Significant outcomes
Patients with major depressive disorder exhibited attenuated adhesive function of circulating endothelial progenitors (cEPCs) compared to healthy controls, independent of inflammatory marker levels.
The reduced adhesive function of cEPCs was associated with worse working memory and executive function, more severe psychosomatic symptoms, poorer mental and physical quality of life, and greater subjective disability in daily living.
Limitations
The findings were unable to determine the causality or temporal relationship between major depressive disorder (MDD) and circulating endothelial progenitors (cEPC) functions due to the cross-sectional design of the study.
The study did not evaluate the possible associations between other cEPC functional parameters such as migration, tube formation and the ability to form colonies, and MDD diagnosis and symptom severity.
These results only apply to adult patients with MDD and not to adolescents, older patients, or those with major depressive episodes of bipolar disorder or depressive disorders due to other medical conditions.
Introduction
Major depressive disorder (MDD) is a debilitating psychiatric disorder; its diagnosis is made based on the presence of one or two core symptoms (depressed mood and diminished interest or pleasure) and at least three or four of seven additional symptoms (including significant weight change or appetite disturbance, sleep disturbance, fatigue or loss of energy, diminished ability to think or concentrate, and recurrent thoughts of death or suicidal ideation) (American Psychiatric Association, 2013). An accumulating body of evidence has indicated that patients with MDD are susceptible to cardiovascular diseases (CVDs), atherosclerosis, hypertension, and stroke (Dhar and Barton, Reference Dhar and Barton2016). Moreover, patients with CVDs are at risks of MDD (Lippi et al., Reference Lippi, Montagnana, Favaloro and Franchini2009; Chaddha et al., Reference Chaddha, Robinson, Kline-Rogers, Alexandris-Souphis and Rubenfire2016) and of clinically significant depression symptoms (Chaddha et al., Reference Chaddha, Robinson, Kline-Rogers, Alexandris-Souphis and Rubenfire2016).
One of the proposed pathophysiological mechanisms underlying the bidirectional association of CVDs and MDD is endothelial dysfunction (ED) (Kahl et al., Reference Kahl, Stapel and Frieling2019; Fadini et al., Reference Fadini, Mehta, Dhindsa, Bonora, Sreejit, Nagareddy and Quyyumi2020). ED involves the impairment of endothelium-dependent vasodilation and the activation of proinflammatory, proliferative, and procoagulant activities following injury to the vascular endothelium (Little et al., Reference Little, Askew, Xu and Kamato2021). Endothelial injury and ED lead to tissue ischaemia and stimulate the differentiation of haematopoietic stem cells in the bone marrow into circulating endothelial progenitor cells (cEPCs) (Chopra et al., Reference Chopra, Hung, Kwong, Zhang and Pow2018). The differentiated cEPCs in the peripheral blood migrate to vascular damage sites, integrate into the endothelial monolayer, promote vascular repair and angiogenesis through paracrine signalling to neighbouring cells, and transdifferentiate into mature endothelial cells. cEPCs have been proposed as direct indicators of endothelial function. Furthermore, quantitative and functional changes in cEPCs are associated with various cardiovascular risk factors, CVDs, and cardiometabolic diseases (Hill et al., Reference Hill, Zalos, Halcox, Schenke, Waclawiw, Quyyumi and Finkel2003; Chopra et al., Reference Chopra, Hung, Kwong, Zhang and Pow2018).
Given the reciprocal and bidirectional relationships between MDD and CVDs and the involvement of cEPCs in ED, several studies have investigated the role of the quantity of cEPCs in the development of depression symptoms or in MDD diagnosis in patients with and without CVDs and with and without psychosocial stressors (Yang et al., Reference Yang, Ruan, Ye, Cui, Mu, Lou, Ji, Li, Sun and Chen2011; Liou et al., Reference Liou, Chen, Hsu, Huang, Huang and Bai2021; Yang et al., Reference Yang, Sun, Duan, Lv, Liang, Zhang, Yu, Tang and Lu2021). However, in addition to the number of cEPCs, their functional properties appear to play key roles in cEPCs’ regenerative and repairing activities and in numerous pathological conditions; cEPC function can be characterised by the cells’ proliferation, migration, adhesion, and apoptosis (Sen et al., Reference Sen, Mcdonald, Coates and Bonder2011; Chopra et al., Reference Chopra, Hung, Kwong, Zhang and Pow2018). cEPC adhesion enables the cells to adhere to endothelial injury sites and is a fundamental step in cEPC functioning for both angiogenic processes and the maintenance of endothelial homeostasis (Fadini et al., Reference Fadini, Sartore, Albiero, Baesso, Murphy, Menegolo, Grego, Vigili De Kreutzenberg, Tiengo, Agostini and Avogaro2006). Numerous studies have demonstrated that the pathophysiology of MDD involves inflammation and increased oxidative stress, which are detrimental to cEPC survival and lead to cEPC apoptosis (Dowlati et al., Reference Dowlati, Herrmann, Swardfager, Liu, Sham, Reim and Lanctot2010; Black et al., Reference Black, Bot, Scheffer, Cuijpers and Penninx2015; Chopra et al., Reference Chopra, Hung, Kwong, Zhang and Pow2018). Although evidence supports that cEPC numbers are altered in MDD and that cEPCs are associated with symptom severity in MDD, no study has reported on cEPC function in patients with MDD (Yang et al., Reference Yang, Sun, Duan, Lv, Liang, Zhang, Yu, Tang and Lu2021). Moreover, the correlation of the level of cEPC adhesion with the numbers of mature and immature cEPCs, which are, respectively, positive for surface markers CD34/kinase insert domain receptor (KDR) and CD34/CD133/KDR, has not been demonstrated (George et al., Reference George, Shmilovich, Deutsch, Miller, Keren and Roth2006). Therefore, in the present study, we investigated whether the adhesion properties and apoptosis of cEPCs are associated with MDD and are correlated with the level of cognitive deficit and clinical presentations of MDD, including depression symptom and anxiety severity, somatic symptoms, subjective disability in key functional domains, and quality of life.
Materials and methods
Participants
Sixty-eight patients with MDD and 56 healthy controls (HCs) were recruited. The participants aged 20–65 years were recruited between September 2010 and December 2020. The patients with MDD were recruited from the psychiatric outpatient department of Taipei Veterans General Hospital (VGHTPE) (Taipei, Taiwan), and HCs were recruited via advertisement. The patients met the criteria for MDD in Diagnostic and Statistical Manual of Mental Disorders, Forth Edition-Text Revision, or Fifth Edition (DSM-IV-TR or DSM-V). A psychiatrist conducted the Mini-International Neuropsychiatric interview with the participants to make the diagnosis of MDD. The patients had any condition listed in the exclusion criteria were excluded. Exclusion criteria included major physical illnesses (i.e. epilepsy, cerebrovascular disorders, autoimmune/immune diseases), active infectious diseases or unstable physical illnesses, current pregnant of breastfeeding, and a lifetime history of other psychiatric illness (i.e. schizophrenia or other psychotic disorder, alcohol or substance use disorders, intellectual disability, and organic mental disorders). The HCs were also interviewed by the psychiatrist and were free of major psychiatric illness and other disorders listed in the exclusion criteria. This study was approved by the Institutional Review Board of VGHTPE and was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all patients prior to their inclusion in the study.
Clinical assessments
The participants’ depression and anxiety symptom levels were assessed using the Hamilton Depression Rating Scale (HAMD), Montgomery–Åsberg Depression Rating Scale (MADRS), and Hamilton Anxiety Rating Scale (HAMA). The HAMD and MADRS are two clinician-assessment scales for the severity of depression symptoms. However, not all core symptoms of major depressive episodes can be assessed through the HAMD or MADRS. The HAMD does not assess oversleeping, overeating, and concentration levels, and the MADRS does not assess interest levels, guilt, and psychomotor activity (Carmody et al., Reference Carmody, Rush, Bernstein, Warden, Brannan, Burnham, Woo and Trivedi2006). Therefore, both rating systems were used in this study to fully assess depression symptom severity in patients with MDD.
The participants completed additional three self-administered questionnaires: the Depressive and Somatic Symptoms Scale (DSSS), 12-Item Short Form Health Survey (SF-12), Perceived Deficits Questionnaire-Depression (PDQ-D) (Lam et al., Reference Lam, Lamy, Danchenko, Yarlas, White, Rive and Saragoussi2018), and Sheehan Disability Scale (SDS). The DSSS includes somatic elements, simultaneously assesses somatic and depression symptoms and overcomes the deficiencies of other depression scales (Hung et al., Reference Hung, Liu, Juang and Wang2006). Total DSSS scores may indicate the severity of concurrent psychosomatic symptoms (Hung et al., Reference Hung, Liu, Juang and Wang2006). The SF-12, a 12-item questionnaire used to assess generic health-related quality of life from a patient perspective, comprises a physical component summary (PCS) and a mental component summary (MCS) (Ware et al., Reference Ware, Kosinski and Keller1996). The PDQ-D is used to evaluate the effects of cognitive dysfunction in daily life according to the participants’ experience of having depression symptoms (Lam et al., Reference Lam, Lamy, Danchenko, Yarlas, White, Rive and Saragoussi2018). The SDS is a participant-rated tool evaluating functional disability in work, school, social, and family life with only three self-rated items (Sheehan and Sheehan, Reference Sheehan and Sheehan2008).
Assessment of working memory and executive function
The study participants’ working memory and executive function were evaluated using a computerised 2-back task and Wisconsin Card Sorting Test (WCST). Regarding working memory, all participants were instructed to respond as quickly as possible when a number appeared the second time on-screen after a different number had appeared. For example, if 25, 31, and 25 were consecutively displayed on the screen, the participants would respond when the number of “25” appeared the second time. After the participants completed the preliminary test with all correct answers, formal tests were administered to record their number of commission errors, omission errors, and reaction time variability as performance parameters. With regard to WCST, each participant was required to match response cards to four stimulus cards by pressing one of the 1–4 number keys on the computer keyboard. The stimulus cards consist of three dimensions: colour, form, or number. During the test, the participants were neither informed of the correct sorting principle nor told of when the principle would shift, but were provided a ‘Right’/‘Wrong’ feedback on the screen after each trial. The testing continued until all 128 were sorted (Fleck et al., Reference Fleck, Shear, Madore and Strakowski2008; Nyhus and Barcelo, Reference Nyhus and Barcelo2009; Cotrena et al., Reference Cotrena, Branco, Shansis and Fonseca2016).
Measures for biochemical parameters
Blood samples were drawn after 12-h overnight fasting by the participants. Plasma biochemical parameters and fasting glucose (FBS), triglyceride (TG), cholesterol (CHOL), high-density lipoprotein cholesterol (HDLc), uric acid (UA), creatinine (CREAT), alanine aminotransferase (ALT), and aspartate aminotransferase (AST) levels were determined using standard laboratory procedures.
Measures for the levels of inflammatory markers
Proinflammatory cytokines in the blood samples of all participants, including soluble interleukin-6 receptor (sIL-6R), C-reactive protein (CRP), and tumor necrosis factor-α receptor-1 (TNFR1), were measured using enzyme-linked immunosorbent assay (ELISA) kits from R&D systems. The fasting serum samples were collected in serum separator tubes and stored at −80°C until testing. The ELISA tests were carried out according to the instructions provided by the vendor, and the final absorbance of each sample at 450 nm was measured and analysed using an ELISA plate reader with Bio-Tek Power Wave Xs and Bio-Tek’s KC junior software (Winooski, VT, USA). To ensure accurate results, a linear regression R-square value of at least 0.95 was used as a reliable standard curve.
cEPC isolation and culture
Peripheral blood samples (20 mL) of the participants were obtained in heparin-coated tubes to study cEPCs in culture. The circulating mononuclear cells (MNCs) were isolated by density gradient centrifugation with Histopague-1077 (Sigma), and the serum was preserved (Chen et al., Reference Chen, Lin, Lin, Wu, Tsao, Huang, Liu, Chen and Chen2007). Briefly, MNCs (5 × 106) were plated in 2-mL of endothelial growth medium (EGM-2 MV Cambrex, East Rutherford, NJ, USA) with 15% individual serum on fibronectin-coated 6-well plates. After 4 days of culturing, the medium was changed, and nonadherent cells were removed; attached cEPCs appeared elongated with spindle shapes (Chen et al., Reference Chen, Lin, Lin, Wu, Tsao, Huang, Liu, Chen and Chen2007).
cEPC characterisation
cEPCs were characterised as adherent cells that were double positive for acetylated LDL uptake and lectin binding by direct fluorescent staining, as previously described (Chen et al., Reference Chen, Lin, Lin, Wu, Tsao, Huang, Liu, Chen and Chen2007). The adherent cells were first incubated with 2.4 mg/mL 1,1′-dioctadecyl-3,3,3′,3′-tetramethylindocarbocyanine perchlorate-acetylated LDL (DiI-acLDL; Molecular Probes, Eugene, OR, USA) for 1 h, then fixed in 2% paraformaldehyde, and counterstained with 10 mg/mL fluorescein isothiocyanate-labeled lectin from Ulex europaeus (UEA-1; Sigma) (Chen et al., Reference Chen, Lin, Lin, Wu, Tsao, Huang, Liu, Chen and Chen2007).
cEPC adhesion assay
cEPCs (day 7) were washed with phosphate-buffered saline (PBS) and were gently detached with 0.5 mmol/L ethylenediamine tetraacetic acid in PBS. The cEPC adhesion level to the injury site was evaluated by plating 1 × 104 cEPCs onto a fibronectin-coated 6-well plate. After 30-min incubation and adhesion at 37°C, gentle washing with PBS was performed, and adherent cells in six random, high-power (×100) microscopic fields of each well were counted by two independent and blinded investigators. The test was conducted as previously described (Sung et al., Reference Sung, Wu, Chen, Chen, Huang, Lin, Shih and Chen2013; Liou et al., Reference Liou, Chen, Hsu, Huang, Huang and Bai2023).
cEPC apoptosis assay
Terminal deoxynucleotidyl transferase–mediated deoxyuridine triphosphate nick-end labelling (TUNEL) assay was performed using the In Situ Cell Death Detection kit (Roche Diagnostics, Basel, Switzerland) according to the manufacturer’s instructions. Apoptosis was evaluated as the percentage of positive cells per 1000 DAPI-stained nuclei, and cEPCs were examined under a fluorescence microscope (Nikon Eclipse 50i) at a magnification of ×100. The test was conducted as previously described (Wu et al., Reference Wu, Huang, Lai, Leu, Chen and Lin2014; Liou et al., Reference Liou, Chen, Hsu, Huang, Huang and Bai2023).
Power and statistical analyses
An a priori power analysis was conducted using G*Power version 3.1.9.4 (Faul et al., Reference Faul, Erdfelder, Buchner and Lang2009) to determine the minimum sample size needed to test the study’s hypothesis. The results showed that with a medium effect size of 0.5, a total of 134 participants were required (with 67 in each group) to achieve 80% power at a significance level of α = 0.05 for the Mann–Whitney Test. The sample sizes of 68 in the MDD group and 56 in the HC group were sufficient for testing the difference of cEPC functional indices with medium effect size between MDD and HC groups.
The normality of continuous variables was evaluated using the Shapiro–Wilk test. Because most of the continuous variables deviated from normal distribution assumption, they are presented as medians and interquartile ranges (IQRs). Their differences were analysed using the Mann–Whitney U test. Rank-Biserial correlation (r RB) values are reported as effect size measures for the Mann–Whitney U tests.
The differences in the distributions of categorical variables between the groups were determined using the chi-square test (and Fisher’s exact test, if necessary). The strength and direction of the correlations between cEPC functional indices and clinical symptoms were determined through Kandell Tau-b partial correlation analysis. Linear regressions were performed to adjust for potential confounding effects on continuous variables. In univariate analysis, the threshold of statistical significance was set at corrected p (p corr ) < 0.05 after adjustment for multiple comparisons using the Benjamini–Hochberg procedure (https://tools.carbocation.com/FDR). In multivariate stepwise linear analysis, the threshold of statistical significance was set at p < 0.05. The extent to which cEPC adhesion affects executive function through working memory was examined with mediation analysis. Statistical analyses were performed using SPSS (version 21; SPSS, Chicago, IL, USA) and JASP 0.16.1 (https://jasp-stats.org/download/).
Results
Basic and clinical characteristics
The characteristics, clinical and cognitive profiles of the participants are summarised in Table 1, and the data of blood pressures, biochemical profiles, and inflammatory markers in supplementary Table 1. The MDD patients were treated with the following antidepressants: Bupropion (n = 7), Duloxetine (n = 2), Escitalopram (n = 9), Fluoxetine (n = 1), Mirtazapine (n = 3), Paroxetine (n = 2), Sertraline (n = 10), Venlafaxine (n = 2), and Vortioxetine (n = 5). There were two patients treated with two antidepressants simultaneously. Some of the patients had diagnosed with hypertension (n = 3), heart disease (n = 2), diabetes mellitus (DM; n = 4), and hyperlipidaemia (n = 3). The MDD group had more current smokers than the HC group. The MDD patients received fewer years of education than the HCs. Compared with the HCs, the MDD patients exhibited greater DSSS, PDQ-D, and SDS scores, but lower MCS and PCS scores. The patients with MDD displayed more omission errors in 2-back task, and more percent perseverative response and percent perseverative errors but less categories completed in WCST compared to the HCs (Table 1, all p < 0.01).
Table 1. Demographic characteristics and clinical and cognitive profiles of patients with major depressive disorder and of healthy controls. Continuous variables are presented as medians and interquartile ranges (IQRs)
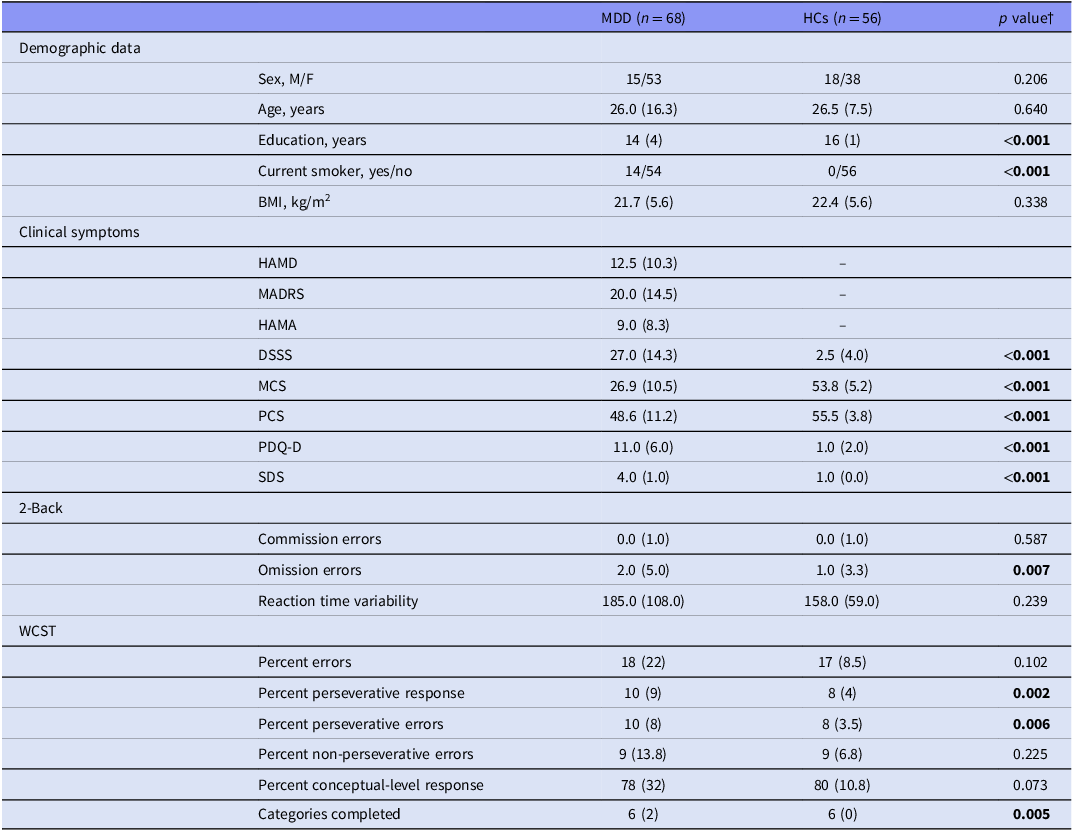
Abbreviations: BMI, body mass index; DSSS, Depressive and Somatic Symptom Scale; F, female; HAMA, Hamilton Anxiety Rating Scale; HAMD, 17-item Hamilton Depression Rating Scale; HCs, healthy controls; M, male; MADRS, Montgomery–Åsberg Depression Rating Scale; MCS, Mental Component Summary of the 12-Item Short Form Health Survey; MDD, major depressive disorder; PCS, Physical Component Summary of the 12-Item Short Form Health Survey; PDQ-D, Perceived Deficits Questionnaire-Depression; SDS, Sheehan Disability Scale; WCST, Wisconsin Card Sorting Test.
† Chi-square, Fisher exact, or Mann–Whitney U test. Bold indicates a p-value less than 0.05.
cEPC adhesive and apoptotic functions in MDD and HC groups
The patients with MDD had significantly lower numbers of adherent cEPCs compared with the HCs (Fig 1A. MDD vs. HC = 105.4 [92.8] vs. 166.0 [102.2] cells/high-power field, Mann–Whitney U test, p = 0.000053, p corr = 0.0012, rRB = −0.42 [95% CI: −0.58 to −0.24]). The discrimination ability of cEPC adhesive levels for the patients with MDD and the HCs was acceptable (Fig. 1B, area under the curve [AUC] = 0.71, 95% CI = 0.62 to 0.80, p < 0.001).
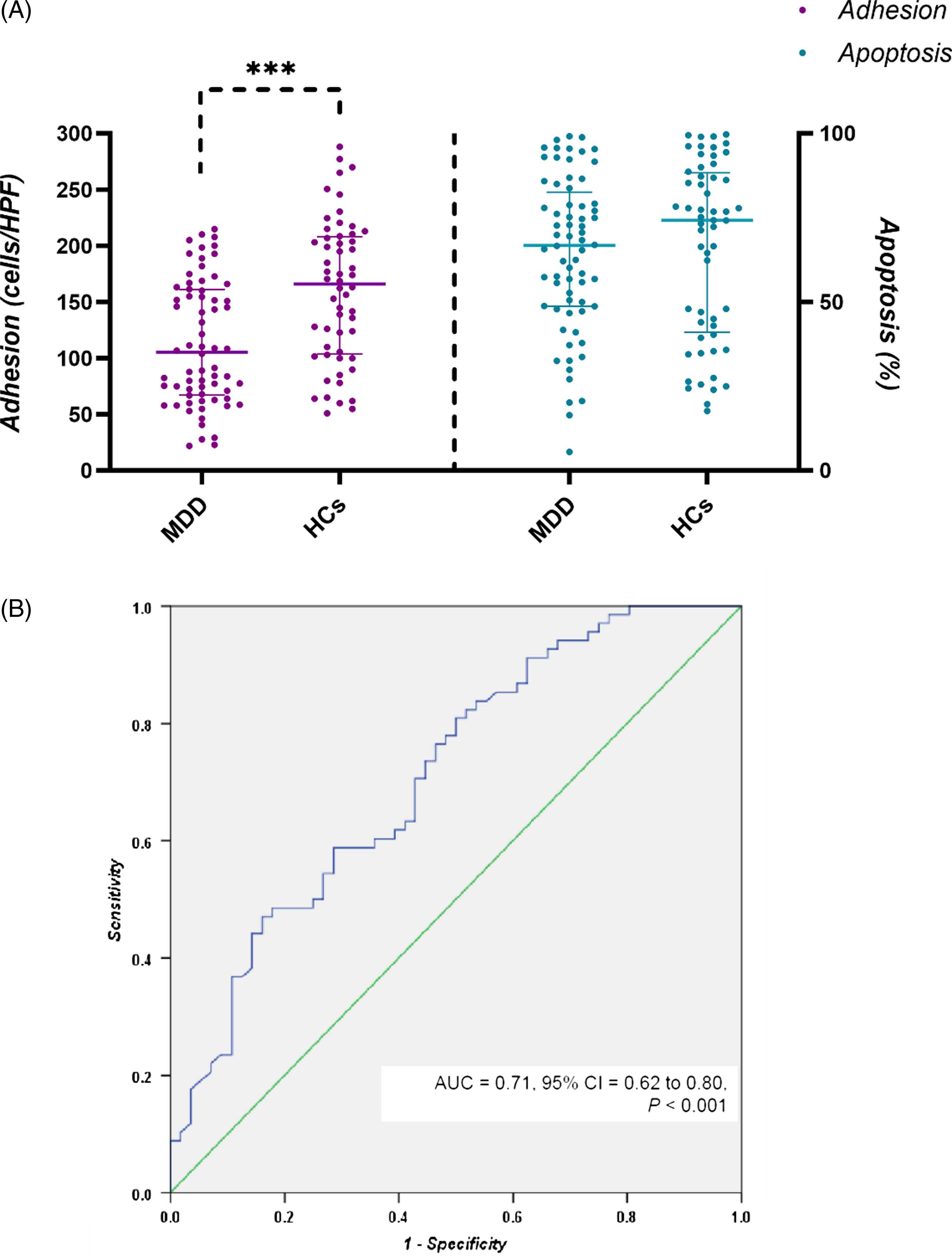
Figure 1. Adhesive and apoptotic properties of cEPCs and MDD. (A) Levels of adhesion (left) and apoptosis (right) of cEPCs in patients with MDD and in HCs. (B) Receiver operating characteristic curve for cEPC adhesive function to discriminate the MDD from HC group. *** p < 0.001. Abbreviations: AUC, area under the receiver operating characteristic curve; cEPCs, circulating endothelial progenitor cells; HCs, healthy controls; HPF, high-power field; MDD, major depressive disorder.
There was no significant difference in the number of adherent cEPC between the smoker and the non-smoker groups (smokers vs. non-smokers = 126.0 [113.4] vs. 137.5 [108.1], Mann–Whitney U test, p = 0.554). When the comparison was restricted to non-smokers, the finding of lower numbers of adherent cEPCs in the MDD group remained (Mann–Whitney U test, p = 0.000052, r RB = −0.45 [95% CI: −0.60 to −0.26]). To control for the influence of inflammatory markers and other covariates, three linear regression models were applied. Model 1 adjusted for the levels of inflammatory markers (sIL-6R, CRP and TNFR1). Model 2 additionally adjusted for age, sex, smoker, and BMI in addition to inflammatory markers. Model 3 additionally adjusted for systolic and diastolic pressures, FBS, TG, CHOL, and HDLc levels in addition to inflammatory markers and clinical covariates of model 2. The results of the three regression models showed the association of reduced cEPC adhesive levels with MDD remained (model 1: β (95% CI) = 47.7 (25.4 to 70.0); model 2: β (95% CI) = 54.8 (30.9 to 78.7); model 3: β (95% CI) = 58.4 (34.3 to 82.5), all p < 0.001).
No significant difference was identified in the percentage of cEPC apoptosis in patients with MDD (66.8% [31.5]) and HCs (74.2 % [45.3]; Fig. 1A. Mann–Whitney U test, p = 0.532). The percentage of cEPC apoptosis in non-smokers was not different from that in smokers (smokers vs. non-smokers = 67.1 [29.2] vs. 71.8 [41.9], Mann–Whitney U test, p = 0.754).
Associations among cEPC functional indices, working memory, and executive function
The results of Kendell’s partial correlation analyses for cEPC functional indices and performance on 2-back task and WCST are presented in Table 2. The correlations were adjusted for age, sex, years of education, smokers, and the levels of sIL-6R, CRP, and TNFR1. cEPC adhesive levels were in significantly negative correlation with the commission errors (p = 0.0017, p corr = 0.031) and omission errors (p = 0.0039, p corr = 0.035) of 2-back task and also in negative correlation with percent perseverative response (p = 0.005, p corr = 0.023) and percent perseverative errors (p = 0.004, p corr = 0.024) of WCST.
Table 2. Correlation analyses for the performance parameters in 2-back task and WCST and cEPC functional indices†
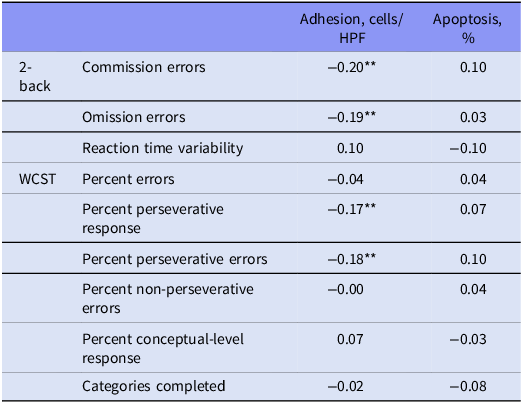
Abbreviations: CRP, C-reactive protein; cEPC, circulating endothelial progenitor cells; HPF, high-power field; sIL-6R, soluble interleukin-6 receptor; TNFR1, tumour necrosis factor-α receptor-1; WCST, Wisconsin Card Sorting Test; sIL-6R, soluble interleukin-6 receptor.
†with adjustment for age, sex, years of education, smokers, and the levels of sIL-6R, CRP, and TNFR1; data are Kendall Tau-b correlation coefficients. **p < 0.01.
Mediation analyses for the interactions between cEPC adhesion, working memory, and executive function
The results of mediation analysis are shown in Fig. 2. A significantly indirect effect of omission errors (Fig. 2A, β = −0.002, 95% CI = −0.003 to −0.000, p = 0.044) on the negative correlation of cEPC adhesion and percent perseverative response was found. The direct effect of cEPC adhesion or indirect effect of commission errors on the level of percent perseverative response was not significant. Likewise, the indirect effect of omission errors on the negative correlation of percent perseverative errors and cEPC adhesion was statistically significant (Fig. 2B, β = −0.002, 95% CI = −0.004 to -0.000, p = 0.013). There was no indirect effect of commission errors nor direct of cEPC adhesion on the association with percent perseverative errors.
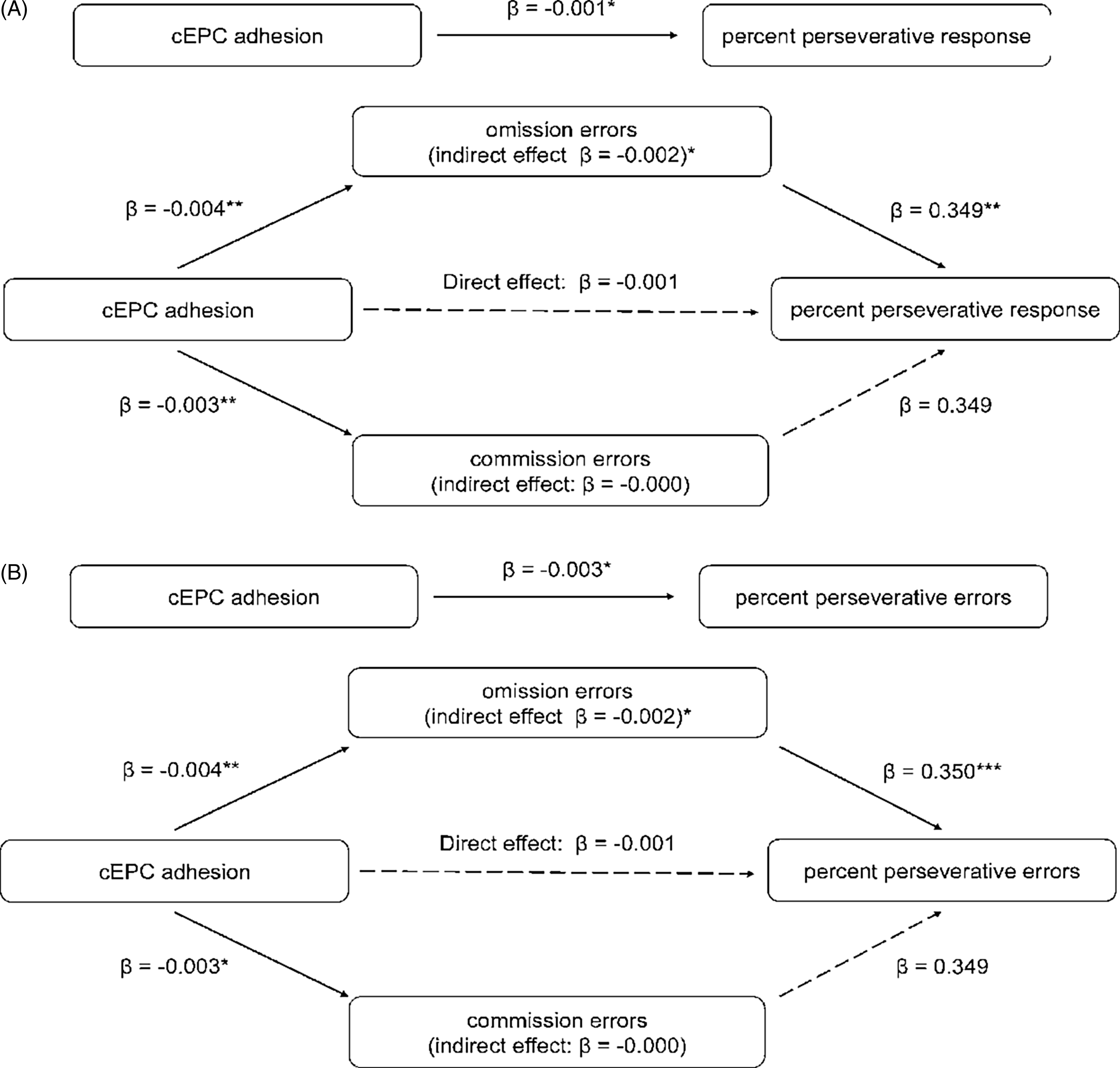
Figure 2. Mediation analyses for the effect of omission and commission errors on the correlation of cEPC adhesion and percent perseverative response (A) and percent perseverative response (B) in WCST. The number indicates standardised regression coefficients. * denotes statistical significance (* p < 0.05, ** p < 0.01, *** p < 0.001, respectively, two-tailed) or the 95% CI not including zero. Abbreviations: cEPCs, circulating endothelial progenitor cells; WCST: Wisconsin Card Sorting Test.
Associations between cEPC functional indices and clinical measurements related to MDD
The results of correlation analyses of cEPC adhesion properties and apoptosis and clinical presentations related to MDD are presented in Table 3. Levels of cEPC adhesion were negatively correlated with DSSS (p = 0.019) and SDS (p = 0.00012) scores but positively correlated with MCS (p = 0.027) and PCS (p = 0.038) scores. The inverse correlation of cEPC adhesion properties with SDS scores remained significant after adjustment for multiple testing (p corr = 0.002).
Table 3. Correlation analysis of adhesive and apoptosis properties of cEPCs and clinical measurements related to major depressive disorder†
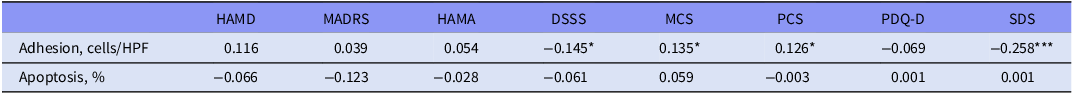
Abbreviations: cEPCs, circulation endothelial progenitor cells; DSSS, Depressive and Somatic Symptom Scale; HAMA, Hamilton Anxiety Rating Scale; HAMD, 17-item Hamilton Depression Rating Scale; HPF, high-power field; MADRS, Montgomery–Åsberg Depression Rating Scale; MCS, Mental Component Summary of the 12-Item Short Form Health Survey; PCS, Physical Component Summary of the 12-Item Short Form Health Survey; PDQ-D, Perceived Deficits Questionnaire-Depression; SDS, Sheehan Disability Scale.
† with adjustment for age, sex, and current smoker status; data are Kendall Tau-b correlation coefficients and corresponding p-values indicating statistical significance: * < 0.05; *** < 0.001.
Discussion
In this study, we explored the associations between cEPC functions (i.e. adhesion and apoptosis) and MDD and its clinical presentations. Our study has several main findings. First, compared with the HCs, the patients with MDD had significantly lower cEPC adhesive function. Second, the reduced cEPC adhesive function was associated with increased errors of commission and omission in the 2-back task, and with more percent perseverative response and errors in WCST. Third, the reduced cEPC adhesive function was correlated lower MCS and PCS scores but higher DSSS and SDS scores. These results suggest that cEPC adhesion is attenuated in MDD, and that attenuated cEPC adhesive function is associated with worse working memory and executive function, severer psychosomatic symptoms, poorer mental and physical quality of life, and greater subjective disability in daily living.
The underlying mechanism for reduced cEPC adhesion in MDD that was discovered by our study requires elucidation. Several studies have already demonstrated associations between attenuated cEPC adhesion and type 2 diabetes mellitus (Tepper et al., Reference Tepper, Galiano, Capla, Kalka, Gagne, Jacobowitz, Levine and Gurtner2002), obesity (Heida et al., Reference Heida, Muller, Cheng, Leifheit-Nestler, Faustin, Riggert, Hasenfuss, Konstantinides and Schafer2010), hypertension (Huang et al., Reference Huang, Chen, Chen, Wu, Chen and Lin2007), HDLc and low-density lipoprotein cholesterol (LDLc) levels (Gordts et al., Reference Gordts, Van Craeyveld, Muthuramu, Singh, Jacobs and De Geest2012), and smoking (Michaud et al., Reference Michaud, Dussault, Haddad, Groleau and Rivard2006). cEPC adhesion can also be influenced by inflammation. Proinflammatory cytokines, such as TNF-α and IL-6, have been reported to be negatively correlated with and to change the adhesive capacity of cEPCs (Chen et al., Reference Chen, Zhong, Sun, Zhou and Zhao2011; Zeng et al., Reference Zeng, Zhang, Zhu, Liu, Liu, Zhang, Tu and Yang2021). However, we found that the association of attenuated cEPC adhesive function and MDD remained after controlling for the effects of BMI, smoking, blood pressure, biochemical data, and inflammatory markers using regression analyses. The result suggests that the association between reduced cEPCs adhesion and MDD may be independent of these factors and that other factors underlie the association. Despite that, attenuated cEPC adhesion may be considered a cellular marker of cerebral microvascular dysfunction and MDD (van Agtmaal et al., Reference Van Agtmaal, Houben, Pouwer, Stehouwer and Schram2017; Maki et al., Reference Maki, Morancho, Martinez-San Segundo, Hayakawa, Takase, Liang, Gabriel-Salazar, Medina-Gutierrez, Washida, Montaner, Lok, Lo, Arai and Rosell2018; Smith et al., Reference Smith, Blumenthal, Hinderliter, Watkins, Hoffman and Sherwood2018).
We discovered that reduced cEPC adhesion was correlated with increased omission and commission errors in a computerised 2-back task, and with more percent perseverative response and errors in WCST. Commission and omission errors are measures of inhibition control and sustained attention, which are essential to the adequate functioning of working memory measured with 2-back (Pan et al., Reference Pan, Park, Brietzke, Zuckerman, Rong, Mansur, Fus, Subramaniapillai, Lee and Mcintyre2019; Watters et al., Reference Watters, Carpenter, Harris, Korgaonkar and Williams2019). Our results indicate the involvement of cEPC adhesive dysfunction in worse performance on working memory and executive function. Our mediation analyses further showed the relation of cEPC adhesive dysfunction and worse WCST performance was mainly through its correlation with working memory deficit. Impaired attentional control and working memory deficit in acute episodes and remission in MDD have been consistently reported across studies (McIntyre et al., Reference Mcintyre, Cha, Soczynska, Woldeyohannes, Gallaugher, Kudlow, Alsuwaidan and Baskaran2013; Semkovska et al., Reference Semkovska, Quinlivan, O’grady, Johnson, Collins, O’connor, Knittle, Ahern and Gload2019). Evidence has suggested working memory deficit in MDD may be associated with ED. For example, impaired flow-mediated dilation (FMD), a widely utilised biomarker of endothelial function, was associated with poor working memory in a meta-analysis comprising 2791 participants (Naiberg et al., Reference Naiberg, Newton and Goldstein2016) and in patients with MDD (Smith et al., Reference Smith, Blumenthal, Hinderliter, Watkins, Hoffman and Sherwood2018). Fewer hyperemic changes, which can be used to assess microvascular endothelial function (Dubin et al., Reference Dubin, Guajardo, Ayer, Mills, Donovan, Beussink, Scherzer, Ganz and Shah2016), were also found to be correlated with impaired working memory (Nation et al., Reference Nation, Tan, Dutt, Mcintosh, Yew, Ho, Blanken, Jang, Rodgers and Gaubert2018). Because cEPCs are another indicator of endothelial function (Chopra et al., Reference Chopra, Hung, Kwong, Zhang and Pow2018), our findings of the associations of attenuated cEPC adhesion with worse performance on working memory and executive function not only support the involvement of ED in MDD but also suggests that cEPCs play a role in cognitive deficit.
We also revealed that cEPC adhesive levels were in positive correlations with MCS and PCS scores but in negative correlations with DSSS and SDS scores (Table 3), indicating that attenuated cEPC adhesion is associated with severe psychosomatic symptoms, poor mental health-related quality of life, and severe social disability. Our previous study demonstrated an association between higher immature and mature cEPC counts and more unsatisfactory mental health-related quality of life (SF-MCS) and more severe social disability (Liou et al., Reference Liou, Chen, Hsu, Huang, Huang and Bai2021). Notably, Yoshida et al., Reference Yoshida, Ishikawa, Niitsu, Nakazato, Watanabe, Shiraishi, Shiina, Hashimoto, Kanahara, Hasegawa, Enohara, Kimura, Iyo and Hashimoto(2012) reported that levels of metalloproteinase-9, which is essential for cEPC functioning, were inversely correlated with quality of life in patients with MDD. Although the underlying mechanism remains unclear, these findings collectively suggest that altered cEPC functions may benefit psychological well-being and reduce subjective functional impairment in workplace/school, social situations, and family/home responsibilities in patients with MDD.
We found that there were no differences in the percentage of apoptotic cEPCs in the patients with MDD and the HCs. High glucose levels, elevated levels of oxidised LDLc, and chronic exposure to hypercholesterolaemia can promote cEPC apoptosis (Chopra et al., Reference Chopra, Hung, Kwong, Zhang and Pow2018). In our study, the FBS, CHOL, and TG levels of the patients with MDD did not differ from those of the HCs, which may account for no statistical differences in the percentage of apoptotic cEPCs between the patients with MDD and the HCs. Furthermore, our negative finding for an association between cEPC apoptosis and MDD may be due to the small sample size and limited statistical power of the study. The role of cEPC apoptosis in MDD requires further study.
Our study provides valuable insights by investigating the links between several key clinical domains, working memory and executive function in MDD, and cEPC adhesion and apoptosis, while controlling for cardiometabolic and inflammatory effects. However, it also has some limitations. The cross-sectional design of the study does not allow us to establish the temporal relationship or causality between cEPC functions and depression, or the connections between cEPC functions and cognitive deficits, psychological well-being, and perceived disability in MDD. Additionally, the study did not evaluate the possible associations between other cEPC functional parameters such as migration, tube formation and the ability to form colonies, and MDD diagnosis and symptom severity. Furthermore, the results cannot be generalised to adolescent or older MDD patients, or to those with major depressive episodes of bipolar disorder or depressive disorders caused by other general medical conditions. Despite these limitations, our study can be considered exploratory for further research to validate the observations made in this study.
Conclusion
Our study demonstrated that relative to HCs, patients with MDD exhibited reduced cEPC adhesion, which was independent to the levels of inflammatory markers. The reduced cEPC adhesion was also correlated with worse performance on working memory and executive function, greater psychosomatic symptoms, poorer mental and physical quality of life, and severer psychosocial disability. Our findings suggest that cEPCs may play a role in the pathogenesis of MDD and that the adhesive function of cEPCs serve as a potential biomarker for the disorder. Further research is needed to confirm these findings and to investigate the underlying mechanisms of this relationship.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/neu.2023.49.
Acknowledgements
This manuscript was edited by Wallace Academic Editing.
Author contribution
Bai YM and Huang PH conceptualised and supervised the project. Liou YJ performed data analyses and drafted the manuscript. Chen MH, Hsu JW, Huang KL, and Bai YM provided the samples and clinical data for the study. Huang PH designed, performed, and supervised the laboratory experiments. All authors have made substantial contributions to the work and reviewed and revised the manuscript.
Financial support
The study was supported by grants from Taipei Veterans General Hospital (V108C-201, V109C-086, VGHUST109-V1-2-3, V110C-005, V111C-029, V111C-112, VN111-08, V111D62-003-MY3-1, and V111D62-003-MY3-2) and Taiwan Ministry of Science and Technology (MOST 105-2314-B-075-025-MY3, MOST 109-2314-B-010-050-MY3).
Competing interests
All authors have no conflict of interest and no financial support relevant to this article to disclose.
Ethical statement
This study was approved by the Institutional Review Board of Taipei Veterans General Hospital (Taipei, Taiwan) and was conducted in the psychiatric outpatient department of the hospital in accordance with the Declaration of Helsinki. Written informed consent was obtained from all patients prior to their inclusion in the study.








