In the interest of road safety, driving license holders who suffer from a medical condition likely to affect fitness to drive must notify the Driver and Vehicle Licensing Agency (DVLA) and not drive. The Secretary of State for the Environment, Transport and the Regions (of the Department for the Environment, Transport and the Regions, DETR) has the responsibility, via his Medical Advisers at the Drivers Medical Unit of the DVLA, to ensure that all licence holders are fit to drive.
This paper explains the implications for road safety of psychiatric disorders in drivers. The medical standards discussed are based on legal requirements.
Importance of medical conditions to road safety
The causes of road traffic accidents (RTAs) are multi-factorial, and the degree to which a medical condition is involved is extremely difficult to establish. The available evidence suggests that medical conditions in drivers, with the exception of the effects of alcohol and drugs, are a small factor in RTAs causing death or injury. They may contribute to only 1–2% of accidents (Reference TaylorTaylor, 1995). However, there have been no well-conducted large studies attempting to establish this relationship. Police forces have no obligation to collect data or notify the DVLA when a medical condition is considered contributory, although they frequently do so. There is, therefore, no clear picture of the extent to which medical conditions are important.
History of driver licensing
Driver licensing has changed dramatically over the past 25 years and the process is continually being refined. The Driver and Vehicle Licensing Centre opened in 1972 and the medical standards governing driver safety were published by the Medical Commission on Accident Prevention in 1968 (Reference RaffleRaffle, 1968). Subsequent legislation has been introduced in the Road Traffic Act 1972 (Reference RaffleRaffle, 1976), the First Directive 1981, the Road Traffic Act 1988, the Second EEC Directive 1991 and the Motor Vehicles (Driving Regulations) 1996. The Royal College of Psychiatrists responded to the legislation by producing the medical standards for Group 1 drivers in 1984 (Reference RaffleRaffle, 1985) and for Group 2 drivers in 1993 (Royal College of Psychiatrists, 1993). Group 1 covers motorcycles and cars, Group 2 large goods vehicles and public services vehicles.
Legal basis of fitness to drive
The law prevents a person who cannot meet the medical standards from holding a driving licence. The Road Traffic Act refers to Prescribed, Relevant and Prospective Disabilities. A Prescribed Disability (see Box 1) is a legal bar to holding a licence unless specific conditions can be met. Any medical condition that would make a person a danger while driving constitutes a Relevant Disability, which also bars. A Prospective Disability is any medical condition that, because of its progressive or intermittent nature, may cause the driver to have a Prescribed or Relevant Disability over the course of time. Such a driver will hold a restricted licence, subject to medical review at appropriate intervals. This will apply to most people who have a severe but stable mental disorder.
Box 1. Prescribed Disabilities
Group 1
Epilepsy of any type within the past year
Inability to read a car number plate at 20.5 m
Any sudden disabling attack of giddiness or fainting
Severe mental disorder
Alcohol or drug misuse, whether or not it amounts to dependency
Group 2 (in addition to Group 1)
Insulin-dependent diabetes
Liability to epilepsy, defined as having had an attack or treatment for epilepsy within the past 10 years
Inability to meet the eyesight standards: a visual acuity of not worse than 6/9 in the better eye; 6/12 in the worse eye un-corrected; and not worse than 3/60 in each eye uncorrected.
The standards for vocational (Group 2) drivers are very high. Professional drivers spend up to a whole working week in their vehicle, which may weigh up to 39 tonnes or carry many passengers. An accident involving such a vehicle could put many people at risk.
Application of the law
The law on fitness to drive remains vague, but it has been put into a practical form by the Secretary of State's Honorary Medical Expert Panels, which cover: cardiology, neurology, diabetes, vision, alcohol and substance misuse and psychiatry. The Panels meet at 6-monthly intervals, and their role is to look at new medical evidence with a view to refining the standards and considering individual cases. The standards are published by Drivers Medical Unit (DVLA, 2000).
Licence holders' responsibility
It is the licence holders' legal responsibility to notify the DVLA if they have a medical condition that may affect safe driving: failure to do so and giving false information constitute an offence. There are, in addition, insurance implications.
Doctors' responsibility
The General Medical Council (GMC) has issued guidelines covering situations in which licence holders cannot or will not notify the DVLA of their medical condition (e.g. those with dementia or a psychosis). These have been published by the GMC (1995) and DVLA (2000). The Royal College of Psychiatrists (1993) has also issued guidance to psychiatrists on medical aspects of fitness to drive.
Causes of accidents
To estimate the impact of psychiatric conditions on road safety, we need to know more about RTAs in general. Numbers of RTAs in the UK peaked between 1965 and 1966, with 8000 deaths. In 1967 the number of fatalities fell by 650. This dramatic drop was attributed to three major pieces of new legislation. The first was the introduction in 1965 of the national speed limit, which led almost immediately to a 20% reduction in casualties. The second was the drink/driving laws and seat belt legislation, which came into force in 1967. Alcohol was at that time the largest contributory factor to RTAs, and the third new legislation, resulting from the Blennerhassett Committee on Drinking and Driving, which reported in 1976, had the greatest impact of all.
The High Risk Offenders (HRO) scheme, a product of the Blennerhassett Committee, was piloted in the 1980s and became operational nationwide in 1991 (for details see DVLA, 2000). It was soon evident that, as a result of the scheme, heavy social drinkers became more responsible and stopped drinking and driving. There was less success with ‘problem drinkers’, who seemed less amenable to anti-drinking and driving publicity and education, and it was intended that these should be identified. Even in 1997, when road deaths were reduced to their lowest annual figure of 3500, alcohol was still considered directly responsible for 15%.
Although there has been an overall trend for the number of serious injuries and deaths to reduce considerably, minor injuries continue to increase, and these have a great socio-economic cost.
Human factors play a major role in RTAs, estimated at 95%; only 18% of RTAs are associated with road deficiencies and a negligible number with mechanical faults in vehicles. The major factors owing to human agency are speed, alcohol consumption and perceptual difficulties. Speed usually means going too fast for the prevailing conditions, and is a reflection of the driver's judgement. Cognitive errors, perceptual problems, misinterpretation of the actions of other road users, looking but not seeing, inattention and distractibility are the major human errors (Reference SabeySabey, 1999). As can be seen, therefore – alcohol aside – cognitive or psychological difficulties are the major causes of accidents.
Driving is a complex skill, which is usually learned by practice at an early age. The technique of managing a vehicle's controls is, however, only the beginning. A new driver has to be adept at information processing. There must be sustained attention or vigilance, concentration and a good memory. Adequate visuo-spatial functioning is required, and indeed over 95% of the sensory input into driving is visual. There must be control over impulse and risk-taking. Judgement should be mature and unimpaired, with the ability to anticipate the actions of other road users. Problem-solving and hazard perception are necessary throughout the drive.
It can be appreciated, therefore, that many psychiatric disorders may present problems with driving (Reference Metzner, Dentino and GodardMetzner et al, 1993). It is for this reason that, although certain psychiatric disorders are listed in the medical standards, it is pointed out that the way in which an illness manifests itself in behaviour and cognitive function is far more important than the diagnosis itself. It is also true that drivers without a formal psychiatric diagnosis may be impaired. For example, a person may be extremely emotionally distressed, but never have had a psychiatric illness. The young man who, having just been told by his fiancée that the relationship was over, jumped onto his motorbike in tears and drove straight into the path of a bus was not ill. The immature, impulsive, excitement-seeking woman of 20 who enjoys alcohol and recreational drugs will be dangerous, but may not have a recognisable or treatable mental illness.
Are people with psychiatric disorders dangerous drivers?
There is very little evidence indeed confirming that psychiatric illness results in dangerous driving. It is not even clear what the evidence base was for the Royal College of Psychiatrists' original fitness to drive criteria (Reference RaffleRaffle, 1985). Common sense tells us that a person suffering an acute psychotic episode, totally engulfed in delusions, will be dangerous while driving: it is estimated that over half of patients with schizophrenia act on their delusions. Similarly, we would expect that a person severely ill with anxiety or depression, whose reactions are retarded, who cannot concentrate or make decisions and who is absorbed in worries and problems will not be a safe driver.
It has been estimated that 25% of drivers involved in accidents are impaired owing to alcohol, drugs, illness or emotional disorder (Reference CremonaCremona 1996).
Silverstone (1988) tells us that there is little evidence that those with schizophrenia are more dangerous than controls. However, suicide attempts at the wheel are worryingly high, and he describes a study in which 10% of accident drivers had suicidal ideation. He also quotes a study showing that patients with neurotic disorders, including anxiety states, have 50% more accidents than controls. His conclusion was that overall, patients with psychiatric disorders had a higher risk of RTAs than expected. The most dangerous were those with dementia, followed by hypomania and mania; severe depression and suicidal ideation, personality disorders and alcohol misuse are the other significant diagnoses.
Elkema et al (1970) found that male patients with a personality disorder had six times as many RTAs as controls.
Gibbons (1976) notes that most mental illnesses tend to reduce activity and interest, and therefore possibly the use of a car. This may lower the anticipated risk. Dangerousness was most likely in the acute phase, particularly in hypomania. However, he quotes evidence suggesting that a psychiatrically ill patient is far more dangerous as a driver before hospital admission and treatment than after it. He points out the unacceptable danger of suicidal thoughts in a driver, commenting that risk-taking may accompany the despair of depression. The risk is much greater if a driver has delusions or preoccupations related to motoring or other drivers. He ends by commenting that personality disorders in which aggression, impulsiveness, intolerance or frustration are exhibited are the most dangerous in drivers, and that indecision, preoccupation and poor concentration may occur in almost any psychiatric illness.
The incidence of driver suicides is probably underestimated. Ohberg et al (1997) describe a study undertaken in Finland between 1987 and 1991 in which a number of teams, each including a police officer, physician, vehicle engineer and road specialist, collected statistics covering the whole country. At least 5.9% of fatal driver accidents were suicides. Single-car accidents were less common than head-on collisions with a heavier vehicle. In 4% of cases, the crash led to the death of another person. The risk factors were youth (50%), stressful life events, psychiatric disorder, alcohol misuse and driving under the influence of alcohol. A significant number of drivers were, however, middle-aged sober men.
Anecdotal evidence comes to the DVLA via police reports (see Boxes 2 and 3). I conducted a brief analysis of the first 250 of just over 1000 police reports received in 1995, and the results are shown in Figs 1 and 2. Where illness or disability were implicated, psychiatric disorders constituted the largest single cause of accidents. Dementia was most prominent, but hypomania and suicide attempts at the wheel were not insignificant.
Box 2. Dementia in a 73-year-old male
A 73-year-old man with dementia set off to visit his daughter. He quickly got lost and drove anti-clockwise around the M25 until he ran out of petrol. The police found him at 04.00 washing his car. It had three punctures and a large dent in the nearside door, which he could not explain. The police found him to be very confused and subsequent medical reports confirmed dementia: his licence was revoked.
Box 3. Schizophrenia in a 46-year-old male
Following a report of a person acting strangely, a police officer found a man sitting in the driving seat of a car on a garage forecourt at Penrith, with the engine running. He told the officer that he had driven there from Birmingham to “get away from it all”. He appeared very nervous and frightened and said that people were “out to get him”. When asked who in particular, the man pointed to passing vehicles and said “Them”. The police officer spoke to the man for over 30 min, during which time he learned that the man had been admitted to hospital four times under Section 2 of the Mental Health Act, the last occasion being 4 months previously. He was not taking any medication because it made him sleep. At one stage a vehicle stopped by the roadside and the man, seeing this, ducked down and said that they had come to get him. The officer was very concerned about his mental health and arrested him under Section 136 of the Mental Health Act. When asked if there was anything he would like to take from his car the man pulled a cricket bat from the passenger foot well. He held the bat in an aggressive manner and said “I will be needing this”. The man was admitted to a psychiatric hospital and his driving licence was revoked.
Alcohol misuse or dependency
The HRO scheme lists three categories of drink/driving offenders for whom a diagnosis of alcohol misuse or dependency must be excluded before a licence is issued (see Box 4). Those designated HROs are legally required to undergo an independent medical examination, which includes an alcohol history, details of medication, a physical examination and blood tests for γ-glutamyl transpeptidase (GGT), aspartate aminotransferase (AST) and mean corpuscular volume (MCV). The medical standards have been laid down by the Secretary of State's Honorary Advisory Panel on Driving and Alcohol and Substance Abuse. About 40 000 HROs are assessed annually. Of these, 10% are found to have a history of recent alcohol misuse or dependency, and their licence application is either refused or restricted.
Box 4. Criteria requiring exclusion of alcohol misuse/dependency diagnosis in high-risk offenders
More than two drink/driving offences in 10 years
Alcohol level >2.5-times the legal limit
Failure to give a specimen
Others come to the notice of the DVLA because they have a history of alcohol misuse or dependency. This is now a Prescribed Disability under the Motor Vehicles (Driving Regulations) Act 1996, and the Secretary of State's Panel states that a person may not resume driving until free from alcohol misuse or dependency for a minimum of 1 year, because of the very high risk of relapse. There is much in the literature about the dangers of alcohol in drivers. There is a clear dose effect: as little as 30 mg/100 ml in the blood causes some impairment; at 50 mg/100 ml there is significant impairment and risk of accident; at 150 mg/100 ml, the accident risk is doubled; most social drinkers would be semi-conscious at 200 mg/100 ml, which is 2.5-times the legal limit.
Substance misuse
Cannabis is the drug most frequently misused and it is often part of polydrug use. It is the most common drug detected in drivers involved in accidents. It increases risk-taking behaviour and impairs judgement and perception. All drugs of misuse impair driving ability and their persistent use is a Prescribed Disability. The dangerousness of ‘recreational’ drugs should not be underestimated.
Dementia
Of all psychiatric conditions, dementia is the most dangerous in a driver. However, the onset of cognitive impairment can be very gradual, and safe driving ability may be retained for a considerable period. It is estimated that 11% of those aged 65 or over have dementia of some type or degree; this rises to 48% in the 85+ age group. As the elderly population increases, so does the potential number of drivers with dementia.
With the help of consultant pyschiatrists, I undertook a small pilot study (unpublished) including 113 consecutive referrals with a diagnosis of dementia to psychogeriatric units in Wales. Of these only 17 were licence holders and 12 were currently driving. Therefore, only 10% of this group were actually driving. All the drivers had early-to-moderate dementia. The reasons for not driving were not studied, although it is known that many elderly drivers fail to renew their licences at 3-yearly intervals and have reduced access to a car. It is possible that the problem of dementia and driving may not be as large as suspected and further study is required.
Accurately assessing the fitness to drive of people with dementia is fraught with problems. An on-road practical test should be the only arbiter, but such assessments are not easy to arrange and require a valid driving licence. Private road systems do not allow full assessment of judgement, hazard detection and anticipation.
A battery of predictive table-top psychological tests would be a cost-effective method of screening drivers with a progressive neurological disease affecting cognitive function. However, developing such a battery is an illusive task. The tests should measure what science considers is the neurophysiological function of driving and require validation by driving assessment. They should be function-based and IQ-free. Unfortunately, the actual processes involved in driving are not yet fully understood, which makes the search for predictive tests even more difficult. Physical control is not the problem, as it is an over-learned skill resistant to decline.
The three systems found to be most predictive are the visual–perceptual system, praxis and executive function. The latter is the most important. All psychological modalities involved in driving, including emotion and thought processes, are interlinked and brought together for action in the frontal lobes. Continuous monitoring of the environment, leading to the decision to transfer attention and make rapid judgements, also takes place in this region (Reference McKennaMcKenna, 1998).
How then can a clinician give an informed opinion about fitness to drive in dementia? Only with great difficulty in its early stages, but with far more certainty as the disorder progresses. Assessment of the activities of daily living is extremely useful: it is most unlikely that a person who cannot find the way to the toilet would be a safe driver.
Psychologists are often asked to assess whether patients can drive safely, but they are handicapped by not having a predictive set of tests or access to an on-road driving assessment. Clinical impression must therefore carry more weight than tests, and this is borne in mind by the Medical Advisers at the Drivers Medical Unit. Patients should be reminded to notify the DVLA as soon as they are diagnosed with dementia, and in the majority of cases the licensing decision will be made on clinical reports. In doubtful cases, on-road assessment is arranged, using the Driving Assessment Centres accredited by the Forum of Mobility Centres (for a full list see DVLA, 2000).
Psychotropic medication
Driving while impaired by drugs, illicit or prescribed, is an offence dealt with by the police and the courts. Most psychotropic medication causes impairment, and any driver taking it requires careful advice about side-effects and the consequences of driving while impaired.
Side-effects can masquerade as symptoms of illness and vice versa, and it is sometimes very difficult to be clear about the cause of impairment. Often, the side-effects of psychotropic medication are individual, even idiosyncratic, and the longer a person is on a drug the less likely is significant impairment. It is wise to advise a person not to drive within 1 month of starting psychotropic medication or of increasing the dose. It is not possible to list here all drugs that are not acceptable in a driver. Drugs having anticholinergic side-effects should be avoided; these include tricyclic antidepressants and phenothiazines. The antihistamine effects of some antidepressant drugs may also cause drowsiness and care must be taken. Selective serotonin reuptake inhibitors, monoamine oxidase inhibitors and noradrenaline reuptake inhibitors have fewer side-effects and are safer. Most antidepressants and some antipsychotics reduce the epileptic threshold and may trigger epileptic attacks in vulnerable people (Reference HarrisHarris, 1997).
Long-acting depot neuroleptics and the newer antipsychotic drugs can impair driving, but the sedative effect usually diminishes after about 3 months. Parkinsonian side-effects can be dangerous. Benzodiazepines are the most dangerous and are over-represented in drivers involved in RTAs. The interaction with alcohol of all drugs acting on the central nervous system will increase impairment and affect driving ability.
It is acknowledged that drivers with psychiatric illnesses are usually safer when well and on regular psychotropic medication than when they are ill. However, inadequate treatment or lack of compliance may render the driver impaired by both illness and medication. Special care should always be taken in prescribing psychotropic drugs in the elderly. It is good practice to ask the patient whether or not they drive and to advise accordingly.
Risk assesment
It is clear that a person who is acutely psychiatrically ill is likely to be a source of danger while driving because of the impairment that the state of mind produces. When recovered that person will be well enough physically and mentally to drive. However, there is usually a risk of relapse.
The shortest period for which a driving licence can be issued is 1 year. Since an episode of psychiatric illness may be accompanied by loss of insight and an inability to realise that driving may be dangerous, it is essential to be confident that a person is not likely to relapse during that year. As insurance companies know, past accidents and convictions are the best predictors of future events. Some drivers are more high risk than others. Silverstone (1988) tells us that patients suffering from psychiatric conditions drive fewer miles per year than average. However, per mile travelled they have twice the number of accidents. Cremona (1996) also reminds us that the possible reason psychiatric disorders are not particularly associated with accidents is that those who have a severe psychiatric disorder may have limited access to a vehicle or voluntarily avoid driving. This will reduce the overall risk, and is an example of risk changing over time and in different situations. A risk is a probability: here, a prediction of a person's behaviour over time. Risk assessment is a difficult process, and in deciding fitness to drive it is based on thorough clinical assessment, addressing the questions “What is likely to happen, when and how?” (Reference MadenMaden, 1996). In this field, case law has defined probability: it is more than the barest possibility.
The risk factors used by the DVLA in assessing the safety of a driver are reflected in the questions posed to clinicians involved in the driver's care. These concern: the diagnosis; the history, including dates of remissions and relapses; the period of stability; compliance with medication and other treatments; intrusive symptoms; suicidal behaviour; cognitive impairment; side-effects of drugs; and alcohol and substance misuse. The risk that a person will pose to the road-using public is reflected in the duration of any temporary ban on driving and the subsequent periodicity of medical enquiry following the granting of a licence.
Medical enquiry process
Figure 3 shows the process of medical enquiry applicable to all medical conditions likely to make a driver unsafe. Notifications are received from many sources and the subsequent medical enquiry requests the licence holder's consent. The law allows a licence to be revoked or refused if unfettered consent is not provided within the time allowed. This frequently occurs in those with severe mental disorder, as they do not read their mail, resent the intrusion or simply forget to return the form. If a doctor follows GMC advice and notifies the DVLA that a person is not fit to drive and will not respond to advice, the licence can be revoked instantaneously.
In normal circumstances medical reports are obtained and, if necessary, the driver may be referred to an independent doctor for an examination. A formal driving assessment may be requested using one of the Forum Centres. The decision about fitness to drive is made by the Medical Adviser. If the licence is refused or revoked, the person has the right of appeal to the Magistrates' Court under Section 100 of the Road Traffic Act 1988. These appeals are now quite rare, as the issue can usually be resolved by additional medical evidence obtained by the applicant in their support.
Medical enquiry may take some time, and during that period the driver still has a licence and therefore an entitlement to drive. One purpose of the At a Glance Guide to Current Medical Standards of Fitness to Drive (DVLA, 2000DVLA, 2000) is for the doctor involved in a patient's care to have some idea of the anticipated outcome of medical enquiry and to advise their patient accordingly. To drive when it is clear that the medical standards cannot be met would be foolish indeed.
The medical standards for drivers who have a psychiatric disorder have been in place since 1984, but two studies published in the mid-1990s (Reference Humphreys and RoyHumphreys & Roy, 1995; Reference Thompson and NelsonThompson & Nelson, 1996) showed that psychiatrists were then largely unaware of them. It is important for medico-legal reasons that all doctors are aware of the medical standards and advise their patients accordingly.
Conclusion
The medical standards of fitness to drive are based on legal requirements and are published by the DVLA (2000).
A licence holder or applicant has a legal duty to notify the DVLA of any medical condition that may affect safe driving. Subsequent medical enquiry is undertaken by the DVLA with the licence holder's consent. The Secretary of State of the DETR is responsible, through his Medical Advisers, for deciding whether a person meets the medical standards and is therefore eligible to hold a driving licence. If a licence is refused or revoked, the Medical Adviser explains the reason and the conditions to be met before a re-application can be accepted. The medical standards are continually revised by the Secretary of State's Honorary Medical Advisory Panels.
Medico-legal implications make it necessary for doctors and psychiatrists to be aware of the GMC guidance and also of the advice of the Royal College of Psychiatrists.
Multiple choice questions
-
1. The most important factors in road traffic accidents are:
-
a medical conditions
-
b human error
-
c illicit drug use
-
d multi-factorial
-
e going too fast for prevailing conditions.
-
-
2. The medical standards of fitness to drive:
-
a with regard to psychiatric conditions have been in place since 1984
-
b are decided by the Medical Advisers at the DVLA
-
c are all detailed in the Road Traffic Act 1988
-
d are currently based on the Second EEC Directive and the Road Traffic Act 1988
-
e are continually updated by the Secretary of State's Panels.
-
-
3. Evidence in the literature tells us that:
-
a psychiatrically ill patients have more road traffic accidents than controls
-
b it is most uncommon for people to attempt suicide at the wheel
-
c the most dangerous drivers are those with dementia
-
d depresion and anxiety are not associated with road traffic accidents
-
e depression is associated with risk-taking.
-
-
4. The Road Traffic Act 1988:
-
a describes three types of disability
-
b does not mention psychiatric disorders at all
-
c has been updated by a more recent regulation
-
d states that a Prospective Disability is a bar to driving
-
e is independent of any of the EEC directives.
-
-
5. Psychiatrists' responsibilities:
-
a include reporting to the DVLA all patients who have a psychiatric disorder
-
b include advising their patients to notify the DVLA when they have a medical condition that might preclude safe driving
-
c have never been formally laid down in any publication
-
d include following the advice of the GMC
-
e are to the patient alone, in support of the doctor–patient relationship.
-
MCQ answers

| 1 | 2 | 3 | 4 | 5 | |||||
|---|---|---|---|---|---|---|---|---|---|
| a | F | a | T | a | T | a | T | a | F |
| b | T | b | F | b | F | b | T | b | T |
| c | F | c | F | c | T | c | T | c | F |
| d | T | d | T | d | F | d | F | d | T |
| e | T | e | T | e | T | e | F | e | F |
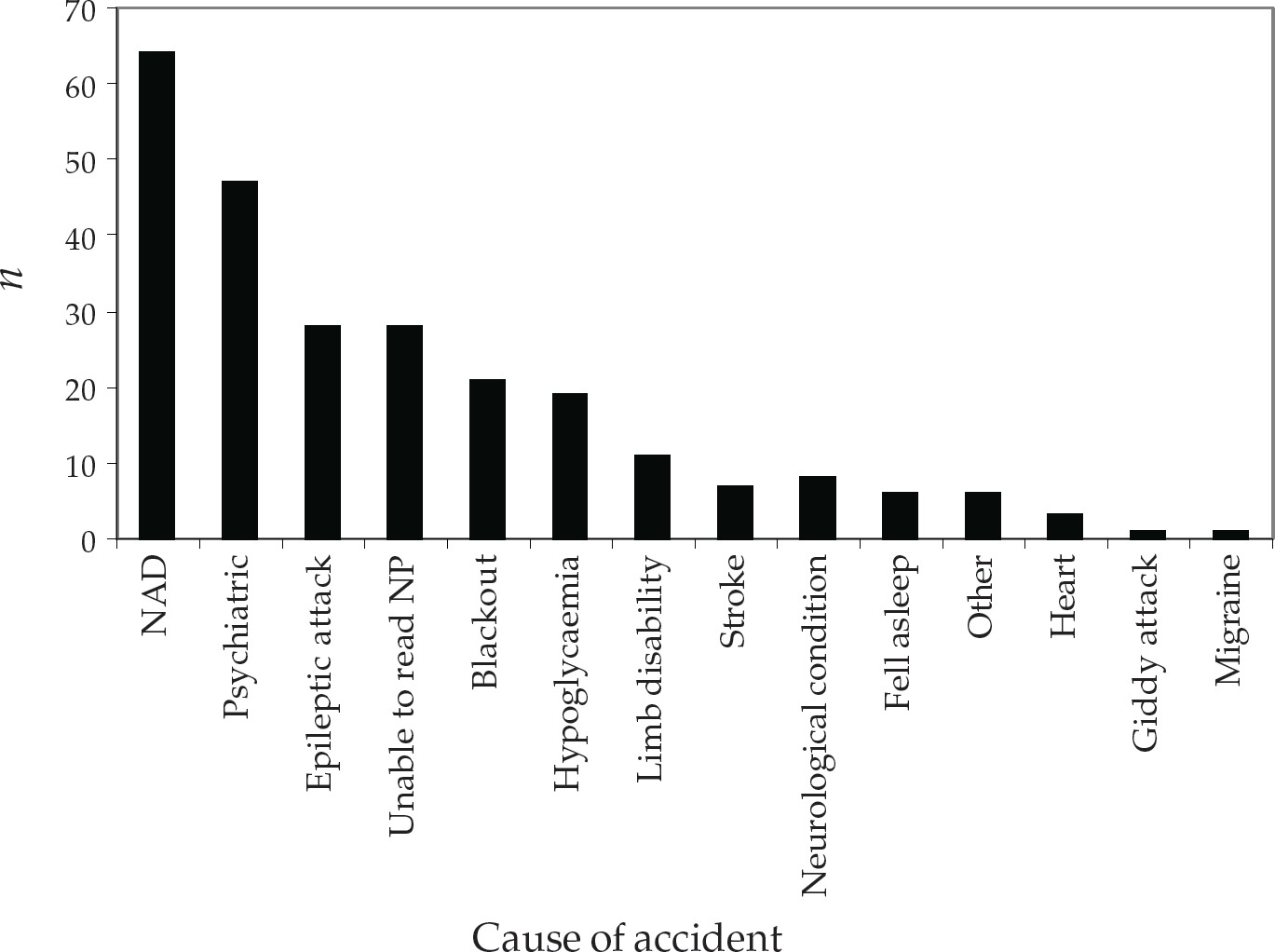
Fig. 1 Analysis of about 25% of police notifications in 1995. n, number of reports (total = 250). NAD, nothing abnormal detected; NP, number plate.

Fig. 2 Psychiatric disorders identified on police reports as the cause of road traffic accidents

Fig. 3 The processes entailed in a medical enquiry into fitness to drive






eLetters
No eLetters have been published for this article.