The merging of behaviour and cognitive therapy into cognitive–behavioural therapy (CBT) occurred in the 1980s in both Europe and North America, particularly on the basis of the successful treatment of panic disorder by Clark (1986) in the UK and Barlow (1988) in the USA. The behavioural emphasis on empiricism with good-quality research design was combined with the cognitive focus on content and meaning. In child and adolescent psychiatry, this process happened rather later but in a similar way, defined by Kendall (1993) thus:
“cognitive–behavioural approaches can be defined as a rational amalgam: a purposeful attempt to preserve the demonstrated positive effects of behaviour therapy within a less doctrinaire context and to incorporate the cognitive activities of the client into the efforts to produce therapeutic change. Accordingly, cognitive–behavioural strategies with children and adolescents use enactive, performance-based procedures as well as cognitive interventions to produce changes in thinking, feeling and behaviour.” (p. 235)
In comparison with CBT for adults, there have been relatively few studies of its use with children, although evidence for effectiveness is steadily mounting.
Adapting CBT for children and adolescents
As with other developments in paediatric medicine, clinicians using CBT with children have initially had to extrapolate from findings with adults, using their expertise with children to adapt appropriately. And as with adult CBT, the therapy model continues to evolve and is beginning to be evaluated.
Particular adaptations that therapists make in working with children are to do with pacing the content and speed of therapy at a level appropriate for the child, bearing in mind the younger child's limitations in metacognition and ineptitude in labelling feelings. With younger children, the therapist is likely to be more active and will make use of a higher proportion of behavioural to cognitive techniques.
Although with adults much work in CBT, especially with patients with neurotic disorders, is concerned with correcting maladaptive and dysfunctional distortions of thinking, many children have major deficits in social skills or interpersonal problem-solving. Training in social skills and problem-solving are a part of interventions not only for children with conduct disorder, attention-deficit hyperactivity disorder (ADHD) or empathy disorders, but also for children with depression or anxiety and whose impaired social relationships are a strong predictor of poor recovery (Reference Goodyer, Germany and GowrusankurGoodyer et al, 1991).
Application of CBT with children and adolescents
Applications to particular disorders have been well described in Graham's Cognitive–Behaviour Therapy for Children and Families (Reference GrahamGraham, 1998), which should be recommended reading for child and adolescent psychiatrists.
The content of the cognition may be typical of the disorder or mood. For example, depression may raise thoughts of worthlessness and personal loss – “no one will love me, I will be alone”; anxiety may give thoughts of danger, fears for personal well-being in the future and catastrophising – “it will be a disaster, I'm going to crack up”; and anger may see transgression of personal rules – “it's not fair”.
Psychiatric disorders in children can be conceptualised as those where the main problem is that of cognitive distortions, which are prominent in emotional disorders, obsessive–compulsive disorders (OCD), depression, somatising problems, and post-traumatic stress disorder, and those where there is mainly a cognitive deficit of social skills and problem-solving, such as conduct disorder or ADHD.
Conditions involving cognitive distortion
Depression
The Beckian cognitive model applies well to emotional disorders, especially depression (Fig. 1). Fennell (1989) gives an excellent description of CBT for depression in adults, which can be used for sophisticated adolescents.
Working with adolescents suffering from depression follows the structured and collaborative approach typical of CBT. Each session includes setting the agenda for the session, review of ‘homework’ from the previous session, goal setting of tasks for the session and practising tasks in the session. Homework is agreed, which may involve tasks practised in the session and problem-solving to anticipate difficulties. Each session will involve frequent summarising with feedback from the young person.
Making a problem list not only clarifies things, but also enables the young person to experience CBT as collaborative, in that the therapist is trying to understand the young person's perspective and priorities.
The formulation (as in Fig. 1) begins to link the present problems with the cognitive model and highlights the vicious cycle of negative thinking, low mood and social withdrawal typical of depression.
Diagrams are often more helpful than words in thinking and communicating about formulations. Positive-feedback loops, which may be crucial in maintaining problems, can be more easily identified. The therapist makes frequent short summaries of the situation and asks for feedback to ensure that these accurately reflect what the adolescent means, using phrases such as “Let's see: have I got this right? That you feel it is all your fault that things have gone wrong?”
The next step is emotional recognition, helping the adolescent in the session to distinguish between different emotional states and starting to link emotions with events and thoughts. This will be expanded by self-monitoring, using charts and diaries in which the young person observes his or her thoughts and makes specific causal links between events, moods and thoughts. For those sensitised to the word ‘homework’, this task may be renamed an ‘assignment’ or ‘an experiment to test a hypothesis’.
Activity scheduling can be used to overcome the social withdrawal and behavioural inertia that frequently accompany depression. Realistic goals should be set, with small steps along the way. Selecting affect-enhancing activities can be used as self-reinforcement for each successive step.
Coping-skills training will involve working on social interaction (e.g. how to start a conversation or make a friend) and social problem-solving (e.g. how to resolve a conflict without antagonising others).
Reducing depressive thinking by cognitive restructuring includes monitoring and evaluating thoughts, detecting negative automatic thoughts (NATs) and reality-testing these NATs by examining the evidence for and against and searching for alternative explanations. This is designed to deal with the negative style of thinking to which an adolescent suffering from depression is liable. It makes use of thought diaries (Fig. 2), verbal challenging and eliciting alternatives in the sessions by the use of sensitive Socratic questioning.
For children and less sophisticated adolescents, Wood & Harrington have produced a clear manual of their Depression Treatment Programme (DTP; available from R. C. Harrington, Department of Child and Adolescent Psychiatry, Royal Manchester Children's Hospital, Hospital Road, Pendlebury, Manchester M20 1HA). This includes useful charts and is supplemented by a videotape for clinicians. It can be used by child mental health professionals with minimal additional training.
After the initial assessment session, including an assessment of suicide risk, the standard intervention comprises eight 40-minute sessions. These may be used in modular form to meet each child's needs.
Although effective for children with depression, particularly minor depression, a programme of five to eight sessions over 8 weeks had a high rate of relapse 2 months after apparent remission. A longer version had a substantially lower relapse rate (Reference Kroll, Harrington and GowersKroll et al, 1996). The present DTP is a 10–14-session programme over 10–12 weeks with four booster sessions over the next 8 weeks (Reference Harrington, Wood, Verduyn and GrahamHarrington et al, 1998).
Anxiety disorders
Pathological anxiety occurs when an individual overestimates the probability that a feared event (catastrophe) will occur, or the severity of the event when it does occur. There is a simultaneous underestimate of the coping resources and the likely rescue factors. For example, a child refusing to go to school may think “I will look an idiot, it will be a disaster, I won't be able to survive it, no one will help”.
Thus, there is a negatively distorted cognitive appraisal, where the child is likely to be obsessively self-focused, hypercritical, concerned about evaluation of him- or herself and biased towards perceiving threat in any ambiguous situation. In addition, there is likely to be physiological alerting and arousal leading to somatic sensations, as well as marked behavioural avoidance (Fig. 3). Because the child is avoiding the situation (e.g. school), there is no opportunity to test predictions of catastrophe. If the child tries to leave home, the anxiety level rises with concomitant somatic symptoms such as a racing pulse, stomach cramps and agitation, together with catastrophising thoughts (“It will be a disaster”) and images (for example, of being taunted at school). These may overwhelm the child, who then returns home. Following the escape/avoidance, the child immediately feels better, reinforcing the behavioural avoidance pattern, which becomes a powerful maintaining factor.
Cognitive–behavioural therapy for anxious children can be built around a formulation of the problem in cognitive–behavioural terms. For example, a boy avoiding school after illness may have potent feelings, images and thoughts of a disastrous inability to cope on return to school; he may, by avoidance behaviour, maintain and increase his fears. A functional cognitive assessment will identify antecedents and consequences of behavioural avoidance, as well as somatic and emotional responses together with the precise thoughts and images relating to that specific situation for that particular child.
A modified thought diary (Fig. 2) may be useful here. Teaching the child to self-rate distress or discomfort on a 0–10 scale, called a subjective units of distress scale, is helpful in reflecting progress and moving the child from helpless victim mode to observer mode. The aim is to enable the child to recognise triggers and early signs of anxious arousal. The child is then taught anxiety management skills such as applied relaxation and positive imagery.
The catastrophising cognitions may be challenged by looking at the evidence supporting or refuting them with questions such as: “Is there another way of looking at this?”, “What would the little green man from Mars think?”, “What would a friend think?” and “What would a friend do?”
Gradually, more positive self-talk is developed, for example “If I just sit still and get on with my work, I will begin to feel better”.
As with treating depression, the level of sophistication of the child may determine the degree to which adult-type cognitive strategies can be used.
A treatment manual for a 16-session programme (Reference Kendall, Kane and HowardKendall et al, 1990) has been produced to provide a ‘coping template’ for the management of anxiety. This uses the acronym FEAR to prompt the child's own four-step coping:
-
• Feeling frightened? (Awareness of bodily cues, identifying anxiety and learning to relax)
-
• Expecting bad things to happen? (Identifying and correcting maladaptive self-talk by using positive self-talk)
-
• Attitudes and actions that can help. (Coping and problem-solving strategies)
-
• Results and rewards. (Self-evaluation and coping with failure)
Kendall has also produced a useful children's workbook containing charts and materials (the Coping Cat Workbook and Notebook; Kendall, 1994a).
This programme was found to be effective in a randomised controlled trial (Reference KendallKendall, 1994b ) with gains maintained at 3 years (Reference Kendall and Southam-GerowKendall & Southam-Gerow, 1996).
A Family Anxiety Management (FAM) programme has been developed (Reference Barratt, Dadds and RapeeBarratt et al, 1996). This teaches parents contingency management (rewarding appropriate coping behaviour and extinguishing avoidance behaviour) and management of their own anxiety, and works on communication and family problem-solving. Adding 12 sessions of FAM improved the effectiveness of an individual programme for children with anxiety disorders.
Obsessive–compulsive disorder
There are currently fascinating developments in the treatment of OCD with CBT. The cognitive model suggests that perceived responsibility for harm to self or others is at the heart of OCD (Reference Salkovskis, Kirk, Clark and FairburnSalkovskis & Kirk, 1997; Reference ShafranShafran, 1997).
Obsessions are intrusive cognitions that make patients think they will be responsible for harming themselves or others unless they take preventive action. The patient's appraisal of experiencing intrusive thoughts and their content leads to intense discomfort. They then attempt to suppress and neutralise the thought, image or impulse. Compulsive behaviours or thought rituals are neutralising actions intended to reduce this discomfort. But attempts to suppress and control intrusive thoughts and the use of neutralising behaviours lead to a rebound increase in the frequency and intensity of the thoughts, with consequent distress leading to a vicious spiral of increasing efforts to control them and their recurrence.
Two further distortions of responsibility are present: the belief that thinking something is the same as doing it – thought–action fusion; and undue sensitivity to responsibility for omission (“If I don't remove every speck of dirt, someone might become contaminated”). Fig. 4 shows a model of OCD for a specific example.
Recently there has been a shift of emphasis towards the view that the problem in OCD is not the intrusive thought itself but its interpretation. Moving the therapeutic focus to the appraisal of the intrusive thought (metacognitive appraisal) has produced promising results in an open study of six adolescents aged between 12 and 17 (personal communication, T. Williams, 1999).
Following a precise diagnostic assessment of the severity of the OCD, the therapist explains to the child that OCD is primarily a disorder of appraisal of normal but unpleasant intrusive thoughts in a person who is liable to feel excessive responsibility. The aim is to enable the child to appreciate that anyone can have odd thoughts and the way to deal with them is to ignore them. Trying to avoid, suppress or neutralise the thoughts will only cause them to return more strongly than before. The therapist might use stories about habits and intrusive thoughts and the effects of control. For example, asking the child to try not to picture a white bear in a red landscape will show that such an attempt at control might actually increase the frequency of this thought. Behavioural experiments using a graded-exposure format may be set as homework tasks. This technique is now being tested further in a randomised controlled trial.
The addition of anxiety management training (AMT) to CBT helps the child to carry out exposure and response prevention. This combination of CBT and AMT has increased the effect size (Reference March and MulleMarch & Mulle, 1998; Reference Van Oppen, de Haan and van BalkomVan Oppen et al, 1995; Reference De Haan, Hoogduin and BuitelaarDe Haan et al, 1998; Reference Shafran and GrahamShafran, 1998).
Eating disorders
There are few studies of treatment with CBT in anorexia nervosa, perhaps because of the often life-threatening presentation. Eclectic multi-faceted approaches are most frequently used.
In bulimia nervosa CBT is the gold-standard treatment (Reference Schmidt and GrahamSchmidt, 1998), but it has not been evaluated for use with adolescents. Furthermore, as only 50% of patients recover fully (Reference WilsonWilson, 1996), further refinements of CBT using exposure methods, including an interpersonal focus, intensifying the cognitive restructuring and treating comorbid personality disorders using dialectical behavioural therapy (Linehan, 1993) are necessary.
An interesting development in CBT for bulimia nervosa is the concept of stepped care, where a lower-cost intervention in the form of a self-help manual is tried first (Reference Schmidt and TreasureSchmidt & Treasure, 1993; Reference CooperCooper, 1995; Reference FairburnFairburn, 1995). Although 20% fully recover with self-care alone, if individual therapist-guided sessions are added after or during the use of the manual – guided or sequential self-care – the recovery rate rises to 30–50% (Reference Schmidt and TreasureSchmidt & Treasure, 1993; Reference Treasure, Schmidt and TroopTreasure et al, 1996).
Disorders involving cognitive deficits
Conduct disorder
Working with children of all ages with conduct disorders is a therapeutic challenge. For young children, parent-management training has been clearly demonstrated as effective in both group and individual formats (Reference Webster-StrattonWebster-Stratton, 1982, Reference Webster-StrattonWebster-Stratton, 1984, Reference Webster-StrattonWebster-Stratton, 1989; Reference PattersonPatterson, 1982). In training the parents, problems of engagement and high drop-out rates remain, but these can be addressed to some extent by sensitive and collaborative use of cognitive–behavioural methods to modify the parental beliefs that prevent effective child management (Reference Webster-Stratton and HerbertWebster-Stratton & Herbert, 1994).
When used for conduct disorder, CBT must be part of a multi-modal approach. This should involve not only parents but also the school, where teachers may be helped by advice on management and by training in positive teaching methods (Reference Wheldall, Merritt and WheldallWheldall & Merritt, 1991) and structured approaches to bullying (Reference OlweusOlweus, 1994).
Children with conduct disorders are frequently deficient in social skills and general problem-solving strategies. Social-skills training is frequently used and it has a small effect as part of a multi-modal package (Reference HollinHollin, 1990). Operant techniques rewarding prosocial behaviour and discouraging antisocial behaviours are supplemented by instruction, discussion, modelling strategies, rehearsal, prompting and feedback. Coping modelling using a model who talks through a task and describes how to deal with setbacks was found to be more effective than mastery modelling of perfect behaviour (Reference Goodwin and MahoneyGoodwin & Mahoney, 1975). Coaching can be used to teach principles of competent social behaviour, supplemented by role-play and the use of videotape feedback.
Most problem-solving skills training (PSST) programmes contain similar elements: emotional education; self-monitoring of feelings and behaviour; self-instruction using inhibitory self-talk; self-reinforcement; social-perspective-taking, using vignettes etc. to enable the child to understand the intentions of others in social situations; and social problem-solving.
The Think Aloud programme (Reference Camp and BashCamp & Bash, 1985) uses a cartoon bear to teach a self-instructional approach to social problem-solving: the bear models the stages in problem-solving by asking such questions as “What is the problem?”, “What can I do about it?”, “Is it working?” and “How did I do?” For older children, stages in problem-solving are identified as: first, identifying and defining the problem and any associated feelings; second, alternative thinking to generate several possible solutions (including asking “What would the little green man from Mars suggest?” as a way of introducing objectivity); third, looking at the pros and cons of each solution; and finally, decision-making, carrying out the plan and monitoring the outcome.
Children with conduct disorders find it hard to generate verbal assertive (negotiating) solutions to interpersonal problems and resort to action-oriented and aggressive solutions.
A PSST intervention for 9–13-year-old in-patients with conduct disorder produced clinically significant improvements evident 1 year later (Reference Kazdin, Esveldt-Dawson and FrenchKazdin et al, 1987), and it was enhanced by combination with parent-management training (Reference Kazdin, Siegel and BassKazdin et al, 1992).
Anger management programmes help adolescents to identify their aggressive behaviour and the conditions that provoke and maintain it. A controlled study of a school-based programme demonstrated sustained improvement of the treated group at 3-year follow-up (Reference LochmanLochman, 1992).
Children with conduct disorders tend to attribute hostility to others and underestimate their own aggression in any conflict. When upset they anticipate fewer feelings of fear or sadness, interpreting strong feelings as anger and react aggressively. They value aggression as effective in problem-solving and enhancing their self-esteem.
In young children these distorted cognitions can be dealt with in parallel with PSST by continued reference to concepts of fairness, safety and what the other person feels (Reference Bailey and GrahamBailey, 1998). In older children the problem is difficult: a range of programmes has been developed (Reference Herbert and GrahamHerbert, 1998). For all age groups, explicit work towards generalisation and programme integrity is important.
Attention-deficit hyperactivity disorder
Self-instructional training programmes might be thought to be appropriate for children with ADHD, who have core problems of inattentiveness, impulsivity and restless overactivity (the inability to ‘stop, look, listen and think’). The programmes essentially train children at home and/or in the classroom using a five-step approach summarised in Box 1. Kendall's (1989) Stop and Think Workbook would be useful support to such a programme.
Box 1. Self-instructional training programme: the five-step approach ( Reference Meichenbaum and Goodwin Meichenbaum & Goodwin, 1971 ; Reference Kendall and Braswell Kendall & Braswell, 1993 )
-
1 Watching a trainer model and talk through a task, including planning and talking through possible difficulties (cognitive modelling)
-
2 Carrying out the task, prompted by a trainer
-
3 Carrying out the task, prompting themselves aloud
-
4 Carrying out the task, prompting themselves by whispering
-
5 Carrying out the task silently using covert self-instruction/self-talk
While these approaches are good practice and a helpful adjunct to behavioural approaches at home and school when combined with medication, results have been variable and disappointing (Reference AbikoffAbikoff, 1991). The training has frequently been too short, unrelated to clinical need and with insufficient focus on generalisation and maintenance for hard-to-train children with ADHD.
Addressing more than the child
A number of related issues need to be addressed in the therapeutic formulation when working with children and adolescents.
The family
The therapist needs to engage both parent and child. The younger the child, the more the parents will need to be included in the therapy and to be instructed in the cognitive–behavioural model and its application to their child's problem.
The parents may also need specific instruction in management techniques, for example avoiding reassurance for a child with OCD and using positive reinforcement for compliance with a child with a conduct disorder.
The therapist must be aware of the family's structure and its belief system, the systemic implications of any intervention and reality factors such as abuse or a specific learning disability.
Complementary behavioural input for parents is particularly important for oppositional defiant disorder and conduct disorder, for which parent management training has been shown to be effective (Reference PattersonPatterson, 1982; Reference Webster-StrattonWebster-Stratton, 1982, Reference Webster-StrattonWebster-Stratton, 1984). Parent training also enhances problem-solving skills training for children, giving a consequent decrease in aggressive behaviour problems at home and at school and an improved overall adjustment (Reference Kazdin, Siegel and BassKazdin et al, 1992). It is also useful for parents whose own anxiety provides powerful modelling for their children's anxiety disorders to have CBT in their own right (Reference Barratt, Dadds and RapeeBarratt et al, 1996, Reference Barratt, Lowry-Webster and HolmesBarratt et al, 1998).
The school
Information and adjunctive behaviour programmes may be necessary to reinforce therapeutic achievements for the child. For example, information about exposure helps a school to support a returning school-avoidant child and reinforcing developing social skills is helpful for a child with a conduct disorder.
Engaging the child or adolescent
Attractive published materials such as Kendall's workbooks (1989, 1994a) may need to be supplemented by individual tailor-made charts or materials prepared by the therapist.
The therapist has a role as reinforcer to increase the child's motivation, and should use appropriate supportive phrases: “Well done. Even though it was difficult, I can see how hard you've tried”.
Overcoming developmental limitations
While a bright well-motivated adolescent's grasp of unmodified adult-type CBT principles or programmes can be very rapid and rewarding for both adolescent and therapist, younger children may find the adult programme and materials, such as thought diaries (Fig. 2), beyond them unless these are suitably modified.
Before therapy proper is begun, many children and young adolescents will benefit from a period of emotional education, during which they learn to distinguish different emotional states and link emotions with thoughts and events.
However, developmental limitations remain for children in working with higher-order abstractions such as reflecting on hypotheses and evaluating evidence for and against a belief, which may not develop for many until middle adolescence.
Issues and trends
The high face validity, clarity and simplicity of CBT theory may give the impression of an easy therapy, which can be carried out by the clinically inexperienced. This is certainly not the case. Cognitive–behavioural therapists need the ability to engage their patients and create a collaborative working alliance, to enable them to implement the therapy effectively.
Cognitive–behavioural treatments are generally specific for particular conditions. It may therefore be appropriate to establish dedicated clinics for certain conditions, for example depression, OCD and ADHD, in order to develop therapists' expertise. As the treatment is condition-specific, there should be increasing use of good-quality, systematic psychiatric diagnostic assessments rather than generic family-therapy assessments. While treatments were more or less ineffective, this was less important, but with the development of effective specific interventions, failure to use the appropriate evidence-based treatment may be considered negligent.
With a broad-based CBT approach, a psychoeducational element of giving information by discussion supplemented with fact-sheets is important. This is likely to increase compliance and is appreciated by the child, family, school and often the referring general practitioner.
Issues of transportability (bridging the gap between the research intervention and the clinic), adherence to ‘manualised treatments’ (treatments based on manuals) and the integrity of the therapy have become more prominent recently (Reference Weisz, Weiss and HanWeisz et al, 1995). However, there are very real difficulties for busy psychiatrists not only in finding time to obtain teaching in and supervision of CBT, but also even in finding the manuals.
Despite these difficulties, many consultants are now making great efforts to train themselves and their departments. This educational input might also prove to be an excellent means of team-building.
Cognitive–behavioural therapies have been cited as generally more effective for children than non-cognitive–behavioural individual and family therapies (Reference Roth and FonagyRoth & Fonagy, 1996). However, they still require much refinement, which is being undertaken. It is likely that consultants will need to consider how best to introduce these developments into their teams and what mix of staff skills is most likely to sustain them. We might do well to heed Stern's (1993) warning:
“If psychiatrists are not trained in BCPT [behavioural-cognitive psychotherapy] it leaves them therapeutically impotent, and therefore less able to lead a multidisciplinary team” (p. 3).
Multiple choice questions
-
1. Cognitive–behavioural therapy for children:
-
a combines behavioural techniques with a cognitive focus on meaning
-
b suggests that behavioural interventions cannot change beliefs
-
c cannot be combined with parent training
-
d can be carried out by a passive therapist
-
e includes social-skills training.
-
-
2. In depression:
-
a the cognitive content is of threat or danger
-
b the Beck model does not apply in children
-
c activity scheduling is unsuitable
-
d using thought diaries will help access negative automatic thoughts
-
e some children need additional work on social problem-solving.
-
-
3. Anxiety disorders:
-
a are characterised by thoughts of threat or danger
-
b are not maintained by behavioural avoidance
-
c can respond to correction of cognitive distortions
-
d relapse quickly after CBT
-
e treated by CBT are unaffected by the addition of interventions targeting parents.
-
-
4. Cognitive distortions are prominent in:
-
a obsessive–compulsive disorder
-
b eating disorders
-
c childhood autism
-
d attention-deficit hyperactivity disorder
-
e depression.
-
-
5. When using CBT for children and adolescents:
-
a emotional education may be necessary
-
b choosing a specific intervention appropriate for the diagnosis is important
-
c adolescents are generally more suitable than young children
-
d giving information about the treatment is unnecessary
-
e there is a good evidence-base for the intervention.
-
MCQ answers
| 1 | 2 | 3 | 4 | 5 | |||||
|---|---|---|---|---|---|---|---|---|---|
| a | T | a | F | a | T | a | T | a | T |
| b | F | b | F | b | F | b | T | b | T |
| c | F | c | F | c | T | c | F | c | F |
| d | F | d | T | d | F | d | F | d | F |
| e | T | e | T | e | F | e | T | e | T |
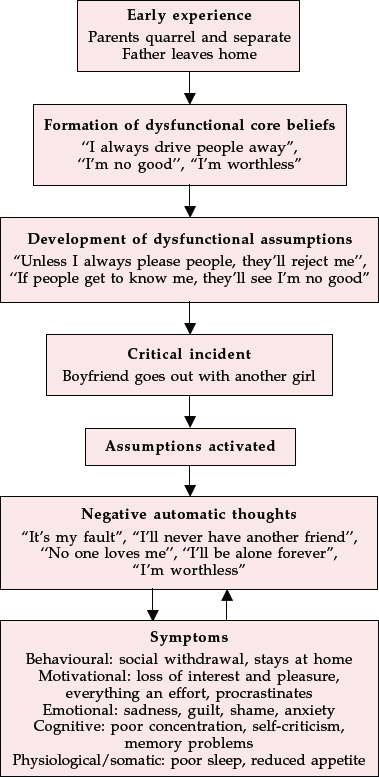
Fig. 1 The cognitive model of depression
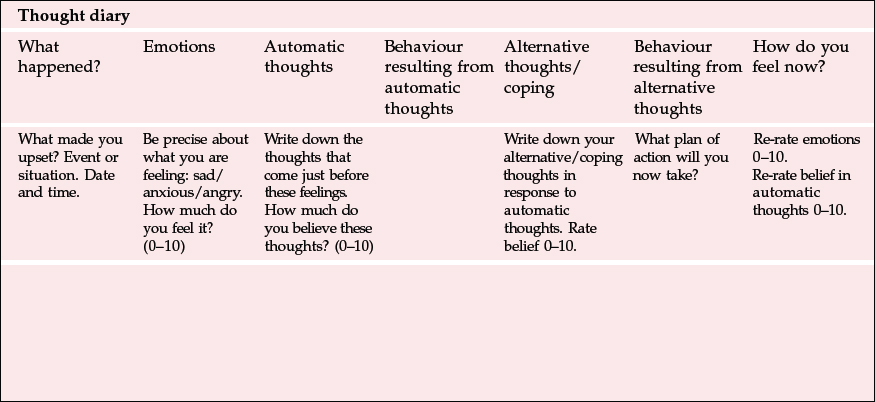
Fig. 2 Thought diary
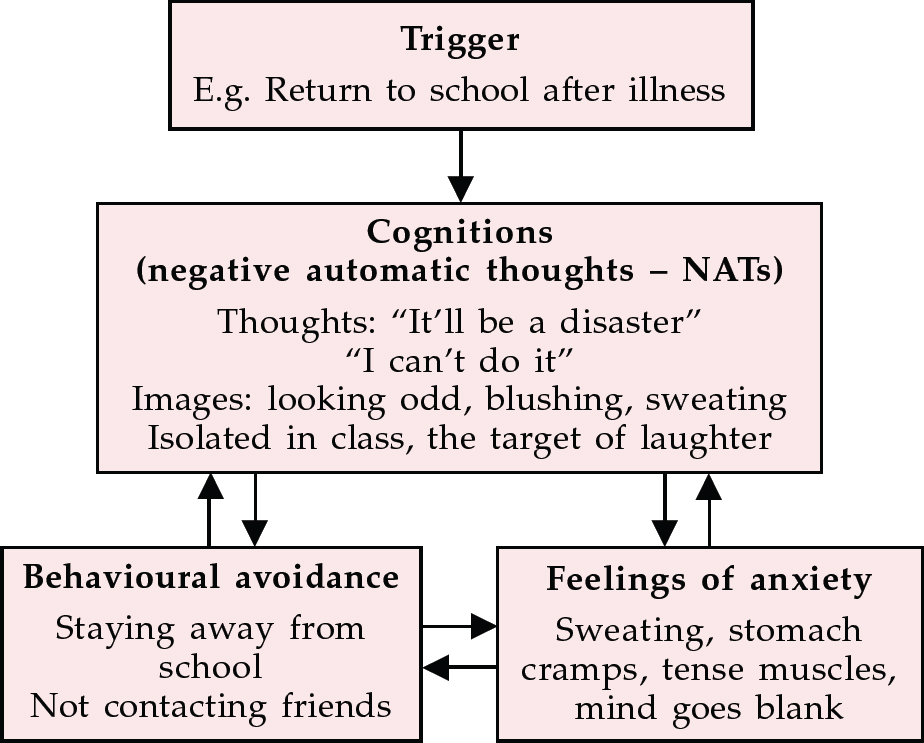
Fig. 3 Cognitive model for anxiety
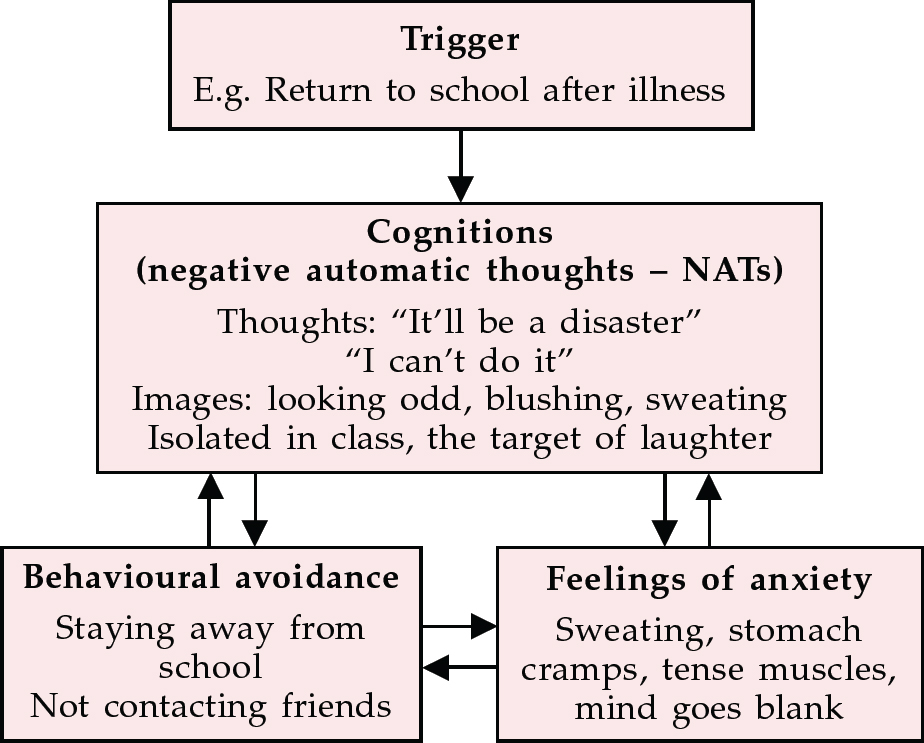
Fig. 4 Cognitive model of obsessive–compulsive disorder







eLetters
No eLetters have been published for this article.