The coronavirus disease 2019 (COVID-19) pandemic placed a heavy burden on acute-care pharmacists including increased demands surrounding medication access and distribution, formulary decision making, and development and implementation of COVID-19 treatment algorithms. Reference Kubin, Loo and Cheng1,Reference Mayi, Mainville and Altaf2 However, detailed information on exactly how the pandemic affected pharmacist work effort and activity is scarce. Furthermore, multiple reports have documented high rates of empiric antibiotic use in hospitalized patients with COVID-19 despite low rates of bacterial coinfections. Reference Langford, So and Raybardhan3 This antibiotic use has raised global concerns regarding the consequences of the pandemic on the longstanding public health crisis of bacterial resistance. Although there is no doubt that antimicrobial stewardship program (ASP) pharmacists supported the pandemic response, it is unknown to what extent to which the pandemic affected non–COVID-19–related antimicrobial prescribing and how ASPs implemented stewardship interventions for patients with suspected or confirmed COVID-19. Therefore, we undertook a national survey to investigate acute-care pharmacist perspectives on the impact the COVID-19 pandemic has had on their work and antimicrobial stewardship efforts.
Methods
Study design and data collection
A survey was sent electronically to 474 hospitals through 4 listservs within Vizient (Dallas, TX), the largest member-driven, healthcare performance improvement company in the United States. Participants could access the survey from March 1, 2021, through April 1, 2021 (Supplement 1). Participants were not required to complete all sections of the survey, and all survey responses were included. The survey was granted a waiver of informed consent and qualified as exempt from the University of Wisconsin Madison Institutional Review Board.
Survey participants were acute-care pharmacists who self-identified as having responsibility in verifying, monitoring, and evaluating the appropriateness of antimicrobial therapy for hospitalized patients. All practicing acute-care pharmacists were included. Participants categorized their extent and type of postgraduate training, current role, and hospital setting. Participants estimated the percent of their typical workday spent completing various task, including those specific to antimicrobial stewardship, prior to and at the December 2020–January 2021 peak of the COVID-19 pandemic. Predetermined task categories were derived by consensus of the study team (Supplement 1). The survey also asked participants to subjectively indicate the impact of COVID-19 on local antimicrobial utilization and antimicrobial stewardship practices.
Statistical analysis
Descriptive statistics were used to compare the percent responses for each survey question. We compared time spent on antimicrobial-focused tasks before and during the December 2020–January 2021 peak of the COVID-19 pandemic using paired t tests. All P values were 2-sided with P ≤ .05 considered statistically significant. Statistical analysis was performed using QuickCalcs GraphPad.
Results
In total, 122 responses were received, representing at least 68 (14.3%) of 475 unique hospitals. (Table 1). All US geographical census regions were represented, with responses from 30 states, primarily in the Midwest region (42%). Most hospitals were in urban settings (58%), academic medical centers (45.5%), and had ≥400 staffed beds (55.7%). Most respondents (73.1%) described their current role as an antimicrobial stewardship or infectious diseases pharmacist. Among all respondents, 75% reported filling a leadership position in the COVID-19 response. Postgraduate training was common (74.4%), with most completing an infectious diseases PGY-2 residency (54.2%).
Table 1. Hospital and Survey Participant Characteristics

Note. PGY-1, post-graduate year 1.
a Respondents could answer more than once.
b Of the 88 respondents who completed hospital demographics, 82 provided the city in which their institution was located. Of these cities, 68 were listed once. Based on this information, we determine that our sample included at least 68 unique hospitals.
Participants reported relative increases in time spent completing tasks related to medication access and preauthorization (2.1% before the COVID-19 pandemic, 6.8% during the COVID-19 pandemic; difference of 323%; P = .018) and administrative meeting time (34%; P = .067) during the COVID-19 pandemic (Table 2). Conversely, decreases in relative time spent completing patient-centered tasks, such as patient monitoring via chart review (4.3%; P = .056), patient-related interventions (1.7%; P = .428), bedside rounding (2.9%; P = .087), pharmacokinetics (1.1%; P = .238), education (1.9%; P = .248), and admission–discharge medication reconciliation (0.2%; P = .118) were reported, although these were not statistically significant. Using a 5-point Likert scale, participants reported that COVID-19 increased the overall utilization of antimicrobials (77.2%) and antimicrobials for acute respiratory conditions (80.0%) (Table 3). Participants also indicated that the inappropriate use of antimicrobials overall and for acute respiratory conditions increased (70.2% and 84.2%, respectively). Inappropriate prescribing during COVID-19 increased the volume of antimicrobial stewardship interventions (Table 3). Nearly 1 in 3 respondents identified an increase in antimicrobial prescribing errors (incorrect or inappropriate medication selection, dose route, frequency, or duration). Most respondents (73.6%) indicated increased use of broad-spectrum antibiotics, leading to more opportunities for antibiotic de-escalation. The perceived rate of adverse effects due to antimicrobials remained unchanged from the prepandemic period.
Table 2. Impact of COVID-19 on Antimicrobial Stewardship Programs and Pharmacist Work Distribution
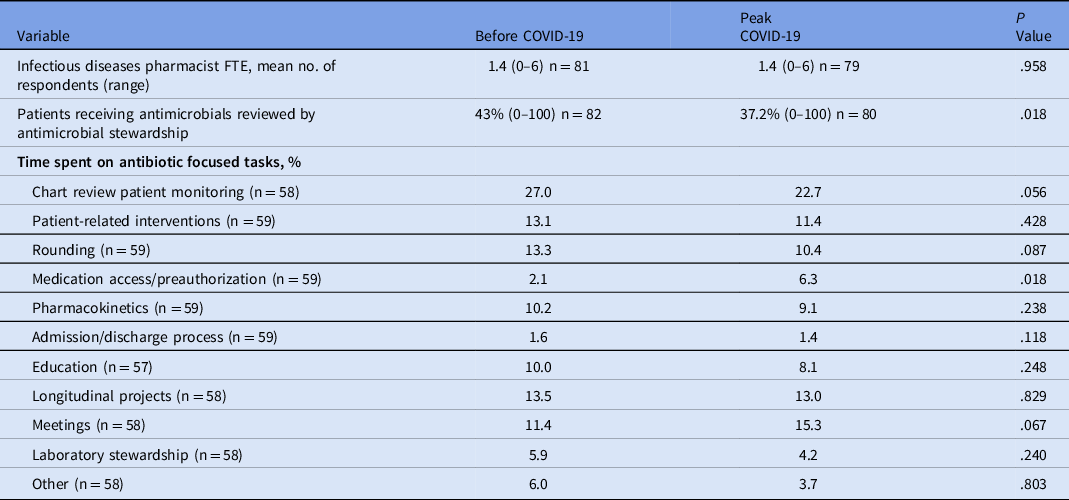
Note. FTE, full-time equivalent.
Table 3. Perceived Impact of the Pandemic on Antibiotic Prescribing Patterns and Stewardship Activities
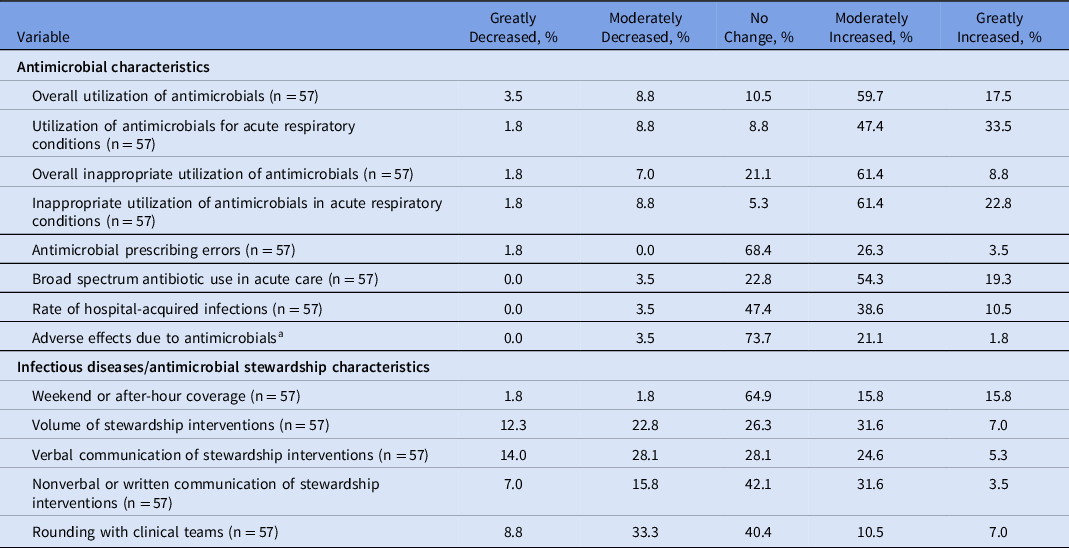
a Adverse effects due to antimicrobials include but are not limited to allergic reactions, nephrotoxicity, encephalopathy, neutropenia.
Methods of stewardship interventions changed throughout the pandemic. Verbal communication of stewardship recommendations decreased in 42.1% of participants while nonverbal or written communication increased in 35.1% (Table 3). Handshake stewardship or time spent rounding with clinical teams decreased in most participants (42.1%) during the COVID-19 pandemic as many institutions limited contact as much as possible. Unique and novel intervention strategies emerged in response to the COVID-19 pandemic as 35.3% of respondents reported making interventions to providers through the electronic health record (EHR) and other electronic-based communication tools (Table 4).
Table 4. Novel Antimicrobial Stewardship Interventions Instituted During the COVID-19 Pandemic

Note. EHR, electronic health record.
a Respondents could answer more than once.
b COVID-19 rounding teams (n = 1), provider education (n = 3), guidelines/protocols (n = 3).
Discussion
In this survey, which sampled 122 acute-care pharmacists from across the country between March 2021 and April 2021, we found that the COVID-19 pandemic significantly affected multiple aspects of ASPs. Most notably, workload tasks shifted toward administrative tasks and away from clinical tasks. This shift away from direct patient care or clinical activities during a time of increased inappropriate antimicrobial utilization may accelerate antimicrobial resistance.
Despite all hospitals facing the same novel pathogen, our report is the first to study antimicrobial stewardship interventions during the COVID-19 pandemic. An abundance of literature describing the role of ASPs in management of drug shortages, development of local treatment protocols, optimization of antimicrobial use, and reduction in antimicrobial resistance have called these programs into action during the pandemic. Reference Mazdeyasna, Nori and Patel4–Reference Tande, Stevens, Wermers and Estes6 However, little has been published on what interventions were actually adapted by ASPs. Recently, Davis et al Reference Davis, McManus and Koff7 described reconfiguration of their EHR antimicrobial stewardship module, which allowed for more efficient chart review of COVID-19 patients. Staub et al Reference Staub, Beaulieu, Graves and Nelson8 found a significant decrease in antimicrobial use after implementation of multidisciplinary clinical guidance teams. In our study, <25% of participants reported their hospital instituting EHR-based order sets, clinical-decision supports tools, or antimicrobial stewardship guidance teams specifically for patients with suspected or confirmed COVID-19. Whether the reported shift in effort toward administrative-related tasks during the pandemic detracted from engagement of ASPs in developing COVID-19 targeted stewardship interventions remains unknown. Given the overwhelming opportunities for ASPs to standardize treatment regimens in COVID-19 patients combined with constantly evolving guidance may have led to inconsistent implementation of COVID-19–specific stewardship interventions across hospitals.
As would be expected with distancing requirements and restrictions in the workplace, pharmacist communication of stewardship interventions shifted from verbal to nonverbal, with text messages and EHR-based communication. This change is concerning given the reported benefit of handshake stewardship. Face-to-face verbal interaction is useful compared to providing written suggestions in intensive care units. Reference Evans, Kosar and Peermohamed9 Furthermore, an ASP utilizing handshake stewardship in a pediatric hospital demonstrated reductions in antimicrobial use of up to 10%. Reference Hurst, Child and Pearce10 The shift in ASP communication of stewardship interventions may have unfortunately contributed to the perceived overall inappropriate increased use of antimicrobials during the COVID-19 pandemic.
Consistent with concerns raised about the impact of COVID-19 on overall antibiotic prescribing in acute care, most participants reported increases in inappropriate prescribing both overall and for respiratory tract infections. An increase in broad-spectrum antibiotics and antimicrobial prescribing errors leading to an increase in stewardship interventions was also reported. At the beginning of the COVID-19 pandemic, data on the incidence of bacterial coinfection and secondary infections were lacking. The initial rationale for using antibiotics in viral infections stemmed from the experience of bacterial superinfection in influenza, in which an 11%–35% incidence of bacterial coinfection or secondary bacterial pneumonia is described in hospitalized patients. Reference Klein, Monteforte, Gupta, Jiang, May and Hsieh11 However, the incidence of bacterial coinfection in COVID-19 is much lower. Early in the pandemic, the literature describes only a 3.1% coinfection rate at diagnosis with few patients (4.7%) developing secondary bacterial infections during hospitalization. Reference Garcia-Vidal, Sanjuan and Moreno-Garcia12,Reference Russell13 The inappropriate overuse of antimicrobials in COVID-19 patients is not unique to our study. A meta-analysis conducted by Langford et al Reference Langford, So and Raybardhan3 reported that 70% of COVID-19 hospitalized patients received antimicrobials. Given that ASP pharmacists described spending less time on patient-centered tasks during the pandemic including reviewing stewardship patients, the use inappropriate antimicrobials may have gone unchecked. Furthermore, the subjective assessment of clinical appropriateness may have been influenced by rapidly changing guidance surrounding antimicrobial prescribing as well as lack of institutional guidelines and other clinical decision support tools reported by our participants. The negative consequences of excessive antibiotic use increase the risk of antimicrobial-related adverse effects, including Clostridium difficile, excess healthcare costs, and antimicrobial resistance. Reference Russell13–Reference Páramo-Zunzunegui, Ortega-Fernández and Calvo-Espino15 Although <25% of participants described an increase in adverse effects related to antimicrobials, the impact the pandemic on long-term antimicrobial resistance trends is still unknown.
Our study had several limitations. First, most respondents described themselves an infectious diseases/antimicrobial stewardship pharmacist, which may have led to selection bias. This group was likely more willing to complete a survey focused on antimicrobial stewardship-related tasks and characteristics. Second, COVID-19 infection rates were not at their peak across the country during the open-survey period. For example, during March and April 2021, the number of confirmed hospital admissions due to COVID-19 was only 27.8% of those experienced during the maximum in January 2021. Participants were asked to answer the survey questions based on their experience during peak COVID-19 rates at their institution. However, because the survey was distributed after January 2021, recall bias may have occurred. Since the survey assessed a percentage of time spent of various activities and was unable to quantify overall time spent on work-related activities, it is possible that some respondents spent a similar percentage of time on each activity while experiencing significantly increased total workload and overall work-related time. Notably, 31.6% of respondents reported increased workload on weekends and after-hour coverage. Third, data reported in this survey are subjective. Although it would be useful to report objective information regarding antimicrobial utilization before and at the December 2020–January 2021 peak of the COVID-19 pandemic, we sought to determine frontline pharmacist perceptions regarding these characteristics only. Further research is needed. Our survey was limited to pharmacists in the Vizient network, and response rates were lower than expected. Low response rates were anticipated, especially from Northeast and Western hospitals where they faced the greatest numbers COVID-19 cases, because this survey was distributed during the COVID-19 pandemic. Although the perspectives of all acute-care pharmacists are unknown, this is the largest survey of its kind with representation from a large number of hospitals.
In this study, we have described changes to pharmacist workload associated with the COVID-19 pandemic. Shifts away from clinical activities toward administrative tasks and variation away from proven tactics to improve antibiotic prescribing may have led to suboptimal antimicrobial utilization and increased rates of antimicrobial resistance.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/ash.2022.37
Acknowledgments
Financial support
No financial support was provided relevant to this article.
Conflicts of interest
All authors report no conflicts of interest relevant to this article.






