LEARNING OBJECTIVES
After reading this article you will be able to:
• understand the complex and two-way causal interactions between substance use and mental illness symptoms or mental disorder
• apply a framework of assessment and formulation for patients with coexisting psychosis and substance misuse
• consider how your approach to assessing coexisting psychosis and substance misuse influences the quality of the information derived from the assessment
A substantial proportion of patients presenting with first-episode psychosis meet the criteria for a substance use disorder diagnosis (Brunette Reference Brunette, Mueser and Babbin2018) and among those with a substance use disorder there is an increased risk of psychotic symptoms (Brown Reference Brown, Kaneko, Donovan, Donovan and Bird2019). The prognosis for people with mental illnesses (including schizophrenia) is markedly worse when there is co-occurring substance misuse (Pinderup Reference Pinderup2018; Khokhar Reference Khokhar, Dwiel and Henricks2018). Despite their greater need, individuals with this mix of problems are more likely to be denied access to appropriate services, which in itself is a plausible contributory factor to the poorer outcomes (Public Health England 2017). Improved approaches to the treatment of patients with a combination of mental illness and substance misuse have been called for (Public Health England 2017). Individualised intervention plans should be based on a formulation of the problems. A necessary condition for a proper assessment and formulation of problems in patients experiencing symptoms of mental illness who use substances is a thorough understanding of the relationship between symptoms/illness and substance use. The way the assessment is undertaken is critical to the quality of information that is derived for use in the process of formulating the problems. It can also have an impact on the patient's engagement with services. This article both describes the complex relationships between mental illness and substance use and presents some practical guidance about how to carry out the assessment of patients with both problems.
Substances are taken to meet needs and acquire benefits (Blevins Reference Blevins, Abrantes and Stephens2016; Patrick Reference Patrick, Bray and Berglund2016). Specific reasons include getting high, relaxing, reducing negative feelings, responding to peer pressure and engaging in a social activity. In a state of active dependence, repeat substance use is also motivated by a desire to avoid or dampen withdrawal symptoms. Mental illness and substance use co-occur more often than by chance and this co-occurrence can be explained in several ways (Dyer Reference Dyer, Easey and Heron2019; Petersen Reference Petersen, Toftdahl and Nordentoft2019). First, using substances increases the risk of symptoms of mental illness via psychosocial or biological processes. Second, symptomatic, psychosocial and neurobiological correlates of mental illness contribute to an increased likelihood of misusing substances. Third, there may be shared risk factors. The different explanations are not mutually exclusive and in many cases there will be multiple and bidirectional effects between mental illness and substance misuse that change over time.
The following exposition of the different ways in which substance misuse and mental illness symptoms may be causally related distinguishes processes as if they were clearly defined and distinct. Although isolating processes may be justified for descriptive purposes, in reality they are overlapping, and it is a better representation of mental processes to conceptualise their causal influence as if they were directional currents rather than distinct vectors. The focus of the article is on psychosis and substance use, although the principles of assessment and formulation apply to co-occurrence of other psychiatric symptoms/disorders with substance use.
Relationship between substance use/misuse and mental illness symptoms/mental disorder
Mental state changes secondary to substance use
The use of an illicit substance usually induces acute mental state changes. These are commonly anticipated and desired. Substance use can also lead to adverse effects on the user's mental state (Table 1). Substances that are commonly associated with psychotic experiences in clinical settings include cannabis, synthetic cannabinoids, stimulants (amphetamines, methamphetamines and cocaine) and hallucinogens (Weibell Reference Weibell, ten Velden Hegelstad, Johannessen and Preedy2016). Psychosis can also occur in association with misuse of inhalants (Mustonen Reference Mustonen, Niemelä and McGrath2018), nitrous oxide (Chien Reference Chien, Huang and Chen2020), ketamine (Huang Reference Huang, Lin, Hashimoto, Ide and Ikeda2020) and steroids (Hall Reference Hall, Hall and Chapman2005).
TABLE 1 Effects of commonly misused substances
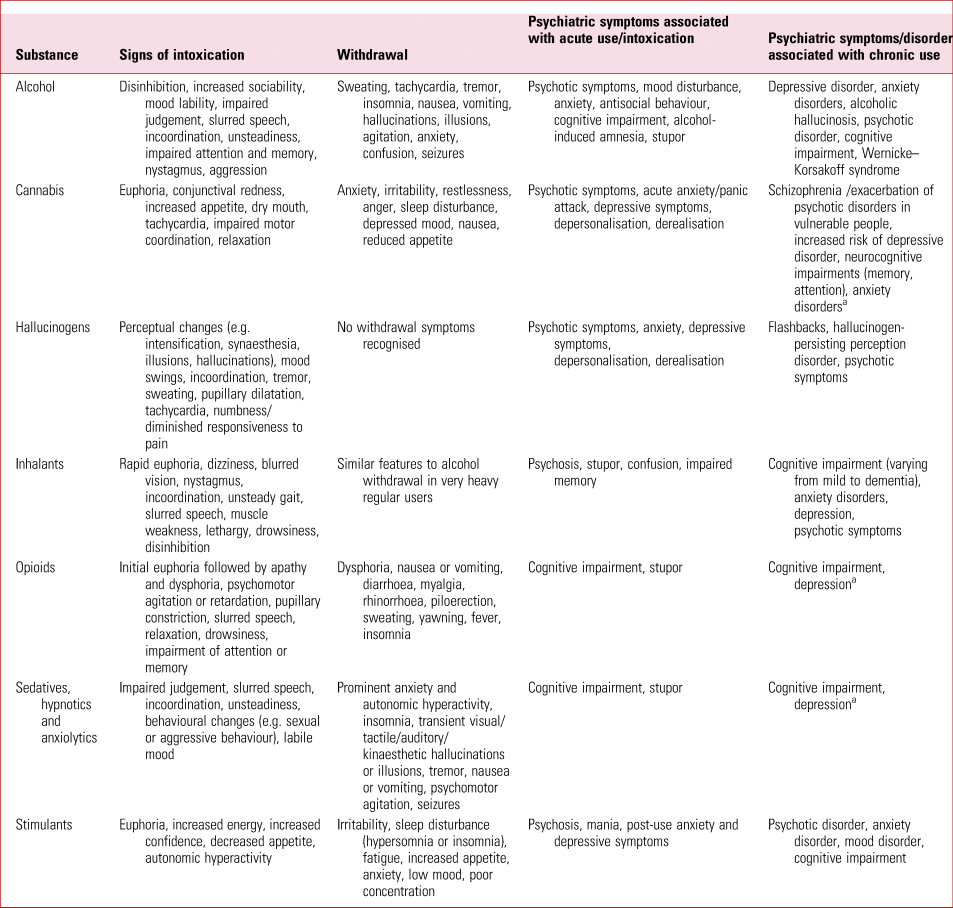
a Reported but the evidence base is inconsistent.
The relationship between alcohol use and psychosis is more complex, since psychotic symptoms are a recognised feature of alcohol withdrawal, hallucinations can develop in chronic use (alcoholic hallucinosis) and there are rare reports of idiosyncratic reactions to acute use in which psychotic symptoms occur (Brown Reference Brown, Kaneko, Donovan, Donovan and Bird2019). Psychotic symptoms can also be a feature of benzodiazepine withdrawal, and they have been reported in acute intoxication with benzodiazepines (Brown Reference Brown, Kaneko, Donovan, Donovan and Bird2019). Acute use of, or withdrawal from, opiods is not generally associated with psychosis (although exceptions have been described) (Freudenreich Reference Freudenreich2020). To the contrary, the available evidence suggests that opioid agonists can have a positive therapeutic effects on psychosis (Maremmani Reference Maremmani, Rovai and Rugani2014, Maremmani Reference Maremmani, Pallucchini and Rovai2020). The explanations for mental state changes secondary to substance use are varied (Table 2).
TABLE 2 Proposed mechanisms explaining adverse mental state changes secondary to substance use/misuse
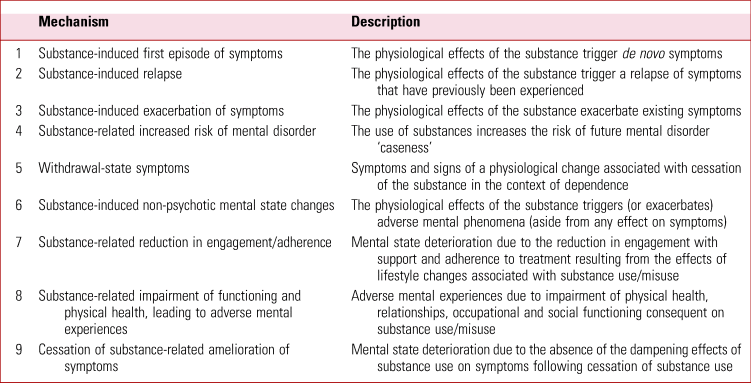
Substance-induced first episode or relapse/exacerbation of symptoms
In addition to triggering a first episode of symptoms in an individual who was symptom free or a relapse in a person with a history of mental disorder, substances may amplify existing symptoms, leading to greater distress and/or dysfunction. Amplification may occur as a result of the direct effects of the substance or because of a more general disinhibiting effect on underlying emotions and urges.
Substance-related increased risk of mental disorder
Aside from immediate effects of substances on an individual's mental state, substance misuse increases the likelihood of subsequently developing schizophrenia (Nielsen Reference Nielsen, Toftdahl and Nordentoft2017). The effects of substances may differ depending on the developmental stage in which the substance is used. For instance, adolescents appear to be more vulnerable to the adverse effects of cannabis and cannabis use in this period may disrupt normal neurodevelopment (Volkow Reference Volkow, Swanson and Evins2016; Oldani Reference Oldani, Grancini, Altamura and Brambilla2019).
It may be assumed that a drug has induced or exacerbated an abnormal mental state if the mental state disturbance arises soon after the substance is taken and resolves once the level of the active metabolites has diminished sufficiently (Ghose Reference Ghose2018). However, it does not necessarily follow that the episode is wholly attributable to the substance, since not all individuals have the same vulnerability to those effects (Engh Reference Engh and Bramness2017). The current evidence suggests that individuals who experience drug-induced psychotic episodes are at an increased risk of developing a psychotic disorder (Alderson Reference Alderson, Semple and Blayney2017; Ghose Reference Ghose2018). Thus, about one-third of patients who experience a drug-induced psychosis go on to meet the criteria for a schizophrenia spectrum disorder or bipolar disorder, not having met the criteria for these diagnoses before (Ghose Reference Ghose2018). Further, there is recent evidence of a shared familial and genetic risk between drug-induced psychosis and schizophrenia. Therefore, rather than drug-induced psychosis being conceived of as a stand-alone entity, it is better represented as a manifestation of an underlying vulnerability and a potential risk indicator for a future psychotic illness (Ghose Reference Ghose2018).
Substance-induced non-psychotic mental state changes
As well as increasing the likelihood of psychotic symptoms, substance use often triggers non-specific unpleasant mental state changes (such as negative affect or dissociative experiences). These lead to increased stress, which is a risk factor for worsening of pre-existing symptoms and/or may reduce tolerance to symptoms. Cognitive impairment associated with substance misuse can further complicate the clinical presentation (Toledo-Fernández Reference Toledo-Fernández, Brzezinski-Rittner and Roncero2018).
Substance-related impairment of functioning and physical health, leading to negative mental experiences
An individual who is misusing illicit substances is at increased risk of non-adherence with treatment and disengagement from support services, leading to reduced mental stability (Dixon Reference Dixon, Holoshitz and Nossel2016; Foglia Reference Foglia, Schoeler and Klamerus2017). Substance misuse, particularly if regular, increases the likelihood of physical ill health (e.g. liver disease) and social, occupational and relationship problems, which in turn may be associated with distress and mental health problems (Hall Reference Hall, Patton and Stockings2016). The latter can be manifest in the form of a first episode of mental illness or the destabilisation of an existing mental illness.
Cessation of substance-related amelioration of symptoms
In rare cases, the cessation of substance use may lead to a deterioration in the patient's mental functioning. For example, there have been reports (and R.N. has clinical experience) of patients with psychosis who have reported a reduction in symptoms while taking opioids going on to experience a persistent relapse with onset soon after they start abstaining (Cobo Reference Cobo, Ramos and Peláez2006). For this reason, close monitoring is recommended for patients with coexisting psychosis and substance misuse for whom withdrawal of opioid substitution treatment is planned.
Substance use secondary to mental state/functioning characteristics
The direction of causality can also run from mental health factors to substance use and misuse (Table 3). Self-medication is a commonly reported explanation for substance use secondary to mental state disturbance (Torres Reference Torres, Papini and Preedy2016). It includes a pattern of taking the substance with the intention of reducing symptom intensity and/or symptom-related distress. This may be via a direct effect on symptoms (which include withdrawal symptoms) or an indirect effect by making the individual less distressed or concerned about the symptoms. This article focuses on psychotic symptoms co-occurring with substance misuse, but it is important to remember that other mental health problems (e.g. attention-deficit hyperactivity disorder and post-traumatic stress disorder) may increase the propensity to use (or misuse) substances (Head Reference Head, Goodwin and Debell2016; Groenman Reference Groenman, Janssen and Oosterlaan2017; Mergler Reference Mergler, Driessen and Havemann-Reinecke2018).
TABLE 3 Proposed mechanisms explaining substance use/misuse secondary to mental state disturbance
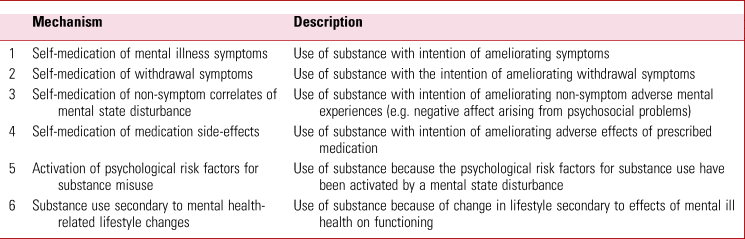
The term self-medication can be extended to include a broader range of reasons for substance use as a consequence of mental state disturbance. For example, substance use may be motivated by a desire to reduce negative affect secondary to non-symptom consequences of the mental disorder such as social and interpersonal problems (Fresán Reference Fresán, Robles-García, Tovilla-Zarate, Compton and Manseau2018). Also, substances may be taken with the intention of ameliorating the side-effects of psychotropic medication. Substance use in response to antipsychotic-induced dysphoria is one suggested mechanism for which there is some empirical support (Awad Reference Awad and Preedy2016).
Mechanisms other than self-medication have been presented to explain the increased propensity for drug use among people with schizophrenia. Impulsivity and its subfacet, negative urgency (a tendency to act rashly in negative affect states), which are risk factors for substance misuse (Smith Reference Smith and Cyders2016; D'Agostino Reference D'Agostino, Peterson and Smith2019), have been found to be increased in schizophrenia (Hoptman Reference Hoptman and Ahmed2016). Recent studies point to the possibility that neurobiological changes in schizophrenia increase proneness to substance misuse (Dyer Reference Dyer, Easey and Heron2019; Petersen Reference Petersen, Toftdahl and Nordentoft2019).
Shared risk for psychiatric disorder and substance misuse
There is empirical evidence for shared genetic risks across different psychiatric diagnostic categories, including alcohol and drug misuse (Carey Reference Carey, Agrawal and Bucholz2016; Pettersson Reference Pettersson, Larsson and Lichtenstein2016). More specifically, substance misuse and schizophrenia have been shown to have a shared genetic liability (Hartz Reference Hartz, Horton and Oehlert2017). If such liability is manifest initially in adolescent substance use, this use may increase the vulnerability to both later substance misuse and psychosis (Khokhar Reference Khokhar, Dwiel and Henricks2018), illustrating the interactive and dynamic nature of the relationship between substance use and psychosis.
Similarly, stress (arising from early adversity and/or more recent life events) is both a shared risk factor for psychosis and substance use (Mizrahi Reference Mizrahi2016; Valentino Reference Valentino2019; Kisely Reference Kisely, Mills and Strathearn2020) and a risk factor that may, in combination with substance use, cumulatively increase the risk of psychosis (Arranz Reference Arranz, Monferrer and Algora2018). A history of multiple acute and chronic adverse experiences over the life course (e.g. trauma, deprivation, homelessness, loss and abandonment) may compromise mental health and personality functioning over and above the increased risk of psychosis and substance misuse (Padgett Reference Padgett, Smith and Henwood2012).
It has been proposed that individuals who are at risk of antipsychotic-induced dysphoria (which is a risk factor for self-medication with substances) are also at increased risk of substance misuse, indicating a very specific type of shared risk underpinning coexisting psychosis and substance misuse (Awad Reference Awad and Preedy2016). Certain personality traits (such as neuroticism) have been found to be associated with both schizophrenia and substance misuse (Ohi Reference Ohi, Shimada and Nitta2016; Rogers Reference Rogers, McKinney and Asberg2018).
Assessment approach for coexisting psychosis and substance misuse
The assessment of patients with co-occurring psychiatric psychopathology and substance use should be informed by a recognition of the potential complexities in the relationship between substances and symptoms (Avery Reference Avery and Barnhill2017; Givon Reference Givon, Donovan and Bird2019). It follows from the earlier description of the multiple and bidirectional explanatory processes that the oft-assumed categorical dichotomy between, on the one hand, a substance-induced mental/behavioural condition and, on the other hand, a so-called primary mental illness that coexists with (but is not caused by) substance use is in many cases likely to be a gross oversimplification. Questions have even been raised about whether the reductionist basis of the term dual diagnosis misleads the clinician into seeing a straightforward relationship between substance use and mental illness where it usually does not exist (Pycroft Reference Pycroft, Green and Winstone2016). A pictorial representation of the problem (such as that presented in Fig. 1) can help the clinician keep in mind the dynamic nature of the relationship between use/misuse and symptoms/disorder.
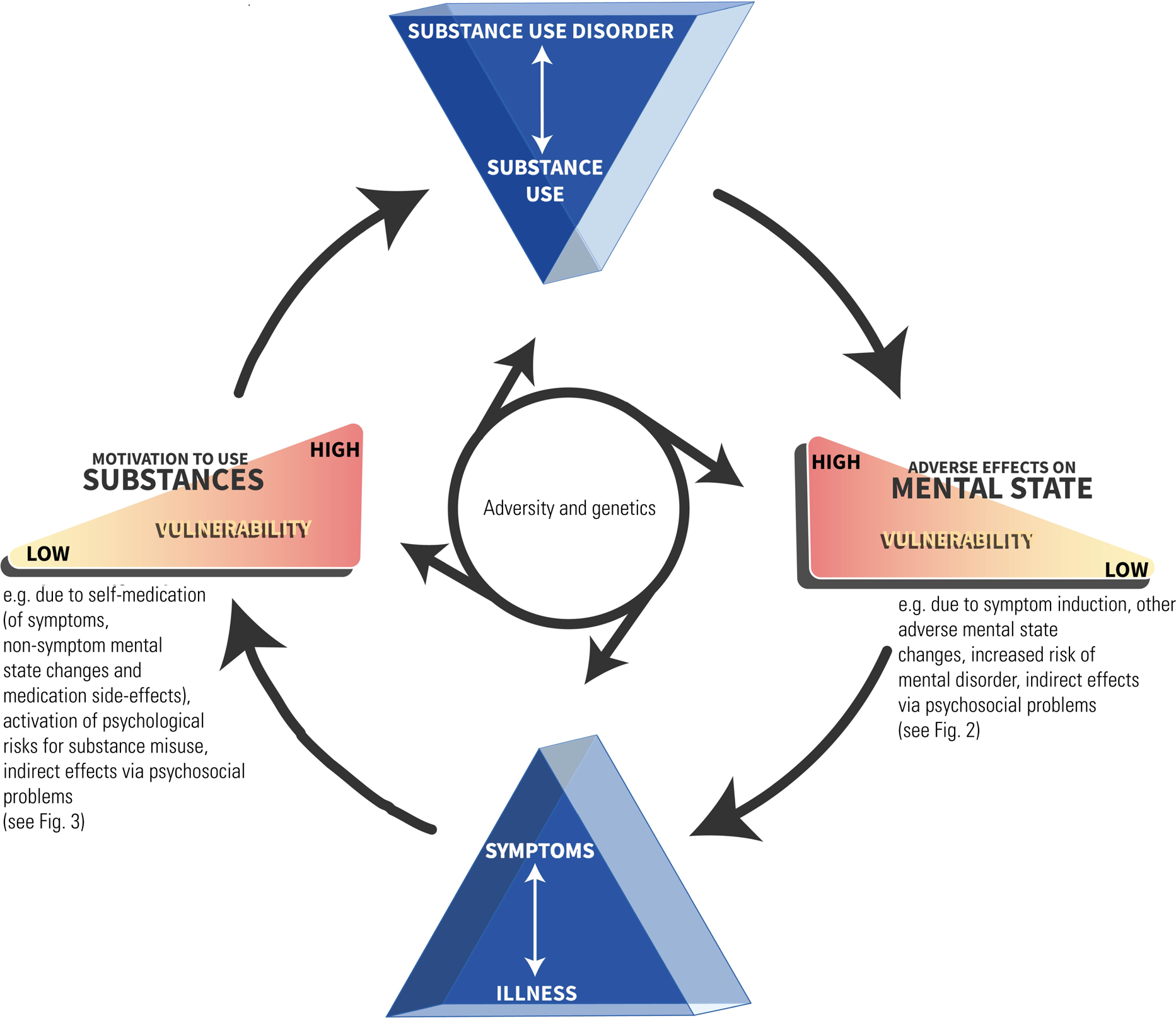
FIG 1 Pictorial representation of the interaction between substance use/misuse and mental illness symptoms/disorder.
The second implication of accepting the complexity is that even a thorough assessment may not lead to an unambiguous depiction of the nature of the relationship (Ghose 2018; Brown Reference Brown, Kaneko, Donovan, Donovan and Bird2019). Nevertheless, the clinician should endeavour to explore for the different mechanisms that explain the relationship, so that an informed formulation can guide the best clinical approach.
Building a longitudinal account of the relationship over time between substance use and mental illness symptoms may shed some light on directions of causality (Givon Reference Givon, Donovan and Bird2019). The prototypical drug-induced picture (which is accounted for by explanatory processes 1, 2 and 3 in Table 2) comprises a clear sequence from drug use to onset or worsening of symptoms and then symptom remission following drug abstinence. However, if there is an opportunity for a comprehensive assessment in everyday practice, such a picture often still does not come into clear focus. This may be because the complex bidirectional influences that are commonly present in the same patient confound such a straightforward unidirectional formulation. The clinician's focus on ‘what came first’ can come to unhelpfully dominate the assessment, at the expense of understanding the patient's needs (Hawkins Reference Hawkins and Gilburt2004). However, it is essential to identify those occasional cases where there appears to have been a discrete time-limited episode of symptoms following the use of a substance that is known to induce psychosis.
Research into the differences between substance-induced conditions and primary mental illness has found evidence of substantial overlap of psychopathology (Pauselli Reference Pauselli, Compton and Manseau2018; Wearne Reference Wearne and Cornish2018), suggesting that symptom profile alone has limited value in delineating the explanatory formulation.
A good theoretical understanding of the topic under consideration and the collation of as much relevant information as possible are necessary conditions for any psychiatric assessment, but they are not sufficient. Attention must also be paid to subjective aspects of the assessment process, particularly for patients who are at risk of being excluded from services (Green Reference Green and Pycroft2019). Stigma, negative attitudes and the nature of the relationship between practitioners and patients are all potential barriers impeding access to appropriate services for patients with coexisting psychosis and substance misuse. To reduce the potential effect of these factors, as well as developing an improved explicit understanding of coexisting psychosis and substance misuse, clinicians should reflect on how certain implicit processes may influence their therapeutic stance and approach to formulation. Of particular importance to clinical scenarios where co-occurring problems interact with each other (such as in coexisting psychosis and substance misuse) are implicit causal assumptions that influence the clinician's judgements about the nature of the interaction between the problems.
Biased causal assumptions
An innate predisposition to understanding cause and effect can be traced to the survival advantages of the consequent ability to make anticipatory evaluations of one's environment and, specifically, to make general predictions about future events (Stuart-Fox Reference Stuart-Fox2015). Although making sense of the complex interrelationship between a large array of events draws on explicit reasoning processes, humans have an innate tendency to implicitly generate causal representations (Muentener Reference Muentener and Schulz2014). Such implicit causal reasoning processes provide an estimate to guide immediate action, but they are prone to produce erroneous conclusions in the face of complex data. Since the causal inferences can occur in the moment without the opportunity for reflective analysis, the underlying processes are more likely to be implicit or at least to rely on pre-existing explanatory paradigms.
Clinical experience suggests that practitioners are particularly vulnerable to making assumptions that favour a formulation involving a causal chain from drug use to mental illness symptoms (often informally described as ‘drug-induced’). The notion of ‘drug-induced psychosis’ is not only overly simplistic, but the way that it is used in practitioners’ explanatory narratives can give the impression that the psychotic symptoms have a lesser status in comparison with psychotic symptoms that are not seen to be causally related to substance use (Wilson Reference Wilson, Shaw and Williams2017). Another common causal inference assumes that the patient's motivation to attend for assessment is linked to an underlying desire to obtain more substances (prescribed substances in this scenario) (so-called ‘drug-seeking’). These types of causal assumption contribute not only to the clinician's interpretation of the patient's responses to questions, but also to the approach to questioning adopted by the clinician. Thus, the clinician is prone to seek out and pay attention to information confirming their biased assumptions. It is not just a matter of the choice of questions and therefore the answers being influenced by a confirmatory bias. Patients’ feedback in clinical settings indicates that they often recognise clinicians’ biases and sometimes they respond in a way that interferes with the assessment. Examples of responses by patients include emphasising a narrative contrary to the one being suggested by the clinician, expressing frustration and/or disengaging from the process. Although understandable, they may be interpreted by the clinician as further evidence in favour of their preconceptions. For instance, if a patient responds oversensitively to a pattern of questioning that appears to be focusing on one causal explanation at the expense of other explanations (such as a drug-induced condition as opposed to an underlying mental illness), the clinician may take this as evidence that the person lacks insight that the ‘real’ problem is their drug use or that they are trying to exaggerate or even feign mental illness symptoms. The patient may, at the same time, interpret the clinician's approach as invalidating, since whatever the causal explanation, to them the symptoms are also a ‘real’ problem. Reaching an informed opinion about the nature of the relationship between substance use and symptoms is likely to be made more difficult by an assessment dynamic in which the clinician is revealing their biases in a way that may provoke a negative response from the patient.
Assessment model
A number of steps can be taken to reduce the influence of pre-existing causal assumption biases on the assessment process and the quality of the therapeutic relationship (Box 1).
BOX 1 Principles of assessment and formulation for patients with coexisting psychosis and substance misuse
• Use a vulnerability/dimensional model of psychopathology in developing an explanatory formulation
• Remain mindful of the complexity of the relationship between substance use and psychiatric symptoms
• Develop an awareness, and resist the interfering influence, of the distorting effect of implicit causal reasoning processes on assessment and formulation
• Adopt an overt and genuine ‘not knowing’ approach to assessment
• If a clear explanatory formulation does not emerge from the assessment, tolerate uncertainty
First, a model of understanding that relies on the notions of vulnerability to, and the dimensional expression of, psychopathology facilitates a more nuanced explanatory formulation of psychiatric symptoms that co-occur with substance use (Szerman Reference Szerman, Parro-Torres, Didia-Attas, Javed and Fountoulakis2019). In such a model, psychiatric symptoms are seen as a reflection of a vulnerability to developing this type of psychopathology. Approaching the assessment using a framework of the dimensional expression of psychopathology not only is more consistent with the empirical evidence (Ayhan Reference Ayhan, McFarland and Pletnikov2016), but it also encourages attention to symptoms even if it is not possible to be clear about diagnosis. Thus, although active substance misuse may make a definitive diagnosis difficult, it should not be the basis of rejecting the possibility that there is an underlying vulnerability that may be manifest in symptoms even if abstinence were achieved. Removing the pressure to definitively decide whether or not there is a diagnosable mental disorder and focusing on exploring the nature and degree of symptoms allows a more considered approach to exploring the relationship between symptoms and substance use and reduces the risk of patient disengagement. This dimensional approach to the assessment does not preclude a categorical approach to decision-making, such as whether to commence a treatment or refer to a service. Where such a decision needs to be made, this can be done using the best-fit formulation at the time of the decision, while at the same time acknowledging, if necessary, that the formulation is provisional and should remain under review in light of ongoing assessments (Brendel Reference Brendel2003). The dimensional framework also allows problems on different dimensions (such as substance misuse and mental illness symptoms) to be addressed even if it is not possible to reduce the relationship to either a simple drug-induced condition or mental illness.
Second, the clinician should retain an awareness of the potential for the multiple, changing two-way interactions between substance use and symptoms in the same patient (Fig. 1).
Remaining mindful of the complexity of the relationship between substance use and psychiatric symptoms helps with the application of the third element of this model: the clinician should reflect on and resist the influence of their own biased causal representations of the relationship between substance use and mental disorder. These may comprise a tendency to apply oversimplified explanations (such as those relying on the false dichotomy between mental illness and a drug-induced condition) and/or to favour certain causal narratives. As already noted, the narratives that involve substances having a primary causal role appear to be widely prevalent, despite the empirical evidence suggesting a more complex explanation even for those cases where there appears to be a temporal sequence involving substance use first, followed by symptoms.
Fourth, clinicians should represent their open-mindedness overtly in assessment. Adopting a ‘not knowing’ stance in which the clinician remains genuinely curious reduces the constraining influence of predetermined theoretical explanations that the patient may experience as invalidating, with negative consequences for the quality of both the interaction and the information arising from it (Anderson Reference Anderson, Goolishian, McNamee and Gergen1992).
Fifth, if a clear explanatory formulation does not emerge from the assessment (which, in light of the potential for complexity, should not be a surprise), the clinician should be able to tolerate uncertainty rather than imposing unwarranted certainty (Brendel Reference Brendel2003). As already highlighted, if it is necessary to make a decision while there is still uncertainty, the clinician may indicate their preferred formulation on the basis of the available information and advise that the formulation should remain under review.
Management considerations
A comprehensive review of models of treatment for patients with coexisting psychosis and substance misuse is beyond the scope of this article, but in general the approach to management should involve collaborative care planning, attention to physical health and wider social needs, partnership working between health and other support services, adaptation of specialist mental health services for the needs of patients with coexisting psychosis and substance misuse, psychologically informed approaches and the avoidance of excluding these patients from specialist mental health services because of substance misuse (National Institute for Health and Clinical Excellence 2016; Crockford Reference Crockford and Addington2017; Baker Reference Baker, Denham, Pohlman, Badcock and Paulik2020).
With specific reference to pharmacological treatment of psychotic symptoms, it is worth noting that standard treatments used in non-comorbid patient groups may not be appropriate for patients with coexisting psychosis and substance misuse. For instance, maintenance treatments for opioid dependence are sometimes preferable to abstinence-based treatments, which may destabilise individuals with comorbid psychosis and substance misuse. It should be noted, though, that methadone can induce QTc prolongation, as can many psychiatric drugs, so patients with comorbid conditions need extra monitoring for this complication, and medications that are more likely to induce QTc prolongation should be avoided if possible. Individuals who misuse substances are at increased risk of hepatic disease (due to, for example, hepatitis C and the toxic effects of alcohol), resulting in a greater potential for medication toxicity.
There are also specific additional risk considerations in this group. For example, parental mental health problems and substance misuse, together with domestic violence, make up the so-called ‘toxic trio’ for childhood maltreatment (Brandon Reference Brandon, Bailey and Belderson2009). People with coexisting mental problems and substance misuse are at increased risk of being targeted by dealers’ attempts to infiltrate provincial towns (known as ‘county lines’ dealing) through processes such as ‘cuckooing’ (in which a dealer takes over premises for use as a provincial base for drug dealing) (Coomber Reference Coomber and Moyle2018; Williams Reference Williams and Finlay2019).
Conclusions
When developing a formulation of the problems experienced by a patient with symptoms of mental illness who uses substances, the practitioner needs to keep in mind the complex interrelation between substance use and mental illness symptoms. There are three types of high-level explanation: (a) substance use adversely affects mental state; (b) mental state disturbances increase the likelihood of substance use; and (c) shared factors increase the risk of both substance misuse and mental illness. Each of these types of causal relationship may be accounted for by a combination of different mechanisms, which can act in different directions and take effect directly and indirectly. It may be difficult to unpick the exact configuration of explanatory processes in a single case, but the assessment is more likely to contribute to a valid formulation if the clinician recognises the potential for complexity, is able to tolerate uncertainty and addresses any biased causal assumptions they hold in relation to explaining coexisting psychosis and substance misuse. A model in which the occurrence of symptoms is taken to be an indication of vulnerability to that type of psychopathology and the expression of those symptoms is seen to occur on a dimension (from a diagnostically subthreshold form to one that allows the diagnostic criteria to be met) not only is more in keeping with the empirical evidence base, but also facilitates formulation and clinical decision-making in cases where there is coexisting psychosis and substance misuse.
Author contributions
Both authors contributed substantially to the conception, writing and final manuscript.
Declaration of interest
None.
ICMJE forms are in the supplementary material, available online at https://doi.org/10.1192/bja.2020.45.
MCQs
Select the single best option for each question stem
1 Patients presenting for the first time with psychosis in the context of drug misuse:
a very rarely go on to meet the criteria for a schizophrenia spectrum disorder or bipolar disorder
b are experiencing symptoms that can be wholly attributable to the substances taken
c are at an increased risk of developing a psychotic disorder
d are no more vulnerable to psychosis that individuals who misuse substances without developing psychosis
e can be assumed to be suffering from drug-induced psychosis.
2 The following substances commonly trigger psychotic experiences, except:
a cannabis
b cocaine
c LSD
d amphetamines
e heroin.
3 As regards explanations for co-occurrence of mental illness and substance use, which of the following statements is false?
a the relationship between mental illness and substance use can change over time
b the different explanations are not mutually exclusive
c the relationship can be bidirectional
d the relationship is always straightforward and unidirectional
e the interactions between the mental illness and substance use are multiple and complex.
4 Of the following, which describes the most typical profile of symptoms in alcohol withdrawal?
a diarrhoea, myalgia, rhinorrhoea, piloerection, yawning and insomnia
b there is no recognised withdrawal syndrome
c fatigue, increased appetite, anxiety and low mood
d sweating, tachycardia, tremor, insomnia, vomiting, hallucinations, anxiety and seizures
e disinhibition, increased sociability, nystagmus, slurred speech.
5 The recommended assessment model for patients with co-occurring substance use and psychopathology includes:
a concentrating exclusively on diagnosable disorders
b exploring the relationship between symptoms and substance use in an overtly open-minded manner
c establishing what came first to decide whether there is a primary mental illness
d assuming until otherwise disproven that the psychosis is caused by the substance use
e relying on pre-existing causal assumptions.
MCQ answers
1 c 2 e 3 d 4 d 5 b








eLetters
No eLetters have been published for this article.