In this article we focus on practical aspects of the use of cognitive–behavioural therapy (CBT) as an adjunctive treatment for people with chronic physical illnesses. The standard application of CBT for psychiatric disorders has been comprehensively described elsewhere (e.g. Reference BeckBeck 1995). We therefore concentrate here on features of treatment that are different or particularly pertinent for people who are chronically ill.
The fundamental premise of CBT is that thinking, mood, physical symptoms and behaviours are all interrelated (Fig. 1). It is not merely what happens to a person that determines their responses, it is also their cognitive appraisal of the event. This appraisal will in turn be influenced by past experiences and other aspects of the current situation. For example, being given a diagnosis of colour blindness may have little significance or emotional impact for a young man who wishes to be a psychiatrist, but it would be devastating if he wants to be a fighter pilot. This cognitive appraisal is seldom a one-off static process and it often includes further appraisal of the person's responses. For example, a woman who experiences chest tightness and hyperventilation in response to a brief stressful situation may correctly interpret this as anxiety, in which case the symptoms are likely to be self-limiting. If, however, she had watched her brother die from an acute asthma attack, she may interpret her symptoms as life-threatening and react accordingly. If that response is a further increase in anxiety this will exacerbate the original somatic symptoms.
Cognitive–behavioural therapy may be used not only to treat psychiatric disorder in patients with chronic physical illness. It also has potential use in patients without psychiatric disorder, but who have difficulties related to illness beliefs, illness behaviours or adjustment to illness. In clinical practice this is often not a clear dichotomy, as some of the case vignettes below illustrate.
For a more comprehensive guide to the psychological assessment and treatment of patients with chronic physical illness the reader is referred to the excellent text by Reference WhiteWhite (2001); a description of how psychological principles may be applied to the care of the physically ill is given by Reference SalmonSalmon (2000). Further discussion of the use of CBT and other psychotherapies with patients who have physical illnesses can also be found in The Handbook of Liaison Psychiatry (Reference Guthrie, Sensky, Lloyd and GuthrieGuthrie 2007). The use of CBT in patients with medically unexplained symptoms is based on similar principles. However, it is sufficiently distinct to warrant separate consideration, which is beyond the scope of this article.Footnote †
The case vignettes presented here are fictional; however, they are representative of our experience in working with patients with physical illness, of their difficulties and the approaches used.
Use of CBT in physical illness
The core elements of the CBT model that we use to treat people with chronic physical illness remain very similar to the CBT model described by Reference Beck, Rush and ShawBeck et al (1979). We have also made use of the model described by Reference Williams and GarlandWilliams & Garland (2002) and the materials published by Reference WilliamsWilliams (2001), which are relatively jargon-free and therefore have a high level of acceptability to patients. When using CBT with patients with comorbid physical illness it is usually necessary to adapt and tailor treatment rather than using a standardised treatment package for the psychiatric disorder alone.
Although the remit of CBT in the overall treatment of people with chronic physical illness can be broader than simply treating comorbid psychiatric disorder, Reference Brown, MacHale, Freeman and PowerBrown & MacHale (2007) note in their literature review that the evidence is strongest for psychological interventions when they are targeted at patients with significant psychological symptoms (usually depression or anxiety) rather than being applied across the board to all patients with chronic physical illness.
Some potential indications for the use of CBT in the treatment of patients with chronic physical illness are listed in Box 1 and discussed in the following sections.
BOX 1 Possible indications for the use of CBT in patients with physical illness
-
• Comorbid psychiatric disorder
-
• Difficulties in adjustment to illness
-
• Difficulties in adherence to treatment
-
• Problems related to illness behaviours
Comorbid psychiatric disorder
The association between chronic physical illness and psychiatric disorder is long established. The evidence is particularly strong for depressive illness. The prevalence of depression in people with physical disorders has been reported to be as high as 40% (Reference Katon and SullivanKaton 1990; Reference Crum, Cooper-Patrick and FordCrum 1994). A number of other psychiatric disorders are also associated with physical illness, including anxiety disorders, adjustment reactions, post-traumatic stress disorder, and (more rarely) psychotic disorders.
Physical illness is a risk factor for developing psychiatric disorder. This may be mediated through psychological, biological and/or social processes. The two conditions can also occur coincidentally. The degree of interrelationship between the physical illness and the psychiatric disorder will vary on a continuum from a coincidental comorbidity with minimal overlap to high levels of interaction in symptoms, behaviours and contributory factors.
There are particular issues in the management of psychiatric disorder in patients with physical illness. The use of medication may be restricted by the risk of medical complications. Responses to illness can precipitate, perpetuate or exacerbate the psychiatric disorder. Psychiatric disorders can also lead to behaviours or require medication that influence the course of physical disorders.
There is evidence to support the use of both psychological (Reference Brown, MacHale, Freeman and PowerBrown 2007) and pharmacological treatment (Reference Gill and HatcherGill 2000) as adjuncts in the management of depression in chronic physical illness. It should be noted that CBT models are entirely compatible with the use of psychotropic medication.
The application of CBT to treat psychiatric disorder in patients with physical illness has been extensively studied. For example, a randomised controlled trial of CBT reported an improvement in anxiety and other psychological symptoms in people with cancer (Reference Greer, Moorey and BaruchGreer 1992). Other trials showed its beneficial effects on anxiety and depression in people with rheumatoid arthritis (Reference Sharpe, Sensky and TimberlakeSharpe 2001; Reference Evers, Kraaimaat and van RieaEvers 2002) and on depression in people with multiple sclerosis (Reference Larcombe and WilsonLarcombe 1984).
Depression is undesirable in its own right. It also has been shown to worsen the outcomes of physical disorders. In ischaemic heart disease, for example, depression is associated with increased morbidity and mortality independent of physical risk factors (Reference Frasure-Smith, Lespérance and TalajicFrasure-Smith 1993). The aetiological route of this association is not yet clear. This finding led to a great deal of interest in interventions that, by treating depression, might improve physical as well as psychosocial outcomes in coronary heart disease. In the Enhancing Recovery in Coronary Heart Disease (ENRICHD) trial, patients with a diagnosis of depression or with little social support were randomised following myocardial infarction to receive treatment as usual or CBT (Reference Berkman, Blunthal and BurnleyBerkman 2003). Those in the CBT arm were also treated with anti-depressants if they had severe depression or failed to respond to CBT. Disappointingly, CBT had no significant impact on mortality or recurrent myocardial infarction at follow-up. There has been debate about the reasons for these findings (Reference Frasure-Smith and LespéranceFrasure-Smith 2003). However, it is reasonable to conclude that we have no evidence that the relationship between depression and increased cardiac morbidity can be reversed by treating the depression with CBT.
Adjustment to illness
In the context of psychological treatment of people with cancer, Reference Faulkener and MaguireFaulkener & Maguire (1994) have described six hurdles that these patients have to negotiate. Failure to do so, they argue, leads to psychological problems. These hurdles are:
-
• managing uncertainty about the future
-
• searching for a meaning
-
• dealing with loss of control
-
• having a need for openness
-
• need for emotional support
-
• need for medical support.
Although this notion was developed in relation to cancer, we have found it a helpful concept with most chronic physical illnesses.
Adjustment to illness involves cognitive, behavioural and social change. There is evidence that a patient's perception of their illness rather than the illness itself has a greater influence on their psychological adjustment to chronic medical disorders (Reference SenskySensky 1990). Poor adjustment to illness and impaired functioning have been associated with negative perceptions of illness, rather than with measures of illness severity (Reference Scharloo, Kaptein and WeinmanScharloo 1998). Poor psychological adjustment to chronic health problems has undesirable consequences. For example, adherence to treatments for the medical illness is reduced (Reference Kimmel, Peterson and WeihsKimmel 1995) and ability to cope with physical symptoms such as pain is compromised (Reference Leibing, Pfingsten and BartmannLeibing 1999).
A number of studies have assessed whether CBT interventions to alter illness-related beliefs improve adjustment to illness in patients where this has been problematic. One reported that a self-management programme involving CBT reduced levels of disability and use of services, increased social activity and improved individuals' perception of health (Reference Lorig, Sobel and StewartLorig 1999). Another found that CBT reduced in-patients' psychological distress about inflammatory bowel disease (Reference Mussell, Bocker and NagelMussell 2003). A third, which used a cognitive–behavioural intervention designed to alter patients' perceptions of their illness following their first myocardial infarction (Reference Petrie, Cameron and EllisPetrie 2002), found that the treatment group returned to work earlier and had a significantly lower rate of angina symptoms than the control group.
Illness behaviours
A further potential application of CBT in the treatment of patients with physical illness is addressing illness-related behaviours, that is, the way in which people perceive, evaluate and act on physical symptoms (Reference MechanicMechanic 1962). For example, good glycaemic control in diabetes requires lifestyle management, appropriate responses to symptoms and adherence to treatment. A systematic review of randomised controlled trials of psychological interventions to improve glycaemic control in people with type 2 diabetes found twelve trials suitable for meta-analysis, eight of which were of CBT (Reference Ismail, Winkley and Rabe-HeskethIsmail 2004). There were improvements in long-term glycaemic control and psychological distress in the intervention groups.
Responses to illness may be perpetuated by secondary gain – positive outcomes contingent on the patient's sick role or behaviours. Note that this does not imply conscious malingering.
Case vignette 1: Secondary gain
Mr G had marital difficulties before he developed bowel cancer. During his illness, surgery and chemotherapy his wife was very attentive, caring and involved with him. He subsequently developed generalised anxiety disorder and did not return to his former level of functioning. During therapy it became apparent that he believed that ‘If I become more able and independent she will leave me’. This needed very sensitive exploration during treatment.
Adherence to treatment
Optimising patients' adherence to treatment is a very important aspect of the management of chronic physical illness, and the World Health Organization (2003) has produced a valuable overview of the subject. Cognitive–behavioural therapy may have a role to play in this field by intervening at the level of beliefs that are influencing adherence behaviours. For example, a randomised controlled trial found that group-based CBT was effective in improving adherence to fluid restrictions in patients undergoing haemodialysis (Reference Sharp, Wild and GumleySharp 2005).
Stages of CBT
Below we describe the stages of CBT with patients who have chronic physical illnesses. For simplicity it is described as a linear process. However, in clinical practice, aspects of assessment, formulation and engagement will recur throughout treatment.
Assessment of patients for CBT
Comprehensive assessment is central to effective CBT. The aim of assessment is to establish an overview of the patient's difficulties, to decide whether CBT is appropriate, to introduce the CBT model and to develop a preliminary CBT-based formulation. The assessment process we describe here should complement rather than replace the standard psychiatric assessment: both are necessary. During the assessment the therapist will be looking for links that provide information for the formulation. For example, in a person with diabetes the belief that ‘There is nothing I can do to change my illness’ may lead to a behavioural response of not checking blood sugar. Assessment can also highlight areas of strength and resilience. In complex cases it will usually take more than one session to carry out this assessment. This detailed exploration of the patient's presentation can be a very helpful way of establishing rapport and therapeutic alliance.
Box 2 lists a number of assessment issues that require particular emphasis in people with chronic physical illness. These are discussed in the following sections.
BOX 2 Important aspects of assessment
The clinician should assess:
-
• the patient's understanding of the reason for referral
-
• the patient's symptoms
-
• the patient's illness-related beliefs
-
• locus-of-control issues
-
• illness behaviour
-
• the social impact of illness
-
• the patient's self-concept
-
• suicide risk
The patient's understanding of the reason for referral
It is our experience that patients are often not sure why they have been referred for psychiatric or psychological assessment. It is important to ensure that they understand the reason for the referral and also to clarify what they expect from it.
Symptoms
A detailed comprehensive account of all of the patient's symptoms is an essential part of assessment. Important symptoms such as sexual dysfunction may not have been previously disclosed. The exploration of symptoms provides information for the formulation and also demonstrates the clinician's interest in the patient's physical illness.
Illness-related beliefs
These include the patient's beliefs about:
-
• the cause of the illness (in particular, whether the patient thinks that they or others may be to blame for it)
-
• the potential duration and course of the illness
-
• the seriousness of the illness and the likelihood of recovery, recurrence or death
-
• how the illness will affect the patient's life (and the lives of significant others)
-
• the significance or meaning of particular symptoms
-
• the adequacy of medical treatment and investigations.
Locus-of-control issues
-
• How much control does the patient believe they have over their illness or symptoms?
-
• How much control does the patient think they have over illness-related events, for example treatment, consultations with healthcare staff?
-
• How does the patient see their relationship with professionals?
-
• What are the patient's beliefs about what can influence outcome?
Illness behaviour
It is important to assess the following aspects of the patient's illness behaviour:
-
• consulting behaviour: attendance at arranged appointments; additional contacts with hospital services, general practice, accident and emergency
-
• adherence to treatment: an uncritical stance and questions such as ‘Do you ever try to cope without your medication?’ or ‘Many people forget to take regular medication. Is this a problem for you?’ can help patients disclose non-adherence
-
• use of potentially health-promoting behaviours such as diet, exercise and avoiding drugs and alcohol
-
• expression of affect, emotional responses to the illness and symptoms
-
• use of aids such as wheelchairs and crutches
-
• assessment of denial and avoidance
-
• any illness-related checking behaviours
-
• assessment of any secondary gain that may be promoting abnormal illness behaviour.
Social impact of illness
-
• Employment status, any changes due to illness, receipt of state benefits, status of any illness-related compensation claims
-
• Behavioural change, new behaviours, reduction of previous activities
-
• Effect on relationships, others' behaviours in response to the illness.
Self-concept
-
• Beliefs about role and any role changes that have occurred as a result of the illness
-
• Body image, how the patient views their body, how they perceive that it is viewed by others
-
• What the patient thinks the illness means about them as a person
-
• Beliefs about self-worth.
Assessment of risk of suicide
Suicide rates in people with chronic physical illnesses are higher than in the general population (Reference Moscicki and JacobsMoscicki 1999; Reference Appleby, Shaw and SherrattAppleby 2001). People with physical illnesses have high rates of depressive illness. They may also have ready access to means. Suicide is strongly associated with hopelessness, which in physically ill individuals may occur independently of depressive illness. It may relate to concerns about the inevitability of imminent death (which may be real) or the uncontrollability of painful and distressing physical symptoms. Being aware of the risk of suicide, assessing it regularly and considering appropriate risk management are essential in dealing with these patients.
Suitability for CBT
The Suitability for Short-Term Cognitive Therapy Rating Scale (Reference Safran and SegalSafran 1990: pp. 251–266) is a validated tool containing factors that indicate suitability for generic CBT. These include shorter duration of psychiatric illness, ability to access thoughts, and evidence of potential for therapeutic alliance.
Additional factors need to be considered in assessing the suitability of patients with chronic physical illness. There may be logistical difficulties associated with attending CBT sessions, such as poor mobility or appointments for medical treatment. For example, a patient who is attending hospital three times a week for haemodialysis may find it difficult or undesirable to add further appointments for CBT. Other factors to consider include impaired concentration due to physical symptoms, the prognosis of the medical condition and the acceptability to the patient of receiving a psychological treatment.
Other aspects of assessment
The traditional advice to ‘read the notes’ needs to extend to the patient's general hospital case notes. Much can be learnt from these, not just about the individual's illness but about the way they interact with staff and how others perceive them to be adjusting to the illness. The use of standard CBT assessment tools, including activity diaries and rating scales such as the Revised Illness Perception Questionnaire (Reference Moss-Morris, Wienman and PetrieMoss-Morris 2002), is encouraged. Other potentially useful rating scales include the Illness Attitudes Scale (Reference KellnerKellner 1986) and the Illness Behaviour Questionnaire (Reference PilowskyPilowsky 1969). Although these two scales have mostly been used with patients who have medically unexplained physical symptoms, we have at times found them also helpful in assessing people with diagnosed physical illnesses. Rating scales commonly used in the assessment of symptoms of anxiety and depression are subject to confounding in patients with physical illness. Symptoms such as sleep disturbance, appetite change and weight loss may be caused by the physical health problem or its treatment. Alternatives such as the Hospital Anxiety and Depression Scale (Reference Zigmond and SnaithZigmond 1983), which excludes somatic symptoms, can be more useful.
At the end of the assessment process it is useful to agree with the patient a list of problems and to carry out a functional analysis of each problem. Reference WhiteWhite (2001) has produced a useful list of questions to assist functional analysis, which we reproduce in Box 3.
BOX 3 Questions to assist functional analysis
-
• What makes the problem better/worse?
-
• Are there particular situations/times of day/people present when this occurs?
-
• Can you take me through a recent example in great detail?
-
• What situations does this problem occur/ not occur in?
-
• What happens right before you feel/think/do this?
-
• What happens after you feel/think/do this?
-
• What do you do then?
-
• What do others do when you feel/think/do this?
-
• What feelings do you get before this thought/before you do this?
-
• Do you get a warning that this is about to happen?
-
• What do you feel/think/do at this time?
(Reference WhiteWhite, 2001. © John Wiley & Sons. Reproduced with permission)
Engagement
Engagement is an important aspect of any psychotherapeutic treatment. There are some particular issues in relation to CBT for patients with physical illness. These include the information given by the referring clinician, the setting of treatment delivery, stigma regarding psychiatric treatment, and misconceptions that referral for psychological treatment indicates a psychological attribution of symptoms on the part of the referrer or the CBT therapist. Attention needs to be paid to these factors, to establishing a therapeutic alliance and to generating a shared understanding of the role of CBT in the patient's overall treatment. For further discussion of engagement in CBT see Reference Newman, Gilbert and LeahyNewman (2007).
Formulation
Formulation is essential in order to guide a coherent course of therapy. It is the conceptualisation of the patients' presentation within a CBT framework. The formulation is developed collaboratively and shared openly with the patient. A good formulation can enable interventions to be appropriately targeted and timed, difficulties to be understood and obstacles in therapy to be predicted or negotiated. Some people think that interventions in CBT are no more than formulaic responses to symptoms. However, the formulation enables the therapist to select interventions that are appropriate to the overall conceptualisation of a patient's difficulties. For example, social avoidance in a patient with diabetes may relate in patient A to fear of having a hypoglycaemic episode, but in patient B to the belief that they are now worthless. The interventions used will be very different.
Physical health problems are always accompanied by cognitive, behavioural and emotional responses. This can usually be easily conceptualised within a top-level CBT formulation such as that shown in Fig. 2. Note that the layout of this formulation has been adjusted from the typical layout that appears in Fig. 1. We have found that it is helpful to place the physical symptoms at the top of the formulation. This assists in the therapeutic alliance, as it reflects the patient's own experience of the prominence of their physical symptoms. The idea can be introduced at this stage that although physical symptoms may remain, change in the other domains can lead to an overall improvement in quality of life.
In some cases, a more comprehensive CBT formulation such as that illustrated in Fig. 3 may be needed. This incorporates broader aspects of the patient's experience, beliefs and premorbid vulnerabilities. Microformulations related to a particular area of difficulty may also be used (Fig. 4).
In enabling change it is very helpful first to understand what is perpetuating the current pattern of thoughts, feelings and behaviours.
Case vignette 2: The ‘purpose’ of behaviours
Mr B, a patient with diabetes, was referred with non-adherence to dietary change and medication. Careful assessment found that this was functioning to reduce his anxiety in the short term as it helped him to avoid reminders of being ill and risks of morbidity and death.
Within the formulation it is also important to elucidate the personal meaning of symptoms. Anyone experiencing a physical symptom will make a cognitive appraisal of its significance (Fig. 5). This may not be immediately apparent to the patient but is very important, since it governs behavioural and emotional responses and may be amenable to change.
Case vignette 3: Personal meanings
Mrs J, a woman with epilepsy and panic disorder, interpreted symptoms of light-headedness and tingling in her fingers to signify that she was about to have a seizure. This led to marked restriction in her activities. Re-evaluating this cognition during CBT and re-attributing these physical symptoms to anxiety led to marked improvement in her functioning.
Goal setting
Treatment aims are devised collaboratively with the patient, and associated goals are set. Where possible these goals should be specific and measurable. To enhance motivation they also must be achievable and relevant to both the problem and the patient. Each goal may need to be broken down into a series of steps, with cognitive and behavioural obstacles identified and addressed. Vague goals such as ‘to be healthier’ are unhelpful in guiding therapy and ascertaining outcomes. A more useful goal here might be to go for a 10-minute walk three times a week.
Interventions
Interventions should be guided by the formulation and by the patient's choice of targets for treatment. Treatment uses the standard features of CBT, including structured sessions, guided discovery, a collaborative approach and homework.
Cognitive interventions
The formulation
The development of a formulation is in itself an intervention that can lead to change.
Socratic questioning
The aim of Socratic questioning (Box 4) is to bring to the patient's attention information that they have but are overlooking. This can help in the reevaluation of previously held beliefs. Reference Beck, Rush and ShawBeck et al (1979) described it as eliciting ‘from the patient what he is thinking rather than telling him what the therapist believes he is thinking’.
BOX 4 Examples of the use of Socratic questioning
-
• To understand the problem
-
• What did that mean to you?
-
• If that did happen what would be bad about that?
-
• To look for exceptions
-
• What things don't fit this view?
-
• Have you been in a similar situation before? What was different?
-
• To reflect or summarise
-
• Am I right in thinking that…?
-
• So when you feel X, you think Y and do Z?
-
• To devise solutions
-
• What would you do differently next time?
-
• How would you check that out?
Case vignette 4: Socratic questioning
Mr C, a 40-year-old man with multiple sclerosis, spoke of being useless as a father because he was no longer able to be physically active with his sons. While acknowledging the loss this represented, the therapist used Socratic questioning to elucidate what playing football had meant to him and his sons, what was important to him about ‘being a father’, and the ways he could achieve this without being physically active.
Education
Education may be needed to fill gaps or redress errors in the patient's knowledge. In patients with physical illness this may include information about both psychiatric and physical disorders. Since people assimilate information better when they use active learning processes, the CBT therapist might set the patient a homework task of finding out more information and feeding back on this to the therapist. The therapist might also promote effective information-seeking behaviours for the patient to use in interactions with members of the general hospital service who are providing their care.
Cognitive restructuring
The starting point of cognitive interventions is to introduce to the patient the notion that thoughts are not facts: they may or may not be accurate. Cognitive restructuring often uses formal thought diaries that allow therapist and patient to evaluate the evidence for and against thoughts that are associated with negative affect or behavioural responses. An alternative appraisal is generated and tested using behavioural experiments.
Case vignette 5: Evaluating the evidence
Mrs K, a 50-year-old woman with diabetes and depression, noticed every occasion when she had poor memory, attention or concentration and catastrophically interpreted this as indicating that she was developing dementia. This exacerbated her low mood and anxiety, which in turn made her memory and concentration worse. The evidence for and against her belief that she had dementia was evaluated and she generated the alternative thought that although it was possible that she had dementia it was much more likely that depression and anxiety were causing her current memory difficulties.
In Beck's CBT model the focus is on dysfunctional beliefs, which are considered to cause or perpetuate maladaptive patterns of thinking, behaviour and emotion. In physical illness it must be recognised that illness-related beliefs might not necessarily be inaccurate. Indeed, dealing with ‘realistic’ negative thoughts is a not uncommon problem when using CBT in the setting of chronic and sometimes life-threatening illness. Reference Moorey and SalkovskisMoorey (1996) provides an excellent and comprehensive account of how to deal with this. One of the golden rules of CBT is ‘never assume you understand what the patient means’. This is an exhortation to regularly ask clarifying questions, and the value of this when faced with a patient's realistic negative thoughts is clear. For example, when treating a patient with a poor prognosis whose most troublesome thought is ‘I'm going to die’, it is pointless to try to challenge reality but fruitful to explore what it is about dying that troubles the patient most. Asking clarifying questions along these lines may identify a range of issues that can be tackled, such as religious concerns, worry over how they will cope with distressing symptoms before death or how others will cope with their loss.
Cost–benefit analysis
A cost–benefit analysis can be a useful way of helping a patient to evaluate a pattern of behaviour or thinking that is being reinforced by short-term gains.
Case vignette 6: Costs v. benefits
Mr D, a 27-year-old man, had a severe asthma attack necessitating intubation and admission to intensive care. Following his physical recovery he remained very anxious. He restricted the places he would go to, so that he could always be near a hospital ‘just in case’. He also frequently attended the accident and emergency department and his general practitioner. He had many readily accessible automatic thoughts and images relating to his asthma. These included ‘If I have another severe attack I'll die’ and ‘If I'm not close to a hospital I'll die’. Some of his automatic thoughts were not entirely unrealistic. He was at risk of further asthma attacks and significant morbidity or death. However, the formulation suggested that he was overestimating the probability of this, finding it very difficult to cope with the uncertainty, and functioning in a very limited way because of his excessive focus on aiming to avoid the possibility of becoming unwell. One intervention used was a cost–benefit analysis that highlighted the costs to him of his behaviours versus the benefits.
Schema-focused therapy
The concept of a schema uses the hypothesis that people have relatively stable underlying core beliefs. These may not be problematic until a set of circumstances makes it impossible for the patient to maintain healthy functioning. Schema-focused therapy involves an in-depth exploration of these beliefs and the introduction of interventions to alter them. Alternative beliefs are generated and strengthened.
Case vignette 7: Challenging core beliefs
Mr B had core beliefs that he was worthless, un acceptable and that others were harsh and judgemental (see formulation in Fig. 3). He had been able to compensate for this by working hard. When diabetes forced him to give up work, his core beliefs became more dominant. In addition to interventions targeting his current symptoms it was necessary to work with him at the level of his core beliefs in order to help him to achieve and maintain change.
Behavioural interventions
Behavioural activation
The sick role (Reference ParsonsParsons 1961) includes the idea that the person is no longer obliged to fulfil previous roles. It is entirely normal and appropriate in acute illness for people to reduce activity. This can encompass social withdrawal, absence from work and reduction in family responsibilities. It can facilitate rest and recuperation. However, when illness and symptoms persist, this response can become problematic. It no longer offers the prospect of recovery but carries detrimental effects that include physiological changes with de-conditioning, muscle wasting, pain and heightened fatigue. There will also be a reduction in experiences of pleasure and achievement. The patient can become socially marginalised and to a degree resented by those around them. Behavioural activation seeks to reverse these effects by increasing levels of activity.
Case vignette 8: The downward spiral of inactivity
Mr G, aged 48, was on renal dialysis and presented with fatigue, low mood and hopelessness. There was clearly a biological component to his difficulties. It was also unrealistic, given his physical illness, for him to return to his premorbid work and level of activity. This had contributed to his sense that there was no point in doing anything. He completed activity diaries for two weeks, and these showed a very low level of activity and few things that gave him any sense of enjoyment or achievement. He was able to see how this exacerbated his low mood. He then started to engage in gradually increasing levels of activity, prioritising those that gave pleasure or achievement. He began with sending emails and built up to resuming social contact with friends he had been avoiding.
Graded exposure
Graded exposure can be used in working towards a planned goal. One application is in the treatment of phobias. Needle phobia is common (Reference MarksMarks 1988) and can be an undisclosed reason for poor adherence to treatment and failure to attend appointments.
Case vignette 9: Overcoming phobias
Mrs L had haemochromatosis but her phobia of needles had prevented her from attending venesection or haematology appointments for more than 12 months, leading to significant risk of complications. She was treated with systematic desensitisation to needles through graded exposure. A hierarchy of anxiety-provoking stimuli was drawn up, from those she perceived as mildly threatening up to those she rated as highly anxiety-provoking. They included imagining having blood taken, the smell of alcohol wipes, handling a syringe, seeing a syringe and needle and having blood taken. She was taught counterresponse techniques to enable her to generate responses inconsistent with anxiety and a vasovagal attack. These included tensing muscles, self-reassurance and visualisation of a situation that would provoke anger. She was then exposed to each item in the hierarchy in turn either in session or as homework.
Behavioural experiments
A behavioural experiment is an agreed activity, the purpose of which is to gather more information, change an existing behaviour or test a cognition. Such experiments can be very powerful in facilitating change, as previous avoidance may have resulted in the patients' failing to gather information which would counter maladaptive cognitions. Moreover, behavioural experiments are experiential and therefore can generate powerful affect, which can produce change.
Case vignette 10: Steps towards recovery
Mrs B was a 58-year-old woman with a history of hypertension, who had had a stroke (from which she had made a complete recovery) 5 years previously. She was anxious and had become increasingly housebound. During assessment she revealed that she believed if she exercised she would raise her blood pressure and have another stroke. She therefore avoided even gentle exercise. Detailed assessment revealed that she could not climb the stairs in her own home without a number of elaborate checking rituals. At the bottom of the stairs she would check her pulse and look in a small mirror she carried with her at all times (she believed that if her face was flushed this was a sign of an imminent stroke). As she climbed the stairs, she stopped every two steps to repeat this ritual. If her pulse had risen from its baseline level or she thought she looked flushed she would rest until her pulse and appearance ‘normalised’. The therapist gave her information on the role of exercise in cardiovascular and cerebrovascular disease and a behavioural experiment was set up in which she eliminated these checking behaviours when climbing the stairs. Over a period of time this enabled her to challenge her belief that exercise was dangerous and to resume previously abandoned physical activities.
Pacing
People may respond to symptoms with an ‘all or nothing’ pattern of activity. This can become a self-perpetuating cycle. When they feel relatively well they are comparatively overactive, leading to a resurgence of symptoms of pain and fatigue, which are responded to with comparative underactivity. Pacing aims to break this cycle by setting a baseline sustainable level of activity, which can be gradually increased.
Relaxation training
Relaxation can be used as a component of CBT in the treatment of medical illness.
Case vignette 11: Instilling self-efficacy
Miss M, a woman with tinnitus and associated generalised anxiety disorder, believed that there was nothing she could do to influence her anxiety or her tinnitus. She was taught progressive muscle relaxation using a CD. In a subsequent behavioural experiment she rated both her tinnitus and her anxiety before and after using the relaxation CD, and noted a reduction in both. This helped her to manage her anxiety and to increase her belief in her self-efficacy at symptom management.
Refocusing attention
Focusing attention on a particular symptom or body system tends to heighten awareness of them and therefore make them more troublesome. This may be particularly problematic if the symptoms are associated with negative cognitive appraisals. Demonstrating this link through behavioural experiments and information from the formulation, then helping the patient to set goals to shift their focus onto other areas of functioning and experience can be very important components of treatment.
Case vignette 12: Finding another focus
Mrs P had had a mastectomy for breast cancer. She was referred with depression and anxiety. Assessment revealed that she frequently checked for signs of recurrence, palpating the site of the mastectomy, checking her axillae and neck for enlarged lymph nodes and attending to bodily sensations. Her attention led her to become more aware of normal physical sensations and then misinterpret them as being sinister. The frequent palpation also caused pain and lymphadenopathy. The therapist presented this possible explanation to her as a microformulation and asked her to carry out a behavioural experiment. She rated her anxiety for two days of her usual behavioural pattern, then for a week during which she reduced checking behaviours. Initially, her anxiety increased but towards the end of the week of reduced checking she found it easier to redirect her attention to other activities and her overall level of anxiety reduced.
Emotion-focused interventions
Traditional CBT has addressed emotions indirectly through cognitive and behavioural routes. A growing list of new approaches, including acceptance and commitment therapy (Reference Hayes, Luoma and BondHayes 2006) and compassionate mind training (Reference Gilbert and ProcterGilbert 2006),Footnote ‡ incorporate techniques that help the individual to tolerate emotions. There has been specific research investigating the application of acceptance and commitment therapy to patients with physical health problems (e.g. Reference McCracken, Vowles and EcclestonMcCracken 2005). The goal of treatment is to help patients to tolerate and experience their emotions rather than attempt to avoid them. Mindfulness (Reference Segal, Williams and TeasdaleSegal 2001) and mindfulness-based stress reduction (Reference Kabat-ZinnKabat-Zinn 2003) are finding increasing applications for chronic pain and for physical illnesses, including psoriasis (Reference Kabat-Zinn, Wheeler and LightKabat-Zinn et al 1998) and prostate cancer (Reference Saxe, Hebert and CarmodySaxe 2001). These are promising interventions.
Relapse prevention
Towards the end of treatment the therapist addresses the possibility of a future recurrence of difficulties and the need for a plan to deal with this. The patient is encouraged to identify personal warning signs and potential responses. Usually, the patient will plan to use techniques that they found helpful in treatment to maintain and further improve on treatment gains.
Ending treatment
Decisions on ending treatment are not based on complete resolution of physical or psychological symptoms. Complete symptom resolution may not even be possible. The rationale of CBT is to give patients the skills and the ability to address their own symptoms. One indication for discharge would be when a patient has acquired these skills.
The therapist explicitly reviews with the patient their response to CBT throughout treatment. If CBT is proving to be ineffective it is important to acknowledge this, and end treatment. The use of other adjunctive interventions such as antidepressants would also be continuously reviewed.
Treatment delivery
Practitioners of CBT remain a scarce resource, and ways of improving the availability of the intervention are being sought. These include computer-assisted CBT (Reference Gellaty, Bower and HennessyGellaty 2007) and the training of general nurses in medical settings to administer brief CBT-based interventions (Reference Strong, Sharpe and CullStrong 2004).
Clinicians must carefully consider how best to deliver treatment to patients who might benefit from it. Resources are not infinite, so a stepped-care model in which more intensive treatment is targeted at those most likely to need this level of intervention would be appropriate (Box 5).
BOX 5 A suggested hierarchy for service delivery
| Patient group | Clinician | Intervention | Clinical practice example |
|---|---|---|---|
| At risk of psychological problems | General hospital | Use of CBT principles within routine medical care | Cardiac nurses delivering cardiac rehabilitation course |
| Identified as having problems with psychological adjustment to illness | General hospital/community medical staff | Use of CBT principles in targeted care and interventions | Diabetes nurses using CBT formulation and interventions for patients with poor treatment adherence |
| Identified as having mild comorbid psychiatric disorder appropriate for CBT treatment | General hospital/community medical staff | Use of CBT self-help book or computer package | Provision of CBT self-help to patients attending a diabetes clinic identified on screening for depression |
| Identified as having moderate or severe comorbid psychiatric disorder appropriate for CBT treatment | CBT practitioner | Group or individual CBT for psychiatric disorder, some adaptation to physical disorder components of presentation | Patient with arthritis and depression attending community mental health team |
| Complex or intractable difficulties with psychological adjustment to illness | CBT practitioner with training and experience in working with patients with physical illness | Group or individual CBT targeting illness beliefs and behaviours | Patient with diabetes who has persistent poor adherence to treatment and lifestyle modifications |
| Complex comorbidity with high interrelationship between psychiatric and physical disorder | CBT practitioner with training and experience in working with patients with physical illness | Group or individual CBT highly adapted to meet medical and psychiatric components of presentation | Patient on haemodialysis with depression, hopelessness, suicidal ideation and poor treatment adherence |
It would be impractical and inappropriate for all patients with physical illness and comorbid psychiatric or psychological problems to be seen by psychiatric services. Many can receive interventions within primary care; others can be helped by general hospital clinicians who have appropriate training. More controversial, perhaps, is whether any patients without a psychiatric disorder should be seen by psychiatric services. The need for intervention is demonstrated by increased rates of morbidity in patients who have problems adjusting to physical illness. There is evidence that it is cost-effective to intervene (Reference Chiles, Lambert and HatchChiles 1999).
Cognitive–behavioural therapy is most effective when delivered with good adherence to the CBT model (e.g. Reference Davidson, Scott and SchimidtDavidson 2004), but this requires training and supervision. Staff in psychiatric services may have the experience and expertise necessary to engage, formulate and intervene in complex cases. Decisions on service delivery models and training must be made at the managerial level of general medical and psychiatric services.
Cognitive–behavioural therapy can be extremely helpful in the overall treatment of people with chronic physical illness. Careful selection of those most likely to require and benefit from CBT is important, but more research is needed to make these decisions evidence-based.
MCQs
-
1 CBT for patients with physical illness:
-
a is useful only if they have a comorbid psychiatric disorder
-
b must be delivered by a psychiatrist
-
c is contraindicated if the patient is suicidal
-
d is an appropriate intervention with a patient who has capacity but refuses to consent to treatment
-
e can be used in conjunction with pharmacological treatment of both physical and psychiatric illness.
-
-
2 Adjustment to illness:
-
a is a single-stage process
-
b is determined by symptom severity
-
c cannot be improved using CBT
-
d influences adherence to treatment
-
e results in the patient being able to maintain their previous behaviours.
-
-
3 With regard to behavioural experiments:
-
a they can be very powerful in facilitating change
-
b the therapist decides what the patient should do
-
c they have little value in CBT when patients have physical illness
-
d it is important to make sure that affect is minimised
-
e they must be conducted in the presence of the therapist.
-
-
4 Useful CBT interventions often include:
-
a making choices for the patient about their treatment
-
b discharging the patient if their physical illness is terminal
-
c using Socratic questioning to devise possible solutions to a problem
-
d telling the patient not to worry about their symptoms
-
e ensuring patients do the maximum level of activity possible.
-
-
5 Research regarding the use of CBT in patients with physical illness:
-
a showed a reduction in mortality in cardiac patients whose depression was treated with CBT
-
b is limited to uncontrolled studies and case reports
-
c excludes patients with neurological disorders
-
d provides an evidence base for CBT in the treatment of depression or anxiety in patients with comorbid physical illness
-
e shows no effect on adjustment to illness.
-
MCQ answers
| 1 | 2 | 3 | 4 | 5 | |||||
|---|---|---|---|---|---|---|---|---|---|
| a | f | a | f | a | t | a | f | a | f |
| b | f | b | f | b | f | b | f | b | f |
| c | f | c | f | c | f | c | t | c | f |
| d | f | d | t | d | f | d | f | d | t |
| e | t | e | f | e | f | e | f | e | f |
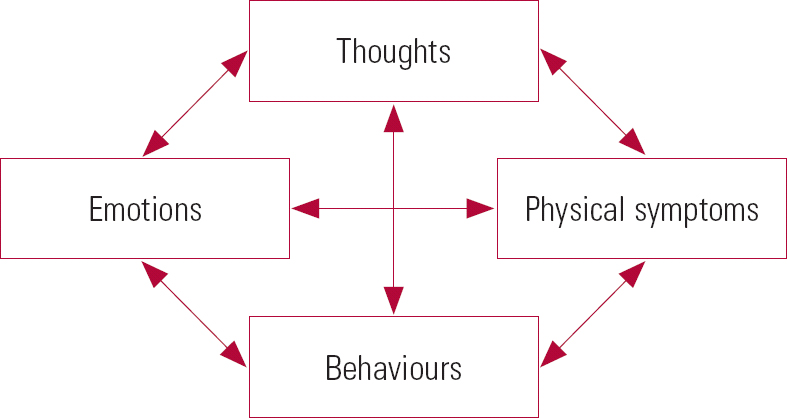
FIG. 1 Top-level CBT formulation.
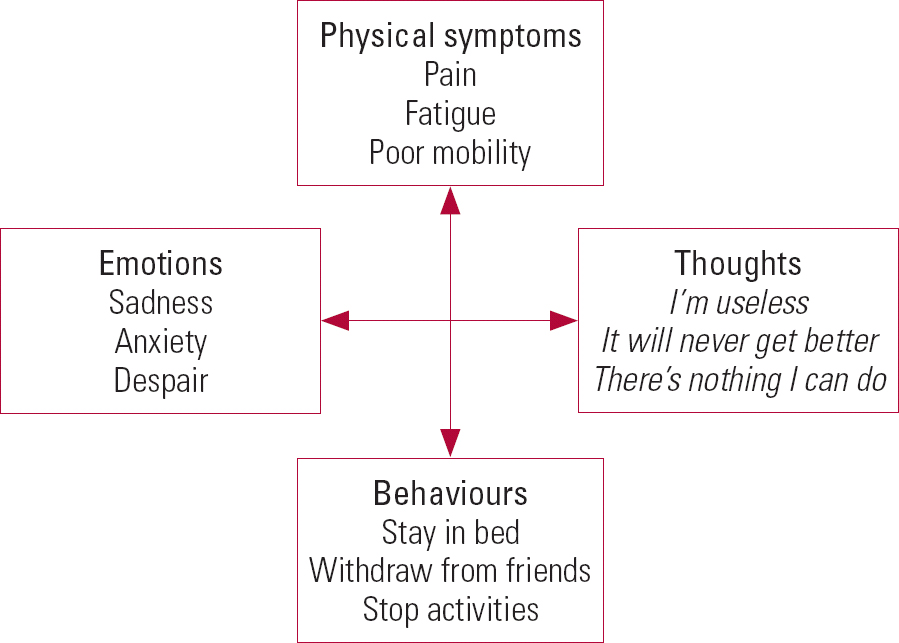
FIG 2 Application of top-level CBT formulation to a patient with multiple sclerosis and depression.

FIG 3 Case formulation in a man with diabetes and depression.
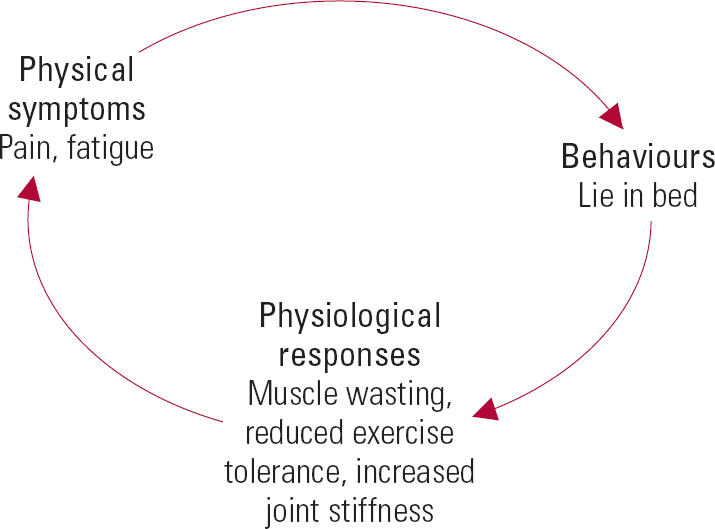
FIG 4 Microformulation of links between symptoms and behaviours in a patient with arthritis.

FIG 5 Symptom appraisal.








eLetters
No eLetters have been published for this article.