Introduction
eHealth
Europe's health and care systems face serious challenges such as ageing citizens with complex care needs, health workforce shortages and continuing urbanisation (European Commission, 2018). Public spending on health and long-term care is expected to continue to rise in all European Union (EU) member states (European Commission and Economic Policy Committee, 2016). In The State of Health in the EU report (European Commission, 2017), it was concluded that the health-care systems need fundamental rethinking and innovative solutions to become more resilient, accessible and effective in providing quality care in Europe. Digital solutions for health and care, referred to as eHealth, are envisioned to have the potential to increase the wellbeing of millions of citizens and to change radically the way health and care services are provided (European Commission, 2018). The benefits of increased eHealth are multifaceted, and eHealth supports continuity of care across borders, promotes health and prevents disease, supports the transition of the health system to new care models, i.e. more centred on people's needs, and enables a shift from hospital-centred systems to more community-based and integrated care structures. However, there have also been concerns regarding technology's availability and usability, especially with older age groups (Heart and Kalderon, Reference Heart and Kalderon2013; Airola et al., Reference Airola, Rasi and Airola2020).
Even though the expectations are high for the potential of eHealth across Europe, EU member states differ greatly with respect to their welfare regimes (Kvist, Reference Kvist2012) and care systems. Lutz (Reference Lutz2016) describes a spectrum of European care regimes. On one end are the traditional care regimes linked to conservative gender regimes, often exemplified by Germany and the southern European countries, while on the other end we have the more equal care and gender regimes, such as the Scandinavian countries (Lutz, Reference Lutz2016). Even though placing European countries in clusters or regimes is problematic, some scholars agree that it is possible to identify different European care regimes (Anttonen and Sipilä, Reference Anttonen and Sipilä1996; Daly, Reference Daly2001; Bettio and Plantenga, Reference Bettio and Plantenga2004; Lister et al., Reference Lister, Anttonen, Gerhard, Bussemaker and Williams2007).
Studies on eHealth have shown the benefits of the technology used in care and promoting wellbeing. Our focus in this article is on older adults, and technology has proven to be beneficial in supporting health assessment and care, and overall wellbeing in this population (e.g. Bradford et al., Reference Bradford, Van Kasteren, Zhang and Karunanithi2018). However, problems associated with eHealth are connected to issues like lost privacy and the frivolous use of the devices (e.g. Cook et al., Reference Cook, Randhawa, Sharp, Ali, Guppy, Barton, Bateman and Crawford-White2016; Lie et al., Reference Lie, Lindsay and Brittain2016), and monitoring devices also risk threatening the good relationship between carers and those being cared for, i.e. carers might get more information than they need or more information than the person is willing to share (Pols, Reference Pols2017). In this article, eHealth refers to the technological solutions designed to be used in elderly care, for example, solutions to promote living at home, remote solutions and older adults’ self-care. eHealth is close to other concepts such as gerontechnology (Delello and McWhorter, Reference Delello and McWhorter2017), assistive technology (Fischer et al., Reference Fischer, David, Crotty, Dierks and Safran2014), mHealth (Spann and Stewart, Reference Spann and Stewart2018), telecare (Bentley et al., Reference Bentley, Powell, Orrell and Mountain2018) and welfare technology (Östlund et al., Reference Östlund, Olander, Jonsson and Frennert2015). Our aim is to analyse and compare Italian, Finnish and Swedish policy documents in terms of how eHealth, digitalisation of care, older adults, sparsely populated areas and care responsibilities are talked about, and what kinds of digital landscapes of care are created as well as what consequences this has on our perception of older people and care.
Conceptual framework: digital landscape of care
To understand the possible similarities and differences in Italian, Finnish and Swedish eHealth policies, we will use the concept of digital landscape of care. The concept of digital landscape of care (Milligan and Wiles, Reference Milligan and Wiles2010; Lindberg and Carlsson, Reference Lindberg and Carlsson2018) is used in this article to analyse how eHealth is understood as part of older adults’ lives and care. The concept refers ‘to the complex embodied and organizational spatialities that emerge from and through the relationships of care’ (Milligan and Wiles, Reference Milligan and Wiles2010: 740). Milligan and Wiles’ (Reference Milligan and Wiles2010: 739) concept is comprehensive, including socio-structural processes and structures, experiences and practices of care, which include issues like support, services, ethics, morals, responsibilities and the spatial politics of care.
Lindberg and Carlson (Reference Lindberg and Carlsson2018) have directed Milligan and Wiles’ concept towards eHealth, and they talk about a digital landscape of care. Lindberg and Carlson (Reference Lindberg and Carlsson2018) have studied ‘virtual health rooms’ and the ideological beliefs that are included in the introduction of digital care in sparsely populated areas in Sweden. They found that eHealth is often welcomed with optimism, and it is believed to improve the quality of care, reduce care costs and encourage older people to take care of themselves. Lindberg and Carlson (Reference Lindberg and Carlsson2018) point out that the discourses of patient participation, active ageing and rurality as a problem are part of the eHealth talk, and that such discourses need to be assessed critically.
Studies on the use of technology in elder-care have examined older adults’ perceptions, attitudes, acceptance and learning of technologies (Peek et al., Reference Peek, Wouters, van Hoof, Luijkx, Boeije and Vrijhoef2014; Claes et al., Reference Claes, Devriendt, Tournoy and Milisen2015: Tsai et al., Reference Tsai, Shillair and Cotten2017), technologies’ effectiveness and feasibility (Khosravi and Ghapanchi, Reference Khosravi and Ghapanchi2016; Barbosa Neves et al., Reference Barbosa Neves, Franz, Judges, Beermann and Baecker2017), and barriers and enablers to technology use (Bentley et al., Reference Bentley, Powell, Orrell and Mountain2018; Spann and Stewart, Reference Spann and Stewart2018). Research results have indicated the positive effects of technology use in old age in terms of reduced falls (Tchalla et al., Reference Tchalla, Lachal, Cardinaud, Saulnier, Bhalla, Roquejoffre, Rialle, Preux and Dantoine2012), improved health management (Bradford et al., Reference Bradford, Van Kasteren, Zhang and Karunanithi2018), increased independence and safety (Stokke, Reference Stokke2016), reinforced social relationships, reduced social isolation, social and spatial barriers, and loneliness (Winstead et al., Reference Winstead, Anderson, Yost, Cotten, Warr and Berkowsky2013; Chen and Schulz, Reference Chen and Schulz2016; Barbosa Nevese et al., Reference Barbosa Neves, Franz, Judges, Beermann and Baecker2017; Bradford et al., Reference Bradford, Van Kasteren, Zhang and Karunanithi2018; Antunes et al., Reference Antunes, Oliveira, Hudec, Crocetta, Ferreira de Lima Antao, de Almeida Barbosa, Guarnieri, Massetti, Garner and de Abreu2019), and decreased need for institutional care (Riikonen et al., Reference Riikonen, Mäkelä and Perälä2010). Technology use can create and enhance ties with friends and family (Barbosa Neves et al., Reference Barbosa Neves, Franz, Judges, Beermann and Baecker2017; Bradford et al., Reference Bradford, Van Kasteren, Zhang and Karunanithi2018), give pleasure (Østensen et al., Reference Østensen, Gjevjon, Øderud and Moen2017), and enable older people to produce knowledge and exchange it with others (Delello and McWhorter, Reference Delello and McWhorter2017). In health care, technology has been proven to be useful in managing health issues or coping with symptoms (Kerssens et al., Reference Kerssens, Kumar, Adams, Knott, Matalenas, Sanford and Rogers2015; Bradford et al., Reference Bradford, Van Kasteren, Zhang and Karunanithi2018) and as a medium for therapy (Choi et al., Reference Choi, Hegel, Marti, Marinucci, Sirrianni and Bruce2014), in rehabilitation (Shulver et al., Reference Shulver, Killington, Morris and Crotty2017), and in health status assessment, monitoring and self-management (Bond and Worswick, Reference Bond and Worswick2015; Brown et al., Reference Brown, Colville and Pye2015). Technology has also proven to be beneficial for homebound people (Mitzner et al., Reference Mitzner, Stuck, Hartley, Beer and Rogers2017) by providing alternative ways for people to connect with other people (Kilpeläinen and Seppänen, Reference Kilpeläinen and Seppänen2014; Hasan and Linger, Reference Hasan and Linger2016; Tsai et al., Reference Tsai, Shillair and Cotten2017).
However, negative outcomes of the use of technology have also been identified, such as loss of trust, safety and privacy (Lie et al., Reference Lie, Lindsay and Brittain2016; Yusif et al., Reference Yusif, Soar and Hafeez-Baig2016; Pols, Reference Pols2017), stigmatisation and increased dependency (Bentley et al., Reference Bentley, Powell, Orrell and Mountain2018), concerns related to costs (Spann and Stewart, Reference Spann and Stewart2018), and the uselessness and unsuitability of certain technologies (Cook et al., Reference Cook, Randhawa, Sharp, Ali, Guppy, Barton, Bateman and Crawford-White2016). Also, negative outcomes such as losing the possibility to meet physically other people (Frennert et al., Reference Frennert, Forsberg and Östlund2013; Currie et al., Reference Currie, Philip and Roberts2015; Shulver et al., Reference Shulver, Killington, Morris and Crotty2017) and care professionals in person (Zwijsen et al., Reference Zwijsen, Niemeijer and Hertogh2011; Kim et al., Reference Kim, Gollamudi and Steinhubl2017) and concerns about the way surveillance changes people's way of life (Bradford et al., Reference Bradford, Van Kasteren, Zhang and Karunanithi2018) have been reported.
Objectives and rationale for the work
In this article, three EU member states – Italy, Finland and Sweden – function as our cases in illustrating different governments’ approaches to eHealth, with a special focus on the ageing European citizen in the rural context. Both Finland and Sweden belong to the more equal care and gender regimes, while Italy is expected to have a more traditional care regime linked to a conservative gender regime. We are interested in how these countries differ in their eHealth policy approaches and how notable these differences are. The objective of the study is to contribute data for the analysis of the social construction of eHealth. The final goal is to also provide relevant information for policy making in rural contexts in terms of the development of eHealth projects. Bringing an international comparative perspective, the three countries participating in the research provide a diverse landscape in terms of digitalisation of eHealth services, population density, ageing, and cultural norms and beliefs. By studying rural eHealth with a socio-cultural approach and in a comparative perspective, it is possible to go beyond a mere technological perspective and to understand how cultural capital, care ideology and territorial context are related to different uses, needs, competences, enthusiasm and fears about digital care for older adults, and how that differs in different national settings.
Contextual information: demographic profiles, health systems and eHealth use
Before presenting the results of our comparative analysis, we offer some useful background information to help understand the different national contexts in which the analysed policy documents were written. In the presentation of the characteristics of the three countries, we will focus in particular on the following three aspects: the demographic profile (in particular the number of older people and their health condition), the health system, and the level of digitisation and eHealth use.
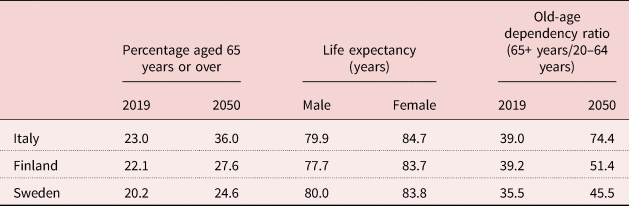
The three countries in our sample are all characterised by substantial populations of citizens over 65 years and by rapid ageing processes (Table 1).
There are profound differences in ‘how’ one gets older. To understand the similarities and differences between the three countries, we use the active ageing index (AAI), which is a synthetic index that describes the ageing processes starting from the weighting of different indicators of the state of wellbeing of older adults. An elaboration of the AAI produced by the United Nations Economic Commission for Europe (2019) divides the European countries into four clusters according to the scores achieved in the different indicators of the AAI. Italy belongs to the cluster of Mediterranean countries that score low in the four domains of the AAI (Employment; Participation in society; Independent, healthy and secure living; and Capacity and enabling environment for active ageing). Sweden and Finland belong to the cluster of the Nordic countries and present well above average results in three domains, and only slightly higher values in the domain of Independent, healthy and secure living (Table 2). Some notable differences between Sweden and Finland are that life expectancy is a bit higher in Sweden, particularly among men, and that expenditures on social services are higher in Sweden, while older adults in Finland use eHealth more than their Swedish counterparts.
Table 2. Active ageing index indicators
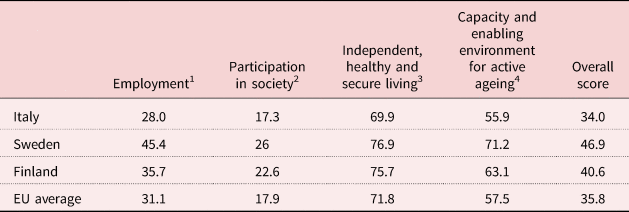
Notes: 1. Indicators: employment rate among 55–74 year olds. 2. Indicators: voluntary activities; care to children and grandchildren; care to infirm and disabled people; political participation. 3. Indicators: physical exercise; access to health services; independent living; financial security; physical safety; lifelong learning. 4. Indicators: remaining life expectancy at age 55; share of healthy life expectancy at age 55; mental wellbeing; use of information and communication technologies; social connectedness; educational attainment. EU: European Union.
Source: United Nations Economic Commission for Europe (2019).
The three countries in our sample have free of cost or low cost, universal and decentralised health systems. Overall, the Italian health system is considered efficient (Organisation for Economic Co-operation and Development (OECD), 2019) and ensures good access to high-quality health-care services at relatively low costs, although there are considerable differences between the regions in the country. The main challenges for the Italian health system are to improve the co-ordination of health-care services for the growing segment of the population affected by chronic diseases and to reduce disparities in access to treatment. In 2017, health-care expenditure per capita in Italy was 15 per cent lower than the EU average. About 75 per cent of health-care expenditures are financed with public funds, while the remainder is mainly paid by patients. The National Health Service is decentralised and organised on a regional basis. The central government puts part of the general tax revenues into the health-care services financed with public funds, defines the package of health services (the so-called Essential Levels of Assistance) and performs a general management role. Each region is responsible for the organisation and delivery of health services through accredited public and private hospitals.
According to the OECD (2019), the Finnish health system is complex and decentralised, and is governed at the national and local levels. At the national level, the Ministry of Social Affairs and Health is responsible for health policies with the support of a network of experts and consultative bodies. Local authorities (over 300 municipalities) play a key role in the provision of health services, and they finance and organise primary care and hospital care. In the past 15 years, the Finnish political system has attempted to implement health and social care reforms. The proposed reforms aim at greater centralisation of resources and responsibilities at the regional level with the aim of improving equality of access to care and controlling costs: ‘While high levels of decentralisation allow the health system to adapt to the needs of a dispersed population, it generates some inequalities and inefficiencies’ (OECD, 2019). Per capita health-care expenditure in Finland has increased in the past 10 years and is slightly above the EU average. Public funding covers 75 per cent of all health-care expenditure, which is somewhat lower than the EU average (79%). The patients pay most of the remaining expenses.
The Swedish health service system is decentralised and provides universal coverage. Sweden has the third-highest health expenditure in the EU as a percentage of Gross Domestic Product and the third-highest per capita expenditure. Most of the health-care expenditure is financed with public funds (84%), which is somewhat higher than the EU average (79%). The national government is responsible for regulation and oversight, while the regions are responsible for funding, purchasing and providing health services. Regions are responsible for primary and specialist care, while municipalities are responsible for care for elderly people, care for people with physical and mental disabilities, rehabilitation services, school health care, home care and social assistance. Health-care costs are mainly paid through local taxes, along with contributions from the national government. Over the last decades, the Swedish health-care system has gone through a significant marketisation, with increased numbers of private care actors envisioned to increase efficiency and quality of care (Blomqvist, Reference Blomqvist2004; Stolt and Winblad, Reference Stolt and Winblad2009, Stolt et al., Reference Stolt, Blomqvist and Winblad2011; Andersson and Kvist, Reference Andersson and Kvist2015).
The three countries in our sample are characterised by profound differences in terms of the diffusion and use of information and communication technologies (ICT). In particular, Italy differs from the Nordic countries in terms of a generally lower level of innovation. However, in terms of the spread of broadband connections, the three countries do not have big differences, and 94.8 per cent of households in Sweden, 93.1 per cent of households in Finland and 83.7 per cent of households in Italy are reached by a fast internet connection (Eurostat, 2019). When comparing the use of the internet, however, the gap begins to grow. The proportion of individuals between 16 and 74 years old who regularly use the internet (at least once a week) are 95.4 per cent in Sweden, 93.4 per cent in Finland and 73.9 per cent in Italy (Eurostat, 2019). In terms of digital skills, the gaps between the Nordic countries and Italy become significant, and the proportions of individuals with above basic levels of digital skills are 50.1 per cent in Finland and 46 per cent in Sweden, but only 22 per cent in Italy (Eurostat, 2019). The gaps become even deeper if the analysis focuses on different age groups, and while internet use is more equally distributed in the populations of Sweden and Finland, Italy suffers from a dramatic age-related divide. Swedish and Finnish citizens between 65 and 74 years of age are regular internet users, at 80.5 and 74.7 per cent, respectively, compared to 39.2 per cent of Italians of the same age. A further element that differentiates Italy from Sweden and Finland is the use of eGovernment services, i.e. the use of technological communication devices to provide social services to citizens. In this case, the gap between Italy and the Nordic countries is even more marked. In the past 12 months, only 23.4 per cent of Italians have used an eGovernment service compared to 87.3 per cent of Finns and 86 per cent of Swedes (Eurostat, 2019).
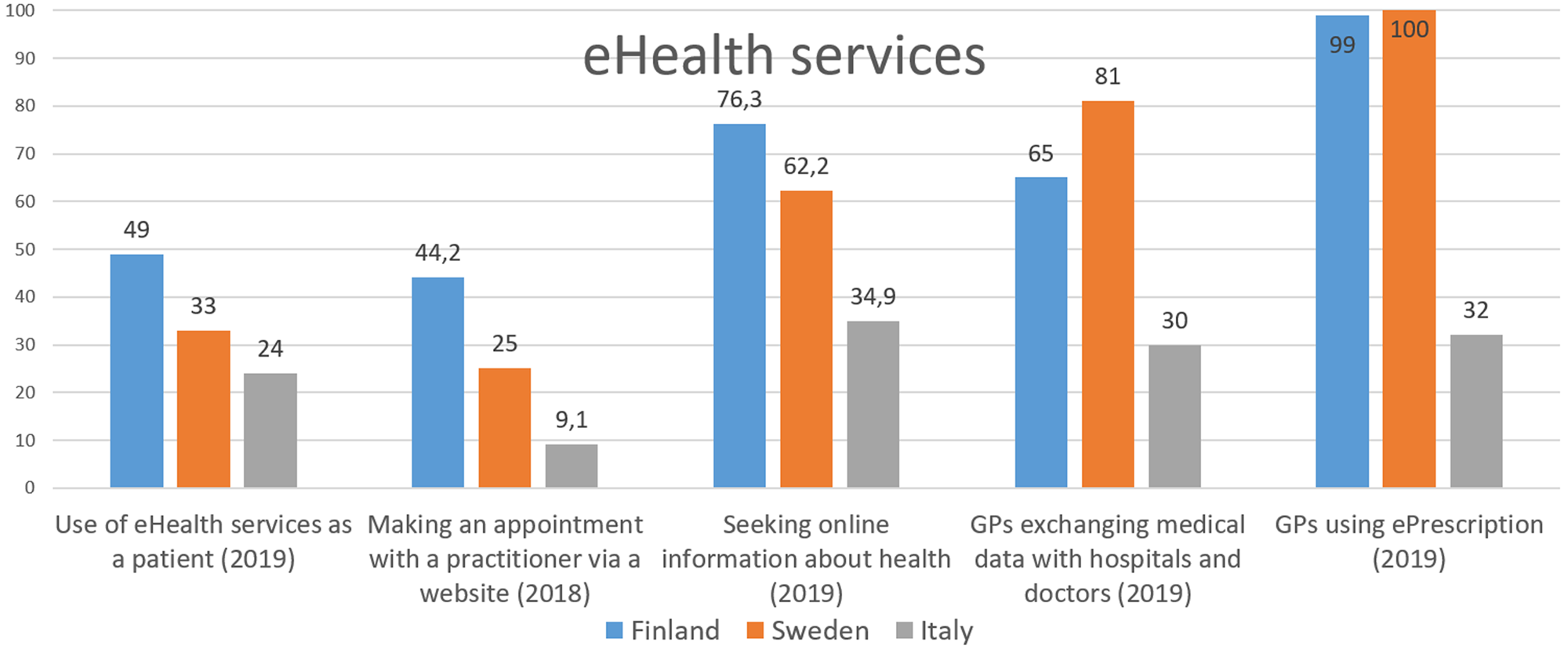
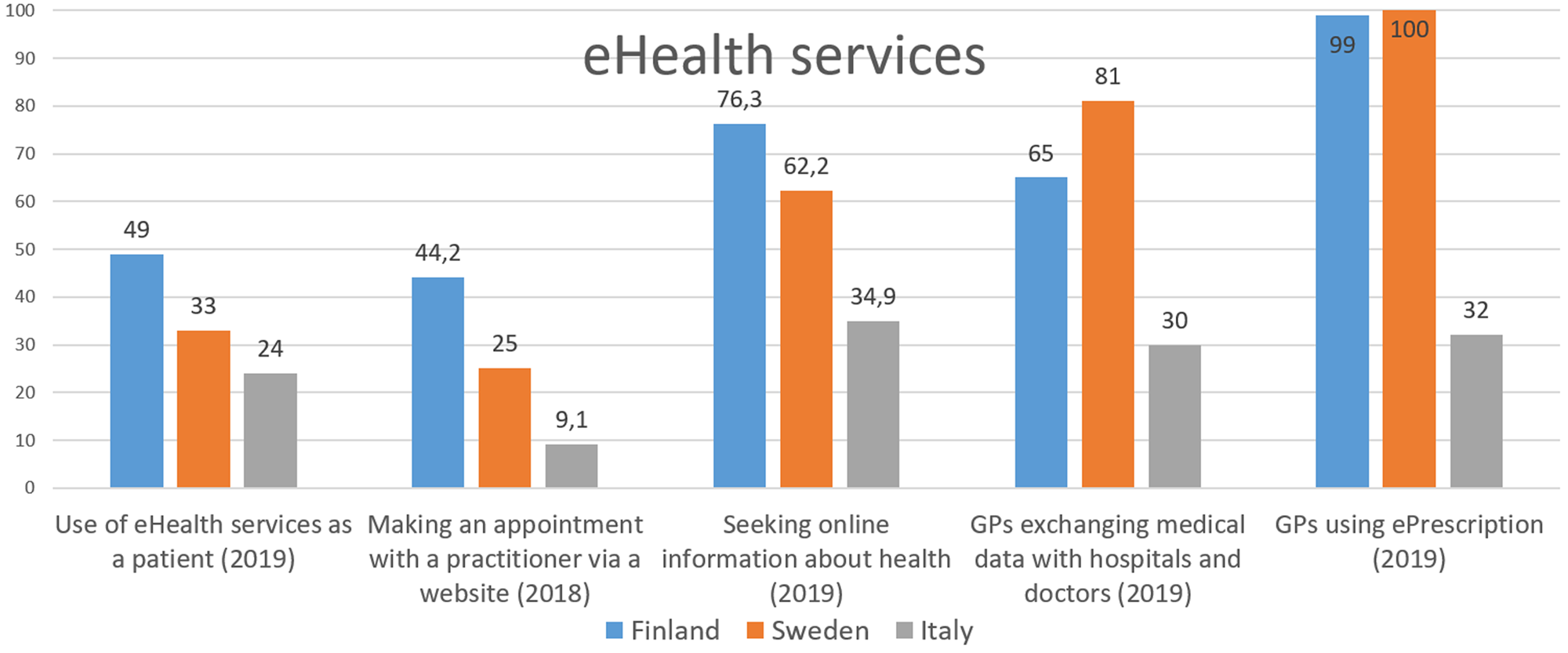
Going deeper into the issue of digital services for eHealth, the differences between Italy and the Nordic countries are also significant. These data are to be contextualised both in terms of lack of eHealth services and in the low digitisation of users, primarily users over 65, including both patients and doctors, and 49 per cent of people in Finland, 33 per cent of people in Sweden and 24 per cent of people in Italy have used online health and care services without physically going to a health-care facility (e.g. by getting a prescription or a consultation online) (Eurostat, 2018, 2019). The gaps between Italy, Sweden and Finland get deeper when looking at the digitisation of general practitioners and the digitisation of the health-care system in general (Figure 1).
Methodology
Sample
Our data consist of national and regional policy documents for promoting eHealth among older adults in Italy, Finland and Sweden. Our sample comprises the most relevant national and regional policy documents about eHealth, ageing, rurality and fragility published between 2009 and 2019.
The Italian sample includes 59 documents, including four documents from national government agencies, one from the Ministry of Innovation, one from the Ministry of Economic Development, seven from the Ministry of Health and 46 from regional administrations. The Finnish sample includes 21 documents, including four laws, two government programmes and four documents from government agencies, six from the Ministry of Health and Social Affairs, two from the Ministry of Finance, one from the Ministry of Transport and Communications and two from the County of Lapland. The Swedish sample includes 15 documents, including 13 Swedish government official reports and two written communications from the government (see the online supplementary material).
Analysis
Starting from the conceptual discussion on the digital landscape of care and using a grounded theory approach (see Strauss and Corbin, Reference Strauss, Corbin, Denzin and Lincoln1994), our qualitative content analysis (see Hsieh and Shannon, Reference Hsieh and Shannon2005) involved three steps: (a) mapping and selecting national and regional policy documents for promoting eHealth among older adults from 2009 to 2019 in the three countries; (b) identifying broad areas of themes and creating a common list of key concepts (‘older people’, ‘ageing’, ‘active ageing’, ‘health’, ‘eHealth’, ‘the rural/remote’, ‘care responsibilities’, ‘technologies’, ‘ICTs’); and (c) applying a non-automated content analysis (Elkins et al., Reference Elkins, Spitzer and Tallberg2019) to map whether/how these key concepts were defined in each document in the sample. At the end of the analysis process, we identified three macro-topics on which to articulate the comparison in the framework of a digital landscape of care, namely the role of eHealth technologies, the role of the rural dimension and the constituted care responsibilities that we discuss further in the following sections.
Results
The role of eHealth technologies
The documents we analysed highlight the positive role of technology in promoting more efficient health care and elder-care, but there are also some critical and problematic issues raised:
The use of technological innovations in patient management is an opportunity to improve the efficiency and sustainability of continuity of care. (Progetto per la Salute. Piano Sanitario Regionale [Health Project. Regional Health Plan], 2019: 305, Italy)
Reducing or curbing health-care costs is a cross-cutting priority in the three countries. In particular, it is underlined that, with the ageing population, elder-care will become one of the largest social service costs. It is, therefore, no surprise to note that in many of the analysed documents the role of eHealth is connected to economic efficiency (Sanyal et al., Reference Sanyal, Stolee, Juzwishin and Husereau2018). The development of digital services allows both the reduction of costs related to the management and communication of information between hospitals, doctors and patients (e.g. the reservation systems for visits) and the reduction of costs of care through self-care, self-service, self-help and self-monitoring.
In this sense, the technologies of communication and health save resources that are otherwise destined, on the one hand, to the development of ‘physical’ structures for the management of health information (offices, counters, telephones, employees) and, on the other, to the provision of medical assistance. In fact, if patients, through technologies, can self-monitor their state of health at home, such monitoring does not have to be done by a doctor in an expensive care facility.
The use of technological innovations in patient management is seen as an opportunity to improve the efficiency and sustainability of ‘continuity of care’ by being able to treat a patient for longer at home instead of in the hospital, thus reducing the costs of hospitalisation. Finally, eHealth is included in the broader opportunities represented by the health industry (technologies, pharmaceuticals, digital services, biotechnologies), and eHealth could be part of the economic strategy of a country. In particular, some Italian documents underline how, in terms of employment and the volumes of turnover produced, the health industry represents a strategic sector for the economic development of the country.
According to the documents analysed, a primary target of health technologies is and will be older people. This is true for reasons of efficiency and efficacy. In terms of efficiency, older citizens are the largest target of the national health systems and therefore are necessarily the ones who are targeted in efforts to achieve significant savings in public expenditures. In terms of efficacy, older people are more likely to have chronic diseases, and health technologies are particularly effective in the care of the chronically ill and those in need of continuous assistance. In particular, technology supports older people's independent living and helps avoid hospital stays for chronically ill people. One way to increase ageing citizens’ utilisation of new technologies is suggested to be to engage them in the design and testing of health-care technologies.
Not all of the analysed texts speak equally of the possible limits and risks associated with the implementation and use of eHealth. In general, the approach to technology is positive, optimistic and deterministic, and not all documents leave room for the possible negative implications of the use of health technologies or for possible limitations in general.
In particular, in the Italian documents the limitations and risks for end users are not emphasised, and most of the documents discuss the advantages (efficiency and efficacy) of eHealth for the health system and less space is given to the implementation of eHealth for end users. In the Finnish and Swedish documents, limitations and possible risks associated with the development of eHealth services aiming towards older users are more articulated, including issues related to integrity, trust, limited economic resources among older people, and digital competence and confidence. Ethical concerns are addressed in some Finnish and Swedish policy texts, and eHealth and welfare technology is advised to be used with caution and ethical issues kept in mind:
Confidence in digital services is enhanced by engaging in an active social debate on data protection, digital exclusion, self-determination and ethics. (Eheä yhteiskunta ja kestävä hyvinvointi. Sosiaali- ja terveysministeriön tulevaisuuskatsaus [An intact society and sustainable welfare. Ministry of Social Affairs and Health future report], 2018, pp.16–17, Finland)
In its report on ethical aspects of robots and surveillance in the care of the elderly, the Swedish Medical and Ethical Council (SMER) has recommended that an assessment of the consequences the monitoring can have for ethical values must be made before monitoring measures are taken in the care of the elderly. In particular, the Council stresses that it is important that a balance is achieved between the benefits of monitoring and the intrusion on the privacy of the individual that the monitoring entails. The measure should be taken in such a way as to minimise the intrusion. If welfare technology is used, it should be for the good of the older person, and careful analysis and considerations are required about it can violate the older adults’ right to privacy and dignity. (Så stärker vi den personliga integriteten [How to strengthen personal integrity], 2017: 126, Sweden)
Other ethical issues in eHealth and elderly users are related to the potential replacing of offline service and more generally the ethical limits of a ‘digital-first’ approach, and digital services risk being perceived as services that ‘replace’ the opportunities for offline and personal face-to-face contact.
According to previous research, welfare technology has the potential to increase safety and security, give greater independence, and facilitate participation and social contacts, and thus the value of virtual contact should not be underestimated (Bradford et al., Reference Bradford, Van Kasteren, Zhang and Karunanithi2018). Despite the many proclamations on the centrality of eHealth, the analysed documents offer few elements to understand what the policies should include for improving the use of health technologies among citizens. The Italian documents in particular emphasise public strategies to support private demand and the purchase of eHealth services, but there is no reflection on the accessibility or costs to purchase technologies. The only generic reference to policy that stimulates the use of technologies is the general need to connect and digitise areas of the country that currently have connection difficulties or that do not have access to the internet. In particular, the Italian documents that include eHealth within the reflection on the country's innovation and digitalisation (e.g. the local implementation of the European Digital Agenda 2020) indicate the increase in the spread of broadband and the adoption of digital technologies as a prerequisite for the development of eHealth policies. In the Swedish and Finnish documents, there are attempts to describe more specific policies and actions that would favour the use of eHealth services, but only a few generic examples are given, such as a tax reduction for information technology services in the home or through encouraging the use of online services through a reduction of traditional channels of access to health care.
The rural issue
In Finland and Sweden, the most rural areas are in the northern parts of the country, while in Italy the mountains are the most remote areas. In rural areas in each country, the population density is lower than in other parts of the country, and there are long distances and travel times from sparsely populated residential areas to municipal centres and services. In addition, sparsely populated areas are ageing more rapidly than other parts of the countries and care needs are higher. eHealth is considered to be one solution to overcoming the distance gap in all three countries. However, ageing and declining rural areas are contradictory to the optimistic expectations on ICT and eHealth.
In all three countries, the idea of equality and equal services for all people, despite where they live, is emphasised highly:
All regions should be able to offer the same service and equal care to all citizens, but it cannot be expected to be designed in the same way everywhere, depending on, for example, changing conditions in sparsely populated and large cities. (God och nära vård [Good and close care], 2017: 69, Sweden)
In the documents, eHealth is seen as a tool to promote equity of access to health care for all citizens, even in more remote areas. However, in the policy documents it is stated that the population cannot expect all health and social services to be performed in the same way, particularly in sparsely populated areas. In the Swedish policy text the concept of ‘close care services’ is introduced as a redefinition of what might count as a care encounter, enabling even sparsely populated areas to offer equal care and social services to all citizens. Traditionally, a care encounter has been understood as a physical meeting between the patient and the care professionals in a care facility, and with eHealth solutions more of the everyday care can be done digitally from the home. The technological solutions are seen as an answer to guarantee that everyone in the population has an opportunity to have their care needs met – citizens have the opportunity to communicate electronically with service providers regardless of their place of residence, and electronic solutions ensure equal access to services in sparsely populated areas. Universal access to care means offering the same standard of care to patients living in cities or in isolated communities:
The current rather one-sided focus on the traditional mediation logic ‘physical meeting in health care’ must be shifted to include other forms of interaction with the patient. The patient's needs and opportunities need to be better met by health care. The technical possibilities are great today to meet needs without physical meetings, but the technology needs to be spread so that everyone in the population has the opportunity to have their care needs met in this way. (Effektiv vård [Efficient care], 2016: 363, Sweden)
As local services are being closed due to austerity policies, there is an increased risk of inequalities in access to adequate health care, particularly in areas with large ageing populations. The analysed policy documents suggest that digitalisation creates opportunities for primary care to develop services that create greater accessibility for patients, enable remote monitoring and monitoring in the home, and streamline work methods and processes for sharing information between care-givers. To some extent, geographical distance is suggested to be compensated for through technical solutions.
There are regional differences and regional diversification in service supply, and municipalities and regions have different starting points and resources to guarantee services. Inequality and segregation of residential areas involve security risks, and rural areas are widely seen as a place for the diffusion of digital solutions. In addition, different areas have their own strengths, which can be emphasised by strengthening regional and local decision-making and co-operation. eHealth is one solution to strengthening rural areas with a strong dispersion of population density. The virtual communications network between citizens and primary care services can use ICT in many ways, and the eHealth services should mainly be provided in areas defined as ‘internal or rural areas’ that are disadvantaged from a geographic point of view.
Rural areas are often not very interesting for private and commercial service producers. The size of the municipality affects the number of ICT solutions that are available and the number of ICT-skilled professionals, including both health-care providers and ICT support personnel, and thus these areas need public intervention for the diffusion of technologies. Rural hospitals and service centres can use broadband to provide care and medical skills identical to those available in units in urban centres. According to the policy documents, eHealth services can offer new opportunities for public service in sparsely populated areas because the service can be provided without the patient having to travel to obtain care. However, remote areas can, from the viewpoint of care services, be challenging. In Italy, for example, a specific mortality and morbidity gap still characterises populations in mountainous areas, especially for tumours and cardio-cerebrovascular diseases. Sparsely populated and remote areas in general face obstacles of low diffusion of ICT, digital divide, interoperability, lack of ICT devices, and lack of digital skills among older adults and health and social care workers.
Care responsibilities
In all three countries, the responsibility to guarantee the supply of needed care is on public actors, be they at the state or regional level. In Finland and Sweden, the right to needed care and services is written into the constitution and elder-care legislation:
The obligation of the municipality is to take care of the wellbeing, health and functional capacity and independent performance of its elderly population and to ensure the social and health services needed by the elderly (2§). (Laki ikääntyneen väestön toimintakyvyn tukemisesta sekä iäkkäiden sosiaali- ja terveyspalveluista [Act on Supporting the Functional Capacity of the Older Population and on Social and Health Services for Older Persons] (980/2012), Finland)
Municipalities are responsible for providing care and services according to the needs of their inhabitants. In guideline documents, it is stated that citizens should be supported in taking responsibility for their own wellbeing, meaning that both society and the individual must take equal responsibility. In Italy, the regions are by law responsible for health care and social services, and the regions have broad autonomy in defining health guidelines. Regional health systems have unequal performance and, being partially funded by local taxation, the wealthier regions have more developed health systems.
In all three countries, de-hospitalisation and ageing in place are emphasised. The grounds for this development are twofold. On the one hand, care and services are increasingly being delivered at home in order to reduce health and social care costs and to increase user comfort. On the other hand, older adults themselves wish to stay in their own home for as long as possible. For example, Italy is moving from a model that includes a small hospital in every medium-sized city to the de-hospitalisation and transformation of hospitals into local health-care centres and the transformation of private homes into ‘nursing homes’. eHealth technologies are used to assist with the provision of care and services in homes and to allow remote online consultations with health specialists, and eHealth services are used as tools to guarantee communication between and continuity of care between specialists and primary care.
In Finland and Sweden, supporting family carers via home help services and combining work and family life are widely supported in the analysed documents. Despite the legislations’ emphasis on the responsibility of the municipalities, the actual responsibility of family members is strongly interwoven into the care of older adults with care needs (Zechner and Valokivi, Reference Zechner and Valokivi2012). Families carry out most of the care responsibilities (Ulmanen and Szebehely, Reference Ulmanen and Szebehely2015), and there is reason to assume that the relatives of older people with great care needs must put significant efforts into organising and delivering their care. This is a major responsibility for these relatives:
Care responsibility can affect not only the physical and mental health of the relatives, but can also affect their opportunities to work, engage in leisure activities and recreation, and to maintain other important relationships. (Effektiv vård [Efficient care], 2016: 449, Sweden)
The versatility of service providers in the field will be taken into account, and different forms of care services, including family care and other intermediate solutions, will be further developed. (Pääministeri Sanna Marinin hallituksen ohjelma 2019 [Prime Minister Marin's Government Programme 2019], 2019: 159, Finland)
Studies on care show that co-ordination often fails for family carers, and they have few opportunities to be involved in the co-ordination of the care, and in many cases poor co-ordination leads to poorer care as well as an uncertain situation for the person in need of care. In addition, the relatives are often forced to take responsibility for the co-ordination of care (Szebehely et al., Reference Szebehely, Ulmanen and Sand2014). At the same time, it is more common among women than among men that caring leads to negative consequences in terms of the ability to uphold gainful employment and in terms of physical and mental health. Family care is also more common in lower-income groups (Ulmanen and Szebehely, Reference Ulmanen and Szebehely2015). There is no evidence to suggest that the proportion of care-givers is greater in northern Europe than southern Europe, although the scope of social care is narrower in southern Europe. In the Nordic countries and in the Netherlands, with extensive public funding, it is less common for families to provide intensive and time-consuming care efforts to their ageing relatives (Szebehely, Reference Szebehely2014).
In the documents, self-responsibility is emphasised:
[Territorial health services] must promote patient self-care and users’ awareness of their personal resources by trying to offer alternative visions to those of ‘dependency’. (Strategie aree interne Lazio [Internal areas strategies Lazio], 2019: 284, Italy)
The fact that the public administration is responsible for ensuring basic rights does not negate the responsibility of the individual for his/her choices (Sosiaalisesti kestävä Suomi 2020. Sosiaali- ja terveyspolitiikan strategia [Socially sustainable Finland 2020. Social and health policy strategy], 2011: 10, Finland)
The patient's ability to actively participate in and manage his own care needs to be strengthened. (Effektiv vård [Efficient care], 2016: 380, Sweden)
Self-care and digital self-care are seen as future solutions for meeting increasing care needs, but self-care and digital self-care cannot succeed without help from informal networks. Peer and family support are called for in the documents, and this call increases the digital care responsibilities of the informal network. However, if older persons do not receive this ICT support from informal carers, or they do not have family or support networks, they will be in an unequal position:
Peer support is a way of providing digital support by a number of organisations, especially older people's organisations … One major informal form of support for digital devices and services is support from friends and relatives. (Digituen toimintamalliehdotus. AUTA-hankkeen projektiryhmän loppuraportti. Valtiovarainministeriö [Ministry of Finance, Digital support policy proposal. Final Report of the AUTA Project Team], 2017: 17, 21, Finland)
eHealth is seen to open possibilities of digitalisation and new opportunities for rapid information transfer and opportunities to develop support systems for the health-care professions. Digitalisation also gives patients and their relatives new opportunities to become involved in care and brings the professionals and patients closer together. From an ethical perspective, the most important questions are how welfare technology can contribute to the ability of older people to be independent and can facilitate communication with relatives as well as with health-care staff and how such technology can increase older people's safety, health and wellbeing.
In Italy there is a growing role of pharmacies as principals not only for medical advice, but also as a place for the management of digital health activities. Pharmacies, given their widespread diffusion in urban and rural centres, are points of reference in the case of emergencies in the area and are a ‘technological’ node for the provision of services such as booking networks for visits to hospitals and surgery, downloading medical reports, receiving electronic prescriptions and managing the patient's electronic health record. Faced with the contraction in medical supplies and the number of general practitioners, pharmacies have become essential nodes of the ‘Territorial Health Information System’ developed by the regions:
The social function for health protection that rural pharmacies in particular perform in disadvantaged areas in order to protect the population and in particular the elderly, also assumes particular importance. (Progetto per la Salute. Piano Sanitario Regionale [Health Project. Regional Health Plan], 2019: 305, Italy)
Another example of extended care networks in Italy is the ‘family and community nurse’ who contributes to helping older inhabitants in the area live independently at home for as long as possible. A ‘community nurse’ model of taking charge of and supporting the older population functions as a connection between the older person, their family network, and the various professionals and eHealth services (general practitioners, specialists, hospitals and pharmacies, as well as governing bodies, associations and private individuals) in order to promote inclusion, health, and psychological and physical wellbeing.
The introduction of technology in older person's care involves new actors and professionals in the already-complex networks of care surrounding ageing adults. For example, children or grandchildren who are more familiar with technologies are asked to help more often, and formal care-givers sometimes assume their help. In addition, technology advisers might be new professionals in older persons’ care networks (Outila and Kiuru, Reference Outila and Kiuru2021). These changes might challenge the nature of family relationships as well as the quality of care, something that must be kept in mind. A Swedish study also showed how children and grandchildren are
strongly involved in nearly every stage of technology domestication, from appropriation (i.e. identifying the need, buying the item, and installing and adjusting it) to incorporation (i.e. choosing and downloading suitable apps, teaching how to use them, and solving technical problems). (Olsson and Viscovi, Reference Olsson and Viscovi2018: 324)
Olsson and Viscovi (Reference Olsson and Viscovi2018) point out that even though elderly Swedes have been accustomed to online activities for more than a decade, the need for continuous assistance seems to prevail also among experienced users.
Comments and concluding remarks: the landscape of eHealth care in policy documents
To understand the differences and similarities found in the three studied countries’ eHealth policy processes, we use the notion of digital landscape of care. The care of older adults is complex, relationally as well as spatially, bodily and organisationally (Milligan and Wiles, Reference Milligan and Wiles2010; Lindberg and Carlsson, Reference Lindberg and Carlsson2018). In understanding these complex relations, it is important to take into consideration socio-structural processes and structures, experiences and practices of care, as well as support, services, ethics, morals, responsibilities and the spatial politics of care. In Lindberg and Carlsson's (Reference Lindberg and Carlsson2018) analysis of eHealth and digital landscapes of care, they concluded that eHealth is often welcomed with optimism and that it is believed to improve the quality of care, reduce the costs of care and activate older adults in taking care of themselves, but they also concluded that these discourses need to be critically analysed. We found similar discourses in this study. All studied countries formulated eHealth as a mainly positive development, with an emphasis on increased economic efficiency and cost reduction in health care. eHealth is thus seen, in line with the general interpretation of digitalisation, as a tool capable of doing the same things as face-to-face services but at lower costs (see Sanyal et al., Reference Sanyal, Stolee, Juzwishin and Husereau2018).
In all three countries, increased digitalisation is seen not only as an opportunity, but also as a necessity to meet the increased austerity in the health-care system. It is also argued that eHealth will provide opportunities for a new care model that will increase user involvement and accessibility in health care. This care model is thought to be particularly beneficial for ageing populations, the chronically ill and those living in rural areas. eHealth is expected to facilitate older adults to remain in their homes longer, to avoid unnecessary and prolonged hospital stays, to increase safety and security, to reduce loneliness and social isolation, to provide opportunities to intervene against anticipated and preventable health deterioration, to assist in physical rehabilitation and medicine distribution, and to encourage physical activity. However, in the policy texts in all three countries it is pointed out that the digital competence and economic means, as well as mental and physical abilities, vary greatly among older adults. This is something that needs to be taken into consideration in relation to eHealth.
Digitalisation of health care can offer the opportunity to connect with the highest quality health services even if one lives far away from them or if one is unable to leave one's home. However, we find this eHealth discourse problematic because it mainly points to individual factors, such as individual competence or means, in relation to the digitalisation of elder-care. A greater reliance on digitalisation in elder-care and health care demands that the problems in digital infrastructures be addressed properly. Digital accessibility needs to be considered as a social right, particularly in rural areas, not just as an issue for the individual to take up or the market to take care of. There are some initiatives in the policy processes, such as tax rebates on ICT services and redefining the role of pharmacies, but especially from the rural perspective these are not enough.
These problematic questions could be found in all three studied countries. However, as could be expected due to the profound differences between the three countries, particularly between Italy and the Nordic countries, with respect to welfare organisation, territorial structuring and digitalisation among government agencies and citizens, there were also differences in the countries’ approaches to eHealth. One such example is that in the Italian documents there was hardly any problematisation of the impact of technological transformations in the health system, in the lives of older adults, or in the relationship with the health system and health-care professionals, while such discourses were emphasised in the Finnish and Swedish documents. In the Nordic documents, there was a reflection on both ethical issues and risks, such as technological dysfunctions on both the user and system levels (see also Pirhonen et al., Reference Pirhonen, Lolich, Tuominen, Jolanki and Timonen2020). The Italian documents seem less nuanced from this perspective. Instead, they accent the need for an optimistic push due to the lack of digitisation in remote areas of the country and the ageing sections of the population. The Italian policy is characterised by a techno-positive approach that mainly emphasises the positive sides of increased digitalisation, and it argues for the benefits for society, the health-care system and citizens, and in line with this there is an absence of problematic or more complex issues regarding eHealth. In the Nordic texts there are, for instance, discussions about user involvement, including both of ageing citizens and health-care professionals, in the early stages of the design processes of digitalisation, something that is only marginally described in the Italian texts.
Another major critical observation is the lack of consideration of the impact of increased digitalisation of health care on the care networks that surround older adults. Informal carers, family members and friends also need to be taken into consideration in the implementation of eHealth and the digitalisation of the care of older adults. When greater emphasis is put on the individual's responsibility for their own health care, a heavier care burden might land on the shoulders of significant others and informal carers. The cost reduction for the health-care systems might be made up for through rising care responsibilities for the families and informal care networks, along with increased inequalities in accessing elder-care (Szebehely, Reference Szebehely2014). This is a development that risks becoming even more problematic when such care networks of family and friends are missing or insufficient.
In light of our study, eHealth as a digital landscape of care needs to be evaluated from the perspective of the construction of a ‘proper’ care receiver and ‘reasonable’ care, as well as the power structures and rationales that lie behind these constructions. Studies (e.g. Schou and Hjelholt, Reference Schou and Hjelholt2019; Sundberg, Reference Sundberg2019) have pointed out how digitalisation is made to seem inevitable and how a ‘digital citizen’ (Schou and Hjelholt, Reference Schou and Hjelholt2019) is constructed to promote the legitimisation of digitalisation. Similarly to our study, Schou and Hjelholt (Reference Schou and Hjelholt2019) see digitalisation as being strongly connected to economically sound-looking politics in the sense of efficiency and flexibility. The construction of a ‘digital citizen’ also includes the idea of responsibilisation (see Juhila et al., Reference Juhila, Raitakari, Hansen Löfstrand, Juhila, Raitakari and Hall2017). In contrast to the inevitable nature of digitalisation, the making of a ‘digital citizen’ should be understood as a political figuration (Schou and Hjelholt, Reference Schou and Hjelholt2019).
Sundberg (Reference Sundberg2019) calls attention to how many eGovernment policies contain myths and visionary images about technology. According to Sundberg, current discourses on digitalisation represent views where technology dictates the conditions that lead us towards an inevitable technology-driven future. For example, issues such as digital divides are left in silence because the proposed solution to the problems presented in the policy is that everyone should embrace the technology. From the perspective of the digital landscape of care, the care of older adults is a complex and relationally as well as spatially, bodily and organisationally driven phenomenon, and it needs to be analysed thoroughly. Digitalisation of elder-care and eHealth needs to take into consideration the complexities that surround each older adult with care needs by asking questions about where they live, how they live and who is caring for them, and by addressing issues regarding the functionality and support of digital devices and the practicality of the digital infrastructure. Policy makers need to be less concerned with convincing reluctant older adults, their close relatives and grassroots-level professionals of the benefits of the eHealth and be more concerned about providing functional digital infrastructure and diminishing inequalities that exist in the field. Issues related to exclusion that should be addressed here are the first-level digital divide including physical and material access, the second-level digital divide including user skills and usage (van Deursen and Van Dijk, Reference van Deursen and Van Dijk2019), and the third-level digital divide including tangible outcomes of use, e.g. the use either resulting in benefits or not (van Deursen and Helsper, Reference van Deursen, Helsper, Robinson, Cotten, Schulz, Hale and Williams2015).
As we write this, we are in the middle of the COVID-19 pandemic crisis, which has affected us all but with particularly devastating and lethal consequences for the elderly and most vulnerable citizens. During the crisis, social distancing has become one main advised strategy, especially for older persons, and the pandemic has in some ways become a devastating stress test for digital solutions for health and care and shows how increased digitalisation in health care can contribute to preventing contagious diseases. Because we have studied policy documents on eHealth from the last 10 years in Italy, Finland and Sweden, we can conclude that this major societal challenge was not foreseen by these governments and policy institutions. Until now, the development of eHealth has been thought of as a slow digital transition process and not as a tool to offer care in the context of unexpected widespread ‘domestic isolation’. From this point of view, the COVID-19 pandemic will probably represent a fundamental watershed both for eHealth policies and for a general rethinking of new (digital) models of care.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0144686X21000945
Author contributions
All authors contributed equally to the text.
Financial support
This work was supported by the HARVEST Project which received funds under the JTC 2017 launched by Joint Programming Initiative (JPI) MYBL. JPI MYBL is supported by J-Age II. J-Age II is funded by Horizon2020, the EU Framework Program for Research and Innovation (grant agreement number 643850, ‘More Years, Better Lives’).
Conflict of interest
The authors declare no conflicts of interest.
Ethical standards
No ethical approval was needed (open-source policy data).