Munchhausen syndrome by proxy is a form of child abuse in which parents (usually mothers) present their children to healthcare professionals as ill when in fact the symptoms of the illness are falsified, fabricated or actively induced by the parent. Individual cases have attracted considerable interest, especially those that have resulted in criminal prosecutions (e.g. the cases of Beverley Allitt in the UK and Julie Gregory, a victim of illness induction, in the USA: see Further reading). Since its first description in 1977 (Reference MeadowMeadow, 1977) there have been multiple accounts of different presentations of the behaviour, which carries an appreciable morbidity that is similar to other forms of child abuse (Reference RosenbergRosenberg, 1987, Reference Rosenberg2003).
There has been considerable debate about the proper terminology to be used for this form of abuse (Reference Ayoub, Alexander and BeckAyoub et al, 2004): potential for confusion exists because the behaviour results in fabricated or induced illness in the child, but may be associated with various types of disorder in the abuser. The Department of Health (2002) uses ‘fabrication or induction of illness in children’, although ‘Munchhausen syndrome by proxy’ is probably the most common popular description. In the USA, DSM–IV recognises ‘factitious disorder by proxy’.
Despite extensive research into the behaviour, there still seems to be some doubt about its reality. A number of women who were thought to have induced illness in their children were recently acquitted in the UK courts, and these highly publicised cases have led at least one journalist to question the existence either of the behaviour, or of a disorder in mothers that might give rise to it (Reference LiddleLiddle, 2005). Regrettably, this type of comment has distracted from the key aspects of induced illness, which are that:
-
• it is a form of child abuse
-
• it is perpetrated by those who have care of the child (usually the mother) and usually involves secondary medical services (although it may first be manifested, although undetected, in primary care settings)
-
• detection requires detailed and painstaking enquiry involving the collection of information from many different sources and discussion with different agencies, e.g. social services, general practice staff and the police.
Prevalence and manifestations of the behaviour
A hierarchy of evidence now exists, which ranges from detailed accounts by victims to the confessions of perpetrators and published case series. Information from these various sources provides unequivocal evidence that caregivers do fabricate or induce illness in children, and this requires appropriate responses from professionals (Department of Health, 2002). The largest case series includes 451 cases from many different countries (Reference SheridanSheridan, 2003).
The behaviour takes different forms, which may indicate a range of disturbance in the individuals concerned. Behaviours include:
-
• giving false accounts of symptoms (e.g. ‘He keeps having fits’, ‘She suddenly stops breathing’)
-
• fabricating symptoms (e.g. putting substances in a child's urine sample to simulate haematuria)
-
• inducing symptoms of illness (e.g. administering medications inappropriately, smothering to simulate apnoeic attacks, tampering with hospital equipment).
Although the induction of illness usually carries a greater risk of causing serious physical harm to the child, children can also suffer harm as a result of repeated inappropriate investigations, such as lumbar punctures, which are administered as a result of false accounts of symptoms or fabricated symptoms. One of the most problematic aspects of this behaviour is that general practitioners, accident and emergency (A&E) staff and paediatricians may be unwittingly involved in causing potentially dangerous iatrogenic complications (Reference Eminson and PostlethwaiteEminson & Postlethwaite, 2000). Well over half of the children involved suffer indirect psychological harm, including emotional and behavioural problems, school non-attendance and major concentration difficulties. Furthermore, affected children live in a fabricated sick role and may eventually go on to simulate illness themselves (Reference SandersSanders et al, 1995). The family context within which fabricated or induced illness is perpetrated may also account for the fact that up to three-quarters of index children are affected by other forms of maltreatment, neglect, further fabrications or inappropriate medicating (Bools et al, 1992).
A decade ago, Reference McClure, Davis and MeadowMcClure et al(1996) reported that the combined annual incidence of fabricated or induced illness, non-accidental poisoning and non-accidental suffocation in the UK and Ireland in children under 16 years of age was 0.5 per 100 000, and for children less than 1 year old it was 2.8 per 100 000. It is likely that this is an underestimate: not all cases are detected, especially those that involve false accounts of symptoms or fabricated symptoms (such as tampering with a child's specimens). Induced illness, which results in greater morbidity or even death, may be more easily detected, although there remain concerns that some types of sudden death in children may be the result of this form of child abuse (Craft & Hall, 2004; Galvin et al, 2005). Fabricated or induced illness is most often seen in children less than 5 years of age (who are unable to verbalise their own problems), although older children are also involved and may actively collude in the sick role with their parents.
Social and demographic characteristics
There are described characteristics of people who fabricate or induce illness in children that are unusual compared with other child abusers, and these may offer tantalising hints at the origins of the behaviour. The overwhelming gender differential makes this abuse different: in most forms of child abuse, newborns are most likely to be harmed by their mothers, whereas abuse of children over 12 months old is perpetrated equally by males and females (Reference Marks and KumarMarks & Kumar, 1996). However, people who fabricate or induce illness in children are nearly always female. Furthermore, they are usually the child's mother, although the behaviour has also been described in professional carers who abuse those dependent on them, which again suggests that the reciprocal role relationships may be important for this type of abuse (Reference Adshead, Falkov, Gopfert, Gopfert, Webster and SeemanAdshead et al, 2004). Some disorder of the caring role function may explain why professional carers are also overrepresented among mothers who treat their own children in this way. Finally, unlike other types of child abuse, fabrication or induction of illness seems to be perpetrated by all social classes, is not always associated with other types of family violence or crime, and is not associated with young inexperienced parents or socio-economic deprivation. In one series of 37 mothers, however, there were high rates of privation, childhood abuse, significant loss or bereavement (Reference Gray and BentovimGray & Bentovim, 1996).
Psychopathology of the fabricators
Fabrication or induction of illness in children is offending and anti-social behaviour perpetrated on the vulnerable. It is therefore useful to consider it in the context of the psychopathology of child abusers more generally, and then to focus on the possible mechanisms that may give rise to this particular form.
Psychiatric illness and personality disorder
It is important to state at the outset that there is no clear relationship between any mental disorder and abusive behaviour towards children (Reference Adshead, Falkov, Gopfert, Gopfert, Webster and SeemanAdshead et al, 2004). Personality disorder is reported as highly prevalent in child abusers generally (Reference Dinwiddie and BucholzDinwiddie & Bucholz, 1993), but there is a danger of circularity of argument, because the diagnosis of personality disorder is based on the abusive behaviour. It is likely that some types of personality disorder (for example, antisocial personality disorder) are a risk factor for child abuse generally, but the diagnosis alone provides little information.
This point is of particular relevance in cases of fabrication or induction of illness in children. At least one study found high rates of borderline personality disorder in fabricators (Reference Bools, Neale and MeadowBools et al, 1994). However, it would be misleading to suggest that borderline personality disorder causes the behaviour, since so many mothers with borderline personality disorder do not abuse their children in this way. Nevertheless, borderline personality disorder is associated with a variety of parenting problems (Reference Hobson, Patrick and CrandellHobson et al, 2005), almost certainly mediated through the attachment style of affected mothers. Behaviours associated with borderline personality disorder, including self-harm and minor forensic behaviours such as shoplifting, have been found in individuals who fabricate or induce illness in children in their care.
Of more relevance may be the prevalence of somatoform disorders in perpetrators, since the behaviour indicates some abnormality of illness behaviour and relationships with healthcare professionals. Reference Bools, Neale and MeadowBools et al(1994) found a high prevalence of somatising and factitious disorders in their sample. Factitious disorder in adults and fabrication or induction of illness in children can co-occur, so the detection of one may trigger a search for the other (Reference Feldman, Rosenquist and BondFeldman et al, 1997).
Psychiatrists whose work brings them into contact with parents with chronic somatoform or factitious disorders should be alert to the impact of these disorders on the patients’ children. There is evidence that somatising behaviour in adulthood is associated with adverse experiences of care and illness in early childhood (Reference Craig, Cox and KleinCraig et al, 2002).
The distinction between somatising disorders and factitious disorders is chiefly one of perceived and conscious motive (Reference Bass, Halligan, Bass and MarshallBass, 2001), and it is possible that a subgroup of somatising mothers go on to become those who ‘somatise’ their children's experience.
Clinically, it is common to see mothers with multiple physical symptoms, as well as symptoms of anxiety and depression (Box 1).
Box 1 The psychopathology of fabricators
The following results were recorded by Reference Bools, Neale and MeadowBools et al(1994):
-
• Of 47 individuals who had fabricated or induced illness in children:
-
34 (72%) had somatoform disorders
-
26 (55%) self-harmed
-
10 (21%) misused alcohol and/or drugs
-
-
• Of the 19 individuals interviewed, 17 (89%) had a personality disorder
In contrast, Reference Adshead and BluglassAdshead & Bluglass (2005) found personality disorders in only 23% of a sample of individuals most of whom had been referred from social services to an adult psychiatrist for child protection purposes. All of the Bools et al sample had been referred to a paediatrician after fabricated illness had been established in the child. Furthermore, Bools et al used a structured interview, whereas the Adshead & Bluglass study used a self-rating scale.
In many mothers with somatoform disorders who fabricate or induce illness in their children the use of healthcare services is chaotic, with frequent visits to different A & E departments, frequent changes of general practitioner (for themselves and their children) and lack of continuity of care. It is important to note that the parents of children who are victims of serious and substantiated physical abuse and neglect change their child's primary care provider more frequently those of non-abused children (Reference Friedlaender, Rubin and AlpernFriedlaender et al, 2005).
Of the medically unexplained symptoms reported by somatising mothers, a high proportion are ‘pseudoneurological’ (faints and pseudoseizures) and gastroenterological (abdominal pain and nausea) (C.B., personal observation). It is of interest that the symptoms most commonly fabricated in children by carers are epilepsy and syncope (Reference Barber and DavisBarber & Davis, 2002).
Motives
The issue of motive has been a major cause of debate among workers in this field. Meadow's original contention was that the mothers carried out this behaviour to draw attention to their own needs. Authors such as Reference Schreier and LibowSchreier & Libow (1994) have suggested that the mothers form disturbed relationships with healthcare professionals that replicate disturbed past relationships with carers. Of relevance here may be that some case series have revealed that many of these mothers themselves experienced childhood abuse (Reference Gray and BentovimGray & Bentovim, 1996; Reference Bools, Neale and MeadowBools et al, 1994; Reference Adshead and BluglassAdshead & Bluglass, 2005). However, a history of childhood abuse is neither necessary nor sufficient to explain fabrication or induction of illness in children, since most adult survivors of abuse do not abuse their children.
It has been suggested that fabrication or induction of illness is a form of complex deceptive behaviour. Scrutiny of social service records or discussions with relatives or other informants such as the general practitioner (GP) may reveal a history of lying dating from childhood or adolescence. Pseudologia fantastica is a dramatic form of pathological lying that consists of grandiose stories, often built on a matrix of truth (Reference Dike, Baranowski and GriffithDike et al, 2005). Fact and fiction are woven together until the two are virtually indistinguishable. Unlike a person with delusional psychosis, someone with pseudologia fantastica will abandon the story or change it if confronted with contradictory evidence or sufficient disbelief.
Disturbance of attachment representations
It may be more fruitful to see fabrication or induction of illness in children as a function of a disturbed mother–child attachment bond, which in turn may be influenced by the mother's own attachment experience. There is ample evidence that early childhood experience and associated attachment style have a direct effect on parenting of one's own children (Reference Van Ijzendoorn, Juffer and Duyvesteynvan Ijzendoorn et al, 1995), especially on caregiving behaviour. Furthermore, insecure attachment style is associated with higher levels of somatisation. Controlling for age, income and recent experience of violence by an intimate partner, Reference Waldinger, Schulz and BarskyWaldinger et al(2006) showed that fearful attachment fully mediated the link between childhood trauma and somatisation for women.
Reference Adshead and BluglassAdshead & Bluglass (2001, Reference Adshead and Bluglass2005) have examined attachment models in mothers who had fabricated or induced illness in their children and found high levels of insecure attachment and unresolved bereavement, compared with established norms. In attachment terms, these mothers were more similar to clinical and forensic patients. Insecure attachment is common in many clinical samples and is too non-specific to have explanatory power. However, the link with bereavement may be of interest because it echoes Reference Gray and BentovimGray & Bentovim's (1996) finding of high levels of bereavement in this group. Unresolved bereavement reactions might sensitise an individual to see dependent others as more ill than they really are, or to dread that a potentially fatal illness may be missed.
As with other childhood abuse, not every child in a family will be victimised in this way. Although there are multiple victims in some families, it is more common for one child to be the main target. Reference JureidiniJureidini (1993) has suggested that the disturbed relationship with this child may begin in the womb, as is evidenced by the high rates of antenatal and obstetric complications in women who carry out this behaviour. This may indicate that more attention should be paid to mothers who have such problems when they present in primary care and on obstetric wards.
The role of the psychiatrist
Investigation
Strictly speaking, the psychiatrist has no role to play until the behaviour has been identified and confirmed. This process relies heavily on paediatric assessment and investigation, and the exclusion of other causes for the child's ‘symptoms’. However, psychiatrists (either from liaison or child psychiatry) may be called in to assess parents who have a history of psychiatric disorder, as part of the determination of what is happening. In such circumstances, it is important for the psychiatrist to remind colleagues that a psychiatric history does not automatically make a parent more likely to abuse their child, nor does it mean that all of their concerns about their child will be abnormal. Specifically, it is important to state that a history of borderline personality disorder, factitious disorder or a somatoform disorder does not necessarily help to identify fabrication or induction of illness in children.
Psychiatrists should be especially wary of accepting instructions in legal proceedings (either family or criminal), where fabrication or induction of illness in a child is suspected, but has not been confirmed as legal fact. Psychiatrists may come under enormous pressure to provide an opinion as to whether a parent ‘has MSBP’ (Munchhausen syndrome by proxy) and therefore by inference has carried out the behaviour in question (Reference AdsheadAdshead, 2005). Since there is no evidence base that supports a link between any psychiatric diagnosis and either past or future abusive behaviour, it would be highly misleading for psychiatrists to offer any opinion until the facts about the identity of the perpetrator have been established. It must be remembered that there is no diagnosis of ‘fabrication or induction of illness in children’ (or of Munchhausen syndrome by proxy), so it is therefore not possible to say that a mother ‘has’ this, especially not on the basis of a single interview conducted in an out-patients department.
Assessment
Both adult and child/family psychiatrists have important roles to play in the management of identified cases in which illness has been fabricated or induced in a child. When decisions are being taken about the care of children involved, adult psychiatrists may be asked to assess the risk posed by both the abusing and the non-abusing parent. Child psychiatrists may be asked to provide assessments of family dynamics, parenting skills, opinions about the possibilities of family interventions and support, assessments of the effect on the child of the behaviour and treatment for both the child and the other family members.
The assessment of the perpetrating parent is a complex process that requires the collection of information from a wide variety of sources (with the parent's consent). It is essential to read the medical records of the parent (both hospital and primary care) and also, if possible, of the abused child or children. Specifically, it may be useful to look at past hospital attendance rates and put these in context of the other events in the parent's life. Social services records should be accessed (if relevant) and, if possible, any history of a criminal record. The amount and type of information available will depend to some extent on the context in which the assessment is taking place: most commonly it will be in the context of care proceedings, where the parent's solicitor may have to be approached to gain access to both health and criminal records.
Despite what has been said above, both adult and child psychiatrists may find themselves in situations where they are interviewing a parent who is only suspected of having fabricated or induced illness in their child, but that it has not yet been proven. If this is the case, then the process of preparation before interviewing the parent is especially important and complex (Box 2). It involves the collection and reading of a considerable amount of information, as well as interviews with key informants such as social workers and the child's grandparents. This process may take many hours, and during the reading of the (usually) extensive medical and social work notes the assessor should be looking for evidence of inconsistencies in the medical history, comments from medical practitioners and social workers about parenting skills, evidence of antisocial behaviour and dissimulation or frank lying. Examination of past medical, psychiatric and social work records may reveal long-standing emotional and behavioural difficulties, often beginning in childhood. However, we reiterate that psychiatrists should be very wary of acting as detectives and drawing inferences from various, and not necessarily impartial, sources.
Box 2 Assessment of a mother under suspicion
Preparation for the assessment of a parent suspected of inducing or fabricating illness in a child should include:
-
• the mother's medical records (hospital and GP records, both paper and electronic)
-
• the child's medical records
-
• social work records/reports
-
• police records/videos
-
• legal documents (mother's and father's statements; reports written by the child's guardian ad litem)
-
• interview with the mother and partner (audiotaped, with consent)
-
• interview with the grandparents (audio-taped, with consent)
-
• telephone interview with GP, social workers, paediatrician and guardian
Psychiatrists are often asked to provide opinions about the parenting capacity of a parent suspected of this type of abuse or of the non-abusing parent. It is important that psychiatrists who do this have expertise in the field, which usually means that they are child/family psychiatrists. Adult psychiatrists should not offer expert opinions about parenting capacity unless they (a) have the skills to carry out a thorough parenting assessment and (b) can demonstrate to the courts exactly how they have done so. Parenting capacity (or its absence/lack) cannot be established by an ordinary psychiatric interview of the adult alone: it usually includes assessment of the parent with the child, and information from foster carers or those who supervise contact.
Management
Where parent and child are permanently separated
Detection of fabricated or induced illness in a child usually results in care proceedings to determine whether the abusing parent should continue to care for the child. In most cases, courts will place the child in the care of the non-abusing parent (if separated), grandparents or the local authority. Abusing parents may or may not have contact or access, depending on individual circumstances.
Ideally, the parents (over 90% of whom are mothers) would have access to therapy to address their abusive behaviours, not least because they may be of reproductive age for some time to come. Psychological therapies are not indicated for individuals who cannot admit their behaviours, or who are so deceptive that they cannot establish a therapeutic alliance. Unfortunately, there are almost no services available to treat parents who have abused their children in any way, even if they have quite severe personality disorders or other psychiatric conditions. They will often be rejected by regular psychological therapy services as too disturbed, but are not disturbed enough for forensic services. Services for these offenders are in painful contrast to services for individuals with dangerous and severe psychiatric conditions (Reference AdsheadAdshead, 2003).
Where reunification of parent and child is possible
The courts seek psychiatric advice on whether abusing parent can be sufficiently rehabilitated to be reunited with their child and the rest of the family. As suggested above, where there is frank denial of the behaviour or other evidence of antisocial attitudes or cruelty, this is not likely to be possible. In about 20% of cases, the abuse recurs if the child remains with the parent who abused them (Reference Bools, Neale and MeadowBools et al, 1993). Other siblings are also at risk.
However, there is evidence that reunification of such families is possible and successful. A study by Reference Berg and JonesBerg & Jones (1999) followed up all 17 children from 16 families selected for admission to a specialist unit between 1992 and 1996. There was one recurrence, leading to mild harm to the child. Overall, the children's development, growth and adjustment were acceptable at follow-up. A better outcome was associated with: acknowledgement of fabrication (Fig. 1) and the psychosocial context within which it occurred; less severe abuse; improvements in the parent's psychological functioning and empathy for the child; and improved parent–child relationships and child attachment behaviours towards parents. A better outcome was seen where changes in the family system and a therapeutic alliance with the fabricator's partner and extended family could be established. This enabled a safety network to be established around the child that incorporated the parent's continuing vulnerability.
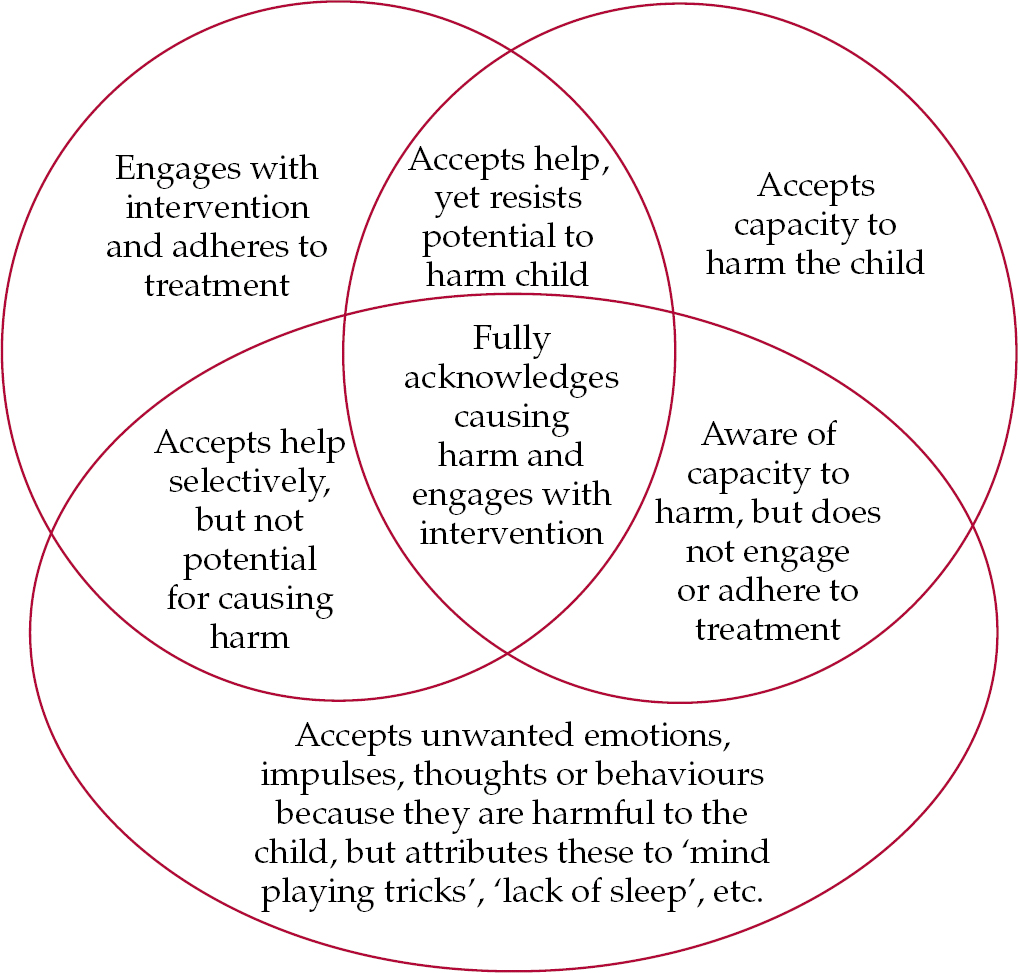
Fig. 1 The main components of acknowledgement. (Adapted by D. Jones from Reference DavidDavid, 1990.)
Prognostic factors can be organised into different domains (Table 1) that are associated with better or less good outcome (Reference Jones, Bools and DavidJones & Bools, 1999).
Table 1 Prognostic factors in fabricated and induced illness
| Domain | Poor prognosis | Better prognosis |
|---|---|---|
| Maltreatment | Induced harm Accompanying sexual or physical abuse of the child Sadistic element Deaths of previous children Harm to animals |
Fabrication Shorter duration of FIP |
| Child | Developmental delay Physical sequelae of an induced illness Development of somatising behaviour |
Absence of delay or sequelae of abuse |
| Parent | Personality disorder Somatisation Denial Lack of cooperation Alcohol/substance abuse Abuse in childhood - unresolved |
Personality strengths Acknowledgment of abuse Cooperation Treatment responsive mental illness Adapted to childhood abuse |
| Parenting and parent–child interaction | Disordered attachment Lack of empathy for child Own needs before child |
Normal attachment Empathy for child Positive co-parenting |
| Family | Interparental conflict/violence Multigenerational abuse |
Non-abusive partner; Supportive extended family |
| Professional | Lack of resources Poorly informed and/or prejudiced |
Partnership with parents Long-term psychological treatment and social casework |
| Social setting | Violent, unsupportive neighbourhood Isolation Involvement with false allegation network |
Local child-support facilities Social support |
Families are selected for possible intervention where a psychiatric formulation is apparent and a treatment plan can be applied to it. Further factors that influence selection include: the potential for working in partnership, some degree of parental acknowledgement of problems and the existence of better prognostic features.
Reunification: treatment phases
Initial denial of responsibility is the norm, but this can waver in the face of parental digestion of the outcome of a split hearing within the family court. Total denial of maltreatment or any problems means that intervention is not feasible, except in the mildest of cases. If treatment aimed at reunification is embarked on, a clear treatment plan with explicit criteria for success is necessary and this should be distributed to all the professionals concerned(Reference Jones, Hindley, Ramchandani, Rose, Aldgate and JonesJones et al, 2005). The time frame for intervention must always be sensitive to the developmental needs of the child.
Treatment can be considered in terms of three phases (Reference Jones, Byrne, Newbold, Eminson and PostlethwaiteJones et al, 2002):
-
1 acknowledgment (Fig. 1);
-
2 improving parental competence and sensitivity to the child;
-
3 resolution.
The acknowledgement is not restricted to admission of acts of illness induction or fabrication. It should also include a much broader acknowledgement by each parent of the scope and scale of parenting problems in the family and any other forms of maltreatment that affect the child. Often there are other aspects of parenting breakdown or parent–child attachment difficulties, within which context fabricated or induced illness has occurred. The acknowledgement extends to the effect of all these aspects on the child and on other family members.
The phase of increasing parental competence and sensitivity to the child depends on change both within individuals and in family interactions. Normally, clinical intervention includes individual therapy and family work. The abuser will need help to distinguish their overconcern about their child's health from healthy affection, care and medical help-seeking. Often the abuser's needs are deflected from somatisation into more direct and healthy help-seeking for psychological dis-ease.
Resolution may be in the direction of a care plan with safe reunification of the child with the parents, or alternatively towards a separation if safety cannot be established. Normally, a safe care plan will involve the abuser's partner and/or other family members or friends, in order to provide a safety net of adults around the abusing parent. Often at this stage the abuser will want to discuss the script for the episode of parenting breakdown and child maltreatment that has occurred, deciding what the child and any siblings – as well as other family members – need to know. The script and care plan will usually incorporate the long-term perspective on the risk of repeating somatisation, together with plans for minimising this possibility or recognising the signs of recurrence if they occur, i.e. a combination of relapse prevention and early intervention if problems do arise.
The whole professional network will need to work together if a plan for reunification is to go ahead safely. Substitute or alternative care for the child will be necessary if there is an unacceptably high persisting risk of recurrence or risk of poor outcome for the child's development.
Reunification: future planning
The primary healthcare team and one named and identified paediatrician are key professionals in any long-term care plan involving reunification. All professionals need to be alert to risks of a range of possible outcomes, including subsequent fabricated or induced illness in any form, significant parenting problems, parent–child relationship difficulties, and psychological maltreatment. Effective management includes containment of the fabricator's long-term tendency to somatise or deceive, harnessing the strength of the non-abusing carer or family members, and management of any parenting breakdown that has accompanied fabricated or induced illness behaviour.
Fabrication or induction of illness in children still provokes considerable fear among professional groups that can lead to difficulties within the professional system itself. This is important to overcome because long-term follow-up by primary health, paediatric and child and family psychiatric teams will be necessary to prevent the emergence of further fabricated illness or a return to somatisation by the abuser.
Further reading
-
• The Clothier Report (Reference Clothier, MacDonald and ShawClothier et al, 2004) is an account of the enquiry into the behaviour of nurse Beverly Allitt, who was charged with 4 murders and 9 attempted murders of children on a paediatric ward in 1991. Allitt had a factitious disorder but ceased fabricating illness in herself for a period of 3 months, during which she induced illness in the 13 children.
-
• Julie Gregory described her experience of being reared by a mother who induced illness in a book that became a best-seller in 2004–2005 (Reference GregoryGregory, 2004).
-
• The story of another individual who's mother induced illness is described by Reference Bryk and SiegelBryk & Siegel (1997).
-
• Reference Sanders and BurschSanders, M. & Bursch, B. (2002) offer useful guidelines for assessment of possible fabricated or induced illness at the request of the courts.
Declaration of interest
None.
MCQs
-
1 Fabrication or induction of illness in a child:
-
a used to be called Munchhausen syndrome by proxy
-
b is most commonly carried out by men
-
c is synonymous with non-accidental injury (NAI)
-
d never occurs in more than one sibling
-
e is not regarded as a form of child abuse.
-
-
2 People who fabricate or induce illness in children have been shown to exhibit:
-
a low rates of somatoform disorders
-
b normal attachment representations
-
c low rates of abuse, neglect and separations in their own childhood
-
d abnormal ECGs
-
e pseudologia fantastica.
-
-
3 Fabricated or induced illness in children:
-
a is always first detected in a general hospital
-
b is never fatal
-
c does not include smothering
-
d may lead to iatrogenic illness in the child as a consequence of over-investigation
-
e is never associated with a factitious disorder in the abusing adult.
-
-
4 Reunification of mother and child after identification of fabricated or induced illness:
-
a should never be attempted
-
b is less likely to be successful if the mother acknowledges the deceit
-
c should involve close collaboration between social services and child psychiatry services
-
d is always successful
-
e should never involve both parents (if a partner is involved).
-
-
5 Establishing that an adult is fabricating or inducing illness in a child:
-
a often requires painstaking examination of medical and other records
-
b is best undertaken by a paediatrician
-
c can often be done in a single interview with the alleged fabricator in the psychiatric out-patient department
-
d is exclusively a medical issue and does not require information-gathering from social services
-
e does not have implications for the fabricator's subsequent employment status.
-
MCQ answers
| 1 | 2 | 3 | 4 | 5 | |||||
|---|---|---|---|---|---|---|---|---|---|
| a | T | a | F | a | F | a | F | a | T |
| b | F | b | F | b | F | b | F | b | F |
| c | F | c | F | c | F | c | T | c | F |
| d | F | d | F | d | T | d | F | d | F |
| e | F | e | T | e | F | e | F | e | F |





eLetters
No eLetters have been published for this article.