LEARNING OBJECTIVES
After reading this article you will be able to:
• identify and assess the different types of eating disorder, and be aware of core clinical signs and symptoms
• confidently manage the physical and psychological consequences of eating disorders in accordance with current evidence-based guidelines
• understand current controversies in the field and evolving research themes.
Traditionally, the ‘eating disorders’ have been characterised by intense fear of gaining weight, although DSM-5, (American Psychiatric Association 2013) omitted fear of weight gain from criteria for binge eating disorder and some childhood eating disorders.
Far more than eating behaviour is disordered. Starvation, and consequences of purging and overexercise, cause psychosocial and physical damage. Anorexia nervosa has the highest mortality rate of all psychiatric disorders (Franko Reference Franko, Keshaviah and Eddy2013). Behavioural and psychotherapeutic approaches are the mainstays of treatment.
This review summarises the current state of the specialty, covering eating disorders characterised by preoccupation with weight, shape and calorie balance. Disordered eating behaviour stemming from autistic, affective or other underpinnings warrants a separate review.
Contemporary models of eating disorders
Clinicians commonly hold an ‘illness model’ of eating disorders, whereas lay people, journalists and patients, particularly on social media, may assume that eating disorders represent a lifestyle choice. Charland and colleagues proposed that anorexia nervosa be considered a ‘passion’ – an overriding affect-laden philosophical priority (Charland Reference Charland, Hope and Stewart2013). This notion is fruitful in suggesting that treatment should ‘fight passion with passion’.
Others emphasise endemic ‘eating-disordered’ symptoms in society, stressing the role of physiological dysregulation in perpetuating restriction–binge–purge cycles. Proponents of family-based treatment (FBT) (Lock Reference Lock and Le Grange2015) observe that early refeeding alone treats many teenagers with anorexia nervosa. Such diverse opinion suggests heterogeneity despite many common features. Clinicians who address only physical disruptions are unlikely to engage their patients or provide alternative coping strategies, whereas those who neglect physiological maintaining factors may inadvertently perpetuate chronicity.
Diagnostic classification
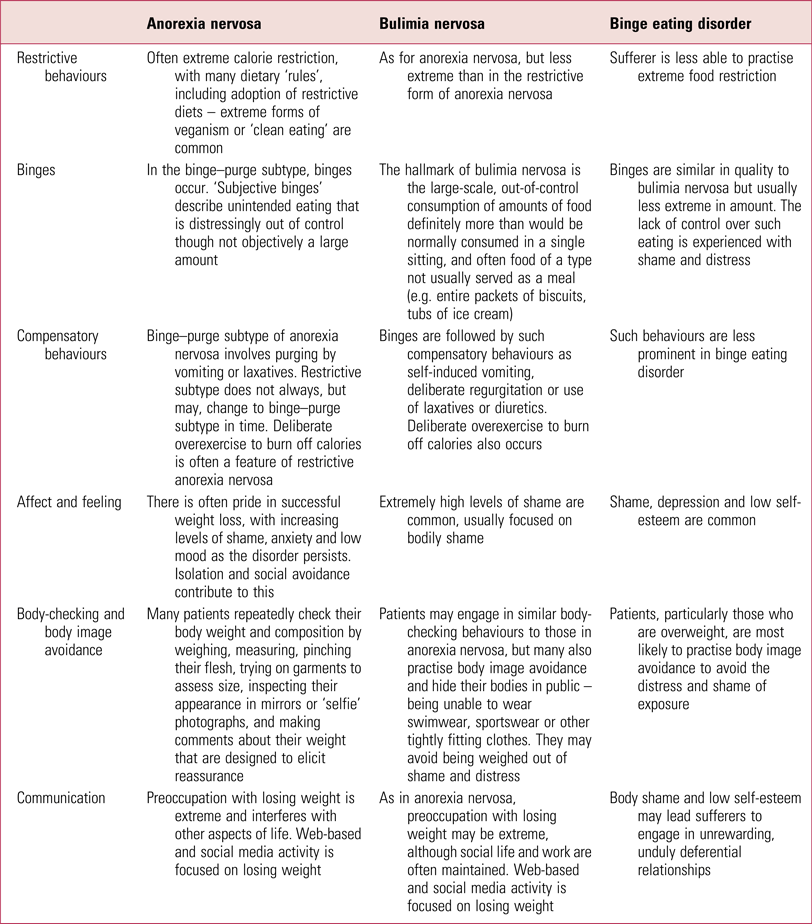
Eating disorders share features of preoccupations and behaviours aimed at weight loss (Table 1). Both DSM-5 and ICD-11 (World Health Organization 2018) discriminate between anorexia nervosa and bulimia nervosa on the basis of weight. The hallmark of anorexia nervosa is significant weight loss, whereas those who are not underweight are diagnosed as having bulimia nervosa if they purge (induce vomiting or use laxatives) but binge eating disorder if they ‘binge’ without purging. Anorexia nervosa has existed for centuries, but bulimia nervosa appeared in the later 20th century. Binge eating disorder is an even more recent phenomenon. Adult eating disorder services specialise in disorders sharing the core psychopathology of preoccupation with weight and shape.
TABLE 1 Main features of the eating disorders
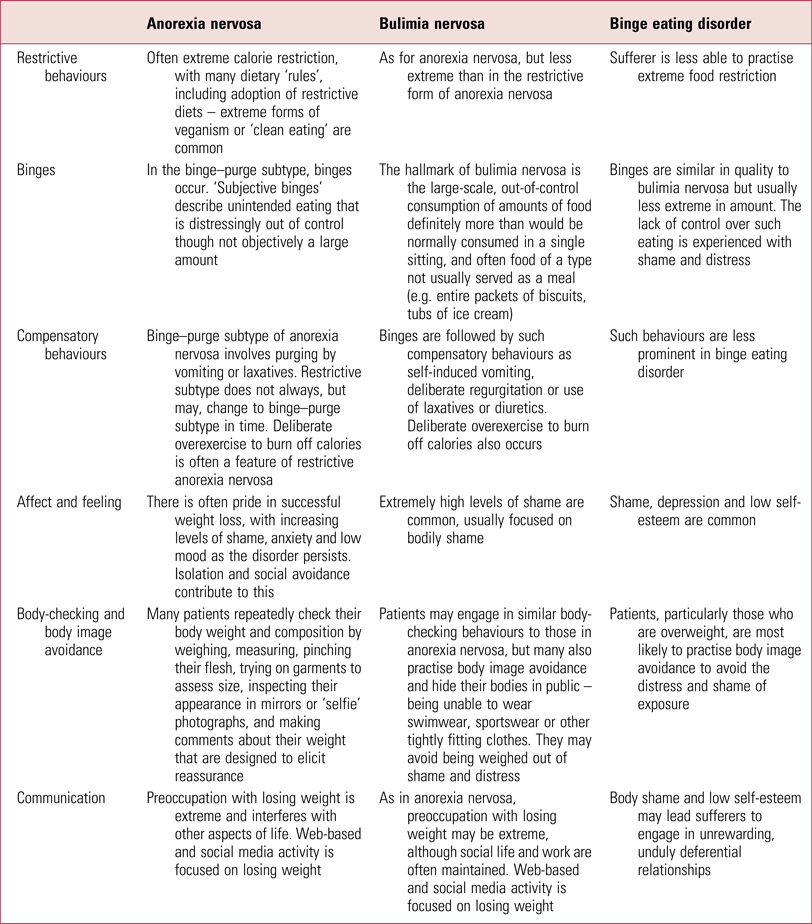
Psychiatric classifications are limited by reliance on symptoms, whereas research is hampered by inaccurate diagnostic groupings. Treatment evidence is inextricably tied to existing categorisation. Clinicians should remember that a patient's failure to precisely meet listed criteria does not automatically exclude an eating disorder. Moreover, patients’ diagnoses commonly migrate across categories during the course of illness.
Epidemiology
Eating disorders typically begin in early to mid-adolescence, but can emerge at any age (Nicholls Reference Nicholls, Lynn and Viner2011; Steinhausen Reference Steinhausen and Jensen2015; Micali Reference Micali, Martini and Thomas2017). Lifetime prevalence of anorexia nervosa in the general population in Western countries is about 1% among women and 0.5% among men. Gender distribution is less skewed in children. Adolescents have higher rates of full recovery and lower mortality than adults (mean mortality 2 v. 5%).
A recent Scandinavian register-based study (Reas Reference Reas and Ro2018) found that, for both genders aged 10–49 years, incidence rates of anorexia nervosa were stable across the 7-year period to 2016, at 18.8–20.4 per 100 000 for narrowly defined and 33.2–39.5 per 100 000 for broadly defined anorexia nervosa. There was a significant annual increase in anorexia nervosa among 10- to 14-year-old girls. Overall rates of bulimia nervosa declined.
Register-based studies substantially underestimate true community prevalence, and it is reported that half of those who meet diagnostic criteria in the community do not access treatment. Not receiving treatment is even more likely in low- and middle-income countries, now seeing increased prevalence of formerly ‘Western’ disorders.
Risk factors
Genetics
Early family studies, large twin-based studies and smaller adoption studies demonstrate both a heritable component and significant influence of non-shared environmental factors in eating disorders. There is a strong familial component to anorexia nervosa, with estimates of heritability between 28 and 74%. The genetic contribution is polygenic. Large genome-wide association studies (GWAS) highlight the need to consider psychiatric and metabolic mechanisms involved in anorexia nervosa (Watson Reference Watson, Yilmaz and Thornton2019). These studies, together with further research in the genetics of bulimia nervosa and binge eating disorder, may help elucidate new avenues of treatment.
Gene–environment interactions are complex. Recent work on gut microbiota has found reduced gut microbial diversity in anorexia nervosa, significantly associated with depression, anxiety and eating disorder symptoms (Kleiman Reference Kleiman, Watson and Bulik-Sullivan2015).
Structural and functional brain abnormalities
Neuroimaging often disappoints in revealing structural and functional abnormalities (Frank Reference Frank, Favaro and Marsh2018). Studies in anorexia nervosa may reflect consequences of starvation rather than the psychiatric disorder. Re-scans at normal weight cannot assume that brain nutrition is fully restored or that damage is reversible, although studies suggest that some brain tissue abnormalities recover with weight regain.
Reward and satiety circuits in the orbitofrontal cortex are important in both anorexia nervosa and bulimia nervosa. Structural magnetic resonance imaging has revealed that individuals with anorexia nervosa had increased right insula grey matter compared with controls (Frank Reference Frank, Favaro and Marsh2018). This area is associated with self-recognition and interoceptive awareness. Prospective studies may explore whether these changes are biomarkers or sequelae.
Functional imaging, with symptom provocation, suggests abnormal responses in subcortical regions associated with stimulus-driven responses, and in prefrontal regions involved in evaluation and executive control (Kaye Reference Kaye, Wierenga and Bailer2013). Abnormalities in reward circuit activation have also been found in anorexia nervosa (Monteleone Reference Monteleone, Castellini and Volpe2018).
In anorexia nervosa the observed rigid thinking, poor central coherence and emotional avoidance may improve, at least partially, with re-nutrition (refeeding), but may persist and may also be observed in unaffected relatives (Kanakam Reference Kanakam and Treasure2013; Lang Reference Lang, Lopez and Stahl2014).
Different eating disorders show different abnormalities of attentional bias. In bulimia nervosa and binge eating disorder there is increased attentional bias towards food-related cues, whereas individuals with anorexia nervosa have increased attentional bias towards disliked aspects of body image (Stojek Reference Stojek, Shank and Vannucci2018). This could guide specific interventions for different disorders.
Sociocultural factors
A prospective study of healthy adolescent girls (Stice Reference Stice, Gau and Rohde2017) found that impaired interpersonal functioning and negative affect were transdiagnostic risk factors. Pursuit of the thin ideal, body dissatisfaction, dieting and unhealthy weight-control behaviours increased risk for bingeing and purging disorders. Inherently lean girls, even if not pursuing the thin ideal, were at risk for anorexia nervosa.
The increase in eating disorders in lower-income societies follows Western lifestyle aspirations, nutritional habits and internalisation of the thin ideal. Sociocultural pressures appear more powerful in triggering bulimia nervosa and binge eating disorder than anorexia nervosa but may also trigger genetically vulnerable individuals to try to lose weight.
Childhood deprivation and trauma are important risk factors for many mental disorders and appear to be associated with increased risk of bulimia nervosa and binge eating disorder, but not anorexia nervosa (Larsen Reference Larsen, Munk-Olsen and Bulik2017).
Anorexia nervosa and bulimia nervosa are more common among females than males (Hoek Reference Hoek2006) and there are higher rates of disordered eating among sexual minorities, particularly transgender people (Calzo Reference Calzo, Blashill and Brown2017).
Social media use and competitiveness can maintain and perhaps trigger eating disorders (Ferguson Reference Ferguson, Munoz and Garza2014; Mabe Reference Mabe, Forney and Keel2014). Treatment and prevention strategies might benefit from identifying differences between helpful and harmful behaviour online and in social media.
Prevention
A large number of prevention programmes are under development and evaluation. The most promising interventions use cognitive dissonance, cognitive–behavioural therapy (CBT) and media literacy. Although prevention programmes generally improve participants’ knowledge, and sometimes reduce risk factors, there is no evidence that they actually reduce development of diagnosable eating disorders.
Combined preventive approaches developed by eating disorder and obesity experts might avoid inadvertent triggering of disorders by focusing on the dangers of either extreme. Parent and carer groups regularly report onset of eating disorders following anti-obesity campaigns in schools.
Assessment of symptoms and risk
Prompt referral and treatment is important. Specialist intervention in the first 3 years gives the best prognosis (Stice Reference Stice, Gau and Rohde2017) and evaluation of a novel service in the UK – the First Episode and Rapid Early Intervention for Eating Disorders (FREED) service – suggests that early treatment of young adults reduces the need for later, more costly interventions (Fukutomi Reference Fukutomi, Austin and Mcclelland2020).
Signs and symptoms
Signs and symptoms of eating disorders should be positively elicited by sympathetic enquiry. Individuals often present with physical symptoms – weight loss, weakness, fainting, constipation, nausea and amenorrhoea – or psychiatric symptoms such as depression and anxiety. The need to exclude organic causes should not delay assertive re-nutrition, particularly in younger patients. Any organ system may be affected, and Table 2 lists possible signs and symptoms.
TABLE 2 Possible signs and symptomsa
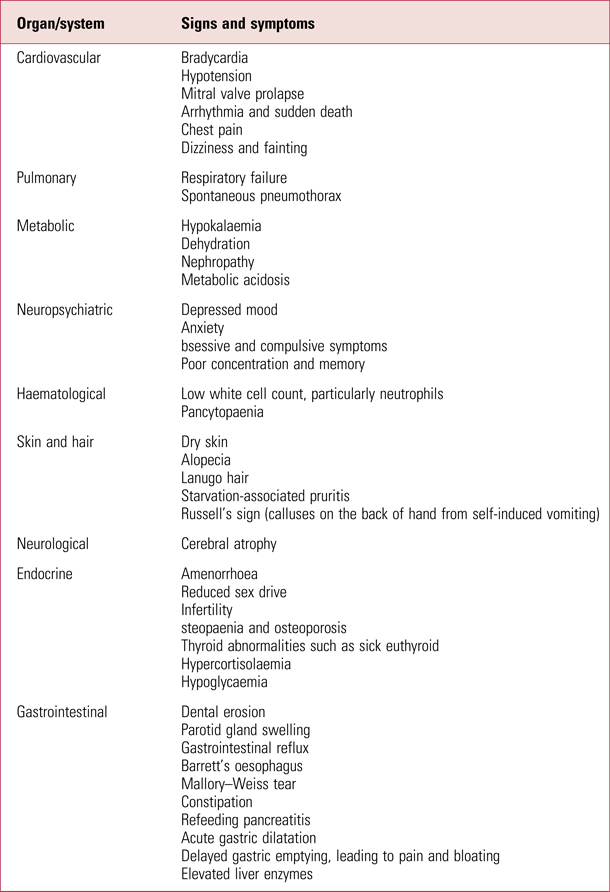
a. Note that any organ system can be affected by an eating disorder and this list is not exhaustive.
Psychosocial disorder may be assessed by asking the patient, or better still a friend or relative, to describe a typical day. The Eating Disorder Examination Questionnaire (EDE-Q) (Fairburn Reference Fairburn and Beglin1994) is the gold-standard validated self-report questionnaire and is available free of charge. Widely used standard measures may be used to assess quality of life, anxiety and depression. The Clinical Impairment Assessment (CIA) questionnaire (Bohn Reference Bohn, Doll and Cooper2008) assesses clinical severity.
Physical investigations
Blood tests may reveal the low white cell count of starvation and deranged liver function (starvation or substance use). At any weight there may be physical evidence of purging (e.g. low potassium) or of the ‘fluid loading’ in which many patients engage to fill their hungry bellies or to disguise their weight. Overhydration can cause low sodium levels and low gravity in urine samples. Electrolyte derangements may cause cardiovascular irregularities, seizures and even permanent damage. Asymptomatic low glucose levels in starved patients are less worrying than often feared, since the body adapts to metabolise ketones. Thyroid and other endocrine changes are mostly adaptive, to optimise energy expenditure.
After initial screening, patients at normal weight may need no further investigation. Those at low or changing weight, or with abnormal findings, require further monitoring.
Abnormal electrolytes, dizziness, fainting, palpitations, drug use or heart conditions should trigger electrocardiogram (ECG) investigation, looking for prolonged QTc interval. Patients at low weight, particularly with amenorrhoea, should undergo a non-urgent dual-energy X-ray absorptiometry (DEXA) bone density scan because of the risk of osteopaenia and osteoporosis (Schorr Reference Schorr, Thomas and Eddy2017). This allows advice on safe activity and provides a baseline to show response to nutrition. Bone mineral density loss is mostly reversible with healthy nutrition over several years.
Patients may omit prescribed medication if they believe it causes weight gain. This can include insulin, steroids or anticonvulsants, with catastrophic results.
‘Compensatory behaviours’ that may be hidden or subtly disguised include purging by self-induced vomiting, taking diuretics or laxatives, overuse of prescribed or acquired drugs associated with weight loss and compulsive overactivity. These may be prioritised over pleasurable and useful experiences.
Body-checking, reassurance-seeking and ‘coaching’ in ways to lose weight maintain the preoccupation with eating, shape and weight. Compulsive accessing of social media sites is a powerful maintaining factor (Mabe Reference Mabe, Forney and Keel2014).
Risk
Management of the acute physical risks of eating disorders is addressed further below (in the section ‘Acute medical treatment’). Risk of self-harm and suicide should be considered and monitored – distress sometimes worsens as weight increases. Physical compromise increases the lethality of self-harm that is not necessarily intended to end life.
Risk assessment is particularly delicate when sufferers have social responsibilities such as parenting, nursing, medicine and teaching. Patients sometimes coerce others to eat, or neglect children to engage in compulsive exercise. Witnessing purging and self-harm is traumatic. Clinicians are also responsible for giving advice on safety to drive (Box 1).
BOX 1 Checklist to guide fitness to drive of people with eating disorders
1. Is the patient suicidal or insufficiently caring of whether they live or die?
2. What medication is prescribed and taken? Might it interfere with driving?
3. Does the patient use alcohol, other over-the-counter, online-purchased or street drugs (including painkillers, diuretics, laxatives, etc.)?
4. Are there comorbid physical or psychiatric conditions that may be inadequately managed, e.g. diabetes, epilepsy.
5. Has the patient had any episodes of collapse, faints, falls?
6. On examination of heart and brain, is there risk of collapse?
7. Is the patient stable at their current weight or have there been fluctuations (in both directions)?
8. In particular, has the patient had a recent increase in their weight so that there will be increased metabolism without corresponding replenishment of glycogen stores?
9. Does the patient have adequate physical strength to do an emergency stop etc. if necessary?
10. Has the patient ever had a recorded low blood glucose? If so, has there been normal blood glucose (above 4) in the last four blood glucose tests (>4 using venous blood, >5 on blood glucose test strips)?
11. Does the patient induce vomiting on the same days as driving? If so, how long elapses after vomiting before driving, and does the patient eat/drink again before driving? Frequent vomiting is likely to result in unstable electrolytes and fluctuating concentration.
12. Is the patient so preoccupied by obsessional thoughts, ruminations and calculations that they cannot prioritise road safety? Sometimes their behaviour in therapy will reveal preoccupations.
13. What about impulsivity and rage? Patients who have to satisfy their binges at all costs (e.g. shoplifting) may not be able to show the patience needed e.g. at traffic or pedestrian lights.
14. Does the patient eat while driving or engage in compensatory behaviours such as purging while driving?
15. Do ‘checking behaviours’ occur in the car, such as using mirrors to check appearance rather than for traffic, or using phones or calculators to add up calories while at the wheel?
Acute medical treatment
A thorough knowledge of medical complications can be life-saving, if backed up by clinician and service networks. The Management of Really Sick Patients with Anorexia Nervosa (MARSIPAN) guideline, first published in 2010, was developed in response to a number of avoidable deaths of patients with anorexia nervosa in medical units. The second edition (Royal College of Psychiatrists 2014), as well as the Junior MARSIPAN guideline (Royal College of Psychiatrists 2012), are currently under review and readers should ensure that they access the most up-to-date editions. General (family) practitioners and generalist health professionals should be aware of their local specialist eating disorder team, which will aim to work closely with an identified physician or paediatrician to enact MARSIPAN.
Psychological recovery from low-weight anorexia nervosa must be supported by medical management to prevent or mitigate lasting physical damage. Death is preventable with timely, effective treatment. The key to safe management is for key clinicians to have prepared and trained together, rather than improvise care plans in crisis.
When MARSIPAN is enacted, medical rather than psychiatric wards can be the safest setting, meeting the need for frequent blood tests, intravenous treatment, continuous ECGs and intensive care unit (ICU) availability. Keeping the individual warm, rested, nourished and protected from infection is usually taken for granted with medical patients, but compulsive eating disorder behaviours may sabotage this and alienate staff. Both psychiatric nursing skills and dietetic expertise are indispensable in refeeding low-weight patients.
The potentially fatal refeeding syndrome is caused by the switch from fasting gluconeogenesis to carbohydrate-induced insulin release, inducing considerable intracellular uptake of potassium, phosphate and magnesium from the bloodstream. Unfortunately, avoidance of overfeeding can result in lethal underfeeding and MARSIPAN guidelines advise on this.
Continuing physical management involves balancing the need to relieve constipation without fuelling an obsessive laxative habit, improving bone density without recourse to ineffective treatments, and following up on emerging or relapsing instabilities and abnormalities. Infections and hypothermia are risks in winter. Regular dental assessment is helpful. Contraceptive discussions are important even with low-weight patients.
Evidence-based psychological treatment
When physical stability, with appropriate monitoring, is assured, the most effective treatments for eating disorders are psychological therapies specifically adapted to target eating disorder pathology, as summarised in National Institute for Health and Care Excellence (NICE) guidelines (National Institute for Health and Care Excellence 2017).
Anorexia nervosa
Treatment for anorexia nervosa combines emotion regulation, distress tolerance, body image acceptance and interpersonal interventions alongside weight gain. In effect, the patient is exposed to a normal healthy weight and learns to tolerate this without eating disorder responses. In-patient or carer containment may be needed initially, followed by careful transition to the patient taking back responsibility.
Manualised FBT (Lock Reference Lock and Le Grange2015) has the best evidence base for anorexia nervosa in the under-18s, with individual eating disorder focused cognitive–behavioural therapy (CBT-ED) as a second choice. Family-based models are being adapted for young adults, and for adults and their partners (Bulik Reference Bulik, Baucom and Kirby2011; Wierenga Reference Wierenga, Hill and Knatz Peck2018).
NICE acknowledged the ‘low- to very-low’ quality of evidence for psychological treatments for adult anorexia nervosa, but recommended CBT-ED, the Maudsley Anorexia Nervosa Treatment for Adults (MANTRA) and specialist supportive clinical management (SSCM). Randomised controlled trials (RCTs) are underpowered to show superiority for any specific therapy. Even the best current treatments bring about significant improvement in only 50% of patients (Brockmeyer Reference Brockmeyer, Friederich and Schmidt2018; Murray Reference Murray, Quintana and Loeb2019).
A systematic review and meta-analysis of 35 treatment-outcome RCTs for anorexia nervosa generated concern about lack of effect (Murray Reference Murray, Quintana and Loeb2019) and disconnect between weight gain and psychological improvement. Clearly, further research is urgently needed.
Bulimia nervosa
There is more evidence for the effectiveness of CBT-ED for bulimia nervosa than for anorexia nervosa. Guided self-help appears beneficial and cost-effective, and individual CBT-ED is effective for adolescents as well as adults (Slade Reference Slade, Keeney and Mavranezouli2018). Treatment involves resetting dysregulated cycles of restriction–binge–purge. Patients establish regular mealtimes and stabilise electrolyte levels. As hunger comes under control, avoided foods are reintroduced. Intrapsychic and interpersonal skills are learned for coping with life stresses.
Binge eating disorder
There is evidence that guided self-help and group CBT-ED improve binge frequency and EDE total score compared with waiting-list control (Vocks Reference Vocks, Tuschen-Caffier and Pietrowsky2010), but there is no evidence that this treatment brings about weight loss.
Pharmacological treatment
Anorexia nervosa
Many patients are prescribed psychotropic drugs for associated symptoms of depression, anxiety and obsessive–compulsive disorder (OCD), although there are scant data on effectiveness in the presence of anorexia nervosa. The main medications directed at the eating disorder pathology are the atypical antipsychotics, particularly olanzapine, shown in some studies to reduce illness preoccupations and anxiety during refeeding. Surprisingly, weight gains are not significant in pooled meta-analyses of placebo-controlled trials. A recent out-patient RCT showed modest benefit on weight gain for olanzapine, but with no significant benefit on psychological symptoms (Attia Reference Attia, Steinglass and Walsh2019). Cannabinoid receptor agonist studies are at an early stage. A network meta-analysis is underway to build evidence for both pharmacological and non-pharmacological treatments for anorexia nervosa (Wade Reference Wade, Treasure and Schmidt2017).
Bulimia nervosa
High-dose antidepressant treatment has been shown to be of benefit in bulimia nervosa. CBT-based psychological therapies are more effective and longer lasting, but prescribing is an attractive choice if depressive symptoms are prominent, if CBT is unavailable or as adjunctive treatment.
Binge eating disorder
A recent meta-analysis (Peat Reference Peat, Berkman and Lohr2017) found that lisdexamfetamine (LDX) increased binge abstinence more than second-generation antidepressant drugs. LDX is not approved for the treatment of binge eating disorder in the UK and European Union.
Mental health legislation
UK mental health legislation allows compulsory treatment when the illness is of a nature or degree that warrants hospital treatment and there are risks to health or safety. Any fully registered medical practitioner can detain patients for brief periods. For longer periods, psychiatrists approved under the relevant legislation must be involved. Clinicians should be aware of the relevant legislation where they work. Individuals with eating disorders also perceive high levels of ‘informal coercion’. Ambivalence and the perception of coercion often fluctuate over the course of treatment.
Compulsory treatment may increase eating disorder behaviours in an attempt to regain control. Clinicians may then impose yet more restriction, so the vicious circle strengthens, unless this is managed by working to engage the patient. Studies have shown that compulsory treatment may improve survival, even when detained patients had poorer functioning before admission (Ward Reference Ward, Ramsay and Russell2016). Detention may retain people in treatment long enough to establish an effective therapeutic alliance that will then be the basis for ongoing work towards recovery.
Prognosis
The standardised mortality ratio for anorexia nervosa is 5.9 – the highest mortality rate of all psychiatric disorders (Franko Reference Franko, Keshaviah and Eddy2013). Most deaths result – shockingly – from starvation. Significant numbers are attributed to suicide. With treatment, around 50% of people with anorexia nervosa recover fully (Murray Reference Murray, Quintana and Loeb2019). Lower body mass index (BMI) or higher age at admission, persistence of binge eating and purging behaviours, substance misuse and type 1 diabetes all predict poor outcome. Motherhood is related to better outcome, as is access to specialist eating disorder services.
Recovery from bulimia nervosa is widely considered greater than from anorexia nervosa. At 9-year follow-up, 68.2% of participants with bulimia nervosa had recovered, compared with 31.4% of those with anorexia nervosa; however, by 22-year follow-up, 62.8% of participants with anorexia nervosa had recovered (the recovery rate for bulimia nervosa remained at 68.2%) (Eddy Reference Eddy, Tabri and Thomas2017). In contrast, despite optimistic long-term results from centres of excellence (Franko Reference Franko, Tabri and Keshaviah2018), other evidence suggests recovery rates from anorexia nervosa decrease over time, particularly after 12 years (Papadopoulos Reference Papadopoulos, Ekbom and Brandt2009).
There is disagreement about what constitutes ‘recovery’ from eating disorders, with consequent variation in outcome figures. Qualitative meta-analysis finds that recovered individuals value self-acceptance, autonomy and interpersonal relationships as much as reduced eating disorder symptoms (de Vos Reference de Vos, Lamarre and Radstaak2017).
Comorbidity
Psychiatric disorders
Behavioural symptoms of eating disorders often overlap with those of other psychiatric conditions, although the meaning of such behaviours may be different. Some apparent comorbidity may be secondary to the eating disorder – for instance, starvation from any cause frequently causes depression.
Over 70% of people with anorexia nervosa report a lifetime mood disorder (Keski-Rahkonen Reference Keski-Rahkonen and Mustelin2016). Between 25 and 75% report a lifetime history of an anxiety disorder (Raney Reference Raney, Thornton and Berrettini2008), typically preceding the anorexic illness. Bulimia nervosa is even more robustly associated with affective and anxiety disorders (Becker Reference Becker, Fischer and Crosby2018). Around 80% of people with anorexia nervosa experience OCD symptoms at some point. Prior OCD is associated with increased risk of subsequent bulimia nervosa (Hofer Reference Hofer, Wahl and Meyer2018). Register-based studies confirm aggregation of autism spectrum disorder in probands with anorexia nervosa and their relatives (Koch Reference Koch, Larsen and Mouridsen2015).
The prevalence of alcohol misuse in restrictive anorexia nervosa is similar to that in the general population. People with bulimic illnesses have a higher prevalence of substance misuse (Root Reference Root, Pinheiro and Thornton2010). Eating disorder sufferers use harmful substances to reduce appetite, trigger vomiting, burn off calories or permit overexercise despite pain. There is increased prevalence of other disorders of impulsivity and lack of control in people with bulimia nervosa (Kim Reference Kim, Von Ranson and Hodgins2018; Sala Reference Sala, Martinotti and Carenti2018).
Insulin-dependent diabetes
Type 1 diabetes is a disease of insulin deficiency, resulting from destruction of pancreatic insulin-producing cells. This causes hyperglycaemia, glucosuria, ketone production and weight loss. Diabetics lose weight easily by omitting insulin rather than by diet, overexercise and purging. Between 30 and 40% of young people with diabetes omit or reduce insulin with the intention of losing weight (Hasken Reference Hasken, Kresl and Nydegger2010). Longitudinal studies suggest an increase in eating disorders among young women with type 1 diabetes (Larranaga Reference Larranaga, Docet and Garcia-Mayor2011). The peak onset of type 1 diabetes is at age 10–14, unfortunately just as puberty brings increased body image concerns.
The term ‘diabulimia’ (not recognised in official diagnostic criteria) implies that causing calories to be excreted in the form of glycosuria and high blood glucose levels is analogous to purging. In type 1 diabetes conventional eating disorder behaviours are unlikely, so we recommend use of the Diabetes Eating Problem Survey – Revised (DEPS-R) screening tool (Markowitz Reference Markowitz, Butler and Volkening2010).
In addition to the serious but mostly reversible complications of non-diabetic eating disorders, diabetic complications are cumulative and irreversible. They include retinopathy, kidney disease and peripheral neuropathy. Insulin reduction increases muscle breakdown, risk of dehydration, fatigue and risk of infection. The presence of an eating disorder significantly and greatly increases rates of ketoacidosis, hospital admissions, morbidity and mortality and there is an association between poorer glycaemic control and self-reported eating disorder symptoms.
There is a potential for preventive approaches in diabetes clinics. Clinicians need awareness of eating disorder patients’ acute sensitivity to weight and body image, and psychological ‘denial’ of the risks of diabetic complications. Such patients avoid giving insulin, avoid monitoring their blood glucose to prevent being confronted with ‘bad’ results and avoid clinic appointments for fear of being ‘told off’.
Personality disorders
Around 30% of patients with an eating disorder meet criteria for at least one personality disorder (Solmi Reference Solmi, Collantoni and Meneguzzo2018). Many meet criteria for more than one. Some features are common to both disorders, and it is possible that some are consequences of the eating disorder or its treatment, rather than primary features of a personality disorder.
The presence of a comorbid personality disorder causes difficulties in terms of diagnosis and management. There are likely to be additional problems in engaging such patients, and increased risk of suicide and other mortality. The eating disorder may be used to manage the symptoms of the personality disorder, or the personality disorder may predispose to eating disorder behaviours. Individualised formulation helps both patient and clinicians to understand these functions. Alternative emotional coping behaviours can help patients to give up less adaptive behaviours.
Treatment access is complicated by service boundaries. NICE recommends that people with eating disorders are managed by specialists (National Institute for Health and Care Excellence 2017). People with personality disorders tend to be managed by community mental health services and may be referred between services according to dominant symptoms, receiving inadequate treatment in each when the disorders are intertwined. Eating disorder treatment focused on reducing purging may lead to an increase in trauma-related symptoms if purging was a way to cope with flashbacks. Difficulty managing relationships with different clinicians is a notorious aspect of personality disorder presentation, so joint working is essential.
Fertility, pregnancy and the puerperium
The effects of starvation on the hypothalamic–pituitary–gonadal axis often cause amenorrhoea. Women attending infertility clinics have a high prevalence of lifetime eating disorder. Conversely some women become pregnant without having periods, so contraception is still relevant.
Body changes during pregnancy have various effects. Some women ‘suspend’ their eating disorder, attributing the need for nutrition to a cherished baby, but others report increased body image concerns and fear that weight will get out of control (Rocco Reference Rocco, Orbitello and Perini2005).
A mother's eating disorder can significantly affect fetal development, especially neural development. Women with anorexia nervosa are more likely to have smaller-than-average babies and increased risk of postnatal depression. Women with active bulimia nervosa have increased risk of miscarriage (Micali Reference Micali, Martini and Thomas2017).
Severe and enduring anorexia nervosa
Definitions of ‘severe and enduring anorexia nervosa’ (SE-AN) vary. The very concept is contentious. ‘SE-AN’ is evoked when the eating disorder does not appear to respond to our best available treatments or responds only with extreme distress. A rehabilitation model, shifting away from weight recovery to focus on quality of life, may be more appropriate, reducing adverse effects, achieving some symptom control and setting attainable goals (Bamford Reference Bamford, Barras and Sly2015).
Recent studies suggest that CBT-ED is effective for people with long-standing anorexia nervosa in community or in-patient treatment (Raykos Reference Raykos, Erceg-Hurn and Mcevoy2018), but clinicians as well as patients may experience hopelessness. If this is not managed in supervision, ‘therapeutic nihilism’ can blight patients’ chances. Patients may be considered ‘treatment resistant’ when not all appropriate treatment approaches have been attempted. A detailed independent second opinion can suggest other avenues to follow.
Emerging treatments
Current research activity is most active in exploring ever more powerful, more focused or novel psychological therapies such as cognitive remediation therapy and exposure-based therapy, and third-wave behavioural therapies such as radically open dialectical behaviour therapy. There is also research into improved delivery of treatments in a range of web-based or electronic formats, both to exploit media that may be most acceptable to patients and also to provide equitable delivery of care from small specialist services across remote or low-income populations.
One bold, and often controversial, approach to both the understanding and treatment of eating disorders is the practice of neurosurgery and deep brain stimulation.
Controversies, uncertainties and outstanding research questions
Evolving considerations about the nature and classification of the eating disorders affect the precision with which treatments can be researched. Most treatments involve biological, behavioural and psychosocial elements, making it hard to dissect out effects.
Psychological treatments rely crucially on therapeutic attachments. Relationships may be repeatedly interrupted when treatment has to span child and adult services, or local out-patient services follow distant in-patient treatment. Management of such crucial transitions is discussed in a recent report from the Royal College of Psychiatrists (Crockett Reference Crockett, Morris and Winston2017).
The role of social media in causation and maintenance of the eating disorders is a contemporary field for exploration, as is the potential for the proper exploitation of new technology in prevention and treatment. A linked concern is whether obesity prevention campaigns fuel eating disorders.
Ignorance of the scale of the problem, and public perception of eating disorders as ‘self-imposed lifestyle choices’, mean that services struggle for adequate funding. Research suggests that even within specialist services there is inadequate implementation of evidence-based treatments, and problems of ‘therapeutic drift’. Clinicians need skills-based supervision to deliver the most effective interventions rather than those with which they are most comfortable. Meanwhile services need to collect data on both clinical activity and outcomes.
Modern neuroscience holds promise for developing understanding and treatment approaches, while psychotherapeutic, ethical and philosophical work yield insights for overcoming obstacles to progress in these uniquely ego-syntonic disorders. We may learn how to amplify psychotherapeutic benefits by pretreating the brain with surgery, medication or electrical stimulation. In this world of endemic preoccupation with body image and valid concerns about obesity, psychiatry is starved of good evidence and desperate to discover effective prevention and treatment.
Conclusions
This review has not attempted to describe the whole range of psychologically driven disorders characterised by derangement of eating behaviour, since, in UK practice at least, specialist eating disorder services and academic research focus on those disorders characterised by a maladaptive drive to lose weight rooted in extreme fear of weight gain and fatness. Various restrictive and ‘compensatory’ behaviours pose physical dangers and involve preoccupations and emotions that interfere with human experience and life achievements. Despite the appalling suffering, which also affects family and friends, the obsessive fear of weight gain often obliges sufferers to avoid rather than seek effective treatment.
Genetic research has identified a substantial, complex genetic contribution to causation and suggests that anorexia nervosa and bulimia nervosa, though overlapping, may be somewhat differently inherited. Adverse childhood experiences appear to have a non-specific relationship with all mental illness, but the body image competitiveness of modern society and social media may be triggering increased incidence in vulnerable young people, and preventive strategies are addressing this, particularly in high-risk groups.
There is little evidence for psychotropic medication as a stand-alone treatment, and most prescribing addresses comorbid psychiatric conditions. Meanwhile, integrated medical and psychiatric interventions save life and safely improve nutrition. Integrated medical expertise is most challenged when the patient is pregnant or has type 1 diabetes.
At our present stage of understanding, psychological therapies are the mainstay of treatment. The CBT model has been variously adapted so that both cognitive and behavioural exercises are used to challenge and tolerate the emotional distress that accompanies acceptance of a normal body weight. A strong, mutually respectful attachment to the therapist or therapeutic team is a crucial element of therapy. In younger patients, family-based models mobilise the strong attachment to parents to permit refeeding and toleration of the distress involved.
Author contributions
The two authors contributed equally to the writing and editing of the main text and preparation of the tables and the box.
Declaration of interest
None.
ICMJE forms are in the supplementary material, available online at https://doi.org/10.1192/bja.2020.24.
MCQs
Select the single best option for each question stem
1 Lifetime prevalence of anorexia nervosa in European women is estimated to be about:
a 0.05%
b 1%
c 5%
d 10%
e 20%.
2 Current knowledge regarding the causation of eating disorders suggests that:
a bulimia nervosa and binge eating disorder are inherited in a polygenic fashion, whereas anorexia nervosa is now thought to show autosomal recessive inheritance with partial penetrance
b a history of childhood sexual abuse is strongly predictive of the development of anorexia nervosa in the early teens
c there is a strong familial component to binge eating disorder, with estimates of heritability between 28 and 74%
d scanning studies have shown that, compared with controls, individuals with anorexia nervosa have increases in brain areas associated with self-recognition and interoceptive awareness
e an ‘over-involved’ style of parenting, particularly in the mother–daughter relationship, predisposes girls to develop eating disorders.
3 Regarding assessment of patients with probable eating disorders:
a the Eating Disorder Examination Questionnaire (EDE-Q) is the gold-standard validated self-report questionnaire for assessment of eating disorders is adults
b the MARSIPAN checklist assesses the psychosocial severity of an eating disorder
c the Clinical Impairment Assessment (CIA) questionnaire rates weight change in recovering eating disorders
d doctors have a responsibility to consider patients’ fitness to drive only if the patient is significantly underweight
e all patients with anorexia nervosa require an urgent DEXA scan of bone to screen for life-threatening osteoporosis.
4 There is evidence of at least moderate effectiveness for:
a family-based treatments for individuals with anorexia nervosa who are under the age of 18
b dialectical behaviour therapy for people with type 1 diabetes and an associated eating disorder
c psychodynamically informed multi-family groups for adults with binge eating disorder
d rebirthing therapies for teenagers with anorexia nervosa
e single-session cognitive–behavioural therapy for bulimia nervosa in adults.
5 Which of the following statements about comorbidities in eating disorders is not true?
a around 30% of patients with eating disorders meet criteria for at least one personality disorder
b the most common cause of mortality in anorexia nervosa is starvation
c prior obsessive–compulsive disorder increases the risk of subsequent bulimia nervosa
d in individuals with comorbid type 1 diabetes and eating disorder, most diabetic complications are reversible
e women attending infertility clinics have a high prevalence of lifetime eating disorder.
MCQ answers
1 b 2 d 3 a 4 a 5 d





eLetters
No eLetters have been published for this article.