LEARNING OBJECTIVES
After reading this article you will be able to:
• identify the most common challenging behaviours associated with developmental disabilities in children
• demonstrate an understanding of common assessment tools used to identify the topography, severity and function of challenging behaviours
• demonstrate an understanding of behavioural techniques used to modify challenging behaviours.
Challenging behaviours often co-occur at high rates among those with developmental disabilities such as autism spectrum disorder (ASD) and intellectual disability (Didden Reference Didden, Sturmey, Sigafoos and Matson2012). Although the term challenging behaviour encompasses a variety of topographies, it generally refers to behaviours that are dangerous, socially unacceptable or negatively affect the person's education (Jang Reference Jang, Dixon and Tarbox2011). Challenging behaviours among those with ASD and/or intellectual disability generally arise from both biological and environmental factors and can result in adverse consequences such as social rejection, increased caregiver stress, exclusion from services or educational settings, and health risks (Didden Reference Didden, Sturmey, Sigafoos and Matson2012). Function-based assessment and behavioural interventions most successfully reduce challenging behaviours. In this article, we discuss the prevalence, risk factors, assessment tools and treatment methods for the primary challenging behaviours exhibited among those with developmental disabilities (e.g. self-injury, property destruction, aggression).
Prevalence and risk factors
Prevalence rates of challenging behaviours among children with intellectual disability range between 10 and 20%, with the prevalence increasing during teenage years (McClintock Reference McClintock, Hall and Oliver2003). Challenging behaviours are more prevalent among children with a diagnosis of ASD (Didden Reference Didden, Sturmey, Sigafoos and Matson2012). As many as 56–94% of children with ASD exhibit one or more challenging behaviours, although prevalence estimates vary greatly based on differing research methodologies (e.g. operational definitions, assessment tools) (Kanne Reference Kanne and Mazurek2010). Between a half and two-thirds of individuals who exhibit challenging behaviours exhibit at least two different forms (Murphy Reference Murphy, Healy and Leader2009).
Several factors may contribute to the likelihood that children will develop challenging behaviours, including diagnostic category (McTiernan Reference McTiernan, Leader and Healy2011). For example, children with a previous ASD diagnosis are more likely to exhibit challenging behaviours compared with their peers (Didden Reference Didden, Sturmey, Sigafoos and Matson2012). Specifically, self-injury, aggression and property destruction are more likely to be demonstrated by children with ASD (Jang Reference Jang, Dixon and Tarbox2011). Furthermore, ASD symptom severity has been found to be positively correlated with both the frequency and the intensity of challenging behaviours exhibited by children with ASD. Similarly, severity of intellectual disability has been found to be associated with increased challenging behaviours (Didden Reference Didden, Sturmey, Sigafoos and Matson2012). Self-injury and stereotypy are particularly more prevalent among those with severe and profound intellectual disability (McClintock Reference McClintock, Hall and Oliver2003). Comorbid medical conditions and psychopathology, such as gastrointestinal disorders, epilepsy, sleep problems, anxiety behaviours and conduct problems, have also been found to be associated with increased rates of challenging behaviour (Klukowski Reference Klukowski, Wasilewska and Lebensztejn2015).
Additionally, challenging behaviours have been found to be associated with deficits in adaptive behaviour in children with developmental disabilities (Baeza-Velasco Reference Baeza-Velasco, Michelon and Rattaz2014). Researchers investigating the relationship between adaptive skills and challenging behaviours among children with ASD and other developmental disabilities found that poorer receptive and expressive communication skills, more severe social deficits, as well as restricted and repetitive behaviours, were associated with challenging behaviours such as aggression, self-injury and tantrums (Park Reference Park, Yelland and Taffe2012). However, other researchers indicated that lower receptive and expressive communication skills were either not associated with challenging behaviour or were strongly associated with lower levels of aggression and self-injury (Kanne Reference Kanne and Mazurek2010).
Demographic factors such as gender and age may also affect the prevalence of challenging behaviours; however, the results of studies on the association between demographic factors and challenging behaviours have varied. Regarding gender, early researchers indicated that males with intellectual disability were more likely to engage in challenging behaviours than their female counterparts, particularly aggression and property destruction (Oliver Reference Oliver, Murphy and Corbett1987). However, more recently researchers have suggested that gender has no effect on the rates of challenging behaviours among children and adolescents with ASD (Murphy Reference Murphy, Healy and Leader2009; Kanne Reference Kanne and Mazurek2010). Similarly, the prevalence of challenging behaviours has been found to increase with age throughout childhood, although younger children have an increased likelihood of exhibiting aggression and self-injury (Didden Reference Didden, Sturmey, Sigafoos and Matson2012). Conversely, several other studies found no association between age and prevalence of challenging behaviour among those with developmental disabilities (McTiernan Reference McTiernan, Leader and Healy2011). Differences in the characteristics of the samples used, the behaviours measured and the measures used may account for the variable findings among studies.
Defining challenging behaviours
Aggressive behaviour
Aggression can be defined as either verbal (e.g. verbal threats or derogatory statements towards others) or physical behaviour (e.g. hitting, biting, kicking or throwing objects at others) that may result in harm or injury to another individual (Fitzpatrick Reference Fitzpatrick, Srivorakiat and Wink2016). Although estimates vary, studies have shown that between 22 and 56% of children diagnosed with ASD exhibit aggression (Kanne Reference Kanne and Mazurek2010). It is essential to treat aggressive behaviour, as it is associated with several adverse outcomes, such as increased use of psychotropic medications, parental stress, educator burnout, relationship deficits and an increased risk of physical abuse (Fitzpatrick Reference Fitzpatrick, Srivorakiat and Wink2016).
Non-compliant behaviour
Non-compliant behaviour is generally marked by a failure to respond with desired and appropriate behaviour when presented with a request (Luiselli Reference Luiselli and Matson2009). Non-compliance may include a ‘passive response’ in which the individual fails to follow through with instructions, although this is often accompanied by other challenging behaviours, such as aggression or property destruction (Luiselli Reference Luiselli and Matson2009: p. 176). Prevalence rates between 25 and 65% are reported by studies of children and adolescents without disabilities (Kalb Reference Kalb and Loeber2003). However, non-compliant behaviours can be especially alarming for caregivers of children with developmental disabilities, as they are associated with poor academic progress and delays in acquiring new skills (Lipschultz Reference Lipshultz and Wilder2017a).
Property destruction
Property destruction can be considered a subcategory of aggressive behaviour. Whereas aggressive behaviour is generally directed towards others, property destruction is directed toward objects and includes damaging personal or public property through tearing, hitting, breaking or kicking objects (Didden Reference Didden, Sturmey, Sigafoos and Matson2012). As previously noted, it is important to treat behaviours involving property destruction, as they are associated with increased caregiver stress, an increased likelihood of out-of-home placements and of psychotropic medication use, and interference with educational instruction (Didden Reference Didden, Sturmey, Sigafoos and Matson2012).
Self-injurious behaviour
Self-injurious behaviour (SIB) is characterised as behaviour directed towards one's own body that can result in harm or tissue damage (Summers Reference Summers, Shahrami and Cali2017). SIB has been reported to occur in approximately 50% of children with ASD and can present on continua of both severity and frequency, ranging from mild forms (e.g. head rubbing, thigh slapping) to severe forms of behaviour (e.g. head banging, eye poking, rumination) (Summers Reference Summers, Shahrami and Cali2017). Among individuals with ASD and intellectual disability, head banging has been reported as the most common form of SIB, although other forms include head hitting, hair pulling, rumination and pica. SIB can cause serious concerns related to the individual's safety, as well as an increased risk of hospital admission, the use of mechanical and/or physical restraints and psychotropic medication use (Didden Reference Didden, Sturmey, Sigafoos and Matson2012).
Stereotypical behaviour
Stereotyped behaviour, defined as repetitive vocal or motor behaviours, are a characteristic feature of ASD (American Psychiatric Association 2013). Some of the most common forms of stereotypical behaviour include body rocking, spinning, repetitive hand movements and posture abnormalities (APA 2013). Although typically developing children may display repetitive motor movements, these often diminish with age and do not interfere with daily living. Compared with other common challenging behaviours, stereotypical behaviour has been considered less problematic. However, engagement in stereotypical behaviours by those with developmental disabilities can impede skill acquisition, be socially stigmatising and may develop into self-injury and other forms of challenging behaviour (Didden Reference Didden, Sturmey, Sigafoos and Matson2012).
Toe-walking behaviour
Toe-walking refers to ambulatory stance in which individuals walk with a toe-to-toe gait, without making heel contact with the ground (Sala Reference Sala, Shulman and Kennedy1999). Although toe-walking can be present in typically developing children in early childhood, it is not considered to be problematic until after 2 years of age. Toe-walking commonly affects children diagnosed with ASD, with a prevalence rate of nearly 20.1% (Barrow Reference Barrow, Jaworski and Accardo2011). Toe-walking can be caused by spinal or muscular abnormalities, although its cause is often unknown in individuals with ASD (Sala Reference Sala, Shulman and Kennedy1999). Assessment and intervention targeting toe-walking are beneficial, as it can lead to medical difficulties (e.g. foot and ankle abnormalities or pain, limping, bunions), social stigmatisation or reduced exercise if left untreated (Caserta Reference Caserta, Pacey and Fahey2019).
Transition-related challenging behaviour
Resistance to change, including extreme distress at small changes and adherence to specific routines, are distinctive features of ASD (APA 2013). Challenging behaviours often occur as a result of resistance to change and can intensify if they are not treated (Neil Reference Neil and Sturmey2014). These transition-related challenging behaviours can adopt multiple topographies, including destructive behaviour (e.g. aggression, property destruction), elopement (e.g. leaving a designated area without permission) or uncooperative behaviour (e.g. tantrum or dropping behaviours) (Lehardy Reference Lehardy, Lerman and Evans2013). Transition-related challenging behaviours can present safety concerns and can interfere with educational and social opportunities in the classroom (Varni Reference Varni, Lovaas and Koegel R1979).
Assessment tools
Indirect assessment
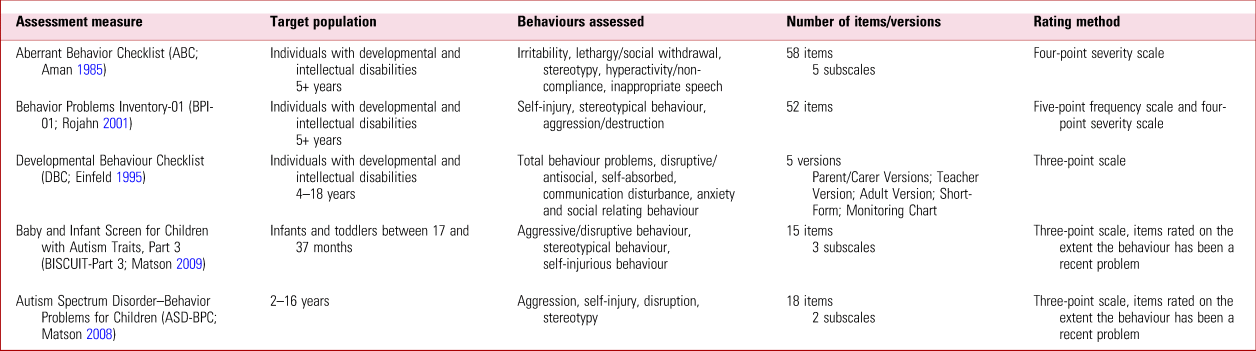
Several tools have been developed to properly assess challenging behaviours in those with developmental disabilities. It is essential to identify the function of presented challenging behaviours so that an appropriate behavioural intervention plan can be developed. The first step in identifying the function of challenging behaviours is often the use of indirect assessment tools. These tools typically consist of interviews, rating scales or questionnaires rated by caregiver informants (e.g. parents or teachers) to obtain information about challenging behaviours and the environmental context in which they occur. Several such assessment tools are available, some of which assess the topography, intensity and frequency of the behaviours while others assess their function (Cividini-Motta Reference Cividini-Motta, Bloom, Campos and Matson2017). Table 1 presents key details regarding a number of rating scales available for the former purpose.
TABLE 1 Rating scales to assess the severity, frequency and topography of challenging behaviours
Although the scales identify the topography, severity and frequency of challenging behaviours, other measures provide indirect assessment of behavioural function. The Functional Assessment Interview (FAI; O'Neill Reference O'Neill, Albin and Storey2015) is a semi-structured interview that consists of 11 sections designed to acquire information about setting events (events that ‘set off’ the behaviour), the immediate antecedent (trigger) and consequences of the behaviour, as well as the possible function(s) maintaining the behaviour. Additionally, information about the individual's communication skills, the efficacy of the behaviour (e.g. amount of effort required, reward frequency), preferred rewards and activities, and previous behavioural intervention strategies is collected to formulate hypotheses about the behaviour. Unlike other indirect measures of behavioural function, the FAI does not produce a score to aid in differentiating a behaviour's functions; however, it provides useful qualitative information for intervention planning (O'Neill Reference O'Neill, Albin and Storey2015). Several brief structured rating scales for assessing the function of behaviour are also available (Table 2).
TABLE 2 Rating scales to assess the functions of challenging behaviours

Direct assessment
Direct assessment requires observation of challenging behaviours in the setting in which they take place, such as the school, home or clinic (Cividini-Motta Reference Cividini-Motta, Bloom, Campos and Matson2017). Direct observation techniques and obtaining quantifiable data can be essential to the development of treatment plans to reduce target behaviours (Cohen Reference Cohen, Yoo, Goodwin, Matson and Sturmey2011). Clinical psychologists primarily use indirect rating scales, whereas psychologists in special education and school psychology may espouse an applied behaviour analysis method to assess challenging behaviours. These direct assessment techniques include constructing operational definitions, antecedent–behaviour–consequence recording and experimental functional analyses (Cohen Reference Cohen, Yoo, Goodwin, Matson and Sturmey2011).
The initial step in direct observation involves the formation of an operational definition of the target behaviour to obtain reliable data. When creating the operational definition, clinicians should describe the target behaviour in detail to prevent disagreement between observers. Rather than identifying the category of a target behaviour (e.g. aggression), the topographies (e.g. hitting, slapping, kicking) should be listed to ensure that the target behaviour can consistently be observed and measured. For example, for one child aggression might consist of multiple behavioural topographies, including biting, hitting and kicking. However, another might engage in just one behavioural topography (e.g. kicking) that serves multiple functions (Cohen Reference Cohen, Yoo, Goodwin, Matson and Sturmey2011).
One of the most widely used forms of direct assessment is known as antecedent–behaviour–consequence (ABC) recording. This form of recording involves tracking the antecedent (events preceding the target behaviour), the target behaviour and the consequence (events following the target behaviour) in a narrative format. These data can aid in hypothesising the function of the target behaviour, as well as identifying any strategies that may reduce the challenging behaviour in the future. ABC recording is frequently used, as it is time effective and requires minimal training. Scatterplots are another descriptive direct assessment method. They can be used to identify time periods that may be associated with challenging behaviours, although they do not assist with the identification of functions maintaining the behaviours (Cividini-Motta Reference Cividini-Motta, Bloom, Campos and Matson2017).
Other direct assessment techniques involve collecting quantifiable data and, in such cases, specifying the procedures for recording observations, length of time for observations and interval between sessions is crucial. One form of collecting data, continuous recording, involves tracking one or more dimensions of a challenging behaviour each time it occurs. These dimensions include frequency, duration, latency, intensity and physical impact (e.g. whether bruising is caused). Continuous measurement systems allow for a comprehensive record under observation. For example, a clinician may track the frequency of a target challenging behaviour (e.g. tantrum behaviour) using a hand-held counter or electronic counting system. Clinicians may use duration recording for behaviours that are non-discrete, such as persistent mouthing of objects, to track the total amount of time the individual engaged in the behaviour during an observation period. Latency recording tracks the time between the occurrence of an antecedent event and the child starting (or ceasing) to engage in the behaviour of concern. Continuous observation and recording can be difficult and demanding, and as a result several methods (e.g. partial interval recording, whole interval recording and momentary time sampling) have been developed to provide estimates of levels of behaviours while reducing demands on the observer (Cohen Reference Cohen, Yoo, Goodwin, Matson and Sturmey2011).
Following the use of scales or interviews and direct observation methods, an experimental functional analysis (EFA) may be conducted to identify the definite function that a target challenging behaviour serves (Cividini-Motta Reference Cividini-Motta, Bloom, Campos and Matson2017). The completion of an EFA is considered best practice in the field of applied behaviour analysis, as it allows for function-based treatment plans. Unlike other forms of descriptive direct assessment, such as ABC recording, EFAs experimentally manipulate the antecedents and consequences of a target behaviour in both control and test conditions (Cividini-Motta Reference Cividini-Motta, Bloom, Campos and Matson2017). Although EFAs are beneficial in developing function-based treatments, they can be impractical to complete in everyday clinical practice as they require specialised training and can be time intensive. As a result, alternative indirect methods that provide information about the functional variables maintaining behaviours, such as the Questions About Behavioral Function (QABF) checklist or Motivation Assessment Scale (MAS) (Table 2), can be especially useful for clinicians.
Treatment
Behavioural intervention
The most widely investigated treatment option for ASD is applied behaviour analysis, which provides the basis for several evidence-based interventions for challenging behaviours. Applied behaviour analysis strives to use the least restrictive intervention. Several non-aversive behavioural interventions have been found to be efficacious in reducing challenging behaviour. Behavioural interventions generally consist of both antecedent-based and consequence-based strategies (Lipshultz Reference Lipshultz and Wilder2017a). Antecedent-based strategies are interventions that modify environmental stimuli to prevent the occurrence of challenging behaviour, whereas consequence-based strategies involve modifying contingencies of reinforcement in the environment to promote the reduction of challenging behaviour (Cividini-Motta Reference Cividini-Motta, Bloom, Campos and Matson2017).
Antecedent-based interventions
Commonly used antecedent-based interventions include provision of advance notice, high-probability instructional sequences, activity choice and non-contingent reinforcement (Lipshultz Reference Lipshultz and Wilder2017a). Advance notice involves providing information about when a present activity will end and another will begin. Advance notice can be given in many forms, including visual cues (e.g. timers), verbal statements and activity schedules. These cues can be beneficial by increasing the predictability of transitions. Research indicates that the efficacy of advance notice as an antecedent intervention may be dependent on certain variables, including the unpredictability of transition-related events such as changes in the sequence, timing or content of a transition (Brewer Reference Brewer, Strickland-Cohen and Dotson2014).
A high-probability instructional sequence (high-p sequence) involves presenting several tasks that the individual is likely to comply with (i.e. high-probability instructions) before presenting tasks with a lower likelihood of compliance (i.e. low-probability instructions). This method has been used to increase compliance in a range of settings with many different populations, including young children with developmental disabilities. Researchers have suggested that a high-p sequence most effectively increases compliance when highly preferred reinforcers are used with high-probability (high-p) instructions during the sequence. The interval between the last high-p instruction and the first low-probability (low-p) instruction should be short, less than 5 s, to increase efficacy and reduce non-compliance. High-p sequences can also be effective when they are combined with other antecedent-based and consequence-based interventions, such as demand fading or extinction procedures discussed in the next section (Lipshultz Reference Lipshultz and Wilder2017b).
Activity choice provides the opportunity for the individual to select the time, location or order in which tasks are presented to them. This antecedent-based intervention can be easily implemented and promotes compliance and reduced challenging behaviours, as it allows the individual to avoid aversive aspects of a task (Geiger Reference Geiger, Carr and LeBlanc2010). However, activity choice is not an intervention that can be used to respond to challenging behaviours while they are occurring; as a result, activity choice may be most effective if it is combined with a consequence-based procedure to further decrease the behaviour (Geiger Reference Geiger, Carr and LeBlanc2010).
Non-contingent reinforcement (NCR) is a reinforcement-based antecedent intervention frequently used to treat challenging behaviours. NCR involves delivering reinforcement on either a fixed or variable schedule regardless of whether the behaviour occurs during the specified time interval (Lloyd Reference Lloyd and Kennedy2014). Unlike differential reinforcement interventions (see below), the individual's behaviour during the specified time interval does not influence the receipt of reinforcement (Tucker Reference Tucker, Sigafoos and Bushell1998). For example, an individual exhibiting challenging behaviour maintained by an attention function may receive adult attention in the form of social praise once every 2 min. For challenging behaviours that are maintained by social reinforcement, extinction procedures are often used in conjunction with NCR, such that reinforcement is provided on a time-based schedule and withheld after the occurrence of a challenging behaviour (Lloyd Reference Lloyd and Kennedy2014). NCR can be beneficial in that it does not require continuous monitoring of behaviour, making it more practically useful in applied settings (Tucker Reference Tucker, Sigafoos and Bushell1998). Because NCR is an antecedent-based intervention, it can prevent challenging behaviours from occurring at all. When challenging behaviours do occur, NCR immediately reduces the behaviours while still providing reinforcement (Geiger Reference Geiger, Carr and LeBlanc2010).
Consequence-based interventions
Differential reinforcement and extinction are frequently used consequence-based interventions for challenging behaviours. Differential reinforcement involves withholding reinforcement in the presence of challenging behaviour (i.e. extinction) and providing access to reinforcement when a target response is produced (Geiger Reference Geiger, Carr and LeBlanc2010). There are several variations of differential reinforcement (Box 1).
BOX 1 Variations of differential reinforcement
• Differential reinforcement of other behaviour (DRO): reinforcement is provided after a specified time interval if the challenging behaviour does not occur during the interval (Tucker Reference Tucker, Sigafoos and Bushell1998)
• Differential reinforcement of alternative behaviour (DRA): reinforcement is provided for a specific alternative behaviour but not for the challenging behaviour (Geiger Reference Geiger, Carr and LeBlanc2010)
• Functional communication training (FCT): a specific type of DRA in which the alternative response is a communication response (verbal, symbol or gestural) requesting the reinforcing event (Geiger Reference Geiger, Carr and LeBlanc2010)
• Differential reinforcement of incompatible behaviour (DRI): reinforcement is provided when an individual engages in a behaviour that is not compatible with the challenging behaviour (Zane Reference Zane, Davis and Volkmar2013)
• Differential reinforcement of low rates of behaviour (DRL): reinforcement is provided when fewer occurrences of the challenging behaviour or longer intervals between responses take place (Zane Reference Zane, Davis and Volkmar2013)
Differential reinforcement of alternative behaviour (DRA) and differential reinforcement of other behaviour (DRO) are the most commonly used differential reinforcement techniques. They have been shown to effectively reduce a variety of challenging behaviours, including aggression, self-injurious behaviour, pica and property destruction, both as independent treatments and in conjunction with other treatments (Matson Reference Matson, Neal and Kozlowski2012). Despite the strong support of differential reinforcement as an effective behavioural treatment, there are some instances in which differential reinforcement procedures can be ineffective. It is essential that differential reinforcement procedures are based on prior functional analyses of the challenging behaviours. If the consequences implemented in a differential reinforcement procedure do not match the maintaining function of the behaviour, then the individual may not experience appropriate reinforcement (Tucker Reference Tucker, Sigafoos and Bushell1998). Differential reinforcement procedures can also be ineffective for challenging behaviours that occur at high rates, such that the behaviour occurs almost continuously and there are few or no opportunities to reinforce the alternative. Additionally, differential reinforcement procedures can be difficult to implement in clinical settings as they require close monitoring of behaviours and timing of intervals (Geiger Reference Geiger, Carr and LeBlanc2010).
Extinction is also a consequence-based intervention that removes reinforcement of a previously reinforced challenging behaviour. For example, extinction procedures for an escape-maintained behaviour (escape extinction) may involve continued presentation of a non-preferred demand or activity while simultaneously eliminating the possibility of escape from the non-preferred demand (Geiger Reference Geiger, Carr and LeBlanc2010). Extinction is commonly combined with positive reinforcement procedures such as differential reinforcement and activity choice (Lipshultz Reference Lipshultz and Wilder2017a). However, extinction procedures alone typically do not immediately reduce challenging behaviours. These procedures also require a high level of monitoring and expert supervision to ensure that the intervention is implemented with integrity, as low integrity could make the behaviour resistant to extinction procedures. Extinction procedures can also result in a burst of responding and high levels of aggression when they are implemented (Geiger Reference Geiger, Carr and LeBlanc2010).
Conclusions
Challenging behaviours occur frequently among children with developmental disabilities. These behaviours can have a negative impact on the children and their families, as they can be associated with increased parental stress, more restrictive educational placements, social stigma and safety concerns. Consequently, it is crucial to correctly identify the function of these behaviours through indirect, descriptive and direct assessment measures to develop appropriate function-based treatment plans. Behavioural interventions are regarded as the primary treatment recommended for reducing challenging behaviours. Several evidence-based antecedent- and consequence-based interventions can be used to reduce challenging behaviours in a variety of settings.
Despite the vast amount of research on challenging behaviours among children with developmental disabilities, questions remain and should be investigated in future research.
Regarding identification, it is essential to detect toddlers and young children at risk for developing severe and chronic challenging behaviours as young as possible. Future research might investigate precursor behaviours that precede the onset of challenging behaviours to allow for early intervention techniques such as functional communication training (FCT). Much of the research on behavioural assessment and intervention has been undertaken in highly specialist services, and not enough is known regarding how effectively they can be implemented in home and school environments. Future research on these behavioural assessment and intervention techniques should aim to increase ecological validity and transferability to naturalistic environments. Although there is a vast amount of research that supports the efficacy of behavioural interventions for children with developmental disabilities, more research is needed on assessment and intervention techniques typically provided. For example, many public education systems in the USA require functional behavioural assessments for children provided services under the Individuals with Disabilities Education Act; however, the content of these assessments varies greatly, often not requiring the use of direct assessment techniques (Lloyd Reference Lloyd and Kennedy2014). Similarly, direct assessment approaches such as experimental functional analysis are more likely to be used in applied clinical settings with a surplus of resources, such as university-based clinics and private schools. Conversely, behaviour ratings scales and checklists are more commonly used to assess challenging behaviours in less well-resourced community settings or developmental centres (Lloyd Reference Lloyd and Kennedy2014). Future research should evaluate the costs and benefits of these alternative approaches to behavioural assessment and intervention planning, especially since treatment failure can ultimately result in individuals with developmental disabilities being admitted to services that are simultaneously more restrictive and costlier than community alternatives.
Author contributions
C.T. wrote the body of the article. J.L.M. wrote the outline and edited the article.
Declaration of interest
None.
MCQs
Select the single best option for each question stem
1 Which of the following is an antecedent strategy used to treat challenging behaviours in children with developmental disabilities?
a extinction
b non-contingent reinforcement
c differential reinforcement of other behaviour
d experimental functional analysis
e antecedent–behaviour–consequence (ABC) recording.
2 Which of the following is not a common challenging behaviour observed in children with developmental disabilities?
a transition-related behaviour
b aggression
c rumination
d property destruction
e non-compliance.
3 Which measure specifically assesses challenging behaviours in toddlers?
a the Behavior Problems Inventory
b the Functional Assessment Screening Tool
c the Aberrant Behavior Checklist
d the Baby and Infant Screen for Children with Autism Traits, Part 3
e the Functional Assessment Interview.
4 Which of the following is not a common consequence strategy used to treat challenging behaviours in children with developmental disabilities?
a differential reinforcement of other behaviour
b punishment
c extinction
d differential reinforcement of incompatible behaviour
e differential reinforcement of alternative behaviour.
5 Which of the following is a common measure used to assess behavioural function in children with developmental disabilities?
a the Behavior Problems Inventory
b the Motivation Assessment Scale (MAS)
c Aberrant Behavior Checklist (ABC)
d Baby and Infant Screen for Children with Autism Traits, Part 3 (BISCUIT-Part 3)
e Developmental Behaviour Checklist (DBC).
MCQ answers
1 b 2 c 3 d 4 b 5 b






eLetters
No eLetters have been published for this article.