Introduction
The Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) have identified antimicrobial resistance (AMR) as an urgent public health threat.1,2 Antimicrobial stewardship programs (ASPs) play a critical role in combating the rising rates of AMR by taking steps to identify and decrease the inappropriate use of antibiotics. The CDC identifies education as one of the core elements of both inpatient and outpatient ASPs, and the WHO explicitly recommends that medical trainees receive targeted education on antimicrobial stewardship (AS).3–5
Children are frequent recipients of antibiotics, with roughly 20% of pediatric ambulatory and emergency room visits resulting in an antibiotic prescription, and an estimated 35-70% of hospitalized children receive at least one dose of an antibiotic.Reference Poole, Shapiro, Fleming-Dutra, Hicks, Hersh and Kronman6–Reference Gourishankar, Agbasi, Kain and Lin8 Furthermore, up to 30% of antibiotic prescriptions provided to children in both the inpatient and outpatient settings are thought to be inappropriate.Reference Hersh, Fleming-Dutra, Shapiro, Hyun and Hicks9–Reference McMullan, Hall and James11 Despite the clear importance of AS in the pediatric population, most published reports describing AS educational interventions targeting trainees have focused on medical students,Reference Abbo, Cosgrove and Pottinger12–Reference Minen, Duquaine, Marx and Weiss15 internal medicine residents, family medicine residents, and infectious diseases fellows,Reference Spicer, Armstrong and Schwartz16 with limited available data that is specific to the needs of pediatric residents.Reference Alshengeti, Slayter, Black and Top17–Reference Shukla, Behnam-Terneus, Cunill-De Sautu and Perez19 The specific needs of pediatric residents are likely to differ from the needs of trainees providing care to adults given substantial differences in the types of infectious diseases (ID) in pediatric patients. There are also likely differences in both the quantity and quality of data informing recommendations on AS topics for pediatric patients, such as empiric therapy, duration of therapy, and antibiotic dosing.
Pediatric residents at Washington University in St. Louis School of Medicine (WUSM) have the opportunity to participate in an elective rotation with the St. Louis Children’s Hospital (SLCH) ASP. Residents on this rotation review a subset of patients with a new order for antimicrobial therapy as part of prospective audit and feedback, present these patients and any suggested optimizations to the ASP team (ID pharmacist and physician), and then shadow the ASP team during “handshake stewardship” rounds. Internal evaluations of this rotation indicate that this is an excellent educational experience. However, educational content is variable during the course of the two-week rotation, based on the personnel present and specific patient cases. Therefore, a standardized curriculum for resident learners to supplement education linked to patient care is desirable and has been effectively implemented at other institutions on rotations such as complex care pediatrics, pediatric pulmonology, and pediatric rheumatology.Reference Kaushik20–Reference Gillispie, Muscal, Rama, Falco and Brown22 Given the limited literature on the knowledge and skills that graduating pediatric residents should have related to AS, we conducted a needs assessment to identify the key components of an AS curriculum.
Methods
This study was approved by the WUSM institutional review board (IRB ID 202308151). The requirement for written consent was waived. Study data were collected and managed using REDCap® electronic data capture tools hosted at WUSM.Reference Harris, Taylor, Thielke, Payne, Gonzalez and Conde23,Reference Harris, Taylor and Minor24 Both surveys were conducted at WUSM/SLCH, an urban 455-bed academic children’s hospital, which includes 110 pediatrics residents and a division of pediatric ID with 19 faculty members. This needs assessment was conducted to inform AS curriculum development, aligned with Kern and colleagues’ framework for curriculum development.Reference Thomas, Kern, Hughes, Tackett and Chen25
Resident survey
The primary purpose of the resident survey was to identify AS domains in which pediatric residents thought additional education would be useful. Secondary aims were to identify resident attitudes toward AS, satisfaction with prior education on AS, and resources utilized by residents when treating suspected or confirmed infections.
Previously published surveys assessing AS-related educational needs of medical trainees (including medical students, residents in any training program, and ID fellows) were reviewed to inform development.Reference Abbo, Cosgrove and Pottinger12,Reference Minen, Duquaine, Marx and Weiss15,Reference Kolberg, Buschbeck and Wagner18,Reference Shukla, Behnam-Terneus, Cunill-De Sautu and Perez19,Reference Abbo, Sinkowitz-Cochran, Smith, Ariza-Heredia, Gómez-Marín, Srinivasan and Hooton26 The survey was refined via the cognitive interviewing technique of retrospective probing, which was conducted with a total of five recent graduates or current residents in the pediatric residency program. Survey questions were modified based on that feedback to ensure that questions were interpreted and responded to as intended by the authors.Reference Willis and Artino27
Questions related to attitudes and usefulness of additional education were assessed using a five-point Likert-type scale, with anchored response options ranging from “not at all useful” to “extremely useful.” The purpose of this component of the assessment was to gauge general interest in broad domains, and no specific thresholds were established for significance or consensus. Respondents selected one or more of their preferred learning methods or formats from a pre-generated list, with the option to add additional methods via free response text. Similarly, respondents selected resources they use when treating suspected or confirmed infections from a pre-generated list, and could add additional responses via free response text. The remainder of the survey consisted of multiple-choice questions and demographic information. The questions used in the final resident survey are included in the supplemental material (Supplement 1).
All categorical pediatric residents were eligible to complete the survey; those who had participated in cognitive interviewing were asked not to complete the survey when it was distributed. The survey was initially delivered via an email distributed by the pediatric chief residents and received responses for an 8-week period. Residents were intermittently reminded of the survey during regularly scheduled conferences and during prospective audit and feedback “handshake stewardship” rounds conducted by the ASP team. Residents also received one reminder email from the pediatric chief residents prior to closure of the survey.
Content expert (CE) survey
The primary purpose of the CE survey was to identify specific AS topics within broad domains on which ID/AS CEs consider important that graduates of a pediatric residency program be knowledgeable. For example, a domain would refer broadly to AMR, whereas a specific topic could include resistance in Staphylococcus aureus. This increased level of specificity compared to the resident survey was intended to ensure that critical topics were included in the curriculum, and to ensure CE buy-in on the curriculum that would ultimately be developed.
The CE survey was initially developed by reviewing Accreditation Council on Graduate Medical Education Pediatrics Milestones 2.0 and the American Board of Pediatrics (ABP) Entrustable Professional Activities (EPAs) for General Pediatrics.28,29 For example, the ABP EPAs identify specific essential skills for pediatricians to meet the needs of their patients and provide a scale on which these skills can be evaluated. EPA 4 in particular (entitled “Manage patients with acute common diagnoses in an ambulatory, emergency, or inpatient setting”) outlines specific conditions, many of which are infectious in nature, that most pediatricians should be able to manage independently, as well as those they should be able to manage with the assistance of a consultant. These topics provided a starting point for questions on the CE survey related to patient management, and topics were added to the survey iteratively based on feedback from study team members. Respondents rated the importance of four to 18 specific topics within nine broad domains (general principles of AS, spectrum of activity, toxicities of antimicrobial therapy, antimicrobial allergies, AMR, antimicrobial prophylaxis, diagnostics, empiric antimicrobial therapy, and duration of therapy). Topic importance was assessed on a five-point Likert-type scale, with anchored response options ranging from “not at all important” to “extremely important.” The CE survey is included in the supplemental material (Supplement 2).
All pediatric ID faculty, fellows, advance practice providers, and pharmacists at our institution were eligible to complete the CE survey. While it is important to note that not all individuals who received the survey would consider themselves experts specifically on AS, they are viewed by the local community as experts on ID as a whole. They engage regularly with residents as teachers and are expected to be able to teach key stewardship concepts. On the other hand, there is a finite amount of time during which broad ID topics can be taught to residents during training, and there may be a concern that teaching on AS content may come at the expense of other topics within ID which are also applicable to pediatric residents. We therefore felt it was important to incorporate the perspective of all ID experts so that the content included in the curriculum we developed would be identified as important by all stakeholders. The survey was announced at a division meeting and subsequently delivered via email. Prospective respondents received reminder emails weekly over a four-week period until they completed the survey. Responses to the survey were de-identified.
Statistical analysis
All statistical analysis was performed using R Statistical Software (version 4.1.2; R Foundation for Statistical Computing, Vienna, Austria). Time to complete each survey was calculated by subtracting the time at which the survey was opened from the time at which the survey was submitted. The number of prior experiences each resident had was calculated by adding the number of ID/AS rotations completed in medical school to those completed in residency. Responses to Likert-type responses on the resident survey were dichotomized as either “top box” responses (4 or 5 on the Likert-type scale) or “not top box” responses (1-3 on the Likert-type scale). Topics on the CE survey achieved consensus as being important to include in an AS curriculum if at least 80% of respondents identified the topic as “very important” or “extremely important.”
Results
Resident survey
The resident survey was distributed to 110 residents, of whom 33 responded (response rate 30%). The median (IQR) time to complete the survey was 3.4 (2.4, 5.2) minutes. Demographic information and prior educational experiences are summarized in Table 1. Overall, 23 respondents (70%) reported having at least one prior clinical experience in either ID or AS.
Table 1. Demographics of resident survey respondents
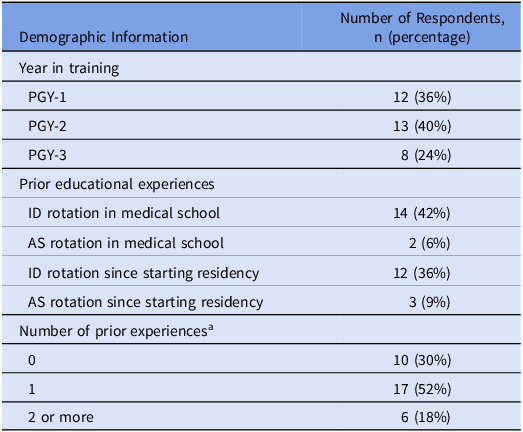
AS: antimicrobial stewardship, ID: infectious diseases, PGY: postgraduate year.
a Refers to number of ID or AS rotations in which the resident participated prior to completing survey. For example, a resident who completed an ID rotation in medical school and an AS rotation in residency would be classified as having two prior experiences.
Respondents rated their satisfaction with AS-related education in medical school and since starting residency. Four respondents (12%) identified that they were “very” or “extremely” satisfied with their education in medical school, whereas 20 (61%) respondents reported that they were “very” or “extremely” satisfied with the AS-related education they had received since starting residency training.
Residents were asked to identify resources they use when treating suspected and confirmed infections. All respondents reported knowing where to access their hospital’s empiric treatment guidelines, and 31 respondents (93%) reported using these guidelines more than half of the time when treating suspected or confirmed infections. Thirty-one respondents (93%) reported knowing how to access the hospital’s antibiogram; of these, 18 (58%) reported using the antibiogram more than half of the time when treating suspected or confirmed infections. Other resources that respondents reported using included UpToDate® (91% of respondents); the ID consult service (82%); ASP team members (79%); the American Academy of Pediatrics (AAP) Red Book (52%); Lexicomp® (40%); clinical practice guidelines published by organizations such as the AAP, Infectious Diseases Society of America, or Pediatric Infectious Diseases Society (36%); primary literature (9%); and textbooks (6%).
Respondents were asked to rate the usefulness of additional education in several different AS domains. Responses to these questions are summarized in Table 2. The percentage of respondents identifying that additional education on a topic would be “very” or “extremely” useful to them ranged from 73% (AMR) to 97% (spectrum of antibiotic activity). Other topics on which more than 90% of respondents identified that additional education would be useful were empiric antibiotic therapy (94%), duration of therapy (94%), and antibiotic prophylaxis (91%).
Table 2. Percentage of resident respondents identifying that additional education on a domain would be “very” or “extremely” useful

Respondents were asked to select methods by which they would like to learn more about AS from a list of possible learning formats. The method most frequently selected by respondents was discussion on rounds with the ASP team (79% of respondents); other methods selected by respondents included board-style questions with answer explanations (70%), handouts to reference in clinical practice (64%), in-person didactic sessions (58%), small group case-based discussions (42%), a curated list of references to read (24%), pre-recorded lectures (21%), and narrated slide decks (12%). No respondents reported that they did not want additional education on antimicrobial stewardship.
CE survey
The CE survey was distributed to 26 individuals, all of whom responded to the survey (response rate 100%). The median (IQR) time to complete the survey was 10.4 (7.8, 12.9) minutes. Nineteen (73%) respondents were faculty, five (15%) were fellows, two (8%) were advanced practice providers, and one (4%) was a pharmacist.
Overall, 39 of 105 topics (37%) achieved consensus among respondents. The domain with the greatest percentage of topics achieving consensus was empiric antibiotic therapy (11 of 13 total topics, 85%), followed by duration of therapy (5 of 8 total topics, 63%), and spectrum of activity (8 of 17 total topics, 47%). Only one topic achieved consensus in the domains of antibiotic allergies, diagnostics, and AMR, which reflected 18%, 14%, and 6% of the potential topics within each domain, respectively. The topics that achieved consensus are listed in Fig. 1 and are organized by domain; a comprehensive list of all topics on which CEs were surveyed and the percentage identifying them as “very” or “extremely” important is included in the supplemental material (Supplement 3).

Figure 1. Topics achieving consensus on content expert survey.
Topics are categorized by domain. A topic was considered to have achieved consensus if ≥80% of respondents identified having knowledge of this topic as “very” or “extremely” important for graduating pediatric residents.
AS: antimicrobial stewardship; BLIs: beta-lactamase inhibitors; BL/BLIs: beta-lactam/beta-lactamase inhibitors; HEENT: head, eye, ear, nose, and throat; TMP/SMX: trimethoprim/sulfamethoxazole
Discussion
This needs assessment identified that pediatric residents perceive additional education to be useful in a variety of AS domains, namely spectrum of antimicrobial activity, empiric antimicrobial therapy, and duration of therapy. Similarly, more than 40% of the topics achieving consensus on the CE survey were within the domains of empiric therapy and duration of therapy, despite accounting for only 20% of the topics on the survey. The results of the two surveys are complementary, indicating that practical topics such as empiric therapy and duration of therapy should be emphasized when building an AS curriculum. This focus is consistent with the tasks laid out in the ABP EPAs for General Pediatrics, which identifies infectious syndromes such as acute otitis media, sinusitis, community-acquired pneumonia, cellulitis, and urinary tract infections (among others) as clinical problems generally within the scope of general pediatricians to recognize, evaluate, and treat.29 AS-related education that increases competency in the management of conditions such as these and focuses on distinguishing these conditions from common mimickers (including viral infections), selecting the narrowest spectrum of therapy, and prescribing therapy for the shortest duration is consistent with the results of both surveys.
There was a lower level of interest in education on AMR when compared to other topics, with only 73% of pediatric residents identifying the topic as “very” or “extremely” important and with only one topic on the CE survey (resistance in Staphylococcus aureus) out of eighteen achieving consensus. The complexity of AMR and the need to focus on content relevant to all pediatricians may account for the low emphasis from CEs and residents in these data. It is likely that respondents did not explicitly recognize that local rates of AMR directly impact empiric therapy (on which they rated the usefulness of additional education highly). This illustrates that a curriculum would likely be less successful if it were built around the topic of resistance, and that education on relevant resistance mechanisms and prevalence should be inserted as needed into a discussion of topics that are of greater interest.
Curricular interventions that have been described in the literature include clinical rotations with ASPs, asynchronous modules on antibiotic prescribing, and lecture series, although most have not been studied in pediatric residents specifically.Reference Hsu13,Reference Luther, Ohl and Hicks14,Reference Spicer, Armstrong and Schwartz16,Reference Alshengeti, Slayter, Black and Top17,Reference Laguio-Vila and Lesho30,Reference Nori, Madaline and Munjal31 Pediatric residents in our cohort reported a low level of satisfaction with AS education that had occurred during medical school, whereas their satisfaction with education since starting residency training was substantially higher. We suspect this reflects the impact of a well-established ASP that connects with trainees on a near-daily basis as part of “handshake stewardship” rounds, in addition to specific education that is provided during resident conferences and formal structured rotations with either the ID service or ASP.
This study has several important limitations. First, it was conducted at a single center with a well-established ASP, and the results may not be generalizable to other centers. Residents at this center interact frequently with the ASP as part of “handshake stewardship” rounds which may impact their experience with AS education, familiarity with possible topics, and openness to additional education. Our data may not be immediately applicable to other centers that engage in different AS practices and may therefore have different educational needs. However, given that we constructed the CE survey in part using tools such as the ABP EPAs and that the results of the resident and CE surveys were in general agreement, we suspect that our findings will be a useful starting point for the development of local curricula for most centers. Furthermore, we have included the survey tools we used as supplemental material, which others can readily implement as part of their own needs assessment. A second limitation is that the response rate to the resident survey was relatively low (30%), which limited statistical analysis. Furthermore, residents who were more interested in AS may have been more likely to complete the survey, which may have inflated the level of interest in learning more about AS. That being said, the concordance with the results of the CE survey, which had a 100% response rate, supports the findings seen in the resident survey.
In conclusion, this needs assessment identified that an AS curriculum that focuses on empiric therapy and duration of therapy is most likely to meet the needs of pediatric residents and CEs. These topics align with the ABP EPAs for general pediatrics. While addressing the challenge of rising rates of AMR is a key focus of ASPs, stewardship-related education that centers on AMR is less likely to be of interest to the broadest swath of pediatric residents, and would come at the expense of other topics identified by CEs as more important for residents. Framing education on essential AMR topics within the broader context of education on empiric therapy may prove a more successful strategy, especially if it is incorporated into the day-to-day teaching that most ASPs already provide. Educators at other institutions who are interested in developing AS-related educational content for pediatric residents can consider utilizing the survey material developed in this needs assessment (included in the supplemental material) as a starting point for developing formal institution-specific curricula in AS.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/ash.2024.492
Acknowledgments
The authors would like to acknowledge Monica Abdelnour, MD for her assistance in distributing the resident survey.
Financial support
None reported.
Competing interests
All authors report no conflicts of interest relevant to this article.
Research transparency and reproducibility
The survey instruments used to create this needs assessment have been included as supplementary material. Data are available upon request; please direct inquiries to the corresponding author.





