Introduction
Ageing of the world's population is becoming one of the most significant social transformations of the 21st century (United Nations, 2017). These transformations will involve great changes in family structures, in society, economics, the job market and the demand for services. According to a United Nations report, the proportion of older adults will double by 2050 and triple by 2100. Europe shows the same trend as the worldwide population: older adults, making up 28.8 per cent of the population in 2015, will increase to 49 per cent in 2050, and the 80–89-year-old population in particular rises from 5.5 per cent in 2015 to 12.7 per cent in 2050 (Eurostat, 2018).
These data foretell problems in the years to come in relation to health-care needs, pensions and social protections for this population group. Consequently, measures must be found for maintaining quality of life in this ageing group, as well as for preventing functional decline and situations of dependency (García, Reference García2014; Manfredi et al., Reference Manfredi, Midão, Paúl, Cena, Duarte and Costa2019). Support, independence and self-management in older adults must be maintained for as long as possible.
When observing the ageing population, we find that their main concerns are loss of autonomy and independence in their day-to-day life (Liu et al., Reference Liu, Luo, Tang and Wong2018). Functional disability is defined as loss of the ability to carry out activities of daily living (ADLs) independently (Pérès et al., Reference Pérès, Verret, Alioum and Barberger-Gateau2005; Albert et al., Reference Albert, DeKosky, Dickson, Dubois, Feldman, Fox, Gamst, Holtzman, Jagust, Petersen, Snyder, Carrillo, Thies and Phelps2011), and can be assessed by measuring the person's ability to carry out such activities (Calero-García and Lendínez, Reference Calero-García and Lendínez2015).
According to the scientific literature, functional performance of older adults is closely related to their cognitive status (Cano-Gutiérrez et al., Reference Cano-Gutiérrez, Bordaz, Reyes-Ortiz, Arciniegas and Samper-Ternent2017). The loss of cognitive abilities has been shown to have an important impact on the ability of older adults to carry out ADLs (Rozo et al., Reference Rozo, Rodríguez, Montenegro and Dorado2016; Huang et al., Reference Huang, Zhang and Wang2019). Thus, neuropsychological impairment, above all in executive functions and memory, is correlated with functional limitations in ADLs (Farias et al., Reference Farias, Park, Harvey, Simon, Reed, Carmichael and Mungas2013) both in normally ageing persons (Farias et al., Reference Farias, Mungas, Reed, Harvey and DeCarli2009), and in persons with mild cognitive impairment (Jefferson et al., Reference Jefferson, Byerly, Vanderhill, Lambe, Wong, Ozonoff and Karlawish2008) or dementia (Razani et al., Reference Razani, Casas, Wong, Lu, Alessi and Josephson2007). This leads to greater dependence and reduced quality of life (Mograbi et al., Reference Mograbi, de Assis Faria, Fichman, Paradela and Lourenço2014).
An especially significant finding in this area is that of a critical window for intervention: the time period when an older adult presents mild functional limitations but is still independent in their ADLs. During this period of time, the application of cognitive training can hold back advancement of the disability (Willis et al., Reference Willis, Tennstedt, Marsiske, Ball, Elias, Koepke, Morris, Rebok, Unverzagt, Stoddard and Wright2006; Rebok et al., Reference Rebok, Ball, Guey, Jones, Kim, King, Marsiske, Morris, Tennstedt, Unverzagt and Willis2014) confirming the idea that training in cognitive functions at this time can improve an older adult's functional capacity in their day-to-day life (Greenaway et al., Reference Greenaway, Duncan and Smith2013; Jacoby et al., Reference Jacoby, Averbuch, Sacher, Katz, Weiss and Kizony2013).
Several reviews on the effect of cognitive interventions in older adults have been published in the past decade (Mewborn et al., Reference Mewborn, Lindbergh and Miller2017; Bahar-Fuchs et al., Reference Bahar-Fuchs, Martyr, Goh, Sabates and Clare2019; Simon et al., Reference Simon, Castellani, Belleville, Dwolatzky, Hampstead and Bahar-Fuchs2020). Cognitive stimulation programmes are shown to be effective, producing gains in the cognitive performance of older adults (Smart et al., Reference Smart, Karr, Areshenkoff, Rabin, Hudon, Gates and Hampel2017; Bhome et al., Reference Bhome, Berry, Huntley and Howard2018; Lobbia et al., Reference Lobbia, Carbone, Faggian, Gardini, Piras, Spector and Borella2018; Gavelin et al., Reference Gavelin, Lampit, Hallock, Sabatés and Bahar-Fuchs2020), with positive effects maintained over periods of two months to five years (Kelly et al., Reference Kelly, Loughrey, Lawlor, Robertson, Walsh and Brennan2014; Chiu et al., Reference Chiu, Chu, Tsai, Liu, Chen, Yang and Chou2017). The concern is whether the effects of such training programmes become transferred to overall cognitive functioning, and if they produce functional gains in the daily life of the older adults, since this ought to be the final objective of all these programmes. Some studies have found the transfer of cognitive training benefits to certain functional domains (Hampstead et al., Reference Hampstead, Gillis and Stringer2013). Nevertheless, transfer and generalisation to daily life have proven to be complicated and minimal (Borella et al., Reference Borella, Carretti, Riboldi and De Beni2010; Richmond et al., Reference Richmond, Morrison, Chein and Olson2011) and findings indicate that transfer to daily life is quite difficult (Tardif and Simard, Reference Tardif and Simard2011; Von Bastian et al., Reference Von Bastian, Langer, Jäncke and Oberauer2013).
Today there are data to suggest that adapted training programmes, where levels of difficulty and types of tasks are fitted to the individual, seem to yield better results in terms of transfer (Cândea et al., Reference Cândea, Cotet, Stefan, Valenas and Szentagotai-Tatar2015; Calero, Reference Calero, Fernández-Ballesteros, Benetos and Robine2019).
For all these reasons, it seems of interest to involve the professional care-givers of older adults as active agents who would incorporate cognitive training into the daily life of these persons. This might be a way to improve the transfer of training results and meet the goal of more autonomous older adults who are more independent in their day-to-day life. From this perspective, professional care-givers are considered facilitators of cognitive training transfer, helping to generalise its effects, since they would be able to help maintain it over time.
Certain care-giver training programmes already exist, but most are oriented to improving the quality of life of the care-givers themselves – to lighten their load, improve their frame of mind, offer them self-help resources, lower their stress, etc. (Harrad and Sulla, Reference Harrad and Sulla2018; Cheng et al., Reference Cheng, Au, Losada, Thompson and Gallagher-Thompson2019) – but not to how they can help the older adults manage their own health or be autonomous, even though care-givers often ask for this type of training (Hartmann et al., Reference Hartmann, Mills, Pimentel, Palmer, Allen, Zhao, Wewiorski, Sullivan, Dillon, Clark, Berlowitz and Snow2018). In recent years an increasing number of programmes have been designed to train professional care-givers in care-giving skills. In this line, we find programmes that train professional care-givers in care strategies, communication, knowledge of disease and intervention guidelines for eliminating behaviour problems (Goyder et al., Reference Goyder, Orrell, Wenborn and Spector2012; Spector et al., Reference Spector, Revolta and Orrell2016; Robertson et al., Reference Robertson, Cooper, Hoe, Hamilton, Stringer and Livingston2017; Bravo-Benítez and Navarro-González, Reference Bravo-Benítez and Navarro-González2018; Sanjuán et al., Reference Sanjuán, Calero, Abarca and Navarro2018).
The STAR programme, for example, was designed to train professional care-givers to address problems of interaction with older adults and to reduce affective and behavioural anxiety (Teri et al., Reference Teri, Huda, Gibbons, Young and Van Leynseele2005). Other programmes (Broughton et al., Reference Broughton, Smith, Baker, Angwin, Pachana, Copland, Humphreys, Gallois, Byrne and Chenery2011; Bird et al., Reference Bird, Anderson, MacPherson and Blair2016; Mills et al., Reference Mills, Pimentel, Palmer, Snow, Wewiorski, Allen and Hartmann2017) seek to implement strategies for improved communication, such as the MESSAGE programme (facilitating communication in dementia) and RECAPS (improving memory and cognition in dementia). Both of these have shown positive effects in memory and communication, in the care-giver's knowledge and ease, and in increased quality of life in the older adults (Broughton et al., Reference Broughton, Smith, Baker, Angwin, Pachana, Copland, Humphreys, Gallois, Byrne and Chenery2011; Robertson et al., Reference Robertson, Cooper, Hoe, Hamilton, Stringer and Livingston2017). A recently published programme, called CUIDA-2 (Calero et al., Reference Calero, Navarro, Sanjuán, Calero-García and Ortega2017), trains care-givers in communication strategies and cognitive, physical and emotional stimulation. The programme is based on the model of person-focused care and uses mediation-based methodology, with guidelines for care-givers on how to train older adults as part of their day-to-day care-giving (Calero et al., Reference Calero, Navarro, Sanjuán, Calero-García and Ortega2017).
The general objective of the present research was to evaluate the effectiveness of the cognitive stimulation part of the CUIDA-2 programme in improving the functional status of older adults. The specific objectives were (a) to verify any improvement of functional skill in older adults under the care of professional care-givers who had received the training, compared to a control group whose care-givers did not receive this training, and (b) to analyse whether – in addition to functional improvement – there was cognitive improvement in older people under the care of professional care-givers who had received training, compared to a control group whose care-givers did not receive the training.
Method
Participants
Older adults
The participants in this study were 69 care-dependent older adults (37 in the treatment group and 32 in the control group). The mean age of the persons selected was 84.12 years (standard deviation (SD) = 7.47). Men represented 14.5 per cent of the sample and women represented 85.5 per cent. Regarding the level of education, 21.7 per cent were unschooled, 62.3 per cent had elementary schooling, 10.1 per cent had secondary or vocational training, and 5.8 per cent had higher education or university training. Thirteen per cent were married, 10.1 per cent were single, 4.3 per cent were divorced and 72.5 per cent were widowed. The older adults were selected from three day care centres (59.4%) and four residences (40.6%) in the province of Granada, southern Spain. Characteristics of the two groups of older adults are shown in Table 1. As can be observed, there were no significant between-group differences.
Table 1. Characteristics of the older adults
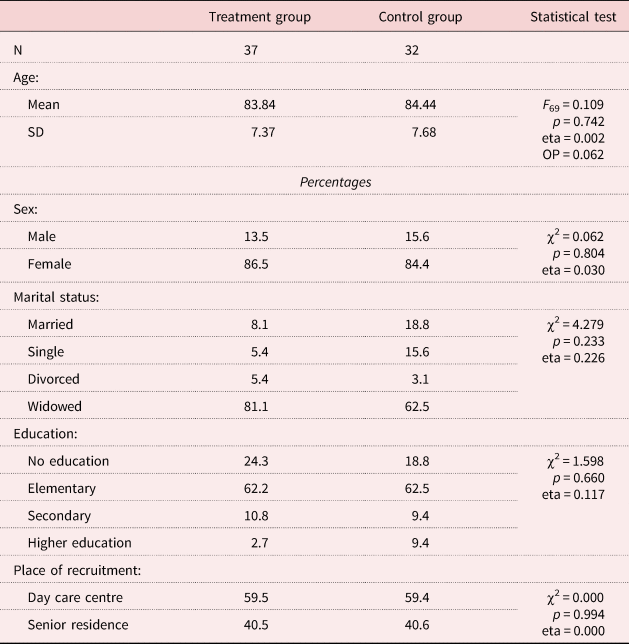
Notes: SD: standard deviation. eta: effect size. OP: observed power.
The inclusion criteria for the older adults were: age 55 or older, receiving care, living at a senior residence or attending a senior day care centre for a minimum of 40 hours per week, not suffering from dementia, having given their informed consent and having initial Barthel Index scores of less than 75 points. Using these criteria, we sought to select older adults who presented mild functional limitations but were still independent in their ADLs. This population sector, according to the literature reviewed in the Introduction, are the ones who can benefit most from a cognitive intervention for improving their functional ability (Greenaway et al., Reference Greenaway, Duncan and Smith2013; Jacoby et al., Reference Jacoby, Averbuch, Sacher, Katz, Weiss and Kizony2013; Rebok et al., Reference Rebok, Ball, Guey, Jones, Kim, King, Marsiske, Morris, Tennstedt, Unverzagt and Willis2014).
The treatment group (N = 37) received care from professional care-givers who were trained in communication strategies, cognitive and functional stimulation, and increased autonomy, through the CUIDA-2 programme (Calero et al., Reference Calero, Navarro, Sanjuán, Calero-García and Ortega2017) (see description in the Intervention Programme section). The control group (N = 32) was composed of older adults selected from the same centres and matched in age and gender to the treatment group, such that there were no significant differences in any socio-demographic variable between participants in the two groups.
Professional care-givers
There were 44 participating care-givers (22 for the treatment group and 22 for the control group). The mean age for all care-givers was 37.36 years (SD = 10.73). Male care-givers represented 18.2 per cent of the sample and female care-givers represented 81.8 per cent. Regarding the level of education, 4.5 per cent had elementary schooling only, 65.9 per cent had secondary or vocational training, and 29.5 per cent had higher education or university training. At the work locations where this investigation was carried out, the average number of adults under the care of each professional care-giver was 34.5 (SD = 23.63). For the purposes of this research, however, this load was reduced to 12 older adults per care-giver. In the case of the treatment group, although each care-giver was assigned 12 older adults to care for on a daily basis, they applied the programme with only one or two of the people assigned to them. Specifically, 15 care-givers applied the programme with two older adults each, and seven care-givers applied the programme with one person. The care-givers in the control group were also assigned 12 older adults to care for on a daily basis. From this set of older adults, a group of 32 persons homogeneous with the treatment group was randomly selected.
The mean number of years they had been working in the care of older adults was 9.64 years (SD = 6.16). Finally, professional care-givers were selected from the same centres as the older adults; these were the care-givers responsible for providing care to the older adult participants. All of them were professional care-givers, that is, they were employees at the centres where this research was carried out. Regarding workplace distribution, 68.2 per cent worked at senior residences and 31.8 per cent in adult day care centres.
There were no significant differences in any of the above variables between care-givers in the treatment group and care-givers in the control group, as shown in Table 2, which presents characteristics of the two groups.
Table 2. Characteristics of the professional care-givers
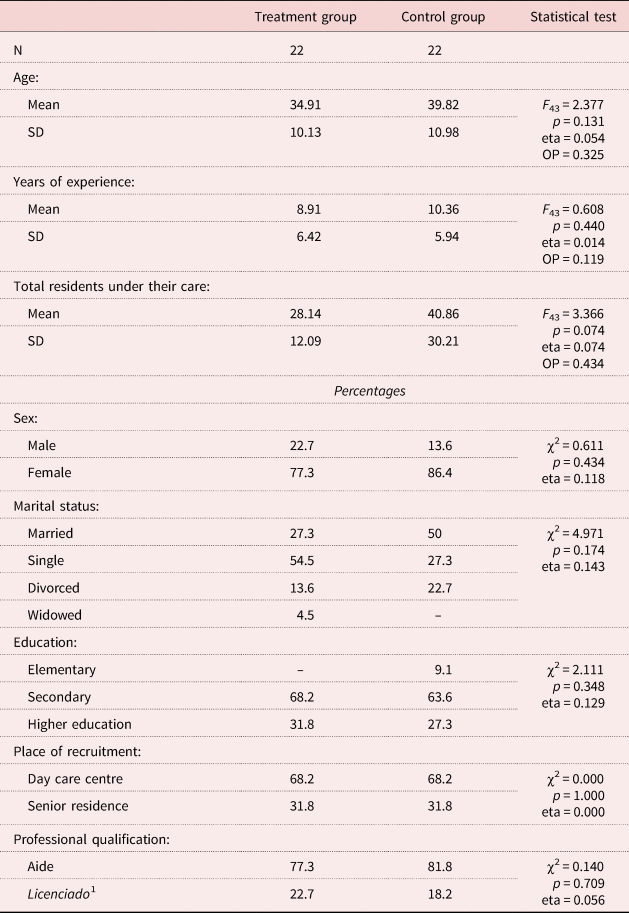
Notes: SD = standard deviation. eta = effect size. OP: observed power. 1. Having a university degree.
The inclusion criteria for the professional care-givers were: (a) to be the care-giver of older adults who had been selected for this study, and therefore, an employee of the centres where the older adults were recruited, and (b) give informed consent to participate, involving a commitment to take the training course and apply it to the persons under their care in the residential facility or day care centre where they worked.
Assessment instruments
The following instruments were used for the older adults:
• Socio-demographic data sheet: here we recorded participant data pertaining to personal variables, medical and social information, and their preferences and hobbies.
• The Barthel Index (Granger et al., Reference Granger, Dewis, Peters, Sherwood and Barrett1979 version, adapted to Spanish by Cid-Ruzafa and Damián-Moreno, Reference Cid-Ruzafa and Damián-Moreno1997) was used to measure the level of dependency. This scale assesses the person's functional ability based on ten items that analyse their ability to carry out basic activities like getting up from a chair or a bed, personal hygiene, bathroom use, going outside, going up and down stairs, dressing and sphincter control. Scores can range from 1 (completely dependent) to 100 (fully independent). Internal consistency presents an alpha coefficient between 0.86 and 0.92 and inter-judge reliability is between 0.84 and 0.97. This test has proven to be a good predictor of mortality and can detect gains or decline in aspects of the individual's functional skills. Optimal structural validity and internal consistency have been demonstrated in a population similar to our study population (Bernaola-Sagardui, Reference Bernaola-Sagardui2018).
• The following instruments were used for the cognitive part:
(1) Mini-Mental State Examination (MMSE; Folstein et al., Reference Folstein, Folstein and McHugh1975). For this research we used the Spanish adaptation (Mini-Examen-Cognoscitivo (MEC); Lobo et al., Reference Lobo, Ezquerra, Gómez, Sala and Seva1979). The MEC is sensitive to detecting cognitive status in an older Spanish population with a low level of education (Manubens et al., Reference Manubens, Martínez-Lage, Martínez-Lage, Larrumbe, Murazabal and Martínez1998). The final score is normally used as a global index in processes such as cognitive impairment and dementia. We used standards developed for the Spanish population (Manubens et al., Reference Manubens, Martínez-Lage, Martínez-Lage, Larrumbe, Murazabal and Martínez1998) to establish criteria for the presence or absence of cognitive impairment. The validity of these standards was confirmed in a previous study (Calero et al., Reference Calero, Navarro, Robles and García-Berbén2000).
(2) The Procedimiento de Evaluación Clifton para Ancianos – Escala cognitive (CAPE) (Fernández-Ballesteros and Guerrero, Reference Fernández-Ballesteros and Guerrero1984), a Spanish adaptation of the Clifton Assessment Procedure for the Elderly – Cognitive Scale (Pattie and Gilleard, 1979). This instrument contains two scales, one cognitive and one behavioural. The present study made use of the cognitive assessment scale. Its test–retest reliability falls between 0.79 and 0.90, and between 0.61 and 0.69 for the information and orientation scale and for the mental skill scale, respectively. It also has convergent validity with Wechsler's Memory Scale, showing a 0.90 correlation between the two.
For the care-giver assessment, we used a data sheet to collect information on all the care-givers’ socio-demographic and work-related variables. Care-givers for the treatment group were also assessed using the Star Staff Feedback Questionnaire (SSFQ) (Goyder et al., Reference Goyder, Orrell, Wenborn and Spector2012) which assesses the degree to which the training was useful and satisfactory for the care-givers.
Intervention programme
The care-giver training programme consisted of applying the cognitive stimulation module of the CUIDA-2 programme (Calero et al., Reference Calero, Navarro, Sanjuán, Calero-García and Ortega2017). This application included theoretical training in three modules that covered: (a) person-focused care, (b) communication strategies, and (c) mediated cognitive training strategies. The first module explains the working approach of the Person-Centered Care Model (Brownie and Nancarrow, Reference Brownie and Nancarrow2013), encouraging care-givers to follow these principles in their work, so that the older adult under their care would improve in autonomy and decision-making ability. The second module explains the communication strategies needed for communicating with older adults, in order to facilitate the interchange and the relationship. The final module explains and works on mediated cognitive training strategies (Tzuriel, Reference Tzuriel2013) for the different cognitive functions that decline in older adults. This model is more extensive and seeks to equip professional care-givers with the tools they need to stimulate older adults on a daily basis and thus ensure better cognitive maintenance. This module develops cognitive trainers that follow a mediated approach for analysis, training and generalisation of basic cognitive skills. This train-the-trainer module was administered to the treatment care-giver group in two two-hour group sessions, followed by 50 hours of hands-on training that consisted of individual, on-the-job practice, supervised by psychologists who were experts in the programme. During these 50 hours, the care-givers implemented the programme by integrating it into their regular interaction with the older adults under their care. Supervision was conducted by direct observation and by weekly meetings to answer questions and help the professional care-givers fill in their log of activities carried out with each older adult. In these weekly logs, care-givers had to plan in advance what activities they were going to carry out with the older adult, and once completed, record how they were carried out and how the older adult responded.
Procedure
First, permission was obtained from the Research Ethics Committee at the University of Granada. The residential facilities and day care centres which had agreed to participate in the research were then contacted and the final sample was formed as described above.
Once we had obtained informed consent from the facilities, the care-givers and the older adults, the following phases where implemented. We started with the initial assessment of care-givers and older adults from the control and treatment groups, and afterwards administered the training programme in small-group format to the care-givers in the treatment group. Once the training course was finalised, the care-givers of the treatment group put into practice what they had learned, working with the older adults for three months under the supervision of the research team. This supervision consisted of direct observation during the first week, weekly meetings to answer questions and helping care-givers with their running log of activities. The log was a weekly register where the care-giver had to first plan the activities they were going to carry out with the older adult, and afterwards record how they were done and how the older adult had responded. The care-givers of the control group, however, did not participate in any training nor were they supervised in their daily work. After the programme application, we administered a post-treatment assessment of all the care-givers and older adults. Finally, a follow-up was carried out and both groups were re-assessed six months after the post-treatment assessment.
Design
We used a quasi-experimental design with repeated measures (pre, post and follow-up) of the different dependent variables. The statistical analyses were analyses of variance, following the univariate and multivariate analysis of the general linear model (GLM) for inter-group comparisons, and repeated-measures analysis through the general linear model in order to check for intra-group differences at three assessment times, as well as the effect size of the study variables. Data analyses were performed using SPSS 19.0 for Windows.
Results
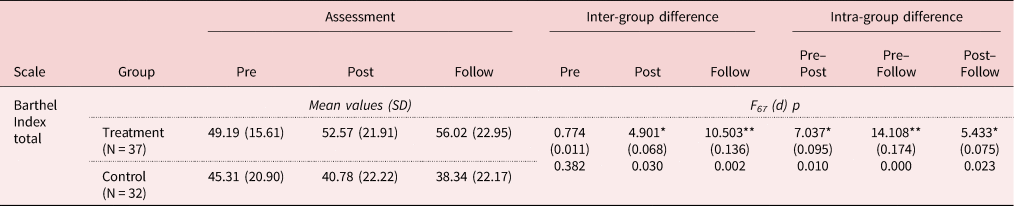
In order to check whether the care-giver training programme produced functional improvement in members of the treatment group, inter-group and intra-group differences in the Barthel Index were analysed using an GLM 3 × 2 analysis (Time × Group).
As seen in Table 3 and Figure 1, no significant inter-group differences in the Barthel Index were observed in the pre-assessment (F 67 = 0.774; p = 0.382; d = 0.011), but there were significant inter-group differences in the post-treatment assessment (F 67 = 4.901; p = 0.030; d = 0.068) and in the follow-up (F 67 = 10.503; p = 0.002; d = 0.136), when the control group obtained lower scores than the treatment group (Table 3 and Figure 1).
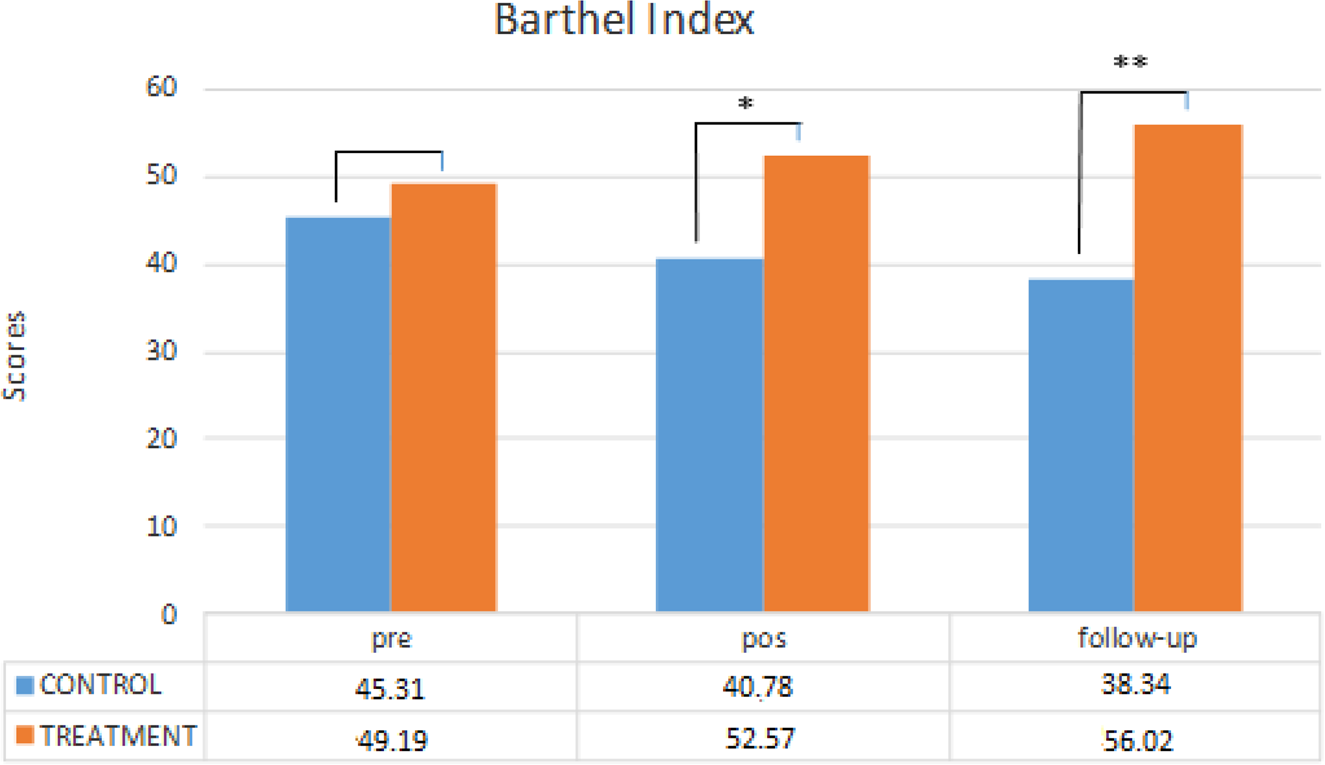
Figure 1. Significant difference between the treatment group and the control group on the Barthel Index at three different assessment times.
Notes: pre: pre-treatment. pos: post-treatment.
Significance levels: * p < 0.05, ** p < 0.01.
Table 3. Means and F scores obtained by the older adults in the control and treatment groups in the Barthel Index, in the pre-treatment (Pre), post-treatment (Post) and follow-up (Follow) assessments
Notes: SD: standard deviation. d: effect size.
Significance levels: * p < 0.05, ** p < 0.01.
Regarding intra-group differences in the Barthel Index (see Table 3), significant differences were found between the initial assessment and the post-treatment assessment (F 67 = 7.037; p = 0.010; d = 0.095), between the post-treatment and the follow-up (F 67 = 7.905; p = 0.000; d = 0.174) and between the initial assessment and the follow-up (F 67 = 14.108; p = 0.023; d = 0.075), with treatment group scores increasing significantly over time, while control group scores declined from one assessment to the next.
To check whether the care-giver training programme brought about cognitive improvement in the treatment group, inter-group and intra-group differences in the Barthel Index were analysed for the three assessments (see Table 4), based on changes in the MMSE and CAPE using an MLG 3 × 2 analysis (Time × Group).
Table 4. Means and F scores obtained by the older adults in the control and treatment groups on the Mini-Mental State Examination (MMSE) and the Clifton Assessment Procedure for the Elderly – Cognitive Scale (CAPE), in the pre-treatment (Pre), post-treatment (Post) and follow-up (Follow) assessments
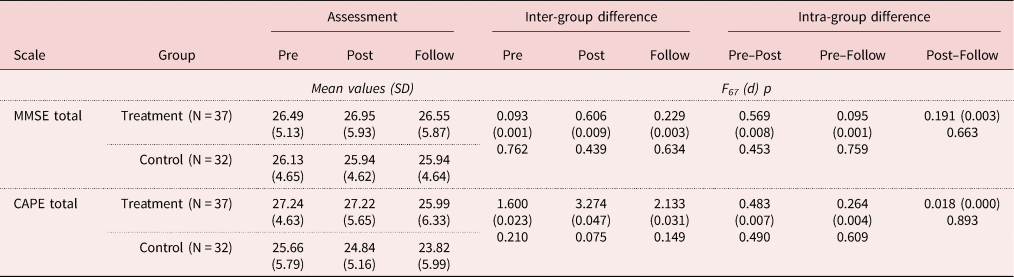
Notes: SD: standard deviation. d: effect size.
As for the MMSE, no significant inter-group differences were observed at any assessment time, neither in the pre-assessment (F 67 = 0.093; p = 0.762; d = 0.001) nor in the post-assessment (F 67 = 0.606; p = 0.439; d = 0.009) nor in the follow-up (F 67 = 0.229; p = 0.634; d = 0.003) (see Table 3). Neither were there any significant intra-group differences between the initial assessment and the post-treatment assessment (F 67 = 0.569; p = 0.453; d = 0.008), between the post-assessment and the follow-up (F 67 = 0.191; p = 0.663; d = 0.003) or between the initial assessment and the follow-up assessment (F 67 = 0.095; p = 0.759; d = 0.001) (Table 4).
Regarding the CAPE test, as can be seen in Table 4, no significant inter-group differences were obtained at any assessment time, neither in the pre-assessment (F 67 = 1.600; p = 0.210; d = 0.023) nor in the post-treatment assessment (F 67 = 3.274; p = 0.075; d = 0.047) nor in the follow-up (F 67 = 2.133; p = 0.149; d = 0.031). Neither were there any significant intra-group differences between the initial assessment and the post-treatment assessment (F 67 = 0.483; p = 0.490; d = 0.007), between the post-assessment and the follow-up (F 67 = 0.018; p = 0.893; d = 0.000) or between the initial assessment and the follow-up assessment (F 67 = 0.264; p = 0.609; d = 0.004) (Table 4).
Nonetheless, even though the results were not statistically significant, one could observe that MMSE scores in the treatment group remained stable throughout the pre-, post- and follow-up assessments, and the CAPE scores remained stable from pre- to post-assessment; while these scores declined in the control group (see Table 4).
We conducted a qualitative analysis of how care-givers from the treatment group rated the training received. Their responses to the SSFQ showed that they positively rated the usefulness of the programme modules, producing a mean of 4.9 (SD = 0.301) on a scale from 0 to 5. The care-givers also indicated that participation in the programme had been a very positive experience and had helped increase their knowledge, satisfaction and sense of confidence on the job. For these reasons, they expressed their willingness to participate again in this type of programme. They also indicated that the main drawback encountered in implementing the programme was the short amount of time they have for attending to each adult.
Discussion
The general objective of this study was to evaluate whether functional improvement was produced in older adults who receive care from professionals that participated in a care-giver training programme.
Information provided by the Barthel Index was our basis for establishing the functional skill of the older adults, thereby verifying whether this skill was improved/maintained in the older adults who received care from the trained care-givers. The Barthel Index thus represented mastery of the skills being targeted by the care-givers. The intervention programme was designed to be implemented in the course of daily activity, such that functional skill would be worked on constantly through cognitive exercises. The Barthel Index was then expected to detect differences produced by the training.
The present study confirms that the older adults whose professional care-givers participated in the cognitive training programme significantly improved in functional skill with respect to the older adults whose care-givers did not receive this training. The ability of cognitive training to improve ADL functional ability in older adults is thus verified (Mograbi et al., Reference Mograbi, de Assis Faria, Fichman, Paradela and Lourenço2014; Lau et al., Reference Lau, Parikh, Harvey, Huang and Farias2015). The increase in score was produced on every scale of the Barthel Index. This finding agrees with previous literature showing that cognitive training can be generalised to functional skills (Greenaway et al., Reference Greenaway, Duncan and Smith2013; Cândea et al., Reference Cândea, Cotet, Stefan, Valenas and Szentagotai-Tatar2015). For instance, regarding the association between executive functions and functional performance, previous studies found that executive functions could predict performance in instrumental ADLs (Bell-McGinty et al., Reference Bell-McGinty, Podell, Franzen, Baird and Williams2002). Another research group (Cahn-Weiner et al., Reference Cahn-Weiner, Farias, Julian, Harvey, Kramer, Reed and Chui2007) investigated episodic memory and executive functions in older adults and found severe executive dysfunction to be associated with a more rapid decline in ADLs. Similarly, a strong association was found between ADLs and performance on a verbal fluency task in a sample of persons with dementia (Maseda et al., Reference Maseda, Lodeiro-Fernández, Lorenzo-López, Núñez-Naveira, Balo and Millán-Calenti2014). All these studies confirm that cognitive functions are closely tied to a person's daily functioning.
In light of the significantly improved scores attained by older persons with initial Barthel Index scores equal to or less than 75 (meaning they were dependent), their functional skill has clearly benefited from the training. Moreover, these gains that represent progress towards greater independence in ADLs (Nirmalan, Reference Nirmalan2010) were maintained over six months. These results indicate fulfilment of our purpose of obtaining functional improvements through cognitive training. Transfer from the training to the older adult's daily life, and maintenance over time, have been demonstrated. The purpose of involving the professional care-givers was for them to make the connection between the cognitive task and day-to-day functioning. The care-givers were able to adapt the different cognitive tasks and adjust them to each older adult's environment and needs (Apóstolo et al., Reference Apóstolo, Cardoso, Rosa and Paúl2014; Williams et al., Reference Williams, Herman and Smith2014). In our opinion, this individualised adaptation of the cognitive training (in the older adult's own setting and with objects and materials from their own daily life) was what helped produce this transfer of benefits from the cognitive training.
As for the cognitive tests, we found no significant differences between any of the assessments. We did observe, however, that cognitive scores in the treatment group remained stable from one assessment to the next, while scores in the control group were declining over the course of this study, even if the changes were not statistically significant. These results are in the line of studies indicating that cognitive interventions help to maintain and improve cognitive functioning in older adults (Bhome et al., Reference Bhome, Berry, Huntley and Howard2018; Lobbia et al., Reference Lobbia, Carbone, Faggian, Gardini, Piras, Spector and Borella2018; Oltra-Cucarella et al., Reference Oltra-Cucarella, Ferrer-Cascales, Clare, Morris, Espert, Tirapu and Sánchez-SanSegundo2018).
The tests chosen to assess cognitive changes (MMSE and CAPE) contained tasks very distant from those that were trained; this may be responsible for the lack of significant changes at the cognitive level. Nonetheless, our results show that cognitive status was maintained in the older adults whose care-givers were trained in the programme.
Finally, we wished to ascertain whether the care-givers who received the training increased their knowledge and were satisfied with the programme received. All the care-givers rated the programme very positively, expressing general satisfaction with the programme, finding it useful, and that it increased their knowledge, their satisfaction with their work and their sense of confidence on the job. The following aspects of the training were indicated as most useful in their daily work: ascertaining the areas of greatest impairment in each adult, identifying exercises for these areas and learning how to perform them. Likewise, they reported having greater knowledge about the adults in their care, greater empathy towards them and greater ability to cope with them when they were worried or depressed. The main limitation noted, with regard to putting the programme into practice, was the short amount of time that they can dedicate to each of the older adults under their care. This problem suggests a need to increase care-giving resources and the number of professional care-givers assigned to work with older adults at these centres, hence, a lower ratio of older adults per care-giver. In this way, lack of time would no longer be a hindrance to proper care of the older adult.
Generally speaking, this training programme – which teaches care-givers how to communicate with the older adults, how to detect their deficits and to work on the deficient areas from an approach of person-centred care – produces transfer of cognitive benefits to the older adult's day-to-day functioning. Decrease in dependency is achieved, since the older adults’ ADL functional ability has increased, and hence their autonomy and independence.
We were also able to verify that the effects were generalised, that is, maintained over time, given that the improvements continued to be found six months after the intervention.
Even so, this study presents certain limitations that should be taken into account in future research studies. One of these is the small sample size, which may be responsible for the lack of significance of some results. Another limitation would be the greater proportion of women in our sample, not allowing us to analyse possible gender-related differences. It would be interesting to analyse the differences in cognitive and functional benefits according to gender or other socio-demographic variables that may affect them.
This study brings to light the importance of the figure of professional care-giver in maintaining the older adult's functional capacity. Data obtained here show that involving the professional care-giver in the training of an older adult is a novel aspect that contributes to generalisation and transfer of results.
Financial support
This work was supported by the Ministry of Education, Government of Spain (grant number FPU15/03966).
Ethical standards
Permission was obtained from the Research Ethics Committee at the University of Granada.







