Background
In 2015, dementia affected 47 million people worldwide, and the condition is a major cause of disability and dependency among older people (World Health Organization, 2017). Dementia care strategies have proposed that people with dementia should be enabled to live in the community and to receive care aligned with their wishes and preferences (Ministry of Health and Care Services, 2015; Organisation for Economic Co-operation and Development (OECD), 2015; World Health Organization, 2017). Living at home as long as possible may benefit people with dementia because it may promote a greater sense of independence and identity and ultimately lead to a better quality of life than living in institutions. In addition, providing informal care at home can reduce public care costs (OECD, 2015).
People with dementia may have special care needs, often requiring more supervision, personal care and more hours of care than care recipients without dementia (Prince et al., Reference Prince, Prina and Guerchet2013). Family care-givers take on substantial care responsibilities (World Health Organization, 2012; Prince et al., Reference Prince, Prina and Guerchet2013; Vossius et al., Reference Vossius, Selbæk, Ydstebø, Benth, Godager, Lurås and Bergh2015), and they are faced with increasing demands over time due to the progressive nature of the disease (World Health Organization, 2012; Prince et al., Reference Prince, Prina and Guerchet2013). Ultimately, the strains that family care-givers experience may cause psychological stress (Gilhooly et al., Reference Gilhooly, Gilhooly, Sullivan, McIntyre, Wilson, Harding, Woodbridge and Crutch2016) and increase the risk of physical ailments (Fonareva and Oken, Reference Fonareva and Oken2014). A recent meta-analysis demonstrated that almost one-third of all family care-givers of persons with dementia experience depression and that approximately one-half perceive their care-giving role to be burdensome (Collins and Kishita, Reference Collins and Kishita2019). Factors such as a higher level of care-giver burden (Hughes et al., Reference Hughes, Black, Albert, Gitlin, Johnson, Lyketsos and Samus2014) and a longer duration of care-giving (Lethin et al., Reference Lethin, Hallberg, Karlsson and Janlöv2016a) have previously been related to greater needs for health-care services.
As part of the Nordic welfare system, Norway provides one of the world's most universal and comprehensive long-term care services (Christensen and Waerness, Reference Christensen, Waerness, Christensen and Pilling2018). Although home-dwelling persons with dementia receive more services than care recipients without dementia (Kjelvik et al., Reference Kjelvik, Herbern, Kaurin, Grønnestad and Johansen2015; Vossius et al., Reference Vossius, Selbæk, Ydstebø, Benth, Godager, Lurås and Bergh2015), several of the services are used to a limited extent (Kjelvik et al., Reference Kjelvik, Herbern, Kaurin, Grønnestad and Johansen2015). A recent Norwegian study revealed that at the time immediately prior to admission to a nursing home, half of all persons with dementia had moderate dementia and one-fifth had severe dementia (Vossius et al., Reference Vossius, Selbæk, Ydstebø, Benth, Godager, Lurås and Bergh2015), which indicates substantial care needs (World Health Organization, 2012; Prince et al., Reference Prince, Prina and Guerchet2013). At the same time, approximately half of all persons with dementia received home nursing, one-fifth used meal delivery and one-fifth used day centres. Moreover, nine out of ten received informal care from family care-givers or social networks, and the amount of informal care constituted the major part of the total care provided (Vossius et al., Reference Vossius, Selbæk, Ydstebø, Benth, Godager, Lurås and Bergh2015).
Low utilisation of community health-care services seems to be an international trend (e.g. Weber et al., Reference Weber, Pirraglia and Kunik2011; Brandão et al., Reference Brandão, Ribeiro and Martín2016; Lethin et al., Reference Lethin, Leino-Kilpi, Roe, Soto, Saks, Stephan, Zwakhalen, Zabalegui and Karlsson2016b; Odzakovic et al., Reference Odzakovic, Hydén, Festin and Kullberg2018). At the same time, several studies have disclosed substantial unmet care needs among persons with dementia and/or their family care-givers (van der Roest et al., Reference van der Roest, Meiland, Comijs, Derksen, Jansen, van Hout, Jonker and Dröes2009; Black et al., Reference Black, Johnston, Rabins, Morrison, Lyketsos and Samus2013; Kerpershoek et al., Reference Kerpershoek, de Vugt, Wolfs, Woods, Jelley, Orrell, Stephan, Bieber, Meyer, Selbaek, Handels, Wimo, Hopper, Irving, Marques, Gonçalves-Pereira, Portolani, Zanetti and Verhey2017). Characteristics of the person with dementia, of family care-givers and of the health-care service system might influence the low utilisation of services. For example, persons with dementia might wish to remain independent for as long as possible (Stephan et al., Reference Stephan, Bieber, Hopper, Joyce, Irving, Zanetti, Portolani, Kerpershoek, Verhey, de Vugt, Wolfs, Eriksen, Røsvik, Marques, Gonçalves-Pereira, Sjölund, Jelley, Woods and Meyer2018), and they might be reluctant to use formal help and support (Brodaty et al., Reference Brodaty, Thomson, Thompson and Fine2005; Stirling et al., Reference Stirling, Andrews, Croft, Vickers, Turner and Robinson2010; Macleod et al., Reference Macleod, Tatangelo, McCabe and You2017). Family care-givers and/or persons with dementia might have low needs for the services (Brodaty et al., Reference Brodaty, Thomson, Thompson and Fine2005) or may be unaware of or lack information about available services (Brodaty et al., Reference Brodaty, Thomson, Thompson and Fine2005; Stirling et al., Reference Stirling, Andrews, Croft, Vickers, Turner and Robinson2010; Macleod et al., Reference Macleod, Tatangelo, McCabe and You2017; Stephan et al., Reference Stephan, Bieber, Hopper, Joyce, Irving, Zanetti, Portolani, Kerpershoek, Verhey, de Vugt, Wolfs, Eriksen, Røsvik, Marques, Gonçalves-Pereira, Sjölund, Jelley, Woods and Meyer2018). Moreover, services may not meet families’ needs (Sutcliffe et al., Reference Sutcliffe, Roe, Jasper, Jolley and Challis2015) or may be of poor quality or inflexible (Macleod et al., Reference Macleod, Tatangelo, McCabe and You2017). Other reasons for the low uptake of services might be related to financial barriers and cultural and language barriers (World Health Organization, 2012). Previous studies have indicated that ethnic minorities and indigenous people report significant barriers to accessing services (Marrone, Reference Marrone2007; Greenwood et al., Reference Greenwood, Habibi, Smith and Manthorpe2015), and a recent review study reported that indigenous populations experienced relatively low formal care and support compared with non-indigenous populations (Johnston et al., Reference Johnston, Preston, Strivens, Qaloewai and Larkins2019). In Norway, indigenous Sami people represent a minority ethnic group, and studies investigating the utilisation of community health-care services by persons with dementia and their family care-givers are lacking (Blix, Reference Blix2016).
Few large-sample studies have investigated the non-use of community health-care services, particularly in Nordic countries. To evaluate and improve the utilisation and quality of community health-care services for those in need of help and support, policy makers, health-care managers and health-care professionals need to understand why these services are utilised to a limited extent. The present study provides such knowledge from the perspective of family care-givers. This perspective is of particular importance because family care-givers of persons with dementia are likely to have knowledge of and information about the person with dementia (World Health Organization, 2017) and are likely to advocate for the care recipient and arrange for health-care services (Alzheimer's Association, 2017). In addition, family care-givers might have substantial needs for help and support; hence, they should have access to formal support and respite care tailored to their own needs (World Health Organization, 2017).
The aim of this study was to examine family care-givers’ knowledge of unused services and their self-reported reasons for non-use of such services. The specific research questions addressed in this study were as follows:
(1) Which demographic and socio-demographic characteristics of the family care-givers are associated with their knowledge of unused community health-care services?
(2) Which factors related to the care-giving circumstances are associated with their knowledge of unused services?
(3) What reasons do family care-givers report for non-use of services?
Methods
Study design
The study has a cross-sectional design, and the data were generated with a self-administered survey to family care-givers. The questionnaire was mainly based on relevant existing validated scales and items found in national and international research studies and reports, and consisted of 63 items covering different aspects of informal care provided by family care-givers and formal care provided by health-care services. The Norwegian translations of English items and scales conformed with the principles of the International Society for Pharmacoeconomics and Outcomes Research (Wild et al., Reference Wild, Grove, Martin, Eremenco, McElroy, Verjee-Lorenz and Erikson2005). During the development of the questionnaire, we collaborated with an expert group consisting of geriatric clinical professionals and researchers experienced in the development of research instruments. To support face and content validity, the entire questionnaire was pilot tested with five family care-givers of varying genders, ages and kinship relations to the care recipients. The pilot included an interview regarding how the respondents interpreted the meaning of the items.
In this study, we used different analyses to answer the central research questions. First, we used quantitative analyses to explore family care-givers’ knowledge of unused community health-care services. We compared care-givers who knew of unused services with those who were unaware of unused services and those who reported uncertainty regarding unused services. A previous study using the same sample as the current study indicated that demographic characteristics (e.g. age, gender, ethnicity, co-habitation status, relationship to the person with dementia) and socio-demographic characteristics (e.g. education level and employment status) of family care-givers were associated with the amount of health-care services used (Moholt et al., Reference Moholt, Friborg, Blix and Henriksen2018). Thus, we assumed that these characteristics of family care-givers and factors related to the care-giving circumstances could predict family care-givers’ knowledge of unused services. Second, the family care-givers’ reasons for the non-use of community health-care services were explored by using qualitative text analysis of written responses to an open-ended question. This question was a follow-up question to those who reported knowledge of unused services. These findings are integrated into the discussion.
Community health-care services
We use the terms community health-care services, health-care services or services when referring to relevant formal care arrangements for home-dwelling persons with dementia, i.e. home nursing, domestic help, remote-control safety alarm, meal delivery, day centre, support person and respite care in nursing homes. Norwegian municipalities have a statutory obligation to provide home nursing, domestic help and a support person to those in need of support. In addition, family care-givers who perform comprehensive care may require respite care (Ministry of Health and Care Services, 2011b). Other relevant services for home-dwelling persons with dementia available in most municipalities are remote-control safety alarms, meal delivery and day centres (Ministry of Health and Care Services, 2019). Day centres and support persons may provide activity services for persons with dementia and/or respite care for family care-givers (Jessen, Reference Jessen2014). Home nursing, support persons and respite care in nursing homes are free of charge (Ministry of Health and Care Services, 2011a), while the other services require out-of-pocket payment.
Participants and sampling
The target population was adult family care-givers of home-dwelling persons with dementia who were ⩾65 years of age. We define family care-giving in accordance with Zarit and Edwards (Reference Zarit, Edwards, Woods and Clare2008: 256) as follows: ‘interactions in which one family member is helping another on a regular (daily or nearly so) basis with tasks that are necessary for independent living’. Although several family care-givers may be involved in care-giving activities, we focused on family care-givers who take the major part of the care responsibilities. In this study, we used the term family care-givers, although the participants were not necessarily family members or represent the closest next of kin in a legal sense. More distant relatives, friends or neighbours were included if they provided the major part of care and were registered as next of kin of the person with dementia in community health-care service records. In line with the inclusion criteria, both family care-givers who lived with the person with dementia and family care-givers who did not live with the person with dementia were included in the study. The included family care-givers provided care on a regular basis at least once a week.
In total, 32 municipalities in Northern Norway participated in the study. The municipalities varied with regard to size, geographical dispersion, residential areas (urban versus rural areas) and ethnic composition (indigenous Sami and Norwegians). Local health-care managers approved the study and appointed research assistants who were nurses or licenced practical nurses. The research assistants used local health-care service records to identify potential participants; thus, the participants were family care-givers of persons with dementia who were users or previous users of the services. Prior to the recruitment of participants, all research assistants received individual training regarding the inclusion criteria and inclusion procedure, how to safely store inclusion records, and how to secure anonymity and confidentiality. Personalised data from the research assistants’ inclusion records were not shared with the research team.
After the initial contact with the research assistants, we noticed that a large proportion of persons with cognitive impairment and symptoms consistent with dementia were undiagnosed. A low diagnosis rate has also been documented in the literature and research regarding dementia (Wergeland et al., Reference Wergeland, Selbæk, Høgset, Söderhamn and Kirkevold2014; OECD, 2015; Prince et al., Reference Prince, Comas-Herrera, Knapp, Guerchet and Karagiannidou2016), e.g. a recent Norwegian survey based on national register data showed that only 56 per cent of all persons with dementia were diagnosed (The Norwegian Directorate of Health, 2019). Exclusion of the family care-givers of undiagnosed persons would potentially lead to a substantial loss of data. Hence, dementia was defined as a dementia diagnosis or cognitive impairment with symptoms consistent with dementia, i.e. progressive memory loss and difficulties with cognitive skills that affected the ability to perform daily life activities (Alzheimer's Association, 2017). All the research assistants were experienced in dementia care within the home-care services or respite care services, and they were dementia co-ordinators and/or members of a memory team and/or had special education in geriatrics. In Norway, these health-care professionals work in multi-professional teams, e.g. they assist the general practitioners during the diagnosis process (The Norwegian Directorate of Health, 2019). During the individual training, we instructed the research assistants to not include family care-givers if cognitive impairment was caused by other conditions (e.g. brain injury, brain tumour or delirium). If they were unsure whether the cognitive impairment was caused by conditions other than dementia, they were instructed not to include the family care-givers in the study.
We used a convenience sampling method, and all eligible family care-givers who fulfilled the inclusion criteria were included in the study (N = 788). On behalf of the research team, the research assistants distributed information about the study and the questionnaire by mail to family care-givers from April to November 2016. The participants returned the completed questionnaire in a stamped and addressed envelope directly to the research team; thus, only the researchers had access to the responses. One selective reminder procedure was carried out after four weeks. The final sample consisted of 430 family care-givers, yielding a response rate of 54.6 per cent.
Dependent variable
As no appropriate validated item regarding knowledge of unused health-care services was available, we created the following question: ‘Are there any community health-care services that are still unused? We are thinking about services you have knowledge of and that can contribute to helping and supporting the person with dementia and/or relieving yourself’. The response options were ‘yes’ (0), ‘no’ (1) and ‘I do not know’ (2). In the following, the ‘yes’ category was labelled knowledge of unused services, the ‘no’ category was labelled unawareness of unused services and the ‘I do not know’ category was labelled uncertainty about unused services. The face and content validity of the item in question was evaluated as good among the expert group and the family care-givers who participated in the pilot test of the questionnaire.
Independent variables
Demographic variables for the family care-givers included age, gender (female = 0, male = 1), relationship to the person with dementia (spouse = 0, daughter = 1, son = 2, other = 3), co-habitation with the person with dementia (no = 0, yes = 1) and ethnicity. Ethnicity was assessed with two items, namely self-identification as a Sami and Sami as first language (Brustad et al., Reference Brustad, Hansen, Broderstad, Hansen and Melhus2014). The variables were merged and coded into three categories: non-Sami = 0, confirming one Sami marker = 1 and confirming both Sami markers = 2. Socio-demographic variables assessing education level, employment status and income level were all drawn from the Tromsø study (Jacobsen et al., Reference Jacobsen, Eggen, Mathiesen, Wilsgaard and Njølstad2012). Education level was measured at four levels and further merged into three categories (elementary school = 0, high school = 1, higher education = 2). Employment status was measured at eight levels and merged into three categories (not employed = 0, part-time employed = 1, full-time employed = 2). Income level was recorded at eight levels and further dichotomised into two categories: a lower-income group (household income <350,000 Norwegian kroner (NOK), i.e. ~€35,000 = 0) and a higher-income group (household income > 351,000 NOK, i.e. ~€35,100 = 1). The classification was based on the European Union's definition of low income as less than 60 per cent of the median income in the population (Statistics Norway, 2016).
In this study, factors related to the care-giving circumstances that might underpin the family care-givers’ knowledge of unused services were duration of care-giving, perceived information level, amount of services used and negative impact of care-giving. The duration of care-giving after the appearance of dementia symptoms was assessed by using an item retrieved and adapted from the Family Collaboration Scale (Lindhardt et al., Reference Lindhardt, Nyberg and Hallberg2008). An item assessing perceived information level was retrieved from a generic scale assessing patient experiences with specialised health-care services (Sjetne et al., Reference Sjetne, Bjertnæs and Iversen2009) and adapted for this study. We asked the participants: ‘Have you received information regarding available health-care services in your municipality?’ The responses were given on a five-point Likert scale ranging from (1) ‘not at all’ to (5) ‘to a very large degree’. In the current analyses, a ‘not relevant’ option was coded as missing (N = 18).
An item assessing the amount of health-care services used was derived from a previous Norwegian study evaluating a care-giver school programme (Norwegian National Advisory Unit on Ageing and Health, 2011) and further adapted for this study. The services were categorised into two care arrangements according to principal component analysis and labelled home-based services (home nursing, domestic help, meals on wheels and remote-control safety alarm) and respite care services (day centre, respite care in a nursing home and support person) (Moholt et al., Reference Moholt, Friborg, Blix and Henriksen2018). In this study, we used the average score of the number of services in each of the care arrangements as independent variables.
The impact of care-giving on family care-givers was assessed with the Carers of Older People in Europe (COPE) Index, which is a screening tool developed to detect family care-givers in need of support (McKee et al., Reference McKee, Philp, Lamura, Prouskas, Öberg, Krevers, Spazzafumo, Bien, Parker, Nolan and Szczerbinska2003; Balducci et al., Reference Balducci, Mnich, McKee, Lamura, Beckmann, Krevers, Wojszel, Nolan, Prouskas, Bień and Öberg2008). In the analyses, we used the average score of the raw scores from all items (range 1–4), where lower scores represent more negative impacts of care-giving. The response option ‘not applicable’ (coded as missing) was included for five items and thus introduced a large proportion of missing data (ranging between 7.2 and 23.5%). The expectation maximisation (EM) method was used to impute missing data. The correlation between the imputed variables and the original variables was almost perfect (r = 0.993).
Statistical analyses
The statistical analyses were conducted in IBM Statistical Package for the Social Sciences (SPSS) for Windows version 24.0. Missing data related to the COPE Index were replaced by the EM function in PRELIS/LISREL 9.20 for Windows (Jöreskog and Sörbom, Reference Jöreskog and Sörbom2015). Descriptive data are presented as proportions, means and standard deviations for those who knew of unused services, those who were unaware of unused services and those who reported uncertainty about unused services. Significant differences between the groups were examined by using F or chi-square/Fisher exact tests for continuous and nominal data, respectively. The alpha value was reduced to < 0.01 due to the number of tests (Bonferroni method). A multinomial logistic regression analysis was used to assess the association between the outcome and the independent variables. The analysis was performed using a backward stepwise regression procedure for removing non-significant variables. An alpha value of < 0.05 was used as an indication of statistical significance.
Qualitative analyses
In an open question, participants who reported knowledge of unused community health-care services (the ‘yes’ category in the dependent variable) were invited to describe their reasons for not using the services in their own words. Overall, 174 participants responded to this question, which was slightly more than those who reported knowledge of unused services (N = 168). All text data were included in the subsequent qualitative analysis because a few of the participants who reported uncertainty about unused services stated their reasons, e.g. insufficient information about available services or that they did not need additional services. The length of the written responses ranged from short notes to lengthy sentences (~200 words). The text material was analysed according to the principles of thematic analyses, as described by Braun and Clarke (Reference Braun and Clarke2006). The analysis process was recursive, as the initial phase consisted of repeated reading of the data, followed by a text coding phase and a code sorting phase to create broader themes. Two of the authors (J-MM and BHB) independently carried out the initial phases of the analyses and subsequently met to discuss the initial themes and conduct the sorting of codes into broader themes. The themes were further revised and finally named in collaboration. The involvement of two researchers in this process provided opportunities for investigator triangulation to moderate the risk for biased interpretations (Polit and Beck, Reference Polit and Beck2017: 566). While we endeavoured to approach the data-set open-mindedly, the analysis was informed by relationship-centred care theories and was hence theory driven (cf. Braun and Clarke, Reference Braun and Clarke2006). Based on such theories, we assumed that non-use of health-care services could be related to the features of those involved in care-giving, i.e. the person with dementia, the family care-giver and/or the health-care services (Nolan et al., Reference Nolan, Ryan, Enderby and Reid2002; Adams and Gardiner, Reference Adams and Gardiner2005).
Ethics
The study complied with the Helsinki declaration for research ethics (World Medical Association, 2018). The Norwegian Centre for Research Data approved the study with regard to the procedures related to the use of local records to identify participants, data collection and data privacy (e.g. de-identification and anonymity) and obtaining informed consent. Along with the questionnaire, all invited family care-givers received written information about the purposes of the study, which also stated that participation was voluntary and included a description of how confidentiality and anonymity were ensured. The participants consented by completing and returning the questionnaire to the research team. A honorarium of two lottery tickets worth 50 NOK (approximately £5) was given.
Results
Knowledge of unused community health-care services – quantitative analyses
The descriptive characteristics of the family care-givers and knowledge of unused community health-care services are presented in Table 1. In total, 40.2 per cent of the participants knew of unused community health-care services, 11.6 per cent were unaware of unused services and 45.6 per cent reported uncertainty regarding unused services. The portion of missing data was low (2.6%); hence, 419 participants were included in the analyses.
Table 1. Characteristics of family care-givers and knowledge of unused community health-care services

Notes: N = 419. COPE: Carers of Older People in Europe. χ2: chi square. F: analysis of variance. 1. Adjusted p-values (Bonferroni method) are significant at the 0.001 level between the ‘knowledge of unused services’ group and ‘uncertainty about unused services’ group and between the ‘unawareness of unused services’ group and ‘uncertainty about unused services’ group. 2. Adjusted p-values (Bonferroni method) are significant at the 0.001 level between the ‘knowledge of unused services’ group and ‘unawareness of unused services’ group and at the 0.01 level between the ‘unawareness of unused services’ group and ‘uncertainty about unused services’ group. 3. Adjusted p-values (Bonferroni method) are significant at the 0.001 level between the ‘knowledge of unused services’ group and ‘unawareness of unused services’ group and at the 0.01 level between the ‘unawareness of unused services group and ‘uncertainty about unused services’ group.
Significance levels: * p < 0.05, ** p < 0.01, *** p < 0.001.
Group differences are presented in Table 1. Differences in the knowledge of unused community health-care services were related to the following characteristics of the family care-givers: gender (more females reported knowledge of unused services than males), co-habitation status (more care-givers who did not co-habit with the care recipient reported unawareness of unused services than those who co-habited with the person), relationship to the person with dementia (more daughters reported knowledge of unused services than spouses, sons and those with other kinship relations), education level (more care-givers with higher education reported knowledge of unused services than those with lower education), employment status (more of those who were not employed or retired reported uncertainty about unused services than those who were employed full-time) and income level (more care-givers with higher incomes reported knowledge of unused services than those with lower incomes). In addition, the following factors were significantly correlated with family care-givers’ knowledge of services: information level (those who were uncertain about unused services reported lower levels of information about available health-care services than those who knew of and those who were unaware of unused services), negative impact of care-giving (those who were unaware of unused services had lower negative impacts of care-giving than those who knew of unused services and those who were uncertain) and use of home-based services (those who were unaware of unused services used more home-based services than those who knew of unused services and those who were uncertain).
Multinomial regression analysis
The variables that were significantly associated with the dependent variable (according to Table 1) were included as predictors in a multinomial regression analysis. The participants who knew of unused services represented the reference group. The odds ratios, confidence intervals and p values are presented in Table 2.
Table 2. Predictors of family care-givers’ knowledge of unused community health-care services
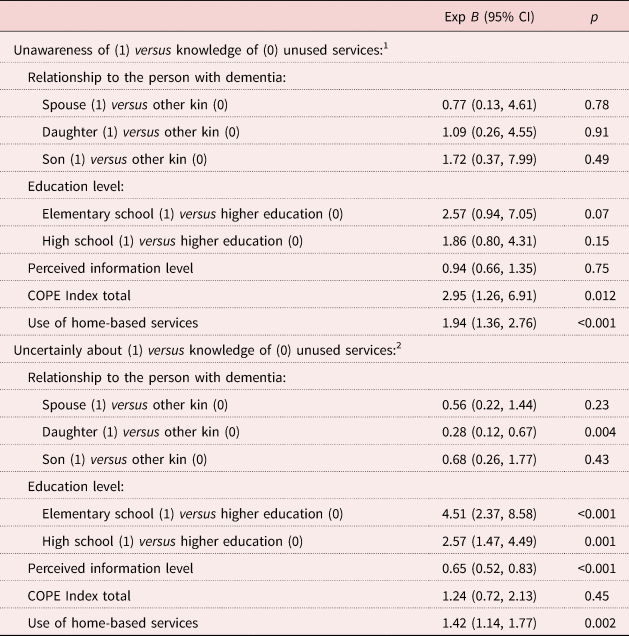
Notes: N = 419. Exp (B): odds ratio. CI: confidence interval. COPE: Carers of Older People in Europe. Nagelkerke pseudo R 2 = 0.25, goodness of fit (Pearson χ2/degrees of freedom) = 1.06. 1. Intercept = −6.37. 2. Intercept = 0.17.
The use of more home-based services and higher scores on the COPE Index (less negative impact of care-giving) significantly increased the odds for reporting unawareness of unused services. The family care-givers with lower education levels (elementary school or high school) and care-givers using more home-based services had significantly higher odds of reporting uncertainty about unused services than the care-givers with higher education levels and care-givers using fewer home-based services. Conversely, the daughters and care-givers who scored higher for perceived information level had significantly lower odds of reporting uncertainty regarding unused services than the other kin groups and care-givers who had lower scores for perceived information level.
Reasons for non-use of community health-care services – qualitative analysis
The initial text codes were examined, sorted, revised and finally merged into four overarching themes: (a) reasons related to the persons with dementia, (b) reasons related to family care-givers, (c) reasons related to the health-care services system, and (d) reasons related to several of the themes.
Reasons related to the person with dementia
This theme included the following sub-themes: the person with dementia was reluctant to use services and the person did not yet need services. The majority of the responses were related to the persons’ reluctance to use community health-care services. The reasons for reluctance were diverse, including that the persons with dementia needed help and support but refused to use services. Several of the family care-givers indicated that the person with dementia lacked insight into his or her own situation:
Community health-care services are not used. He lacks insight in his own situation, and he does not understand the necessity of these services. (Respondent 37, grandchild)
Moreover, some reported that the persons with dementia experienced help and support as humiliating or stigmatising. In addition, help and support could be a reminder of lost capacity:
She experiences the day centre as stigmatising and simultaneously as a reminder about loss of capacity. These are the same reasons for not using respite care in the nursing home. (Respondent 134, spouse)
Several respondents described that persons with dementia preferred to receive help from their families. Other respondents described that the care recipient did not want to interact with strangers or felt unsafe in unfamiliar environments, e.g. at the day centre.
She has a place at the day centre twice a week. She does not want to use this service. She is afraid and unsafe because she does not know where she is. (Respondent 99, son)
To meet the needs for help and support, some of the family care-givers reported that they performed care tasks that could and perhaps should have been performed by health-care professionals. Several of the family care-givers considered that the person with dementia had high needs for the services they refused to use:
He needs more help in terms of home nursing, personal care, cleaning, shopping, meal delivery and respite care in a nursing home, but he is reluctant to receive help. He thinks he manages everything. The home nurses offer him more support, but he refuses. Thus, I have to help him. (Respondent 104, daughter)
Reluctance to use services might be an unresolved problem, as several family care-givers expressed a high need for unused services, e.g. respite care in a nursing home, day centres or a support person:
I have been healthy until recently. The night wandering is burdensome. In periods, I sleep poorly. He smokes at nighttime and sometimes he loses the cigarette on the floor or on the tablecloth. I am very afraid of fire. I need respite care, but he refuses! (Respondent 17, spouse)
The second sub-theme reflected that the person with dementia did not yet need services. Some family care-givers described that the disease was in an early phase and that the need for services was therefore not yet present. Others described that the person with dementia wanted to manage with limited or no help from health-care services:
She does not want more help. Still, she is managing at home in familiar environments. She wants to perform tasks such as cleaning and cooking. (Respondent 32, daughter)
Reasons related to the family care-giver
The theme included the following sub-themes: the family care-giver did not yet need services and the care-giver was reluctant to use services. Within this theme, the majority of responses indicated that the family care-givers did not yet need help and support. Several of the family care-givers reported knowing of unused health-care services that could be relevant in the future, e.g. personal care, respite care and long-term care in an assisted living facility or in a nursing home. Some family care-givers reported that they considered their own help and support, such as household work and cooking, to be a natural part of daily life. However, several reported that they were about to reach the limit for how much care they could provide:
I have performed tasks that I feel are natural within a marriage. In my situation, I am now struggling with physical diseases, which limits how much I can help my husband. We have an adult child who contributes a lot with practical assistance. Conclusion: the society is saving a lot, economically speaking. (Respondent 103, spouse)
The second sub-theme reflected that the family care-givers were reluctant to use health-care services. The family care-givers’ reluctance was closely associated with the reluctance of the person with dementia, as the family care-givers could not force the person to use services. Some were worried about conflicts with the care recipient:
He does not understand that he is ill. Initiating health-care services will make problems for me, e.g. suspicion/aggression. Thus, I have not applied for services. (Respondent 152, spouse)
Reasons related to aspects of health-care services
This theme included the following sub-themes: the family had applied for but not received services, the services did not meet the needs of the person with dementia or of family care-givers, and the quality of the services was poor. The main reason for non-use was that one or more services were applied for but not received. Several respondents referred to lengthy processing and long waiting lists, particularly related to services such as support persons, respite care in a nursing home and long-term care in a nursing home. Several of the family care-givers reported an extensive need for services:
I have applied for the day centre and for respite care when I am away. I think it is madness that she is on her own … I have still not received a response to the applications. I am also ill. (Respondent 165, daughter)
Others reported that their applications had been rejected. The long distance between the location of the services and the care recipients’ home was sometimes a reason for rejection. Several family care-givers described reasons for the rejections, such as services not being available. This issue was particularly related to a support person, which is a statutory service. Others described that the person with dementia was considered too healthy to receive the service. However, the family care-givers disagreed strongly with the assessment:
She did not receive short-term care in the nursing home, they said she is too healthy. Those who administer the services do not know anything about that. They are never here to see how frail she is. (Respondent 111, daughter)
The sub-themes reflecting that the community health-care services did not meet the needs of the persons with dementia and/or of family care-givers and that the quality of the services was poorer than expected were closely related. Some described that the service was not meaningful:
I have been offered respite care once a week. We have tried, but he is too ‘healthy’, he was just sitting there with persons with severe dementia. Nothing to do, no activities. (Respondent 20, spouse)
Several care-givers explicitly reported that the services were of low quality, which was often related to a low quality of readymade meals (meal delivery) or cleaning (domestic help). In addition, a lack of transportation services contributed to the non-use of day centres.
Reasons related to the person with dementia and/or the family care-giver and/or the health-care services
Several of the family care-givers’ responses related to aspects that carried across the themes. As described above, the family care-givers’ reluctance regarding the use of health-care services was closely related to the reluctance of the person with dementia. Moreover, some of the care-givers described that the person with dementia refused to use a particular service and that other services were perceived as unnecessary.
I have chosen to stay at home and take care of my husband … He refuses to meet the support person. I am familiar with the care tasks; thus, home nursing is not relevant. (Respondent 125, spouse)
Several respondents described that the reluctance of the person with dementia was closely related to the quality of the services or insufficient adaptation of the services:
She used meal delivery, but she did not find the dinners tasty … Currently, she has a place at the day centre twice a week, but she does not want to go there because they are simply sitting in a chair. (Respondent 22, daughter)
Some of the family care-givers reported that they managed with limited assistance or without help from the formal health-care services, but their responses simultaneously indicated that they did not have knowledge of additional support. Others reported that help from health-care services was initiated too late and that the information about available health-care services was insufficient:
In the autumn, we found a place for her at the day centre. Until then, I was alone with the care responsibilities, and I did not know of available services … At that point in time, I was exhausted. Friends contacted the community health-care services. The day centre is now a great help for us. I feel that the information from the general practitioners about the disease and available health-care services is insufficient. This disease may still not be talked about or kept within the family. (Respondent 82, spouse)
Discussion
The current study employed both quantitative and qualitative data regarding the non-use of community health-care services. The quantitative data suggest that characteristics of family care-givers and factors related to the care-giving circumstances were associated with family care-givers’ knowledge of unused services. The qualitative data showed that reasons for non-use of services were multifaceted and complex, and were related to attributes of the person with dementia and/or the family care-giver and/or the health-care services. Although services were unused, several family care-givers indicated substantial needs of the services.
The majority of the participants reported uncertainty regarding unused health-care services, whereas approximately two-fifths reported knowledge of unused services. Only one of ten were unaware of unused services. As expected, the use of formal support varied between the groups. Those who were unaware of unused services reported use of more home-based services than the other groups, and simultaneously, they reported less negative impact of care-giving. Previous studies have reported that care recipients who live alone use more home-care services than those who co-habit with family care-givers (Døhl et al., Reference Døhl, Garåsen, Kalseth and Magnussen2016; Moholt et al., Reference Moholt, Friborg, Blix and Henriksen2018). In this study, no differences appeared between these groups regarding knowledge of unused services. This finding was somewhat contrary to our expectations, as we assumed that family care-givers who shared daily life with the person were also more involved in formal care and thus had more knowledge of available services.
The results indicated that the information level regarding available community health-care services varied. Those who reported uncertainty about unused services had a significantly lower information level compared to those who knew of unused services. Moreover, the qualitative data indicated that several participants who reported knowing of unused services also described a lack of information about additional services. These results concur with those of other studies. A study among persons with dementia and family care-givers in eight European countries reported substantial unmet information needs. The study indicated that insufficient information about available services most likely leads to non-use of services (Kerpershoek et al., Reference Kerpershoek, de Vugt, Wolfs, Woods, Jelley, Orrell, Stephan, Bieber, Meyer, Selbaek, Handels, Wimo, Hopper, Irving, Marques, Gonçalves-Pereira, Portolani, Zanetti and Verhey2017). A qualitative interview study suggested that insufficient information is a key barrier to service use, as family care-givers do not know where to find or how to gain access to relevant information (Macleod et al., Reference Macleod, Tatangelo, McCabe and You2018).
In this study, the groups also differed with regard to education level, as the odds for reporting uncertainty regarding unused services were more than four times higher for those with an elementary school level of education and about two and a half times higher for high school-educated respondents compared to those with higher education. Higher education levels have previously been associated with the use of more community health-care services (Lüdecke et al., Reference Lüdecke, Mnich and Kofahl2012; Martindale-Adams et al., Reference Martindale-Adams, Nichols, Zuber, Burns and Graney2016), and similar findings have been found in Norwegian studies (Sævareid et al., Reference Sævareid, Thygesen, Lindstrom and Nygaard2012; Moholt et al., Reference Moholt, Friborg, Blix and Henriksen2018). Individuals with higher education levels might be more aware of their rights to access services (Sævareid et al., Reference Sævareid, Thygesen, Lindstrom and Nygaard2012) or more prone to obtain information about eligible services than individuals with lower education levels. Altogether, the results suggest that the availability of information about health-care services should be improved and adapted to individuals at the municipal level to ensure equal access to and use of health-care services. Raising awareness of appropriate health-care services is important to achieve the best outcomes for both the family care-givers and the person with dementia for whom they are caring (Erol et al., Reference Erol, Brooker and Peel2015: 38).
The qualitative data showed that one of the most commonly reported reasons for not using health-care services was that the family care-givers did not yet need such services. It is reasonable that persons with dementia in the early stage of the disease can manage well with limited formal and informal assistance or that some family care-givers can manage their care responsibilities well through the course of the disease. In addition, services might be assessed as unnecessary, e.g. some of the family care-givers reported that they performed household tasks as a natural part of daily life. Stirling et al. (Reference Stirling, Andrews, Croft, Vickers, Turner and Robinson2010) reported that normative expectations of the spousal role could be the reason that practical help at home was the least used service in their study. The increase in work at home was accepted as an extension of the regular duties implied by the spousal role. A Swedish interview study of women caring for a partner with dementia showed that care-givers tended to downplay their need for formal support. Although they acknowledged that they needed support, they were not yet ready to accept it (Eriksson et al., Reference Eriksson, Sandberg and Hellström2012). In our study, several family care-givers who did not need services also described that they were about to reach their limit for how much care they could provide, and some referred to their own health problems and reduced capacity to provide help and support. A previous study of non-use of health-care services reported that family care-givers might deny a need for health-care services despite a low level of satisfaction with their care-giver role and a high level of overload (Brodaty et al., Reference Brodaty, Thomson, Thompson and Fine2005). To be proactive and offer service options adjusted to a family's needs, health-care professionals should not only inform about available services but also point out the individual advantages of using formal support (Graessel et al., Reference Graessel, Luttenberger, Bleich, Adabbo and Donath2011).
In this study, a commonly reported reason for not using community health-care services was that the care recipients were reluctant to use such services. Moreover, several of the family care-givers recognised crucial needs for the unused services. In a cross-national European study, people with dementia (mostly younger persons with dementia) expressed that they wanted to remain independent as long as possible, and formal care was considered a threat to individual independence (Stephan et al., Reference Stephan, Bieber, Hopper, Joyce, Irving, Zanetti, Portolani, Kerpershoek, Verhey, de Vugt, Wolfs, Eriksen, Røsvik, Marques, Gonçalves-Pereira, Sjölund, Jelley, Woods and Meyer2018). Although maintaining identity and independence is a strong personal driver for many persons with dementia (Erol et al., Reference Erol, Brooker and Peel2015: 6), this might increase the demands on family care-givers when the need for help and support is extensive. In a Norwegian qualitative interview study among family care-givers of older home-dwelling persons with dementia, all family care-givers described that the person they cared for refused admission to nursing homes despite extensive care needs. Simultaneously, the family care-givers strived to balance the assumed duty to provide care with their own needs (Larsen et al., Reference Larsen, Blix and Hamran2018). Despite increased attention to family care-givers in Norwegian governmental white papers (Ministry of Health and Care Services, 2015, 2018), family care-givers have limited statutory rights regarding their own needs for services. In addition, services are allocated according to the estimated needs of the care recipient (The Norwegian Directorate of Health, 2016) rather than the care-givers’ needs. Although previous studies have reported similar findings to those from the current study (Brodaty et al., Reference Brodaty, Thomson, Thompson and Fine2005; Phillipson et al., Reference Phillipson, Magee and Jones2013; Macleod et al., Reference Macleod, Tatangelo, McCabe and You2017), few strategies have been suggested to facilitate service use when care recipients with substantial care needs are reluctant to use services. Future research should address this issue in more detail, e.g. with use of methods such as in-depth interviews with both care recipients and family care-givers.
In this study, a third prominent reason for not using services was related to diverse aspects of health-care services. Long waiting lists, lengthy processing and the rejection of applications indicated that the allocation of services is not a straightforward procedure. Nonetheless, several of the family care-givers reported an extensive need for the services. A previous Norwegian study reported that although allocation of health-care services should be performed in accordance with the principle of proportional justice (justice between competing claims for priority), limited resources might result in prioritising care recipients with urgent needs and fewer coping resources, such as limited access to help and support from family (Vabø, Reference Vabø2011). Altogether, these findings might indicate that informal care from family care-givers substitutes for formal care from health-care services. Future studies should investigate how health-care professionals address the needs of both care recipients and family care-givers when allocating services.
Other respondents described that the care recipients were reluctant to use the services due to the low service quality or the inability of the services to fulfil care needs. With respect to day centres, some respondents reported a lack of appropriate activities. Similar findings are reported in a recent Norwegian qualitative study among family care-givers of persons with dementia. The results indicated that day centres lacked meaningful activities, and the activities were not tailored to care recipients’ physical functional levels (Granbo et al., Reference Granbo, Boulton, Saltvedt, Helbostad and Taraldsen2019). However, a qualitative study carried out in Norway and Scotland reported that the use of day care resulted in benefits and positive experiences for persons with dementia, e.g. increased wellbeing and increased social engagement. Although the persons with dementia were initially reluctant to use the day centre, several reported growing acceptance through everyday experience with the service. Then, once the family care-givers believed that the care recipients were well cared for, they were able to take a break from the caring role (Rokstad et al., Reference Rokstad, McCabe, Robertson, Strandenæs, Tretteteig and Vatne2017). This finding might indicate that services providing positive experiences for the person with dementia, and ultimately for family care-givers, are required to ensure the use of such services.
In this study, several of the family care-givers reported that the persons with dementia did not want to interact with strangers or felt unsafe in unfamiliar environments. An Irish study showed that some persons with dementia preferred in-home respite care (O’ Shea et al., Reference O’ Shea, O’ Shea, Timmons and Irving2019). It is possible that the care recipients would accept the care arrangement and health-care professionals in their familiar home. At the time of data collection, in-home respite care was rarely available in Norwegian municipalities (0.9% of the day activity services) (Gjøra et al., Reference Gjøra, Eek and Kirkevold2014). Altogether, the results from this study and previous research might indicate that flexible and beneficial services for persons with dementia and family care-givers are required, e.g. in-home respite care and activity services adapted to the care recipient's functional level.
Although the family care-givers reported diverse reasons for not using services, we noticed that those who reported knowledge of unused services also reported a more negative impact of care-giving than those who were unaware of unused services. This finding might indicate that family care-givers who reported knowledge of unused services did not receive adequate support in their care-giving role. Due to the complexity of the responses, we did not have the opportunity to investigate the negative impact of care-giving in sub-groups of those who reported knowledge of unused services. Future studies should more thoroughly address the relationship between non-use of services and the negative impact of care-giving/care-giver burden.
The fact that responses regarding reasons for non-use of services disclosed substantially unmet care needs might indicate that more attention should be paid to the efforts of family care-givers. Ward-Griffin (Reference Ward-Griffin2012) argues that the complementary care approach to home-based services contributed to inadequate support for family care-givers. Within this approach, formal care from health-care services supplements informal care when the needs of the care recipient exceed the resources of the formal care-giver. Formal support to family care-givers, e.g. respite care, is often ‘too little’ and ‘too late’ to have the intended effects (Ward-Griffin, Reference Ward-Griffin2012: 176). Schulz and Czaja (Reference Schulz and Czaja2018) suggest that health-care providers should see family care-givers as partners who may need information, care and support rather than just as a resource in the treatment of the care recipient. Family care-giving is often presumed, as care-givers are not asked about their ability to provide care (Schulz and Czaja, Reference Schulz and Czaja2018). A key finding arising from our study was the complexity regarding why health-care services are not used. The reasons were related to aspects of the care recipient and/or the family care-givers and/or the health-care services. Thus, a holistic care approach that includes family care-givers, such as relationship-centred care, is recommended (Ward-Griffin, Reference Ward-Griffin2012; Schulz and Czaja, Reference Schulz and Czaja2018). This approach is based on dynamic interactions between those involved in caring: the person with dementia, family care-givers and health-care professionals (Nolan et al., Reference Nolan, Ryan, Enderby and Reid2002; Adams and Gardiner, Reference Adams and Gardiner2005).
Study limitations
In this study, the majority of the participants were family care-givers of persons who were users or previous users of health-care services. Thus, we had limited opportunities to examine knowledge of unused services and reasons for non-use of services among those who did not utilise services at all. This constraint, combined with the fact that we used a convenience sampling method, may limit the generalisability of the results.
In this study, Sami ethnicity did not predict family care-givers’ knowledge of unused services, and none of the respondents reported reasons for non-use of services related to cultural or ethnic aspects. The low proportion of Sami participants (7%), which entailed a lower statistical power, may explain the lack of a significant association. However, a previous study based on the same data-set as the present study demonstrated that Sami participants used fewer home-based services than non-Sami participants (Moholt et al., Reference Moholt, Friborg, Blix and Henriksen2018). In Norway, the utilisation of community health-care services among Sami has been sparsely investigated, and future studies should address this issue in a larger sample of Sami participants.
We created a single item about knowledge of unused health-care services with categorical response options for this study. It is possible that the three categories did not fully capture family care-givers’ knowledge of unused services or did not appropriately distinguish among the groups. The interpretation of the ‘I don't know’ category as an expression of ‘uncertainty’, i.e. insufficient knowledge about unused services, may raise some concerns. Pilot testing of the survey questionnaire among family care-givers revealed that respondents interpreted the statement correspondingly. The fact that participants who reported higher levels of perceived information had lower odds of choosing the ‘I don't know’ category may seem to support this interpretation. Furthermore, the perceived information level regarding available community health-care services was measured with a single item. In the questionnaire, the item appeared in a sequence of questions addressing help, support and collaboration with the community health-care services. In the pilot test of the questionnaire, family care-givers interpreted the question as information they had received from health-care professionals and not as information they had acquired by themselves. However, we lack data specifying the actual content of information the participants had in mind when responding to the item.
We used a single open-ended question to evaluate the reasons for non-use of health-care services. Open-ended questions following closed questions are useful for clarification of reasons and explanations, and the method can provide informative data. The method requires more deliberation and is more demanding for respondents than closed questions, and the quality of the data is dependent on the participants’ willingness and ability to write their replies (Bowling, Reference Bowling2014: 295). In this study, the generated text data were surprisingly rich, and the majority of the responses were related to themes or aspects that underpinned several of the themes. However, we cannot disregard that family care-givers have other reasons for not using services, although these are likely less frequent.
The main themes identified in the qualitative text analysis were not suitable to create categories that could be analysed by quantitative methods. Thus, we could not examine whether the characteristics of family care-givers were associated with the diverse reasons for the non-use of services. The results emerging from the analyses may guide future research, e.g. in-depth interview studies, or form the basis for developing research instruments to assess the non-use of community health-care services.
Although several significant associations of family care-givers’ knowledge of unused community health-care services were identified, a substantial proportion of the variance in the analysis remained unexplained. Other relevant factors explaining knowledge of unused services may therefore have been omitted, such as the progression of the dementia disease and the degree of disability of the person with dementia. It is reasonable that the need for formal help and support increases as the disease progresses (World Health Organization, 2012; Prince et al., Reference Prince, Prina and Guerchet2013), which might affect family care-givers’ knowledge of services. We did not have permission to collect such data and therefore could not adjust our prediction estimates accordingly. If ethically acceptable, future research about the non-use of health-care services should include measures regarding the progression of the dementia disease and the cognitive and functional capacity of the person with dementia. We did not have access to data regarding the accessibility of health-care services or care arrangement structures in the included municipalities. It is reasonable that these factors might have influenced family care-givers’ knowledge of unused services and their reported reasons for non-use of services. Future studies should investigate how underlying structures and organisation of community health-care services affect the accessibility, availability and use of services among those in need of help and support.
Conclusions
This study provides information about family care-givers’ knowledge of unused community health-care services and reasons for the non-use of services. The results may have implications for both community health-care services and future research. To ensure equal access to and use of health-care services, our results suggest that health-care professionals should provide individually tailored information about available services and information about the benefits of service use for both the care recipient and the family care-giver. Non-use of services might result in more care-giving demands on the family care-givers. Thus, strategies to facilitate service use are needed, and future research on non-use of services should include both persons with dementia and family care-givers to address this issue in a more nuanced manner. To ensure the utilisation of health-care services, the services must be developed and adapted in accordance with both the care recipients’ and family care-givers’ needs. Thus, we recommend a relationship-centred approach to dementia care.
Acknowledgements
The authors would like to thank the management and health-care providers for their assistance with the data collection. Special thanks are given to all the family care-givers who participated in this study. We would like to thank the editor and the two anonymous reviewers for constructive, inspiring and clarifying comments on an earlier draft of this paper.
Author contributions
J-MM participated in the study design, development of the questionnaire, data collection, statistical analysis, qualitative analysis and data interpretation, and writing of the manuscript. OF participated in the study design and the development of the questionnaire and was responsible for the statistical analysis and interpretation of results in addition to writing and revising the manuscript. NH was responsible for the study design, development of the questionnaire and data collection in addition to the interpretation of results and the writing and revising of the manuscript. TH participated in the study design, development of the questionnaire, data collection, and writing and revising the manuscript. BHB participated in the study design and was responsible for the qualitative analysis and interpretation of the results in addition to writing and revising the manuscript. All authors read and approved the final manuscript.
Financial support
This work was supported by the Norwegian Research Council (grant number 238146). The funding body played no part in the study design, data collection, analysis, data interpretation or manuscript preparation.
Conflict of interest
The authors declare no conflicts of interest.
Ethical standards
The Regional Committee for Medical and Health Research Ethics for Northern Norway evaluated the study and concluded that their approval was not required (reference number 2015/1107/REK North). The Norwegian Centre for Research Data (NSD) approved the study with regard to the procedures related to the use of local records to identify participants, data collection and data privacy (e.g. de-identification and anonymity) and obtaining informed consent (reference number 2015/43788/3/KS).




