1 Introduction
This Element examines the workplace conditions that underpin successful improvement of quality and safety in healthcare. It highlights aspects of the workforce and working environment that may thwart or support healthcare improvement in practice, while recognising that good workplace conditions can also be outcomes of healthcare improvement. We examine the role of three key workplace conditions that are prerequisites for the work of improving quality and safety in healthcare: staffing for quality; psychological safety, teamwork and speaking up; and staff health and well-being at work. We summarise the evidence and show how each contributes to organisational capacity to deliver quality and safety and enable improvement, and explain how success can be assessed.
There may be little dispute about some of the preconditions (funding, staffing, training) for improving quality and safety. But many of the issues we present in this Element operate at multiple levels and vary within and between organisations and workplace units, since staff experiences are shaped by their immediate teams as well as the whole organisational context and culture. Accordingly, much of our analysis is based on the principle that, fundamentally, healthcare work is interactional. People’s actions, interactions, and relationships with each other are critical to enabling an organisation to adopt, implement, and sustain improvements.
2 Staffing for Quality
Staffing (including numbers and skills) can be seen as a structural prerequisite – in Donabedian’s sense of structureReference Donabedian1 – both for providing high-quality, safe care and for improving care. A large body of evidence suggests that having the right numbers of staff and skills affects patient care quality and patient outcomes, as well as staff well-being and engagement, staff absence sickness rates, retention, and burnout.Reference Kane, Shamliyan, Mueller, Duval and Wilt2–Reference Dall’Ora, Ball, Reinius and Griffiths6 The links between staff well-being at work and patient experience are also well establishedReference Maben, Adams, Peccei, Murrells and Robert7, Reference Rosenstein and O’Daniel8 (this is discussed in more detail in Section 4).
Most evidence on staffing relates specifically to nurses and is therefore a key focus of this Element. Much less common is research examining staffing from a whole-team perspective or looking at the impact of staffing levels in other groups (e.g. medical, pharmacy, administrative, and facilities staffReference Bond, Raehl, Pitterle and Franke9–Reference West, Barron and Harrison11) on quality or patient outcomes. However, much learning from the staffing literature on nursing may be generalisable, particularly given the key role of nurses in driving the quality of care and improvement in many settings.Reference Albanese, Evans and Schantz12, Reference Draper, Felland, Liebhaber and Melichar13 In this section, we present an overview of the research evidence on links between nurse staffing and quality in acute hospitals; consider the concept of staffing sufficiency and how it is translated into policies and guidance; look at how nurse staffing is applied in practice in relation to quality; and consider the role of nursing staff in improving care quality.
2.1 Staffing and Care Quality: The Evidence Base
A striking finding of decades of research, covering hundreds of studies systematically reviewed on multiple occasions,Reference Kane, Shamliyan, Mueller, Duval and Wilt2, Reference Shekelle14, Reference Griffiths, Ball and Drennan15 is the association between registered nurse staffing, care quality, and patient outcomes. Lower registered nurse staffing is associated with poorer care quality and worse outcomes for patients. This is evident, for example, in the finding of a significant effect of both medical and nurse staffing levels in intensive care units in England on casemix-adjusted patient mortality.Reference West, Barron and Harrison11 Both the total volume of nursing hours (as captured by ratios or by measures such as nursing hours per patient day) and the proportion of the nursing workforce that is degree-educated (as opposed to assistants and support workers without formal qualifications or registration) are important to care quality.Reference Aiken, Sloane and Griffiths16, Reference Ausserhofer, Zander and Busse17 The evidence base on the relationship between nurse staffing and care quality is heavily biased towards studies in general acute hospitals, but a number of key studies cover other settings, such as mental health,Reference Bowers and Crowder18, Reference Cook, Jones and Williams19 nursing homes,Reference Spilsbury, Hewitt, Stirk and Bowman20 and primary care.Reference Murrells, Ball, Maben, Ashworth and Griffiths21, Reference Griffiths, Murrells, Dawoud and Jones22
A 2006 systematic review of 101 studies confirmed a relationship between low levels of registered nurse staffing and adverse patient outcomes, with a meta-analysis of data from 28 of those studies finding that higher nurse staffing was associated with lower odds of hospital-related mortality and adverse patient events.Reference Kane, Shamliyan, Mueller, Duval and Wilt2 More recently, a 2014 review of evidence (including systematic reviews) for the National Institute for Health and Care Excellence (NICE) – to support development of guidelines for safe nurse staffing in adult inpatient acute settings in England – identified 35 primary studies since 2006 looking at nurse staffing and patient outcomes.Reference Griffiths, Ball and Drennan23 A summary of findings is set out in Box 1.Reference Ball and Griffiths24
Box 1 Summary of findings from 2014 evidence review for NICE
Strong evidence from several large observational studies that lower nurse staffing levels were associated with higher rates of death and falls.
Strong evidence that higher nurse staffing is associated with reduced length of stay and lower readmission rates.
Similar but less consistent evidence on infections.
Contradictory evidence on pressure ulcers.
No evidence of an association with venous thromboembolism.
The pattern of findings is broadly consistent across the substantial evidence base: when levels of registered nurse staffing are lower, outcomes are poorer. Analysis of data from nine European countries in the RN4CAST study, for example, found that an increase in a nurse’s workload by one patient is associated with a 7% increased likelihood of patient death following common types of surgery;Reference Aiken, Sloane and Bruyneel25 and the mix of nursing staff (proportion of registered nurses vs care assistants) and their education levels (proportion of workforce that is degree educated) is associated with differences in patient outcomes and experiences.Reference Aiken, Sloane and Griffiths16, Reference Ausserhofer, Zander and Busse17
2.1.1 The Plausibility of a Causal Link
Though the causal relationship between nurse staffing and patient outcomes may seem probable, there are limitations in the research.Reference Griffiths, Ball and Drennan15 One key weakness is that most studies have a cross-sectional (one-off) design, rather than a longitudinal (over time) design. However, research evidence increasingly suggests not only that low staffing is associated with worse outcomes, but that the relationship with care outcomes is causal.Reference Shang, Needleman, Liu, Larson and Stone26–Reference Needleman, Buerhaus and Pankratz28 In 2011, Needleman et al. broke the mould in nursing workforce and patient outcome research with a US longitudinal study that looked at individual patient outcomes following exposure to low nurse staffing.Reference Needleman, Buerhaus and Pankratz28 Using administrative data to capture nurse staffing for every shift, a significantly increased risk of mortality (taking account of patient factors) was observed after periods of exposure to low staffing.
Other research also supports the plausibility of a causal link between staffing, care quality, and patient outcomes. When nurse staffing levels are lower, there is an increased risk of necessary patient care being missed.Reference Ausserhofer, Zander and Busse17, Reference Ball, Murrells, Rafferty, Morrow and Griffiths29 This is a simple but highly significant finding, considering how staffing levels affect services’ ability to achieve (and improve) care quality. Nine out of 10 nurses on acute wards in 32 National Health Service (NHS) hospital trusts reported having left at least one aspect of care (i.e. that was needed by their patients) ‘undone’ on their last shift due to lack of time. The amount of care left undone was strongly related to nurses’ reports on the quality of nursing care on the ward and their ratings of the ward’s environment for patient safety.Reference Ball, Murrells, Rafferty, Morrow and Griffiths29
Further analysis of data from the RN4CAST studyReference Sermeus, Aiken and Van den Heede30 points to ‘missed nursing care’ as partially mediating the relationship between nurse staffing and avoidable patient mortality.Reference Ausserhofer, Zander and Busse17, Reference Ball, Murrells, Rafferty, Morrow and Griffiths29, Reference Ball, Bruyneel and Aiken31 Taking account of different risk factors (e.g. patient age and health conditions), more patients die following common surgical procedures when levels of missed care reported by nurses are higher; an additional 10% of missed care was associated with a 16% increased risk of patient death.Reference Ball, Bruyneel and Aiken31
Findings from a retrospective longitudinal observational study in the NHS confirm the pattern identified by Needleman et al.Reference Needleman, Buerhaus and Pankratz28 and indicated by the RN4CAST analyses. Using routinely collected staffing data over a 3-year period, the study examined its relationship with casemix-adjusted patient mortality.Reference Griffiths, Maruotti and Saucedo27, Reference Griffiths, Ball and Bloor32 The hazard of death increased by 3% for every day that a patient experienced nurse staffing that fell below the average for that ward.Reference Griffiths, Ball and Bloor32, 33
This more recent evidence supports a plausible causal link between nurse staffing levels and patient outcomes. It points to the idea that the number of registered nurses present to provide care influences the ability of a team (potentially beyond the immediate nursing team) to deliver care completely. Nurse staffing sufficiency is thus key to reducing negative care incidents associated with low staffing – such as errors, adverse events, and omissions – which may contribute to potentially avoidable deaths in some cases.Reference Griffiths, Recio‐Saucedo and Dall’Ora34, Reference Recio‐Saucedo, Dall’Ora and Maruotti35
2.1.2 How Many Is Enough?
Despite the strength of the evidence to support the general association between nurse staffing and patient outcomes, studies offer little specificity about exactly what level of nurse staffing is required to enable good quality care to flourish – that is, how many is enough? Few studies go beyond establishing a statistically significant association to provide detailed information on the numbers associated with different effects.
A US study showed that a significant increase in mortality was associated with patients’ exposure to nurse ‘short-staffing’ (defined as 8 or more nursing hours per shift below the target staffing level identified using a validated staffing tool).Reference Needleman, Buerhaus and Pankratz28 And NICE guidance for NHS hospitals identifies a daytime threshold of more than eight adult patients per registered nurse on an acute ward as associated with increased risk.36 (Of course, this varies according to the ward or unit, and for some services significant increases in risk occur well below this threshold.) The guidance does not specify what constitutes a safe minimum but does provide an indication of what unsafe might look like. NICE’s interpretation of the evidence is that a ratio of one nurse to eight patients is not likely to represent an optimal safe-staffing level in any setting; rather, it is a level at which risk is known to increase and therefore a threshold that demands urgent review.
Evidence from the NHS is consistent with international research showing that lower nurse staffing levels are associated with worse outcomes in a variety of acute ward contexts. But an outstanding question concerns the nature of the relationship between staffing and outcomes: is it a standard performance curve in which the benefits of greater nurse staffing gradually taper off once an optimal threshold is reached? In an in-depth study in a single NHS hospital trust,Reference Griffiths, Ball and Bloor32 we explicitly tested for – and found – a linear relationship between patient-level exposure to staffing at different levels and benefits; but we did not find a threshold effect. Patient benefit increased in direct proportion to increased nursing hours. Although there was a range of staffing levels across the hospital wards, we did not find a beyond optimum level – where the benefit of additional registered nurses starts to plateau.
2.2 Sufficient Staffing: Policies, Regulations, and Guidance
The principle of having sufficient staff (including nursing staff) for safe and effective care is embodied in policies, regulations, and guidance – and, in some parts of the world, in legislation. In the UK, the NHS Constitution states that patients have the ‘right to be treated with a professional standard of care, by appropriately qualified and experienced staff, in a properly approved or registered organisation that meets required levels of safety and quality’.37 From a public safety perspective, the Nursing and Midwifery Council’s professional code is explicit about the obligation of staff to raise concerns if staffing levels risk patient safety: ‘[You must] act without delay if you believe that there is a risk to patient safety or public protection.’38
Different approaches are taken to determining safe staffing, with some contention around which is most effective. The pros and cons of mandated minimums have been debated for years.39 Much of the argument stems from an artificial polarisation of the issue: the idea of mandated minimum ratios versus dependency-based tools to support local decision-making. Arguably, each has a place: a limit to ensure safety standards across a system, and judgement and tools to determine optimum levels in different contexts. But the principle that adequate nurse staffing is required to deliver high-quality care is not in question; throughout the world, it consistently underpins policies, guidance, and sometimes legislation.
In parts of the USA and Australia, the law stipulates a minimum nurse staffing level. The number of open beds and patients is limited by the number of staff present. For example, in CaliforniaReference Aiken, Sloane and Cimiotti40 and two Australian statesReference Gerdtz and Nelson41 the safe daytime minimum for an acute ward is typically one registered nurse to five patients. Proponents see this as a safety measure that protects staffing levels from becoming dangerously low; opponents see it as too blunt a measure and fear that, in a context of cost constraints and labour market challenges, a minimum can become a maximum.Reference Buchan42
Policy and law vary within the UK. In Wales and Scotland, legislation is similar to that in many parts of the USA: it makes explicit the principle of ensuring staffing levels are evidence-based, using approved tools or measures to ensure nurse staffing is sufficient to meet patient needs safely. In Northern Ireland, the Delivering Care framework included normative ranges in addition to guidance to support staffing for high-quality care.43 But in England, numbers and the proportion of registered nurses within the nursing team (referred to as the ‘skill mix’) have been determined locally by individual healthcare organisations.
In its role as healthcare regulator, the Care Quality Commission (CQC) ensures compliance with Regulation 18, which requires healthcare providers in England to ‘provide sufficient numbers of suitably qualified, competent, skilled and experienced staff to meet the needs of the people using the service at all times’.44 But the challenge for providers is gauging what is sufficient to enable not just safe but high-quality care. Following the 2013 inquiry into the care crisis at the Mid Staffordshire NHS Foundation Trust,Reference Francis45 NICE introduced guidance recommending that a daytime level of eight patients or more per registered nurse on acute wards should be considered a ‘warning’ – triggering an urgent review of metrics and staffing.36, Reference Ball46
2.3 Putting Staffing into Practice to Improve Quality
NICE guidelines for safe staffing highlight the need for a robust assessment of the nurse staffing levels required to meet patient needs on acute wards, and endorse a tool (the Safer Nursing Care Tool) for this purpose.36 But even with an accurate estimation of need and employers willing to increase staffing to ensure sufficient baseline numbers, challenges in recruitment and retention may stymie efforts to achieve those numbers, as has been the case in the NHS.Reference Ball47 Attention to the wider factors that influence recruitment and retention is therefore key,Reference McClure, Poulin, Sovie and Wandelt48–Reference Halter, Pelone and Boiko50 but one of the biggest drivers for nurses leaving the profession is too much pressure (cited second after retirement in the Nursing and Midwifery Council’s surveys of leavers).51 This highlights a degree of circularity at the heart of the issue: having enough staff is key to having enough staff.
The ability of healthcare organisations to employ sufficient numbers of registered nurses to achieve high-quality care depends not only on recognising necessary staffing levels but also on an effective labour market. In a study on the implementation of safe-staffing policies in England, directors of nursing reported that despite board-level commitment to increase nurse staffing, the biggest impediment to achieving the levels needed was an ongoing national shortage of nurses.Reference Ball47 This is a worldwide challenge, which in the USA led to a specific organisational model: Magnet hospitals.
2.3.1 Magnet Hospitals
In a context of widespread shortages of registered nurses in the USA in the late 1980s, researchers identified considerable differences between hospitals’ abilities to recruit and retain nurses.Reference McClure, Poulin, Sovie and Wandelt48 Some were struggling. But others were succeeding, as though they had magnetic properties that enabled them to attract and keep their nursing staff. These hospitals also had reputations for good quality patient care – a factor that made them attractive to nurses. The positive attributes that made Magnet hospitals attractive places to work were subsequently found to correlate with better patient outcomes (e.g. lower casemix-adjusted patient mortality rates).Reference Aiken, Smith and Lake52 Typical characteristics of Magnet hospitals are summarised in Box 2. We include traits that these hospitals tend to have (based on the original researchReference McClure, Poulin, Sovie and Wandelt48), standards they are expected to have achieved (American Nurses Credentialing Center standards), and characteristics identified in research comparing Magnet and non-Magnet hospitals.Reference Kelly, McHugh and Aiken53
Box 2 Characteristics of Magnet hospitalsReference McClure, Poulin, Sovie and Wandelt48, Reference Kelly, McHugh and Aiken53
Flatter organisational structures.
Good staffing (higher nurse-to-patient ratios).
Collaborative relationships between nurses and doctors.
Broad-based participation in decision-making related to clinical care.
Sufficient core staff (limited use of agency/temporary staffing).
Nursing research that enhances clinical practice.
Higher percentage of degree-educated or masters-educated registered nurses.
Influential nurse executives and visible nursing leadership.
Investment in the education and expertise of nurses.
Better retention and lower turnover of registered nurses.
Positive practice environment with good working conditions.
Nurses feel well supported (e.g. by support services and availability of resources) to provide high-quality care.
The Magnet phenomenon generated considerable interest in the USA.Reference Jones54 Research examining the features associated with Magnet hospitalsReference McClure, Poulin, Sovie and Wandelt48, Reference Kramer55, Reference Kramer and Schmalenberg56 was crucial in establishing that the relationship between nurse staffing and quality is about more than just numbers: a positive working environment is also critically important. Though some factors that may influence a hospital’s ability to keep staff may be intractable (e.g. location, cost of living), many of the characteristics associated with better retention and lower turnover are potentially modifiable (e.g. leadership, communication, and teamwork).
Based on this learning, the American Nurses Association developed a quality improvement programme and established the American Nurses Credentialing Center to help other centres develop the characteristics to achieve Magnet status. Study of the features of Magnet hospitals since then suggests they are associated with better patient outcomes as well as better work environments.Reference Kutney-Lee, Stimpfel and Sloane57–Reference Scott, Sochalski and Aiken59 Kelly et al. report that Magnet hospitals are more likely to have working environments that are supportive of professional nursing care than other hospitals, and to employ more highly educated nurses. They also found that nurses in Magnet hospitals were less likely to be dissatisfied with their jobs or report high burnout.Reference Kelly, McHugh and Aiken53
In 2020 there were 468 healthcare providers in five countries formally accredited as Magnets, but relatively few outside the USA. Adoption of an English Magnet model was proposed in 2015 in Lord Willis’s report on nursing, but there have been mixed views about the usefulness and transferability of the model.Reference Jones54, Reference Willis60, 61 In common with other accreditation schemes, what is unclear is whether the process of becoming a Magnet improves quality or whether the high quality and outcomes achieved by Magnets mean that better hospitals are just better.Reference Friese, Xia, Ghaferi, Birkmeyer and Banerjee62 A study launched in 2020 in five European countries, which includes a randomised controlled trial of the intervention and a process evaluation, will allow a more complete examination of the claimed ‘transformative effect’ of adopting Magnet principles and shed some light on the relative importance of different elements.Reference New63
Either way, the fact that positive nurse staffing traits (good nurse staffing levels, proportion of the workforce with a degree or a higher degree, visible nursing leadership) go hand in hand with success in achieving quality – or, in Magnet terminology, ‘nursing excellence’ – is a testament to the importance of these staffing conditions. It seems likely that the relationships between improvement and staffing may operate in the other direction also; improvement work can create better work conditions, leading to less staff stress and improved staff engagement, which may result in a more efficient use of the staff available.
2.3.2 Assessing the Impact of Staffing Changes
Healthcare organisations need some means of assessing whether they have the staffing and work conditions needed for quality and for improvement. Finding feasible and meaningful indicators for the structures, processes, and outcomes is a recognised challenge,Reference Maben, Morrow, Ball, Robert and Griffiths64 but it is essential to improvement. (For further consideration, see the Element on measurement for improvement.Reference Toulany, Shojania, Dixon-Woods, Brown and Marjanovic65)
We earlier referred to the important research finding that care left undone is associated with low staffing (Section 2.1.1). In Ireland, this has led to its use as an indicatorReference Drennan, Duffield and Scott66 which was adopted by the government. Care left undone events (referred to as safety CLUEs) were used as a metric to assess signs of insufficiency and measure improvement as staffing levels were increased (Box 3).Reference Drennan, Duffield and Scott66
Box 3 Putting evidence into practice: a nurse staffing framework to improve quality
Objective: to apply an evidence-based approach to nurse staffing in healthcare.
Key Project Phases
Develop a nurse staffing framework based on best available international evidence.
Make recommendations for the implementation and monitoring of the framework (including education, training, and guidance).
Apply the framework to change nurse staffing at three pilot sites.
Evaluate the impact of the framework.
Nurse Staffing Changes
Nurse staffing determined using the measure of nursing hours per patient day.
Staffing was increased in understaffed wards.
Increased staffing had a stabilising effect and resulted in improved patient, staff, and organisational outcomes.
Rostered skill mix reached a level of 80% registered nurses in all wards.
100% of clinical nurse managers' time in most wards was available to supervise and lead others (as opposed to having a direct patient caseload).
Impact of Applying the Framework
Reduced use of agency staff (even in the wards that did not have an uplift).
Average patient length of stay shorter (by 2 days or more).
Fewer reports of patient care being left undone (from 76% before to 32% after).
Improved staff views of the practice environment.
Quality of care delivered to patients rated more highly by staff.
2.4 Staffing and Healthcare Improvement
Without adequate staffing and dedicated time, the risk is that improvement work becomes another aspect of service delivery that is neglected or left undone.Reference Zoutman and Ford68, Reference Dixon-Woods69 Addressing staff insufficiency depends, of course, on an accurate local assessment of the work to be done and the skills and numbers of staff needed to do it. For example, initiatives such as the Productive Ward, designed to improve quality and in the longer term release time to care, have often been hampered by lack of staff to backfill and enable implementation of change.Reference Morrow, Robert and Maben70 Staffing fully takes time; improving how care is delivered also takes time; and in healthcare, time means staff. Needleman and Hassmiller argue that goals of assuring the adequacy and performance of hospital nursing, improving quality, and achieving effective cost control need to be thought about collectively and not as competing priorities, noting that:
… simply changing leadership’s view of front-line staff or changing hospital culture to embrace a culture of improvement will be insufficient … improvement must be institutionalized in the day-to-day work of the front-line staff, with adequate time and resources provided and with front-line staff participating in decision making.Reference Needleman and Hassmiller71
However, even with the right staff in the right place and at the right time, care quality is not guaranteed and improvement is not assured. How staff work together within a team, the extent to which they feel safe to raise concerns and challenge unsafe practices, and the extent to which they are well themselves and able to operate to the best of their abilities also have an impact. Sections 3 and 4 look at these other key building blocks to creating the conditions in which healthcare quality and improvement can be achieved.
3 Psychological Safety, Teamwork, and Speaking Up
Acknowledging and attending to the social and cultural context is vital if improvement interventions are to work.Reference Dixon-Woods and Martin72 Regardless of the number or mix of staff, how staff work together influences the chances of achieving safe, high-quality care and the ability to learn from mistakes. Achieving high-quality care is more dependent than ever on how well people work together; this in turn is affected by organisational factors like leadership and the working environment, not just clinical training.
Psychological safety, teamwork, and speaking up are distinct but interrelated phenomena that affect both the quality of healthcare and the ability to improve it. This section focuses on these three factors as an additional set of workplace conditions that affect healthcare improvement.
Psychological safety is defined as an interpersonal climate in which individuals feel able to take interpersonal risks without fear of negative consequences.Reference Edmondson73
Psychological safety is considered especially relevant for enabling speaking up – a behaviour in which people voice their observations, questions, and concerns, especially to colleagues above them in a hierarchy.Reference Edmondson73
Teamwork describes coordination and collaboration activities through which people accomplish interdependent tasks – as noted in a review of research on teams in healthcare.Reference Fried, Edmondson, Burns, Bradley and Weiner74
3.1 Teams and Psychological Safety
Improvement work necessitates small interpersonal risks – including the risk of looking ignorant (asking a question that might expose your ignorance to others), looking incompetent (when admitting a mistake or a weakness), or appearing negative or critical (when pointing out a flaw in a process worthy of improvement). One way for individuals to minimise risk to their image is simply to remain silent. The problem with this approach is that it precludes learning and innovation.
Similarly, by its very nature, teamwork involves interpersonal risk. Rather than carrying out prescribed tasks with scripted interactions, people working effectively in teams must constantly ask questions, offer ideas, and coordinate actions, with the ever-present risk that actions may not align perfectly and so require continuous attention and adjustment. An important responsibility for healthcare leaders, therefore, is to understand psychological safety, its role in teamwork, and its antecedents.Reference Frazier, Tix and Barron75–Reference Edmondson and Lei77
Classic research by Goffman describes how people avoid behaviours that might threaten the image others hold of them,Reference Goffman78 and helps to explain the relationship between psychological safety and teamwork. Social psychologists call this well-documented tendency ‘impression management’. Holding back from speaking up with a comment or question that might lead others – especially those in a formal evaluative role – to see us in a negative light is all but second nature for most working adults. The concept of psychological safety was first described in the management literature in the 1960s as a factor in helping people to learn new behaviours and overcome defensive routines.Reference Schein and Bennis79 Research on psychological safety has flourished since the turn of the century, in part driven by recognition of its importance in complex, interdependent work.Reference Sanner and Bunderson80 Two meta-analyses compiling empirical evidence of the relationship between psychological safety and team outcomes from more than 80 unique studies have further established the construct as a useful one for organisational research.Reference Frazier, Tix and Barron75, Reference Sanner and Bunderson80 Among the positive outcomes of psychological safety are better communication, knowledge sharing, speaking up, learning behaviour, creativity, innovation, engagement, and performance.
The salience of psychological safety for teamwork and improvement work is well established (see Edmondson and LeiReference Edmondson and Lei77 for a review). A lack of psychological safety can be found at the root of many noteworthy organisational errors and failures across industries. A climate of psychological safety, on the other hand, makes it easier for people to voice tentative thoughts. And as team members share ideas, respond respectfully to the views of others, and engage in healthy debate, they establish vital shared expectations about appropriate ways to behave. In particular, a climate of psychological safety can help people override a tendency to default to silence, instead encouraging or allowing them to offer ideas, report errors, and speak up in ways that are vital for healthcare improvement. Improvement starts with clear-eyed identification of quality gaps, including errors and wasteful workarounds (i.e. shortcuts people take at work when they confront a problem that disrupts their ability to carry out a required task). When people feel unable to speak up about such shortcomings, efforts to change work processes for the better are thwarted. A climate of psychological safety may have a particularly important role in efforts to detect errors (e.g. work by Edmondson et al.Reference Edmondson81, Reference Edmondson, Roberto and Tucker82) and in preventing errors before patients are harmed (e.g. EdmondsonReference Edmondson81 and Goodman et al.Reference Goodman, Villarreal and Jones83).
Some adverse events occur when a confluence of small process failures combine in unfortunate ways (the Swiss cheese modelReference Reason84) that no one anticipates; more often, however, someone experiences a flicker of concern but remains silent for fear of the consequences of speaking up. The real-life episodes in Boxes 4 and 5 illustrate this phenomenon.
Box 4 A micro-moment of silence
A nurse on the night shift in a busy urban hospital notices that a dose for a postoperative patient appears not quite right. Fleetingly, he considers calling the doctor at home to check the order but – on recalling her disparaging comments about his abilities last time he had, without a great deal of conscious thought, called her at home – he reconsiders. All but certain that the dose is fine (the patient is on an experimental protocol, after all), he grabs the medication and heads for the patient’s bed. This micro-moment of silence depicts what it means to lack psychological safety in the face of uncertainty.
Box 5 Not safe to speak up in a pandemic
During the 2020 COVID-19 pandemic, there were several cases of clinicians speaking up about PPE shortages only to be bullied, rebuked, or fired by their hospitals.Reference Coronavirus85 Employers had warned that workers should toe the party line and threatened that speaking up will result in positions and careers becoming untenable.Reference Dyer86 Clinicians assumed it was safe to speak up about shortages of lifesaving equipment, only to discover that despite patients’ and their own safety being at risk, they were wrong. Mannion and Davies describe a ‘well-worn path’ where ‘concerns about care are raised and ignored, staff are denigrated or bullied and the situation escalates into whistleblowing to outside authorities’.Reference Mannion and Davies87 A prolonged neglect of concerns, warning signs, and signals from workers can create deep pockets of organisational silence, ‘deafness’, and ‘blindness’.Reference Jones and Kelly88
Some research has found that groups with higher psychological safety report more errors to head nurses;Reference Edmondson81 but crucially, a combination of high psychological safety and nurses’ beliefs that patient safety is a high departmental priority is associated with the fewest errors.Reference Leroy, Dierynck and Anseel89 People can perform the highest quality work and still be willing to talk about the errors that do occur;Reference Edmondson81 moreover, this is how high-quality work (error-free, at the sharp end) is achieved in complex settings – by openness and vigilance along the way. By contrast, error rates may be high when psychological safety is low, even when staff believe the department is committed to patient safety (see Figure 1).Reference Leroy, Dierynck and Anseel89 Psychological safety therefore appears to be vital for continuous improvement and to the quality of patient care.
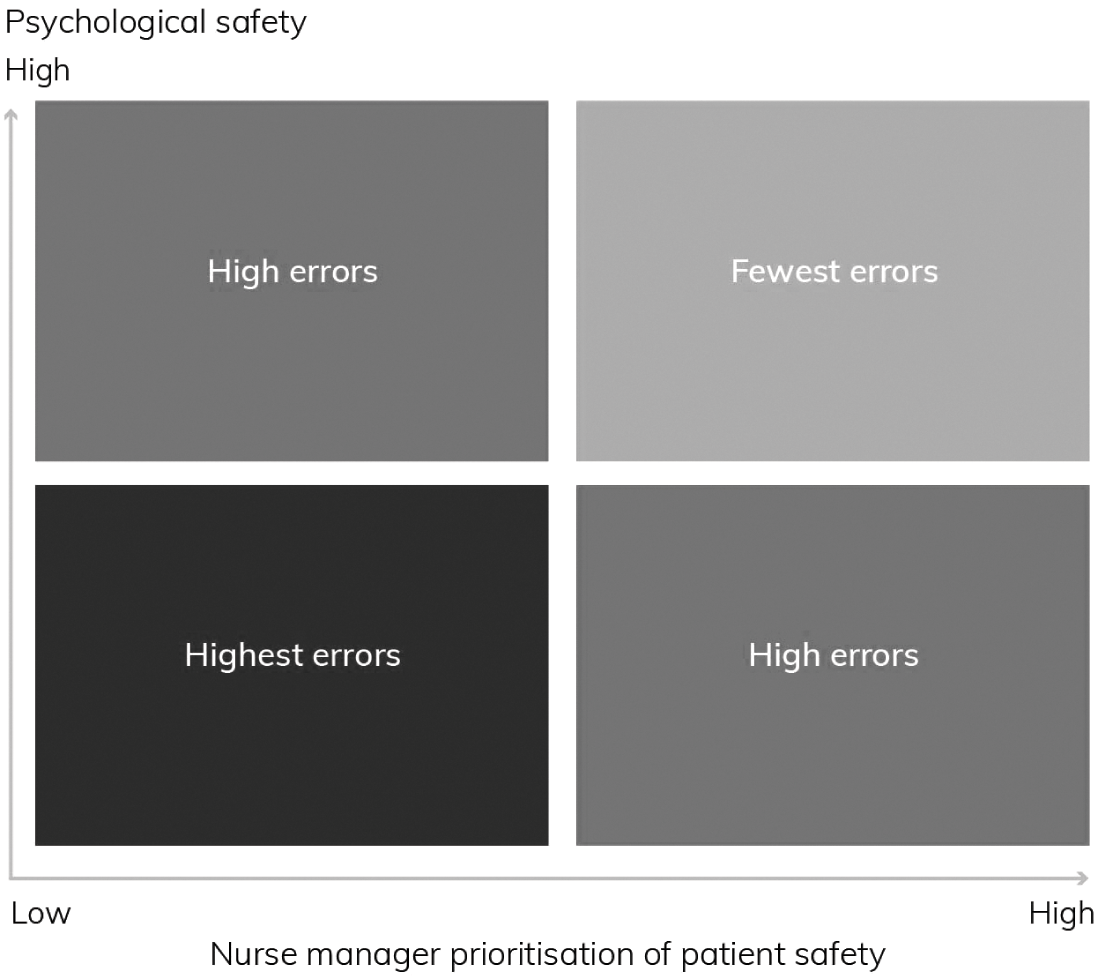
Figure 1 How the relationship between manager prioritisation of patient safety and psychological safety affects organisational errors
The positive effects of psychological safety on employee engagement have also been established.Reference May, Gilson and Harter90–Reference Ulusoy, Mölders and Fischer92 Engagement – the extent to which an employee feels passionate about the job and committed to the organisation – is seen as an index of willingness to put discretionary effort into one’s work. Disengagement can lead to safety risks and high staff turnover, which in turn leads to additional recruitment and training costs and a less experienced workforce. Accordingly, interest has grown in improving healthcare working environments as a strategy for employee retention. In one study of clinical staff at a large metropolitan hospital, psychological safety was related both to a commitment to the organisation and patient safety. The authors note that a working environment in which healthcare workers feel safe to speak up about problems is especially important for helping them feel able to provide safe care and be engaged in their work.Reference Rathert, Ishqaidef and May93
3.2 Psychological Safety and Improvement Work
Merely launching improvement projects is insufficient for ensuring progress: supervisors cannot simply command staff to work on such projects without creating a fertile soil of psychological safety to soften the interpersonal risks. A study of more than 100 improvement project teams in neonatal intensive care units in 23 North American hospitals discovered considerable variation in their success.Reference Tucker, Nembhard and Edmondson94 By asking team members to report on what they did to improve unit processes, researchers identified two distinct sets of learning behaviour: ‘learn-what’ and ‘learn-how’. Learn-what describes independent activities, such as reading the medical literature; learn-how comprises team-based learning, such as proactively sharing knowledge, offering suggestions, and brainstorming better approaches. Arguably, both are vital for improvement work. Psychological safety predicted learn-how behaviours (which involve interpersonal risk) but had no statistical relationship with the learn-what activities. This means that while psychological safety is important for behaviours that involve interpersonal risk, it does not adversely affect learning behaviours that you can do alone (e.g. read a book, take an online course).
Relatedly, psychological safety is associated with nurse engagement in improvement work to reduce ‘workarounds’.Reference Tucker, Nembhard and Edmondson94, Reference Tucker and Edmondson95 A workaround accomplishes the immediate goal but perpetuates the problem that triggered the workaround in the first place. Because workarounds appear to work in the short term, they can delay or prevent process improvement. But the problems that trigger workarounds might more usefully be seen as small signals of a need for change in a system or process. When clinicians do not feel safe enough to speak up and suggest improvements, workarounds are perpetuated. A study of cancer teams found that those with low psychological safety relied more on workarounds, while teams with high psychological safety focused more on diagnosing problems and improving the processes that caused them.Reference Halbesleben and Rathert96 Here again, the crucial mechanism that makes it possible to alter and improve work processes is the ease with which people are able to speak up about problems.
3.3 Psychological Safety in the Broader Context
Speaking up at work can, of course, be difficult. People naturally worry that their boss or colleagues will not like what they have to say, so interpersonal risk remains a formidable barrier to effective teamwork and improvement activities. In the several dozen empirical studies of psychological safety, several types of influences on psychological safety have been identified. In rough order of emphasis, they are: leadership behaviour, organisational support, team attributes, relationship networks, and personality factors (see the 2017 review by Newman et al.).Reference Newman, Donohue and Eva76
Supportive leadership behaviour is the most prominent factor in promoting psychological safety in a team. In healthcare studies, one of the most frequently identified variables is leadership inclusivenessReference Nembhard and Edmondson97 or the degree to which leaders are perceived as accessible, invite input, and acknowledge their own fallibility. An improvement-oriented management style,Reference Halbesleben and Rathert96 behaviour integrity,Reference Leroy, Dierynck and Anseel89 and shared leadershipReference Liu, Hu, Li, Wang and Lin98 are also related to psychological safety in teams. Box 6 illustrates the role of leadership in the use of a dry run in an operating theatre. (For further discussion, see the Element on governance and leadership.Reference Fulop, Ramsay, Dixon-Woods, Brown and Marjanovic100)
Box 6 Feeling safe to speak up in the operating room
In a study of 16 cardiac surgery departments implementing a new minimally invasive technology, clinicians in some (but not all) of these departments were able to speak up. One practice that helped was a dry run (i.e. with no patient present) to make it easier to practise speaking up despite status differences. In one operating team, a technician reported:
The night before [our first real minimally invasive case] we did everything. … We’d had a couple of talks in advance and the night before we walked through the process step by step. … We communicated with each other as if it were happening – ‘the balloon is going in,’ and so on … [And, the surgeon] gave us a talk about … the kind of communication he wanted in the OR [operating room], what results he expected, and told us to immediately let him know if anything is out of place.
Organisational factors that influence psychological safety include perceptions of organisational support,Reference Edmondson, Mannix, Neale and Wageman101 access to mentoring,Reference Chen, Liao and Wen102 and diversity practices.Reference Singh, Winkel and Selvarajan103 Team attributes that influence psychological safety include a climate of continuous improvement (positive) and the existence of subgroups (negative). A growing literature is also investigating the effects of relationship networks on psychological safety. This includes research demonstrating effects on psychological safety of having rewarding co-worker relationships,Reference Carmeli and Gittell104 energising relationships,Reference Cross, Edmondson and Murphy105 and prior interaction with team members.Reference Roberto106
For team leaders and senior clinicians, their own comfort in speaking up is less important for establishing psychological safety than how they respond when other members voice concerns, ask for help, or point out an error. Critical events, especially early in a team’s life, can have an exaggerated influence on team norms.Reference Ericksen and Dyer107 A single instance of a leader critiquing, talking over, or otherwise dismissing a concern raised by a team member can set a precedent for the whole team and increase the perceived risks of raising such concerns well into the future (see Box 7). It is easy for critical incidents to turn into repeated patterns. And once a norm of not rocking the boat becomes established, it takes serious effort to reverse it.
Box 7 Not questioning orders
A neonatology nurse wondered why a premature infant was not being given surfactant to promote the high-risk baby’s lung development. Stepping forward to remind the doctor about the widely used protocol, she instead caught herself – recalling a public humiliation experienced by another nurse when questioning one of his orders.
It is not only leaders who are responsible for creating a healthy climate, however; all employees can help to shape a work environment characterised by candour and commitment to improvement. They do this by taking the very small risks of speaking up with their observations and by asking thoughtful questions that encourage others to do the same.
Overall, a large body of accumulated research suggests that healthcare organisations would do well to emphasise learning and continuous improvement, while providing supportive working conditions and offering training for mid-level leaders (and all people managers) whose behaviours seem to have the most influence on the psychological safety climate in healthcare settings.
4 Staff Health and Well-being at Work
Healthcare staff in many countries around the world, including the UK, work in systems under pressure from workforce shortages, rising patient demand, and increased throughput and work intensity.109, Reference Bodenheimer, Chen and Bennett110 Workplaces may lack adequate resources, effective teamwork, and psychological safety. All these factors can contribute to poor mental and physical well-being, and improvement efforts may be neglected as staff manage day-to-day pressures, firefight in poor working environments, and become stressed and burnt out. This section unpacks the work challenges specific to healthcare; explores the consequences of poor well-being at work, including the link between staff well-being at work and care quality; and identifies interventions to support psychological well-being at work.
4.1 Specific Work Challenges in Healthcare
Healthcare professionals are exposed to a range of emotional and physical challenges in their day-to-day delivery of patient care. Working and learning in the health and care sector is like no other employment environment; staff are confronted daily with extremes of joy, sadness, and despair, and clinical staff may retain traumatic memories.111 NHS staff are more likely to incur a work-related illness or injury than staff in other sectors,Reference Boorman112 and they have a higher rate of sickness absence compared to the average UK worker (in both the public and private sectors).113 Stress among healthcare staff is greater than in the general working population and explains more than 25% of absence.Reference Boorman112 Depression, anxiety, and a loss of idealism and empathy are reported by nurses.Reference Harvey, Laird, Henderson and Hotopf114, Reference Maben, Latter and Clark115 Heavy workloads, bureaucracy, and dealing with challenging patient conditions are all significant contributors to staff well-being,Reference Rupert, Miller and Dorociak116 and pressure from budget constraints and staff shortages can take its toll on staff as well as patients.111, Reference Ham117 The well-being of healthcare practitioners is typically worse than in other professions;Reference Brand, Thompson Coon and Fleming118, Reference Brooks, Gerada and Chalder119 healthcare staff in the UK have been described as running on empty and the ‘shock absorbers in a system lacking [the] resources to meet rising demands’.Reference Ham117 Many countries in Europe and around the world face similar challenges.Reference Afolabi, Fernando and Bottiglieri120
One approach commonly used to understand staff well-being at work is the job demands-resources (JD-R) model.Reference Demerouti, Bakker, Nachreiner and Schaufeli121 Job demands are physical or emotional stressors, such as time pressures, heavy workloads, difficult working environments, emotional labour, and poor relationships. Job resources (positives) are the physical, social, and organisational factors that help achieve goals and reduce stress – including autonomy, good working relationships, and (peer, supervisor, and team) support. The JD-R model suggests that availability of job and personal resources can help cushion the negative effects of high job demands on employee well-being. Staff with high levels of job discretion and support can be expected to cope more effectively with their job demands, while well-being is likely to be lowest in situations characterised by a combination of high job demands and limited resources.Reference Bakker and Demerouti122 In our own study,Reference Maben, Peccei and Adams123 which examined links between staff well-being at work and patient experiences of care, we found that high job demands can significantly dampen, if not completely nullify, the positive effect of job and individual resources on well-being; resources are more likely to have a beneficial effect when job demands are less intense.Reference Maben, Peccei and Adams123
4.2 The Consequences of Poor Well-being at Work
Without the right support, staff are vulnerable to chronic stress and mental illness,Reference Harvey, Laird, Henderson and Hotopf114 and up to one in three healthcare professionals experiences forms of psychological distress that necessitate clinical intervention.Reference Taylor, Xyrichis, Leamy, Reynolds and Maben124 Poor mental health among the NHS workforce is a major healthcare issue, leading to presenteeism, absenteeism, and loss of staff.111 Emotional exhaustion, burnout, high sickness absence, and high turnover are all common.Reference Sturgess and Poulsen125, Reference McCray, Cronholm, Bogner, Gallo and Neill126 Multiple government and industry reports have highlighted the need to reduce stress and improve mental health among NHS staff.111, Reference Limb127–Reference Stevenson and Farmer129 Neglecting the well-being of healthcare staff also has significant implications for patients; rates of sickness absence among NHS staff are double the national average113 and are estimated to cost £1.1 billion per annum.111
International evidence highlights the consequences of adverse workplace conditions. Research across 12 European countries suggests longer working hours in the nursing profession cause poor well-being and lead to higher rates of burnout and medical risk.Reference Dall’Ora, Griffiths, Ball, Simon and Aiken130 Among UK doctors, the effects of work-related stress on sleep, health, and personal relationships have led to early retirement.131 Several international studies indicate that staff are more likely to intend leaving their profession or to experience absenteeism when they suffer from low well-being or burnout.Reference Van der Heijden, Brown Mahoney and Xu132, Reference Willard-Grace, Knox and Huang133 In the UK, the cost to the NHS of the deterioration in staff retention is thought to be as much as £100 million per annum.111
Hall et al.’s systematic review synthesised 46 quantitative studies to determine whether well-being and burnout in healthcare professionals is associated with patient safety.Reference Hall, Johnson, Watt, Tsipa and O’Connor134 Of the 27 studies measuring well-being, 16 found links between poor well-being and poor patient safety. Of the 30 studies measuring burnout, 21 found associations between burnout and patient safety. Poor well-being and moderate-to-high levels of burnout can therefore be linked to poor patient safety outcomes. Patient safety measures often relied on self-reported errors, however. The authors suggest future research could be enhanced by the use of clearer definitions of staff well-being, studies capable of determining causality between concepts, and conducting studies in primary care settings.Reference Hall, Johnson, Watt, Tsipa and O’Connor134
More broadly, there is some evidence of associations between staff well-being at work, patient experience, and safety outcomes.Reference Maben, Adams, Peccei, Murrells and Robert7, Reference Maben, Peccei and Adams123, Reference Raleigh, Hussey, Seccombe and Qi135 Patient experiences are generally better when staff feel they have a good local team/work group climate, job satisfaction, no emotional exhaustion, a positive organisational climate, and support from co-workers, supervisors, and their organisation. In 2009, the landmark Boorman review found that patient satisfaction in acute trusts was higher where staff health and well-being (measured by injury rates, stress levels, job satisfaction, and turnover intentions) were higher.Reference Boorman112 Conversely, poorer outcomes and patient experiences were likely when staff were unhappy or unhealthy and where there were high rates of staff sickness, stress, and turnover.Reference Boorman112 Staff themselves recognised a link: over 80% of staff who contributed to the Boorman review said their state of health affected patient care. In 2016, a systematic review concluded that ‘poor wellbeing and moderate to high levels of burnout are associated, in the majority of studies reviewed, with poor patient safety outcomes such as medical errors’ but ‘the lack of prospective studies reduces the ability to determine causality’.Reference Hall, Johnson, Watt, Tsipa and O’Connor134
While the relationship between staff well-being and the delivery of high-quality care makes intuitive sense, it is often simplified as happy staff meaning happy patients (and vice versa).Reference Edwards136–Reference West138 Studies now suggest a more complex picture: the well-being and experiences of healthcare staff do influence patient experiences of care for good or ill,Reference Maben, Peccei and Adams123 but staff happiness and well-being are also shaped by the quality of immediate working relationshipsReference Adams and Bond139–Reference Carter and West141 and staff workplace behaviours towards one another.Reference Burnes and Pope142 Our study examining links between staff well-being and patient experiences confirms this, highlighting the importance of the local work climate for staff well-being and high-quality patient care delivery.Reference Maben, Peccei and Adams123 A strong climate for patient care, particularly at the team level, can help to reinforce some of the positive effects of individual well-being on patient care performance; and crucially, it can also make up for the absence of high levels of individual well-being.
The Boorman review recommended that staff health and well-being should be embedded in the core business of the NHS in order to deliver long-term savings and improved patient careReference Boorman112 – a recommendation that was adopted in the 2010 NHS white paper. This policy focus seemed overdue then, yet 10 years later the NHS Staff and Learners’ Mental Wellbeing Commission noted that levels of staff stress, bullying and harassment, and sickness absence had all increased and appeared intractable.111
In 2015 Bodenheimer and Sinsky proposed expanding the Institute for Healthcare Improvement’s Triple Aim framework, whose three aims – enhancing patient experience, improving population health, and reducing costs – are widely accepted as a compass for optimising health system performance. Bodenheimer and Sinsky’s proposal was for a quadruple aim, adding the goal of improving the work life of healthcare providers, including clinicians and staff.Reference Bodenheimer and Sinsky143 We endorse this, but we suggest it is important to go beyond the system level that the authors address: improving the work life and psychological well-being of healthcare staff is important in its own right and imperative for good employers and individual staff members and their teams.
4.3 Interventions to Support Psychological Well-being at Work
The well-being of healthcare staff is now firmly on the international agenda, but evidence is limited for which well-being interventions are most appropriate for different staff groups working in different environments. A key debate continues to centre on whether interventions should be individually or organisationally focused – or perhaps both. A 2019 review commissioned by the Department of Health concluded that interventions need to operate at an organisational level and have the commitment and engagement of senior staff in order to improve working conditions.Reference Harvey, Laird, Henderson and Hotopf114 In practice and research, however, interventions are frequently geared towards improving individual coping mechanisms, such as mindfulness training, resilience building, and mentoring.Reference Pezaro, Clyne and Fulton144, Reference Irving, Dobkin and Park145
4.3.1 Individual Interventions
In terms of an individual focus, there is some evidence to suggest that mindfulness has good outcomes. A 2017 systematic review analysed the evidence on mindfulness-based interventions and their effectiveness in reducing stress among healthcare professionals. It concluded that such interventions may reduce stress, but the evidence is limited because of small sample sizes and lack of theoretical framing; longer-term follow-ups are required.Reference Burton, Burgess, Dean, Koutsopoulou and Hugh-Jones146 Lomas et al.’s 2018 review found that mindfulness interventions are associated with positive outcomes, and this appears to be a consistent finding across different healthcare professions, including mental health staff. But mindfulness is constructed in a number of ways across the studies, and only 26 of the 66 studies involved a control group, which make conclusions about well-being improvement difficult to compare.Reference Lomas, Medina, Ivtzan, Rupprecht and Eiroa-Orosa147
Some evidence supports clinical supervision in the helping professions,Reference Wheeler and Richards148 including a controlled trial with mental health nurses in AustraliaReference White and Winstanley149 and restorative supervision with public health nurses in the UK.Reference Wallbank150 The latter seeks to overcome some of the challenges that have become inherent in clinical supervision – the risk that it becomes a managerial approach to oversight and professional surveillance rather than an educational therapeutic space for staff to process and make sense of challenging clinical encounters. Drawing on the evidence to develop interventions to support staff psychologically during the COVID-19 pandemic, we have identified a range of evidence-informed interventions for individuals, teams, managers, and leaders, including the importance of peer support, buddying, and places to reflect on and make sense of practice with colleagues.Reference Maben and Bridges151 Most are also relevant for supporting healthcare staff during non-pandemic times.
There is less good evidence regarding the resilience-based training programmes that have become commonplace in healthcare.Reference Pipe, Buchda and Launder152, Reference Foster, Cuzzillo and Furness153 Traynor delivers a blistering critique of resilience training and resilience as a concept used in nursing to explore the factors that enable nurses to overcome adversity.Reference Traynor154 He argues that warnings from leaders in the field of resilience research have not been heeded; they suggest resilience is not simply an individual’s inner quality but is linked to systems/contexts and the individual’s response to these.Reference Traynor154 An overemphasis on nurses being resilient in the face of understaffing and often intense emotional work is consistently challenged by nurses and nurse academics, who see the framing and targeting of resilience as an individual trait as letting organisations ‘off the hook’.Reference Traynor154 Too often, however, an individualistic focus on resilience has been the primary strategy of healthcare organisations to date.
4.3.2 Organisation or System-Wide Interventions
Carrieri et al.’sReference Carrieri, Mattick and Pearson155 analysis of 179 studies of doctors (45% from the USA) found that interventions that emphasise relationships and belonging, such as those creating a people-focused working culture, were more likely to promote well-being, concluding that multidimensional and multilevel interventions to tackle doctors’ and students’ mental ill health are most likely to be successful.Reference Carrieri, Mattick and Pearson155 Generally, however, the focus on organisation-wide or system-wide interventions – addressing, for example, job redesign and task restructuring – has been lacking (notwithstanding the Magnet hospitals discussed in Section 2.3.1).Reference Awa, Plaumann and Walter156 One systematic review of interventions that included all healthcare staff within a healthcare setting (e.g. the whole hospital or a whole unit/ward) in collective activities to improve physical or mental health or promote healthy behaviours identified just 11 studies that used a whole-system approach.Reference Brand, Thompson Coon and Fleming118 Yet these very structural aspects of work are precisely those identified by proponents of the quadruple aimReference Bodenheimer and Sinsky143, Reference Sikka, Morath and Leape157 and those who have studied poor mental health among healthcare professionals.Reference Brand, Thompson Coon and Fleming118
One organisation-wide intervention that shows promise is Schwartz Rounds (often referred to as simply Rounds), where issues of emotional, social, and ethical complexity are examined and questions and issues about healthcare quality can be explored. Rounds are open to all staff in a healthcare organisation and provide a (usually monthly) forum to discuss the emotional impact of work in a safe and confidential environment.Reference Maben, Taylor and Dawson158, Reference McCarthy, Taylor, Leamy, Reynolds and Maben159 Rounds are widely used in the USA and have grown in popularity in healthcare organisations in the UK, Ireland, and Australia. Rounds last 1 hour and commence with three-to-four staff stories presenting an experience that is collectively shared (e.g. a patient case), or a set of individual experiences based around a theme (e.g. a patient I’ll never forget). Staff tell stories that reflect complex issues, which can provide learning for colleagues and enable ripple effects and changes in practice to occur (see Box 8 for an example).Reference Maben, Taylor and Dawson158
Box 8 Schwartz Rounds: sharing and hearing other staff experiences changes behaviour
A doctor reported hearing colleagues present a story about a vulnerable patient being discharged too soon. He said:
I suppose what’s had the biggest impact on the way I provide compassionate care and what’s changed my behaviour the most is the Round where we had the vulnerable adults team presenting. They presented a story in great detail about a patient, who was medically fit for discharge and therefore perceived by the trust as a ‘bed-blocker’, but actually they were very vulnerable and they couldn’t be safely discharged and what had happened when they’d been discharged inappropriately in the past. For me that’s the situation in which I am most commonly at risk of not providing compassionate care like last night when the hospital has no beds – it was remembering those stories about the risks of sending home vulnerable adults that has made me stop and think. That is the Round that’s changed my behaviour to the greatest extent.
Taylor et al. synthesised evidence for Rounds and compared their effectiveness to other reflective interventions, such as action learning sets, after action reviews, and Balint groups.Reference Taylor, Xyrichis, Leamy, Reynolds and Maben124 Prior to Maben et al.’s 2018 evaluation undertaken in the UK,Reference Maben, Taylor and Dawson158 however, evidence for their effectiveness was limited. Though studies had determined that Rounds were highly valued by attendees, most used non-validated questionnaires and had weak designs with no control group.Reference Taylor, Xyrichis, Leamy, Reynolds and Maben124 Maben et al. used a realist evaluation approach with nine case studies and a survey with control group. The survey found that poor psychological well-being (measured by the clinically validated GHQ-12) reduced significantly more in Rounds attenders (a 13% decrease compared with 3% in non-attenders). Among regular Rounds attenders, poor psychological well-being dropped from 25% to 12%, compared with a non-significant reduction (37% to 34%) in those who chose not to attend Rounds (the control group). Other reported outcomes include a greater understanding of context and therefore insights into the behaviour of colleagues, patients, and caregivers, which resulted in increased tolerance, empathy, and compassion for colleagues and patients. Better support for staff, reduced isolation, improved teamwork and communication, and reported changes in practice were also noted.Reference Maben, Taylor and Dawson158
Rounds could provide a psychologically safe space in which issues of quality, safety, and healthcare improvement could be identified and foregrounded, and organisational behaviour change could be reported (see Box 9 for an example). Rounds are not for everyone, however; some staff struggled to attend, in particular ward-based nurses and community staff.Reference Maben, Taylor and Dawson158
Box 9 A new support group set up for staff as a result of a Schwartz Round
On the back of the Schwartz Round, a colleague emailed the head of nursing. The start of the email read: ‘I attended the Schwartz Round, the panel was all nurses and I heard the stories about nurses feeling unsupported and isolated.’ As a result, the head of nursing took it up to the board, who agreed to reintroduce clinical supervision for nurses.
As we have shown, however, the evidence on intervention effectiveness in terms of improving staff well-being is limited, particularly for interventions involving whole-system approaches (i.e. those that consider both individual and organisational factors) as recommended in the Boorman review.Reference Boorman112 Further, the evidence is often compiled from global sources (e.g. Hall et al.Reference Hall, Johnson, Watt, Tsipa and O’Connor134 and Burton et al.Reference Burton, Burgess, Dean, Koutsopoulou and Hugh-Jones146), thereby neglecting the different contexts of different health systems. Though somewhat constrained, the evidence base that exists on whole-system interventional approaches identifies some that appear to be effective.Reference Harvey, Laird, Henderson and Hotopf114, Reference Brand, Thompson Coon and Fleming118, Reference Taylor, Xyrichis, Leamy, Reynolds and Maben124 We have identified one such example, Schwartz Rounds, and provided examples of how in small, but crucially important, ways staff can be engaged, behaviours can be changed, and outcomes identified that improve care quality. In practice, many interventions that target NHS staff place the burden for good mental health on individuals and exhort them to improve their resilience.Reference Maben and Bridges151 This neglects the wider structural and organisational constraints and contexts that may have a detrimental effect on staff well-being.Reference Brand, Thompson Coon and Fleming118 We are not suggesting this is an either/or; individual interventions and structural interventions are both important, but not the former without the latter. Overall, we suggest that changing the work environment to promote positive staff well-being at work is likely to better enable quality, safety, and improvement work; the benefits are not just an absence of negatives (sickness absence, low morale, high turnover) but an enriched and motivated staff more able to fully engage in their work and improve quality.
5 Conclusions
This Element has focused on the workforce and people dimensions of healthcare improvement, seeking to identify the conditions required to enable staff to engage in their work and improve quality. We have considered how workplace conditions influence the work of improvement and the creation of an optimal culture for improvement where, every day and at every level, the work context must support the question, ‘how could we do this better?’ Fostering conditions that allow staff to flourish and contribute – not just to delivering current services but to continuously improving them – is vital, especially given that in many countries recruiting, supporting, and retaining the healthcare workforce is a major challenge. The NHS People Plan makes this clear: it seeks to make the NHS an employer of excellence and an excellent place to work, improving culture so that staff feel they have fulfilment, voice, and belonging.160 All three of the conditions for healthcare improvement that we identify – staffing adequacy, psychological safety, and staff well-being – depend on leadership, management support, and role modelling. We have drawn on a wide range of evidence to suggest that without attention to the needs of the workforce and to workplace conditions, many improvement interventions or approaches may fail – either because staff are not engaged and actively involved, or because the causes and consequences of poor workplace conditions for staff and for improvement are not given sufficient attention.
5.1 Quality Is the Mainstay of Healthcare Professionals’ Work
Healthcare staff often want more than the opportunity (and resources) to deliver excellent care. They want to use their skills, knowledge, and expertise to improve the quality of care provided. We agree with Needleman and Hassmiller that improving healthcare ‘must be institutionalized in the day-to-day work of the front-line staff, with adequate time and resources provided and with front-line staff participating in decision making’.Reference Needleman and Hassmiller71 This positioning of quality as the mainstay of the work of healthcare professionals thus needs to be reflected in the systems and contexts that healthcare organisations themselves provide and create: the vision for quality and constant improvement should be clear, the resources and training required should be available, and the context should be enabling. Part of enablement involves providing staff and patients with the resources, opportunities, and skills they need to contribute. Recognition of this often manifests in drives from senior leadership or management to build improvement capability; but frontline staff and service users must also feel able to make use of these skills and take ownership of improvement work.Reference Dixon-Woods, McNicol and Martin161
Staff are more likely to come forward with system improvements when there is a culture that supports voicing concerns and speaking up,Reference Mannion and Davies87, Reference Detert and Burris162 in particular where a culture of psychological safety is encouraged.Reference Barzallo Salazar, Minkoff and Bayya163 When teams feel psychologically safe, they share information of significance. They make decisions collectively and perform better together, thereby improving patient safety.Reference Edmondson73, Reference Riskin, Erez and Foulk164 In a healthcare setting, psychological safety enables learning, experimentation, and the production of new practicesReference Edmondson73 – factors that have been shown to reduce patient mortality rates.Reference Tucker, Nembhard and Edmondson94, Reference Nembhard and Tucker165 Linked to this, it is important to recognise how problems of quality and safety are identified, defined, and selected for attention, by whom, through which power structures, and with what consequences – and how the exclusion of some healthcare workers from these processes may be hampering improvements in care for patients.Reference Maben and Engaging166
The question of how to create conditions that will enable healthcare improvement – rather than it being seen as an add-on or becoming one more activity that is left undone due to time pressures – connects with themes about embedding strategies for quality in the culture of an organisation (as described in the Element on making culture change happenReference Mannion, Dixon-Woods, Brown and Marjanovic167). Organisations also need to grasp the relationships between workplace conditions and improvement and that these relationships potentially work in both directions: good workplace conditions enable improvement, but improvement work (and enabling staff to engage in it) may create system efficiencies that then improve workplace conditions, thereby enabling better staff well-being, greater psychological safety, and optimum staffing, which results in a reduction of the workload burden on staff.
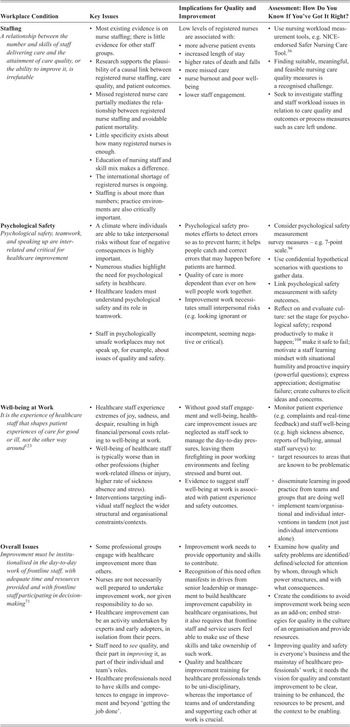
We conclude by drawing together the main themes and insights from all sections (see Table 1) to inform organisations’ thinking about how best to create the necessary conditions to capitalise on their most valuable asset in pursuit of improvement in healthcare: their people.
Table 1 Workplace conditions and healthcare improvement
| Workplace Condition | Key Issues | Implications for Quality and Improvement | Assessment: How Do You Know If You’ve Got It Right? |
|---|---|---|---|
|
| Low levels of registered nurses are associated with:
|
|
|
|
|
|
|
|
|
|
|
|
|
|
5.2 A Future Research Agenda
Despite the significance of the workforce and people dimensions of quality and safety and their centrality as structural conditions, the healthcare improvement literature has to date paid insufficient attention to the three conditions we have outlined in this Element – staffing adequacy, psychological safety, and staff well-being. In Box 10, we identify what might be done to address the gaps in the literature.
Box 10 Future research recommendations
Research on the Interaction between the Three Preconditions and Improvement
Develop and fund longitudinal, multidisciplinary research programmes that examine the impact of staffing adequacy, psychological safety, and staff well-being on healthcare improvement – individually and collectively. Specifically, develop and fund studies that:
investigate the role of emotion work in the development and implementation of improvement work
focus on increasing workforce capacity for improving care by clarifying the staff time and skills required
explore the value of a richer skill mix for optimal improvement work
explore the role of psychological safety (the impact of speak-up cultures and bullying and incivility, for example) in enabling improvement
tease out how the three preconditions together impact on the successful implementation of improvement interventions
evaluate the impact of healthcare improvement on staff well-being at work (e.g. on stress, burnout, engagement, morale, and motivation) and the potential workforce benefits (increased job satisfaction and retention).
Research to Address Each of the Three Preconditions
Specifically, staffing research should include:
more longitudinal staffing research, examining a range of different professional groups
further staffing research studies outside acute general hospital wards
better economic analyses in relation to staffing and outcomes (to identify the cost benefits of better staffing)
system changes in the measurement of outcomes associated with care (better metrics)
more workforce research that examines the full multidisciplinary team including the medical workforce.
Specifically, psychological safety research should include:
research on the effects of interventions designed to increase psychological safety
more research on differences in psychological safety across role groups and organisational levels in healthcare organisations
studies of changes in psychological safety as a result of changes in workload, staffing levels, burnout, or crisis.
Specifically, well-being research should include:
clearer definitions of healthcare staff well-being
more and better evaluation of interventions that support staff well-being
research outside of acute care – for example, in primary care settings
studies capable of determining causality between concepts.
6 Further Reading
Staffing for Quality
Griffiths et al.Reference Griffiths, Ball and Drennan15 – a systematic review of the evidence on staffing levels and skill mix, which was commissioned by NICE to help inform the development of safe-staffing guidelines for adult inpatient care. Only studies that measured staffing at a unit level and considered both registered nurse and support worker staffing were included.
BallReference Ball168 – a special collection editorial weaving together different perspectives on the question of whether we have enough nurses, why the question matters, and disincentives to addressing it.
Maben et al.Reference Maben, Morrow, Ball, Robert and Griffiths64 – a review commissioned by the Chief Nursing Officer for England, recognising that measurement lies at the heart of efforts to improve care quality and meaningful metrics are key to this.
National Institute for Health Research (NIHR)169 – a review summarising evidence from 22 research studies (funded by the NIHR) on planning nurse staffing, skill mix, and the organisation of nursing on hospital wards, with a concise overview of lessons learnt.
Department of Health, Ireland67 – a rare example of a framework for safe nurse staffing that includes reference to the cost and investment needed to enable an overall increase in staffing, and also sets out the expected return/benefits on this investment.
Psychological Safety
EdmondsonReference Edmondson108 – a definitive guide to understanding psychological safety, why it matters in the modern workplace, and how to create more of it. Includes a review of the research literature, more than 20 case studies to bring the ideas to life, and practical tips.
EdmondsonReference Edmondson170 – a book focusing on ‘teaming’ as a set of coordinating and collaborating behaviours, rather than examining teams as structures. It explains that most teams in today’s workplace, especially in healthcare, lack stable, well-bounded membership and provides tips for how to foster effective teaming.
Burns et al. (editors)Reference Burns, Bradley and Weiner171 – the seventh edition of Shortell and Kaluzny’s textbook includes more than a dozen literature reviews and case studies on critical topics to help today’s healthcare managers understand and support success in the modern healthcare delivery ecosystem.
Staff Health and Well-being
BoormanReference Boorman112 – a comprehensive and seminal review of the well-being of healthcare staff, providing a succinct review of the evidence and a strategy for improving NHS staff well-being at work.
Brand et al.Reference Brand, Thompson Coon and Fleming118 – a systematic review of the health and well-being of healthcare workers, advocating for a whole-system (as opposed to an individual) approach to intervention development.
Health Education England111 – an accessible report from a commission that was set up to examine staff and learner well-being in the NHS. It includes an evidence review and testimonies from staff and families of NHS staff bereaved by suicide.
Taylor et al.Reference Taylor, Xyrichis, Leamy, Reynolds and Maben124 – a systematic review of the evidence supporting Schwartz Rounds and a scoping review comparing Rounds to other well-being interventions that use reflection on practice as a process for support.
All authors of this Element were involved in the conceptualisation, curation of included materials, and writing of the original draft, as well as reviewing and editing. Jill Maben drafted the introduction, discussion, and wrote the section on staff well-being, and coordinated the preparation of the manuscript. Jane Ball wrote the section on staffing, and Amy C. Edmondson wrote the section on psychological safety. Jane Ball and Amy C. Edmondson contributed to the review and revisions of the original drafts, providing critical comments and edits. All authors have approved the final version.
Conflicts of Interest
Jill Maben was a member of an advisory group in 2006–09, advising on the development of the Point of Care project at The King’s Fund, and a member of the Point of Care Foundation Board in 2013–14; she stepped down as board member at the start of the Schwartz Rounds evaluation. Jill Maben was also a member of the Engagement and Involvement Advisory Board of THIS Institute (The Healthcare Improvement Studies Institute) during 2019–22. Jane Ball and Amy C. Edmondson have no conflict of interests to declare.
Acknowledgements
We thank Dr Ruth Abrams for some early insights in the staff well-being evidence base, Sara Nicholson for retrieving papers and providing administrative support for Amy C. Edmondson, Susan Salter for editing support and text refinement, and the peer reviewers for their insightful comments and recommendations to improve the Element. A list of peer reviewers is published at www.cambridge.org/IQ-peer-reviewers.
Funding
This Element was funded by THIS Institute (www.thisinstitute.cam.ac.uk). THIS Institute is strengthening the evidence base for improving the quality and safety of healthcare. THIS Institute is supported by a grant to the University of Cambridge from the Health Foundation – an independent charity committed to bringing about better health and healthcare for people in the UK.
About the Authors
Jill Maben is Professor of Health Services Research and Nursing at the University of Surrey. Jill is a nurse and social scientist and her research focuses on the psychological well-being of staff at work to support them to care well for patients.
Jane Ball is Professor of Nursing Workforce Policy at the University of Southampton. Jane has been researching nurse staffing and workforce policy since 1990. A major interest is nurse staffing levels and the interface between research evidence and policy development.
Amy C. Edmondson, the Novartis Professor of Leadership and Management at Harvard Business School, studies psychological safety and teaming in healthcare delivery and other organisations.
The online version of this work is published under a Creative Commons licence called CC-BY-NC-ND 4.0 (https://creativecommons.org/licenses/by-nc-nd/4.0). It means that you’re free to reuse this work. In fact, we encourage it. We just ask that you acknowledge THIS Institute as the creator, you don’t distribute a modified version without our permission, and you don’t sell it or use it for any activity that generates revenue without our permission. Ultimately, we want our work to have impact. So if you’ve got a use in mind but you’re not sure it’s allowed, just ask us at [email protected].
The printed version is subject to statutory exceptions and to the provisions of relevant licensing agreements, so you will need written permission from Cambridge University Press to reproduce any part of it.
All versions of this work may contain content reproduced under licence from third parties. You must obtain permission to reproduce this content from these third parties directly.
Editors-in-Chief
Mary Dixon-Woods
THIS Institute (The Healthcare Improvement Studies Institute)
Mary is Director of THIS Institute and is the Health Foundation Professor of Healthcare Improvement Studies in the Department of Public Health and Primary Care at the University of Cambridge. Mary leads a programme of research focused on healthcare improvement, healthcare ethics, and methodological innovation in studying healthcare.
Graham Martin
THIS Institute (The Healthcare Improvement Studies Institute)
Graham is Director of Research at THIS Institute, leading applied research programmes and contributing to the institute’s strategy and development. His research interests are in the organisation and delivery of healthcare, and particularly the role of professionals, managers, and patients and the public in efforts at organisational change.
Executive Editor
Katrina Brown
THIS Institute (The Healthcare Improvement Studies Institute)
Katrina is Communications Manager at THIS Institute, providing editorial expertise to maximise the impact of THIS Institute’s research findings. She managed the project to produce the series.
Editorial Team
Sonja Marjanovic
RAND Europe
Sonja is Director of RAND Europe’s healthcare innovation, industry, and policy research. Her work provides decision-makers with evidence and insights to support innovation and improvement in healthcare systems, and to support the translation of innovation into societal benefits for healthcare services and population health.
Tom Ling
RAND Europe
Tom is Head of Evaluation at RAND Europe and President of the European Evaluation Society, leading evaluations and applied research focused on the key challenges facing health services. His current health portfolio includes evaluations of the innovation landscape, quality improvement, communities of practice, patient flow, and service transformation.
Ellen Perry
THIS Institute (The Healthcare Improvement Studies Institute)
Ellen supported the production of the series during 2020–21.
About the Series
The past decade has seen enormous growth in both activity and research on improvement in healthcare. This series offers a comprehensive and authoritative set of overviews of the different improvement approaches available, exploring the thinking behind them, examining evidence for each approach, and identifying areas of debate.