LEARNING OBJECTIVES
After reading this article you will be able to:
• understand how to evaluate and interpret outcome measures in psychiatry
• be aware of the role of organisations in developing and selecting outcomes, including the Royal College of Psychiatrists
• consider the opportunities and challenges of implementing outcome measurement in clinical practice
This article builds on a previous article in this journal (Lewis Reference Kingdon2014), which covered many relevant areas of outcome measurement, including:
• the difference between outcome and process measures
• the categories of outcome that can be measured, such as the changes in symptoms and quality of life
• different types of measure, such as patient-reported outcome measures (PROMs), patient-reported experience measures (PREMs) and clinician-reported outcome measures (CROMs)
• psychometric properties, such as validity and reliability.
We expand on these elements and provide an updated view of the current state of the art in outcome measurement.
Current policy context
National Health Service (NHS) policy in this area moves swiftly and the landscape is continuously changing. Outcome measurement has become a hot topic in mental health services, with increasing emphasis on demonstrating that services are achieving good results. Under the auspices of the Five Year Forward View for Mental Health, NHS England and NHS Improvement published guidelines highlighting the need for a framework approach (NHS England and NHS Improvement 2016a). This document articulates the benefits that such measurement can offer both to individual patients and to the system as a whole.
A key aim for many policy makers has been to produce a system for costing mental health services that links quality and outcome to funding. The payment-by-results (PbR) model for mental health systems attempted unsuccessfully to achieve this, but there are continuing projects seeking ways to do so (Kingdon Reference Keetharuth, Brazier and Connell2019). NHS RightCare (NHS England 2019a) highlights using information from across the whole patient pathway to help identify maximal improvements in both spend and outcomes.
Many commissioners have responded by incorporating the reporting of outcome measurement within key performance indicators (KPIs). This can be done at the local level, as has been implemented in Oxford Health NHS Foundation Trust, where a proportion of funding is attached to a series of outcomes (NHS England and NHS Improvement 2016b). Alternatively, it can be done at a national level, such as the dashboards of NHS England's specialist commissioning, whereby providers are asked to supply data on key outcome measures (NHS England 2020).
The Royal College of Psychiatrists recommends the use of routine outcome measures in psychiatric practice and will shortly publish a mental health outcomes paper, with detailed contributions from each of its faculties. This seeks to provide consensus on the way forward for measuring outcomes across the full spectrum of psychiatric services. This will be available in due course from the Royal College of Psychiatrists' website.
Ways to measure outcomes
A range of definitions exist to describe what outcomes are in the context of healthcare. One of the simplest and most apposite is: ‘Outcomes are the results that matter most to patients’ (International Consortium for Health Outcomes Measurement 2020a). This rightly puts the emphasis on the patient, rather than the clinician, as the primary arbiter of what constitutes a good outcome.
This patient-centred approach has the advantage of harnessing individuals’ subjective experience. Many other stakeholders may also have a relevant perspective on which outcomes are important. For example, family members and clinicians are frequently involved. Repeated measures can provide a longitudinal understanding of a patient's trajectory over time.
Stakeholders’ views can be quantified through the use of reporting tools such as patient-reported outcome measures (PROMs) or clinician-reported outcome measures (CROMs). These usually take the form of a questionnaire, which can contain a mixture of question styles. Potential limitations of such an approach include the interpretability of responses, ‘gaming’ of answers and the reliability of scores between respondents or across time.
Another approach is to measure more objective ‘hard’ outcomes, such as hospital admission, relapse or death. These measures have been extensively used for research purposes, as they are often routinely collected in standardised databases. These have the advantage of being easy to measure and highly reliable but can be of limited practical use because they occur infrequently and fail to capture the nuances of the patient's own experience. Furthermore, they may still be subject to interpretation, for example what constitutes a relapse or requires hospital admission may vary between local services.
Performance measures focus on an individual's performance on a prescribed task, with calibrated measurement of their resultant efforts. Such tests are commonly utilised to determine physical functioning, but can also be used to measure psychological concepts such as cognitive functioning.
Biomarkers can also be used as outcome measures, such as blood tests or radiographic images. These are much less frequently employed in psychiatric illnesses, as they often give little information about results that matter to patients.
Other types of measurement in psychiatry
There can be confusion about the purpose of measurement in mental health services. This can lead to the use of measurement instruments for different purposes than those for which they were designed, which in turn can result in them being used in ways that are not supported by the evidence.
Common uses of measurement in psychiatry include for diagnosis and prediction of likely future events, such as disease prognosis, risk or side-effects. In routine practice, diagnosis is usually made on the basis of clinical judgement, supported by categorical or dimensional nosologies such DSM-5 or ICD-10. In research and in some specialist clinical areas, the use of diagnostic instruments is more common, such as the Structured Clinical Interview for DSM-5 – Research Version (SCID-5-RV) (First Reference First, Williams and Karg2015) or the Diagnostic Interview for Social and Communication Disorders (DISCO) (Leekam Reference Kilbourne, Beck and Spaeth-Rublee2013). Such structured clinical judgement tools offer more robust and defensible diagnosis, while still incorporating the perspective of clinicians. Whether a person continues to meet criteria for a diagnosis after intervention can be used as an outcome measure in research studies. However, such diagnostic instruments often lack responsiveness to change and can therefore be unsuitable for use as dynamic outcome measures.
Prediction of future events using identified risk factors was pioneered in medicine with the use of risk tools such as the Framingham Risk Score for future cardiovascular events (Wilson Reference Trigwell, Kurstow and Santhouse1998). The Framingham Risk Score is a gender-specific algorithm used to estimate the 10-year cardiovascular risk of an individual. It is based on data from the Framingham Heart Study, started in 1948 (Dawber Reference Dawber, Meadors and Moore1951). Similar approaches are now being developed in psychiatry to look at a range of risks, such as suicide, recidivism and violence (Fazel Reference Wilson, D'Agostino and Levy2017). In practice, risk assessment tools may be used as outcome measures, especially in areas where risk reduction is perceived as a desirable result of treatment, such as forensic mental health services. Tracking risk over time in this way may offer a useful way of measuring this aspect of care, but clinicians should be cautious because the qualities that make a good risk prediction model do not necessarily coincide with those of a good outcome measure.
What is a good outcome measure?
The spotlight on outcome measurement has seen a corresponding rise in the number of different available measures (Kilbourne 2018). So how can you choose the best measurement instrument from those on offer? The science behind the development and assessment of outcome measures has advanced considerably in recent years. Leading this process is the COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) group, which has created a suite of research tools for evaluating the measurement properties of the growing number of measures (Prinsen 2018). Although these are mainly designed for PROMs, many of the principles translate to measures completed by other raters, such as clinicians.
Recently their emphasis has changed to focus on the content validity of measures, trumping all other parameters of validity and reliability. Assessing the content validity essentially attempts to answer the question of whether the concept of interest is truly being measured – i.e. does this measure capture what is of real importance? Closely related to this is considering the way that a measure has been developed. Complex criteria exist for determining whether a PROM meets the expected standard, revolving around the quantity and quality of patient involvement in the development and testing of the measure (Terwee Reference Terwee, Prinsen and Chiarotto2018). COSMIN takes the view that if there is not adequate evidence that this process has been performed satisfactorily then the measure should be rejected and there is no need to further assess its other psychometric properties.
If a measure has adequate content validity and has been well developed, then a range of other properties should be considered. COSMIN identifies structural validity as the next most important property. This relies on sophisticated statistical techniques, such as factor analysis, to determine whether the structure of the measurement instrument reflects the concepts it purports to measure. For example, if an instrument is designed to measure psychotic symptoms and health-related quality of life in two separate subscales, does the statistical structure of the test population's scores on these subscales reflect two coherent and distinct underlying factors?
Another example of validity is whether the measure under consideration shows good correlation with the scores of other measures that capture similar concepts. A subscale of a measure that is designed to measure social functioning in people with psychosis could reasonably be expected to produce broadly similar scores to a well-established general measure of functioning, such as the Global Assessment of Functioning (GAF) (American Psychiatric Association 2000). This relies on the assumption that the comparison measure also measures the concept of interest. One type of reliability is the test–retest property, which determines whether the same person gives similar scores over time, when no or minimal change has taken place.
COSMIN recommends considering both the quality of the evidence and the performance within each measurement property when determining the overall quality of an outcome measure. They go on to make recommendations about the selection and interpretation of outcome measures. Ultimately it is the intended purpose of the outcome measurement that will determine the most appropriate measures to use are. For example, a measure used for research could be much more comprehensive than one selected for routine clinical practice, as researchers may have more time to administer the instrument and require more detailed information.
Core outcome sets
Increasingly, individual organisations and wider initiatives are seeking to define which outcomes should be measured in a particular context (Webbe 2018). These so-called core outcome sets (COS) aim to capture sufficient information to understand the most important aspects of a particular condition or population. Originating in research, their purpose was to define the minimum set of outcomes that should be measured in any clinical trial in a specific area. These could include a range of different types of outcome, including biomarkers, performance measures and participant or observer-reported measures. The purpose is to enable more meaningful comparisons between trials and facilitate the process of systematic review and meta-analysis. A rigorous standardised process for developing a COS for research purposes has been established by the Core Outcome Measurement in Effectiveness Trials (COMET) group (COMET Initiative 2020).
Core outcome sets differentiate between ‘what’ to measure and ‘how’ to measure. Qualitative methods, such as in depth interviews and focus groups, are often combined with consensus-building activities, such as Delphi surveys and stakeholder meetings, to determine what should be measured (Williamson Reference Terwee, Prinsen and Chiarotto2017). Systematic reviews can then be used to map out relevant outcome measures in the field and assess their quality, allowing experts to select the most appropriate and robust measures for their needs (Gargon Reference Gargon, Gorst and Williamson2019).
This concept has now been extrapolated to clinical practice, where there is increasing interest in what should be measured in services treating different medical conditions. Spearheading this process internationally is the International Consortium for Health Outcomes Measurement (ICHOM). Its approach is described in more detail below.
Outcome measurement in psychiatry in context
A wide range of organisations, each with a different focus, have an interest in the development and evaluation of outcome measures in mental health. We present an overview of these perspectives, so that the reader is aware of the policy context and to signpost a number of useful resources that are available.
Royal College of Psychiatrists
The Royal College of Psychiatrists (RCPsych) has long been interested in good outcome measurement. It will soon publish an occasional paper setting out the College's current position with regard to outcome measurement and that of its constituent faculties. This work has involved extensive consultation with and coordination between the 13 faculties to establish an outcome framework that covers the full range of psychiatric illness and therapeutic approaches. The paper is an expert resource to facilitate conversations about outcome measures between service providers, commissioners of services and those with lived experience using these data to drive service improvement.
The RCPsych endorses the routine use of outcome measures in clinical practice and has previously set out a series of principles to inform the development and selection of outcome measures (Hampson Reference Hampson, Killaspy and Mynors-Wallis2011). These principles are outlined in Box 1.
BOX 1 The Royal College of Psychiatrists’ principles for outcome measurement
• Focus should be on what is important to patients and carers
• Measures should be relevant to patients and clinicians
• Measures should be simple and easy to use
• Measures should be clear and unambiguous
• Measures should allow comparisons between teams and services
• Measures should be validated for the purpose for which they are used
• IT support should simplify data collection and analysis, and ensure maximum use of data already collected
• Data should be checked for reliability
• Data should be used at the clinical, team and organisational level
• There should be immediate feedback of the data to patients, carers and clinicians so that outcomes can influence the treatment process
The recommendations set out by Reference Hampson, Killaspy and Mynors-WallisHampson et al stress that the choice of outcome measure is dependent on the purpose for which it will be used. This may differ at the individual versus the service level. The authors emphasise that outcome measurement is a way of safeguarding the interests of patients, by ensuring that they are receiving treatments of established effectiveness, tailored to their specific needs. The paper also highlights the need to record potentially negative outcomes, such as the side-effects of treatments, alongside desired improvements. The role of outcome measures in the improvement of clinical services is also underlined, with the caveat that many external factors must be adequately accounted for, such as the challenges of providing services in areas of socioeconomic deprivation. The paper concludes that there was insufficient evidence to support the linking of funding to service outcomes.
Each individual faculty of the RCPsych has adopted a different approach to outcome measurement, with some setting out frameworks recommending particular outcome measures. Other faculties have defined overarching principles relevant to their specialty, without recommending specific measures.
One example of a highly developed approach is that of the Faculty of Liaison Psychiatry, which launched its Framework for Routine Outcome Measurement in Liaison Psychiatry (FROM-LP) (Trigwell Reference Porter and Teisberg2015). This built on work partly commissioned by the RCPsych that led to the publication of the Centre for Mental Health's report Outcomes and Performance in Liaison Psychiatry: Developing a Measurement Framework (Fossey Reference Fossey and Parsonage2014). The authors identify several important sources of heterogeneity within liaison psychiatry that provide particular challenges to coherent outcome measurement (Trigwell Reference Prinsen, Mokkink and Bouter2016). These include variations in the setting of liaison work, the wide range of conditions treated and the considerable differences in service models. They also discuss the difficulty of measuring longer-term improvements in mental health within the context of acute hospital admissions, which are often very brief, and the difficulty of attributing outcomes specifically to the input of liaison psychiatry services, as opposed to any other intervention.
The Liaison Faculty responded to these challenges by identifying the need for a ‘balanced scorecard’ that includes measures of structure, process and outcome (Donabedian Reference Donabedian2005). The FROM-LP (Trigwell Reference Trigwell, Kurstow and Santhouse2015) includes recommended and optional measures of process, including waiting time, clinician-reported measures such as the Clinical Global Impression scale (Busner Reference Busner and Targum2007), PROMs such as Recovering Quality of Life (ReQoL) (Keetharuth 2018), PREMs using patient- and carer-satisfaction scales, and also referrer satisfaction, measured using a dedicated scale. The impact of the framework is evaluated through feedback from faculty members and surveys of its use.
International Consortium for Health Outcomes Measurement (ICHOM)
ICHOM is grounded in the value-based healthcare delivery (VBHCD) approach developed by Porter & Teisberg (Porter 2006). This approach hinges on a hierarchy of outcomes that matter most to patients, linked to bundled payments made for whole episodes of care. It initially focused on medical and surgical conditions, advocating for treatment to be organised into integrated practice units (IPU), where all interventions relevant to a particular condition can be delivered in a coordinated fashion. The hierarchy of outcomes conceptualised by VBHCD is divided into three tiers, ranging from survival to the long-term consequences of therapy (Fig. 1). This philosophy has subsequently been expanded and adapted to the needs of psychiatric conditions.
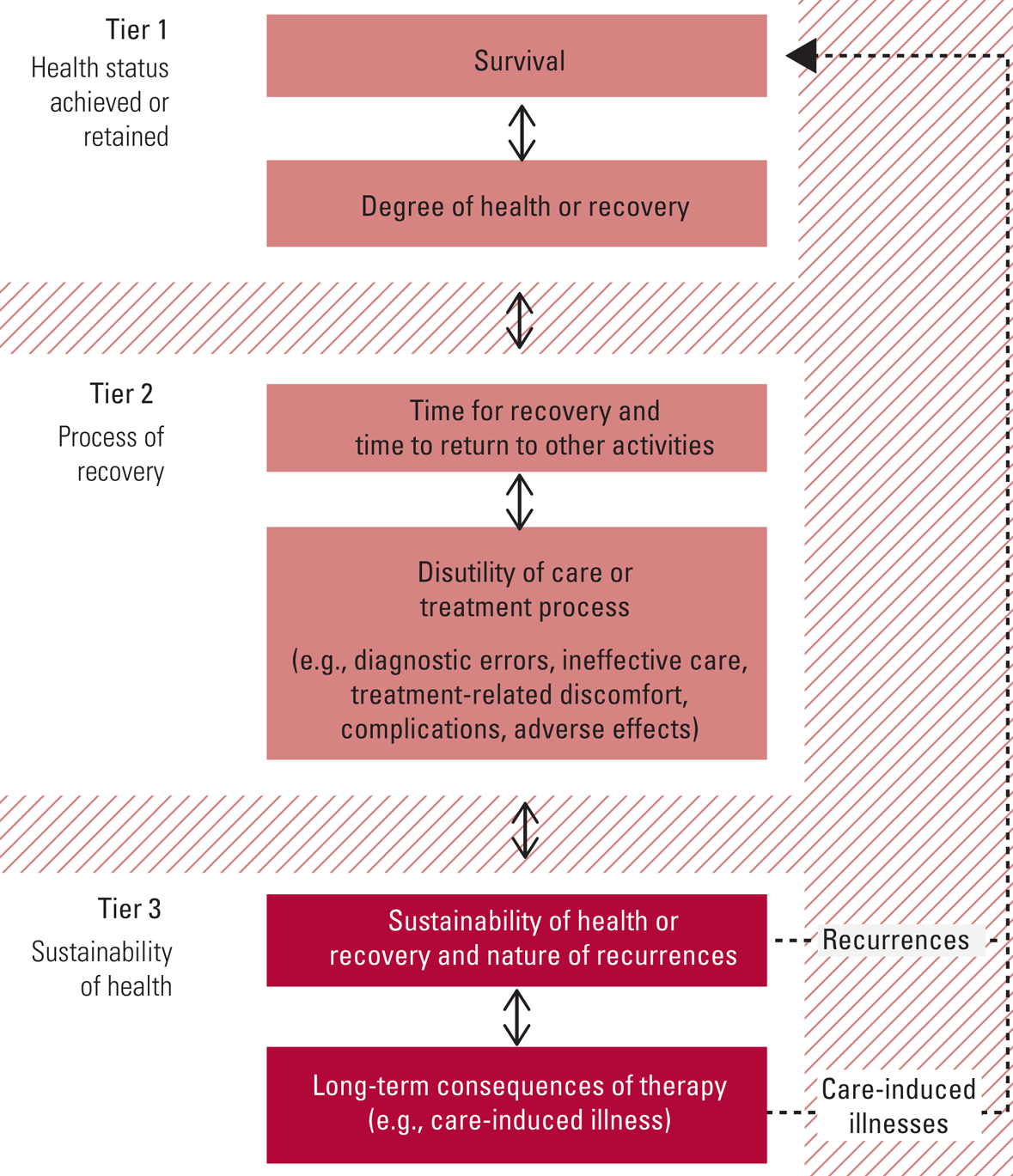
FIG 1 The outcome measures hierarchy (Institute for Strategy & Competitiveness 2020). Reproduced with kind permission of Professor Michael Porter, Harvard Business School.
ICHOM aims to develop internationally relevant core outcome sets for different conditions. It has developed an iterative methodology to create these sets that includes panels of experts and patient partners, supported by administrative and research staff. The sequence of tasks is (1) to prioritise the outcome domains, (2) to select appropriate outcome measures, (3) to prioritise the case-mix domains and (4) to select the case-mix definitions. ICHOM has initially focused on those disorders that are responsible for some of the greatest burden of disease globally (International Consortium for Health Outcomes Measurement 2020b).
The first published ICHOM mental health outcome set covers anxiety and depression (Obbarius 2017). The outcome domains selected were (a) symptom burden, (b) functioning, (c) disease progression and treatment sustainability and (d) potential side-effects of treatment. The recommendations advocate tracking symptoms via a variety of well-documented general and condition-specific scales, such as the Patient Health Questionnaire (PHQ-9), Generalized Anxiety Disorder scale (GAD-7), Social Phobia Inventory (SPIN) and Inventory for Agoraphobia (IFA). Functioning is tracked via the World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0), as well as work status and disease-related absenteeism. Other parameters include time to recovery, overall success of treatment, recurrence of disease and medication side-effects.
The guidelines also recommend recording a series of factors that define the particular characteristics of individuals within a population, such as age, gender, educational level, work status, comorbidities and duration of symptoms. These factors influence the likelihood that a particular individual will achieve a good outcome and therefore offer a way of interpreting aggregate outcomes in the context of that particular population. This process of case-mix adjustment enables more accurate comparison between diverse populations. A predominantly elderly population, with more comorbidities, longer duration of symptoms and less social support may be expected to respond differently to an intervention than a younger population without these factors.
The recommendations finish by setting out a proposed schedule for the collection of data, including both the outcome measures and the relevant case-mix factors. This includes a set of recommended measures at baseline, at annual assessment and during treatment monitoring, designed to capture the impact of specific interventions.
ICHOM aims to publish more outcome sets on mental health conditions, including addictions, depression and anxiety in young people, psychotic disorders and personality disorders.
Outcome measurement in commissioning and quality assurance
Outcome measurement is beginning to be used more routinely in commissioning processes and for the quality assurance of existing services. Some providers of mental health services have started to link payments to outcomes. In 2016 the Oxfordshire Clinical Commissioning Group worked with Oxford Health NHS Foundation Trust to develop an outcome-based commissioning model (NHS England and NHS Improvement 2016b). This consisted of a core payment that was fixed, linked with an outcome-based incentive payment and a mechanism that shared the associated risks between commissioners and providers. The agreed structure linked 20% of the funding to outcomes. Of this, 2.5% was in Commissioning for Quality and Innovation (CQUIN) payments, while the rest was linked to seven outcomes that were co-produced between the service and experts by experience (Box 2).
BOX 2 Outcomes used for linked payments in Oxford Health NHS Foundation Trust
Outcome 1: people will live longer
Outcome 2: people will improve their level of functioning
Outcome 3: people will receive timely access to assessment and support
Outcome 4: carers feel supported in their caring role
Outcome 5: people will maintain a role that is meaningful to them
Outcome 6: people will continue to live in stable accommodation
Outcome 7: people will have fewer physical health problems related to their mental health
(NHS Improvement 2016)At a national level, outcomes have been used by commissioners within specialised services to monitor and incentivise improved quality of care. One example is the quality dashboards used by the Clinical Reference Groups that support NHS England. These include a range of key descriptors of quality that include measures of both process and outcomes. For example, medium and low secure services for adults are expected to report the proportion of patients with an improved score on the Health of the Nation Outcomes Scales for secure and forensic patients (HoNOS-Secure) on discharge (NHS England 2020).
National Institute for Health and Care Excellence (NICE)
NICE aims to improve outcomes for people using the NHS and other public health and social care services, while reducing variations in quality of care. NICE produces evidence-based guidance and quality standards for health practitioners. It also develops quality standards and performance metrics for providers and commissioners.
NICE has developed a sophisticated methodology for assessing particular interventions, which includes a health economic assessment of the cost-effectiveness of interventions (National Institute for Health and Care Excellence 2014). To do this it uses the impact that conditions and treatments have on quality of life to calculate quality-adjusted life-years (QALYs), which can then be compared with the relevant costs. If the incremental cost-effectiveness ratio (ICER) of an intervention is greater than £30 000, then NICE is unlikely to approve its use without strong additional evidence or rationale. To do this consistently, NICE prefers to use a single outcome measure, the EQ-5D, which contains the five domains of mobility, self-care, usual activities, pain/discomfort and anxiety/depression. The respondent is asked to tick a corresponding statement within each domain that they believe correlates with their current status. Despite containing only one domain that is directly related to mental health, the EQ-5D is still used by NICE for assessing interventions for mental health conditions.
A range of documents endorsed by NICE that are relevant to mental health services advocate the use of specific outcome measurement approaches to monitor response to treatment. These are often produced collaboratively with other stakeholders. One example is the implementation of the early intervention in psychosis access and waiting time standard (NHS England, NCCMH and NICE 2016). This sets out the measures and timescale for collection expected for outcomes within early intervention in psychosis services.
Patient-Reported Outcomes Measurement Information System (PROMIS)
PROMIS is an initiative funded by the National Institutes of Health (NIH) in the USA. It is part of the overarching health measures programme, which also includes measures for people with neurological illness and sickle cell disease. The NIH toolbox encompasses a series of performance measures of cognitive, motor and sensory function (Northwestern University 2020). PROMIS is specifically designed for people with chronic health conditions and includes over 300 instruments to measure patients’ mental health, as well as measuring physical health, social health and overall global well-being. Mental health profile domains cover anxiety and depression, with additional domains for adults concerning alcohol use, smoking, substance use, anger, cognitive function, life satisfaction, meaning and purpose, positive affect, psychosocial illness impact and self-efficacy for managing chronic conditions. As well as using conventional ‘short-form’ questionnaires, PROMIS also uses computer adaptive testing (CAT).
Computer adaptive testing ranks items related to a particular concept in a hierarchy of severity (Gibbons Reference Gibbons, Weiss and Frank2016). For example, in depression more people with mild depression would be expected to say that they felt unhappy in the past week than would say that they felt that they wanted to die. This means that feeling unhappy is placed towards the bottom of the hierarchy of questions, whereas feeling that you want to die is nearer to the top. Respondents are initially asked a question that is somewhere in the middle of the hierarchy. Their answer to this determines which question they are asked next, until their position on the scale of severity has been determined. This system has the advantage of identifying the severity of someone's symptoms by using fewer questions than standard approaches, because the sequence of questions is tailored to each respondent. This reduces the burden on respondents by minimising the number of questions they need to answer.
Challenges and opportunities in implementing outcomes
The implementation of outcome measures is a highly complex and evolving area. Outcome measurement can be implemented at the level of the individual patient, as a way of enabling the patient, their friends and family and the clinical team responsible for their care to monitor their progress over time. This can be linked to particular treatments or approaches, as a way of providing an objective assessment of the impact of specific interventions for that patient, which supports clinical decision-making. Outcome measurement can also be used at the aggregate level as a way of determining whether a particular intervention is effective at a population level, to compare services and to improve quality.
Challenges
A number of challenges arise when implementing outcome measurement at an aggregate level. The user-led collective Recovery in the Bin warns that outcome measures can place too much emphasis on the individual patient to recover in a narrowly defined way, which does not take adequate account of the social and political realities affecting a person's wellbeing (Recovery in the Bin 2014). Their ‘Unrecovery Star’ includes items such as poverty and discrimination, as a way to redress this imbalance (Recovery in the Bin Reference Obbarius, Van Maasakkers and Baer2017).
The actual or perceived consequences of outcome measurement may affect the way that those producing the measurement behave and therefore the measurement itself. If certain outcomes are seen to be either rewarded or penalised, then this is likely to affect the way that those outcomes are assessed. This process can happen consciously or unconsciously and can take a number of forms. One way is simply to assign more or less favourable scores depending on the desired result. This process can be done inadvertently, particularly when there is genuine equivocation about which response option to choose. Another approach is to undertake measurement at a point in time when the desired response is more likely, for example asking someone to complete a measure immediately after receiving good news to obtain a more positive score.
Careful thought must be given to what incentives are attached to outcome data at the individual and systemic level. Communication with those stakeholders completing outcome measures is essential to build trust and to understand any perceived incentives, which may or may not have been anticipated.
Finally, there is the risk that services will ‘cherry-pick’ patients they believe are more likely to have good outcomes, neglecting those who will not. The latter may be more vulnerable to begin with, so it is essential that they are not denied the support they need. The use of validated case-mix data can be used to prevent cherry-picking by adjusting for characteristics of a population that may lead to less favourable outcomes.
Opportunities
Data should be collected in a consistent and reliable way, so that the quality of resultant information can be widely trusted. Digital approaches have provided significant improvements in the collection, analysis and presentation of information. Outcomes are now often routinely integrated into electronic patient records, meaning that responses can be recorded faster and more reliably. Digital technology offers greater opportunities for data to be collected over time and presented back to patients and teams to provide a longitudinal graphical representation of changes.
The forthcoming RCPsych paper will recommend using small numbers of well-validated outcomes, consistently implemented and coherently analysed. This echoes the technical guidance issued by NHS England and NHS Improvement, which recommends using only three to seven outcome measures (NHS England and NHS Improvement 2016c). One example where outcome measurement has been implemented at a national level is through the Improving Access to Psychological Therapies (IAPT) programme (National Collaborating Centre for Mental Health Reference Leekam and Volkmar2019). The IAPT programme aims to expand the availability of psychological therapies and monitor the effectiveness of these interventions through integral outcome monitoring. The manual prescribes the type and frequency of measurement for a range of conditions. It also outlines information about how to maintain data quality, stressing the importance of paired measurement, in order to track progress over time.
The Long Term Plan for Mental Health highlights that all providers must submit data to the Mental Health Services Data Set (MHSDS) and IAPT data-set (NHS England 2019b). Transparency regarding the achievement of outcomes and levels of quality supports patient choice, enables benchmarking of care across equivalent services, supports workforce planning and ensures the effective use of resources.
Conclusions
Outcome measurement is a hot topic in healthcare as a whole, including mental health services. Psychiatrists will increasingly be expected to have a basic understanding of how to measure outcomes effectively within their own scope of practice. It is essential to choose outcome measures carefully, ensuring that they are appropriate for the context of use and capture the whole range of relevant domains, not just clinical symptoms. Outcome measures must focus on measuring what is most important and this needs to prioritise the patient's perspective. Implementing outcome measurement offers great potential, but has a number of challenges. Psychiatrists must be aware of these pitfalls and take active steps to guarantee that outcomes are measured robustly, in a way that can lead to meaningful improvement.
Author contributions
All authors fulfil the ICMJE criteria for authorship.
Declaration of interest
J.C. is the Lead for Outcomes in Mental Health and the Specialist Advisor for Mental Health Payment Systems for the Royal College of Psychiatrists.
ICMJE forms are in the supplementary material, available online at https://doi.org/10.1192/bja.2020.58.
MCQs
Select the single best option for each question stem
1 The Structured Clinical Interview for DSM-5 – Research Version (SCID-5-RV) is an example of:
a a patient-reported outcome measure
b a performance measure
c a diagnostic instrument
d a risk assessment
e a clinician-reported outcome measure.
2 The COnsensus Standards for health Measurement Instruments (COSMIN) group approach prioritises:
a structural validity
b test–retest reliability
c the clinician's perspective
d content validity
e reducing costs.
3 Which of the following is not a guiding principle of outcome measurement for the Royal College of Psychiatrists?
a measures should be clear and unambiguous
b the focus should be on what is important to patients and carers
c measures should be relevant to patients and clinicians
d measures should be simple and easy to use
e measures should focus only on psychiatric symptoms.
4 Which of the following is not part of the value-based healthcare delivery (VBHCD) hierarchy of outcomes?
a time for recovery and time to return to other activities
b arranging services into integrated practice units
c survival
d degree of health or recovery
e disutility of care or treatment process.
5 Computer adaptive testing:
a ranks items related to a particular concept in a hierarchy of severity
b is not recommended by the Patient Reported Outcomes Measurement Information System (PROMIS)
c involves additional respondent burden over paper-based measurement
d is inappropriate for psychiatric illnesses
e is recommended by the Framework for Routine Outcome Measurement in Liaison Psychiatry (FROM-LP).
MCQ answers
1 c 2 d 3 e 4 b 5 a





eLetters
No eLetters have been published for this article.