-Delgado29 The authors identified patchy distribution and unavailability of dedicated ADHD UK services,Reference Price, Ford, Janssens, Williams and Newlove-Delgado29 as well as the risk of cessation of medication, with vulnerable individuals with ongoing ADHD symptoms facing barriers to re-entering services and accessing support.Reference Newlove-Delgado, Ford, Hamilton, Janssens, Stein and Ukoumunne28 A recent meta-analysis of international studiesReference Massuti, Moreira-Maia, Campani, Sonego, Amaro and Akutagava-Martins31 found pooled pharmacological treatment rates were 19.1% (95% CI 11.5–29.9) in children and adolescents with ADHD. This research further estimated that 70% of young people with ADHD might benefit from a trial with pharmacological treatment, and that a substantial number of young people with a diagnosis who might benefit from medication were not receiving it.Reference Massuti, Moreira-Maia, Campani, Sonego, Amaro and Akutagava-Martins31
Explaining the factors influencing the observations made in this study is complex, and there are many potential reasons for the discrepancies observed. Geographic discrepancies in ADHD medication use in Scotland are certainly multifactorial in cause. However, one possible explanation is that variations in service provision and available resources in each region, including access to ADHD diagnostic assessment and transition arrangements, are a contributing factor. All areas in Scotland have a children's ADHD pathway, but an analysis from 2021 found only two regional adult ADHD pathways, and no pathways for adults with ADHD without significant comorbidity.21 These issues could be contributing to limited medication use resulting from a lack of expertise and structures. In some areas of Scotland, no adult was identified as having a prescription. These results came from the island communities of Orkney, Shetland and the Western Isles. These areas are remote and rural, with smaller populations. However, it is possible that local mental health teams have not routinely considered ADHD, despite agreements with larger areas to access more complex health services, including adult neurodevelopmental assessments. Additionally, the limited access to practitioners experienced in treating adults with ADHD could be a crucial factor in the low – or in these areas, entirely absent – use of pharmacological interventions.
The evidence from this study tentatively points to an incomplete recognition of ADHD in adult psychiatric practice. The need for frequent professional review and misconceptions and biases about ADHD and stimulant treatments lead to reduced uptake of medication among adults.Reference Biederman, Fried, DiSalvo, Woodworth, Biederman and Driscoll32 Coupled with insufficient skills, staff and services, this is a significant challenge.Reference Young, Asherson, Lloyd, Absoud, Arif and Colley17 The COVID-19 pandemic has exacerbated the situation, leading to delays and backlogs in non-priority appointments, with long waiting lists.21 Stakeholders report difficulties in accessing help, often facing a ‘postcode lottery’ of services.21 People referred for ADHD may experience rejection from mental health services as their condition may not be deemed as serious as more complex cases, which may involve use of the Mental Health Care and Treatment Scotland Act and higher perceived risk.Reference Young, Asherson, Lloyd, Absoud, Arif and Colley17 In cases of ADHD and mental illness, services may prioritise mental health issues over ADHD assessment and intervention and overlook underlying ADHD concerns.Reference Katzman, Bilkey, Chokka, Fallu and Klassen33 Transitions between services can also lead to potential discontinuation of medication.Reference Newlove-Delgado, Ford, Hamilton, Janssens, Stein and Ukoumunne28 Some primary care practitioners may not consider ADHD monitoring or prescribing as their responsibility, and may hold unhelpful attitudes about the validity of ADHD as a diagnosis and the role of medication.Reference Tatlow-Golden, Prihodova, Gavin, Cullen and McNicholas34 The difficulty in accessing support in the UK and Scotland may force individuals to resort to costly private services, creating a two-tier health system that disadvantages lower-income families.
A further issue is substance use disorders (SUDs). Co-occurrence of ADHD and SUD is common in clinical settings, and a question is whether adults with both diagnoses should be prescribed stimulants despite misuse potential.Reference Chamakalayil, Strasser, Vogel, Brand, Walter and Dursteler35 There are higher rates of SUD in people with ADHD, and some indication that genetic liability to ADHD is associated with higher risks of SUD.Reference Wimberley, Agerbo, Horsdal, Ottosen, Brikell and Als36 However, evidence would suggest that ADHD pharmacotherapy does not increase the risk of SUD.Reference Chamakalayil, Strasser, Vogel, Brand, Walter and Dursteler35 If managed correctly, stimulants are an effective treatment for ADHD, and reducing ADHD symptoms may go on to improve global functioning, reducing risk for SUD, rather than increasing it.Reference Chamakalayil, Strasser, Vogel, Brand, Walter and Dursteler35 This is a particularly pertinent issue for Scotland, where drug-related deaths are relatively high and represent a significant public health issue. Effective interventions that target a particularly at-risk group (in this case people with ADHD) and may lead to reduced levels of drug-related harm and deaths are therefore important, and should be prioritised.
Implications
In future research, priority should be given to collecting a broader range of variables, including linked data on diagnoses received, ethnicity, gender and co-occurrence of ADHD with SUDs. Monitoring and evaluating the development, distribution and effectiveness of specialist ADHD practices would provide insights into their impact on diagnosis rates, psychosocial supports offered and medication. Linked data would strengthen the findings of our research, and would be enhanced particularly by diagnostic information about why medications were given. Future research should also explore the possibility of analysing more refined age categories, particularly focusing on young adults versus individuals aged 30 years and above. It is plausible that further insights on prescribing rates would be derived when age is split in this way. Employing research methods that embrace complexity, such as realist evaluation, theory-based approaches and implementation science methodologies,Reference Sridharan and Nakaima37 would provide useful insights. Co-production with individuals who have lived experience, as well as conducting qualitative research to directly understand the challenges perceived by people seeking ADHD diagnosis, would also be beneficial.Reference Beresford, Mukherjee, Mayhew, Heavey, Park and Stuttard38
Results highlight implications for practitioners. It is crucial to recognise that while medication is an important and effective intervention, the emphasis should be on prioritising environmental modifications and psychosocial support as first-line strategies.8 Considering both medication and environmental modifications as complementary components provides individuals with the most effective and tailored support. Findings from this research also emphasise the need for specialised adult approaches that complement those for young people. Building on the recommendations of the recent Royal College of Psychiatrists (Scotland) ADHD update,20 development of cohesive ‘neurodevelopmental’ pathways emerges as a logical response to the growing need. Although integrated neurodevelopmental pathways remain rare in adult services, there are examples for children's services.Reference Rutherford, Maciver, Johnston, Prior and Forsyth22,Reference Maciver, Rutherford, Johnston, Curnow, Boilson and Murray24 Developing and implementing such pathways requires coverage across self-help, skilled non-statutory services and primary, secondary and tertiary care, representing comprehensive multi-level work that addresses practitioner and institutional elements.Reference Maciver, Rutherford, Johnston, Curnow, Boilson and Murray24 Regarding medication, a key challenge is achieving consensus on prescription practices. Non-medical prescribing roles have the potential to assist, but require advanced practitioner status, proper supervision and funding.Reference Kleve, Vardal and Elgen39 Formal cross-sector performance indicators for pathways, such as waiting times, good practice in assessment, post-diagnostic and psychosocial supports offered, would facilitate consistent practice and effective monitoring. Recognising the value of non-pharmacological approaches necessitates investing in allied health professional roles, including advanced practitioner and consultant roles. An important aspect in mental health services is ensuring that care approaches are neuro-affirmative.Reference Rutherford, Johnston and Carotenuto25,40 Non-pharmacological supports (particularly talking therapies) offered to people with ADHD may not fully consider individual needs, and may cause distress or harm if not adequately adapted for neurodivergent people.40
Limitations
The data utilised in this study were sourced from the PIS, facilitated by colleagues at Public Health Scotland, and linked to a unique patient identifier, the CHI number. A limitation is that our data-set does not capture medications dispensed via hospital services or private prescriptions, which could lead to underestimations of medication use. However, it is important to note that in Scotland, at the time of data collection, there were few private providers, and most prescribing would still be in the community. Our analysis employed broad age bands, which might have obscured more nuanced age-related variations. The lack of linked diagnostic records prevents a direct understanding of the actual number of individuals diagnosed with ADHD across different regions. This limitation necessitates reliance on estimated ADHD prevalence rates derived from external studies. These estimates from external sources do not account for local socioeconomic, cultural or environmental variables that affect ADHD prevalence.
Understanding prescription rates is complicated by various interpretation challenges. There are complexities in assuming a straightforward correlation between ADHD prevalence and medication prescription rates. For example, a lower than expected rate of prescriptions being filled does not necessarily imply undertreatment, as some people may opt for non-pharmacological interventions or discontinue medication because of side-effects. This also links to a critique of the idea that higher prescription rates indicate better or more appropriate treatment. Prescription percentages not approaching prevalence of ADHD may be appropriate and consistent with high-quality care. It is very important to reemphasise that prescriptions alone do not sufficiently reflect an index of quality treatment, given the emphasis on behavioural and environmental supports as the primary management strategies for ADHD. The developmental trajectory of ADHD further complicates interpretations. Many individuals with ADHD continue to require support across the lifespan, but some adolescents requiring pharmacological treatments may not need them in adulthood, with a waxing and waning pattern of presentation, suggestive of an episodic treatment trajectory.Reference Sibley, Arnold, Swanson, Hechtman, Kennedy and Owens41 Given these complexities, our findings should be considered carefully.
In conclusion, this study provides insights into medication use for ADHD across adolescents and adults. The discrepancies observed between estimated prevalence of ADHD and rates of medication prescriptions warrant a cautious interpretation. Based on estimates of the likely ADHD population, it was found that approximately a quarter of adolescents and a tenth of adults were recorded as receiving a prescription through the NHS. Although prescription rates have increased over time, there was no evidence to suggest overtreatment or excessive use of medication. Findings indicate less use of medication in certain segments of the population, particularly in adults, but these numbers should be considered alongside the diversity of management strategies in ADHD. The findings highlight a need to further examine current clinical delivery models, particularly in adult services. Although this study is centred on Scotland, insights and recommendations have broader applicability to other regions facing similar challenges.
Data availability
The data that support the findings of this study are available from the corresponding author, D.M., upon reasonable request.
Acknowledgements
The authors acknowledge the contribution of Stephanie Taylor, who undertook the original data extract.
Author contributions
A.R. and B.M. sourced and analysed the data. A.R. wrote the initial draft of the manuscript. D.M., M.R., M.B., A.R. and B.M. contributed to the analysis, interpretation and clinical recommendations. D.M. wrote the final draft of the manuscript. D.M., M.R., M.B., A.R. and B.M. reviewed the content of the manuscript and reviewed the final draft.
Funding
The analysis was undertaken without additional external funding. The NAIT research team are funded by the Scottish Government.
Declaration of interest
None.







eLetters
No eLetters have been published for this article.