1 Introduction
Governance and leadership play a key role in delivering high-quality, safe care. In this Element, we set out what is meant by governance and leadership, discussing the way thinking has developed over time. We describe the role of governance and leadership in quality and safety at different levels, from the team or individual level to national policy. We discuss board governance, performance management, the influence of leadership on improvement efforts, and team-based leadership. Finally, we draw out lessons for practice, policy, and research, noting particular strengths and weaknesses in the evidence and what this means for governing and leading for quality and safety in healthcare settings in the future.
2 Why Are Governance and Leadership Important to Healthcare Quality and Safety?
We begin by outlining the role of governance and leadership in quality and safety (Section 2.1) and show that they can operate at multiple levels (Section 2.2), before we then go on to examine how governance and leadership might be defined and explain how thinking has evolved over time (Section 3).
2.1 The Role of Governance and Leadership in Quality and Safety
The central role played by governance and leadership in the actions (and inactions) relating to quality of care and patient safety has been repeatedly identified by inquiries and investigations into major organisational failures.Reference Brown, Dickinson and Kelaher1 For instance, the 2002 inquiry into paediatric heart surgery at Bristol Royal Infirmary in the 1980s and 1990sReference Kennedy2 (also discussed in the Elements on statistical process controlReference Mohammed, Dixon-Woods, Brown and Marjanovic3 and making culture change happenReference Mannion, Dixon-Woods, Brown and Marjanovic4) identified that there had been insufficient prioritisation and monitoring of quality, as well as a culture that failed to acknowledge problems. The recommendations of the Bristol inquiry were a key driver for the subsequent development of clinical governance (‘inter‐related activities aimed at improving the quality and safety of health care’Reference Travaglia, Debono, Spigelman and Braithwaite5), which remains an important component of healthcare quality in the UK National Health Service (NHS).Reference Brown, Dickinson and Kelaher1,Reference Kennedy2,Reference Travaglia, Debono, Spigelman and Braithwaite5–7
Despite efforts to improve care after the Bristol inquiry, problems have recurred. Investigations into higher-than-expected death rates at Mid Staffordshire NHS Foundation Trust in the late 2000s identified multiple failures of governance and leadership throughout the organisation and the wider system. These included the failure to monitor and enforce standards, insufficient transparency and involvement of patients and the public, and gaps in regional and national leadership.Reference Brown, Dickinson and Kelaher1,Reference Francis8,Reference Francis9 More recently (2015), an investigation into serious incidents in Morecambe Bay maternity services found that poor processes for learning from adverse events, deficient clinical skills, and inadequate teamworking contributed to the organisation’s failure to maintain standards, which in turn resulted in serious incidents, including the deaths of mothers and babies.Reference Kirkup10
These inquiries and other investigations have consistently identified that organisational and system failures result from a combination of many interrelated factors. They also show that governance and leadership – through their influence on priorities, oversight, and management and culture – are often part of both problem and solution.
2.2 Governance and Leadership at Macro, Meso, and Micro Levels
Governance and leadership of healthcare operate at several levels. Here, we distinguish between macro (national), meso (organisational), and micro (team or individual) levels (see Figure 1).Reference Fulop and Ramsay11,Reference Ferlie, Baeza, Addicott and Mistry12
In some systems, macro-level governance sets overarching direction and priorities for quality and safety (e.g. national recommendations), and may feature a variety of bodies serving different functions, including regulatory roles.Reference Francis9,Reference Kirkup10,13
At the meso level, organisations develop and implement strategies aimed at delivering high-quality, safe care to the populations they serve.
Finally, at the micro level, frontline staff deliver this care.
These layers are heavily intertwined, with many points where different levels of governance and leadership interact. For example, at the macro (national/regional) level, a range of bodies may set policies, issue guidance, allocate resources, and operate incentives. Regulators may set standards and put mechanisms in place to oversee them and take action where needed.Reference Walshe14 At the meso (organisational) level, board governance may seek both to influence upwards into national priorities and to influence within their own organisations, and to bridge national drivers and frontline activity.Reference Ferlie, Baeza, Addicott and Mistry12,Reference Lipunga, Tchereni and Bakuwa15 Understanding the interactions between these macro, meso, and micro levels is an important part of understanding how the quality and safety of care can be maintained and improved. In Figure 1, we describe these levels, some key processes, and where the examples selected for discussion in this Element sit in relation to these levels.
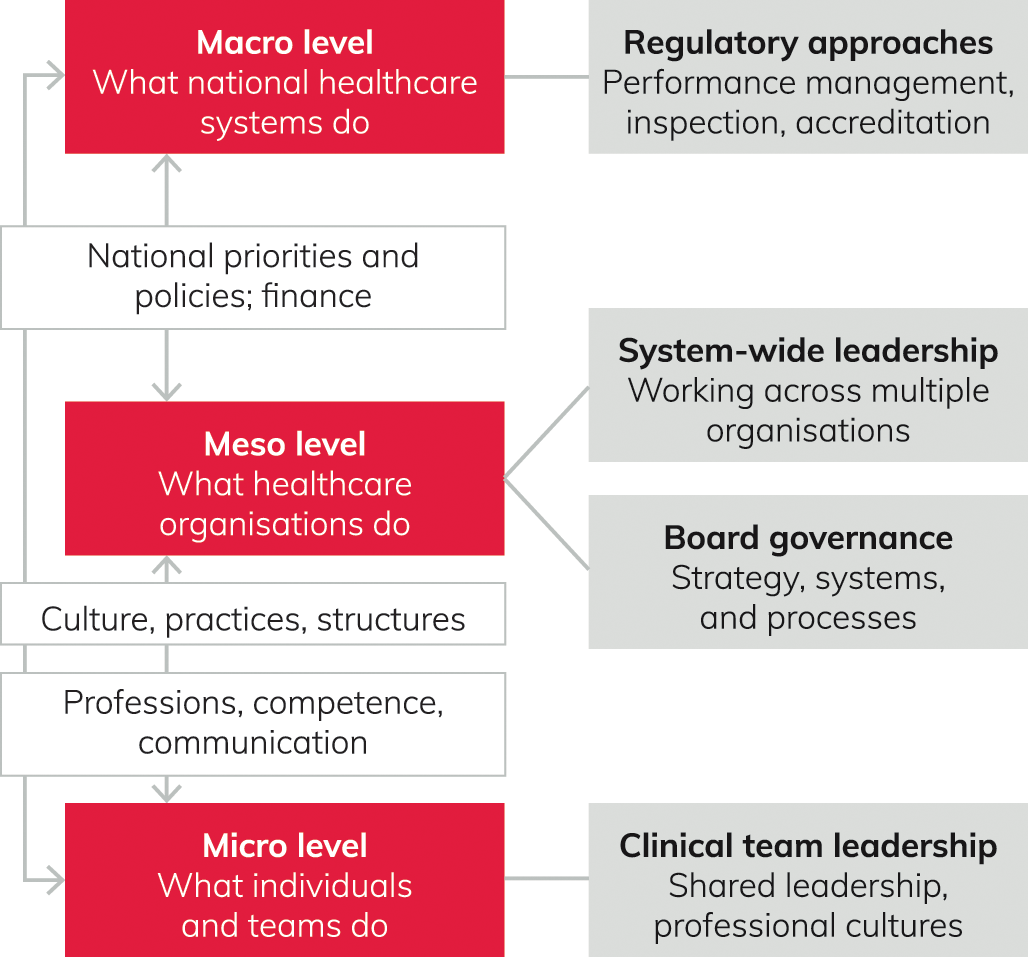
Figure 1 Governance at macro, meso, and micro levels with reference to examples discussed in this Element The figure draws on work by Fulop and Ramsay.Reference Fulop and Ramsay11
3 A Brief History
This section will discuss how thinking about governance and leadership has changed over time. It begins by setting out how the concepts have been defined, and the relationship between the two concepts. It then addresses how thinking about governance and leadership has evolved over the twentieth century to today.
3.1 What Is Meant by Governance and Leadership?
Governance and leadership are overlapping concepts with a complex relationship. Governance has been described as an ‘elusive concept to define’.Reference Barbazza and Tello16 The term derives from Latin words for ‘to steer’ or ‘give direction’.Reference Cornforth and Chambers17 Its current meaning might be explained as follows:
the means for achieving direction, control, and coordination of wholly or partially autonomous individuals or organisational units on behalf of interests to which they jointly contributeReference Lynn, Heinrich and Hill18
ways in which organisations and the people working in them relate to each otherReference Davies, Anand and Artigas19
a set of processes (customs, policies, or laws) that are formally or informally applied to distribute responsibility or accountability among actors of a given [health] system.Reference Barbazza and Tello16
Therefore, governance may be seen in terms of the structures and processes that enable oversight, monitoring, and accountability within that system; but it is also important to note that any formal processes and structures may be shaped by (and should accommodate) the informal interactions between people operating within that system.
Leadership also tends to attract multiple definitions, but it can perhaps be summarised in terms of processes by which individuals or groups are enabled, encouraged, or inspired to achieve agreed goals within a given context. A common theme across various definitions is ‘mobilising individuals, organisations and networks to formulate and/or enact purposes, values and actions which aim or claim to create valued outcomes for the public sphere’.Reference Hartley20
There are important overlaps between the concepts of governance and leadership, for example, in terms of the aim to influence how people operate within a system or service. However, while the concepts overlap, they play different (yet interlinked) roles. That is, governance is a system that enables oversight, monitoring, and accountability of the processes and people operating within it; leadership may be seen as a key component of a governance system, acting both to influence and facilitate that system (e.g. shaping strategic vision and objectives, and enabling engagement with system processes).
3.2 How Has Thinking about Governance Changed?
Approaches to and thinking about governance in healthcare changed during the twentieth century and into the twenty-first century, reflecting broader social and political changes.Reference Davies, Anand and Artigas19 Traditionally, some healthcare professionals (e.g. doctors) operated forms of professional self-governance, in that they worked independently to deliver care while also gaining direction through their peer networks – for example, via the General Medical Council, established to regulate doctors in 1858,Reference Irvine21 and the General Nursing Council, established in 1919.Reference Bradshaw22
Bureaucratic hierarchies emerged in the early to mid-twentieth century, characterised by a centralised authority implementing structures and rules in order to exert influence across the entire system. A key example was the hierarchical command and control approach of the NHS from its post-war inception. This system was led by a minister of government and the state department (the current equivalents being the Secretary of State for Health and Social Care and the Department of Health and Social Care, respectively) exerting influence through layers of authority all the way through to frontline delivery of care. The approach reflected the big government thinking that shaped the welfare state in the UK in the mid-twentieth century; it was embodied in the suggestion of Nye Bevan, the minister who oversaw the creation of the NHS, that ‘when a bedpan is dropped on a hospital floor its noise should resound in the Palace of Westminster’.Reference Exworthy, Powell and Mohan23
The command and control approach to running the NHS broadly continued until the 1980s when many nations, including the UK, parts of mainland Europe, and New Zealand, began to adopt principles of market forces. This so-called new public management approach has been associated with the emergence of the ‘new right’ (e.g. the conservative movements led by Margaret Thatcher in the UK and Ronald Reagan in the USA in the 1980s). Drawing on private sector thinking to reshape approaches to running public services, including healthcare,Reference Ferlie and Aldag24 common features included:
reduced centralised, hierarchical control accompanied by more corporate approaches to governance and management were introduced (e.g. introducing board governance)
a purchaser–provider split and competitive tendering to deliver services
a move from professional self-regulation to external audit and regulatory governance.Reference Ferlie and Aldag24
Policy-makers anticipated that these changes would lead to greater entrepreneurialism and better quality care.Reference Exworthy, Powell and Mohan23 In practice, however, some research suggests that the shift to new public management may have been associated with reduced professional engagement, local democratic influence, and creative central policy-making, as well as depleting local capacity to balance long-term and short-term priorities.Reference Ferlie and Aldag24
Since the early 2000s, the concept of network governance has grown in prominence as a possible way of enhancing collaboration between organisations while also engaging more effectively with a wider range of stakeholders, including the public, the voluntary sector, and frontline staff.Reference Davies, Anand and Artigas19,Reference Provan and Kenis25,Reference Caffrey, Ferlie and McKevitt26 It may take a variety of forms,Reference Provan and Kenis25 with an important example the introduction of managed clinical networks for cancer services, which sought to assist in delivering the NHS national cancer plan.Reference Addicott, McGivern and Ferlie27–Reference Ferlie, McGivern and Fitzgerald29
In practice, many health systems do not reflect different forms of governance in a pure sense, but rather in combination. For example, the current English NHS is characterised by overlapping features of markets (e.g. the purchaser–provider split) and network governance.Reference Provan and Kenis25 At the same time, bureaucratic governance (e.g. the enduring hierarchical influence of the Department of Health and Social Care and NHS England and ImprovementReference Davies, Anand and Artigas19,Reference Osipovič, Allen, Sanderson, Moran and Checkland30) and external regulation (e.g. operated by bodies such as the Care Quality Commission [CQC] and professional regulatorsReference Osipovič, Allen, Sanderson, Moran and Checkland30–Reference Beaussier, Demeritt, Griffiths and Rothstein32) are both highly consequential for the ways in which organisations providing care design and operate their own systems for governance and their leadership behaviours.
3.3 How Has Thinking about Leadership Changed?
Traditionally, thinking around leadership focused on the idea of born leaders and explored how individuals drew on their inherent qualities to lead others – the heroic leadership model.Reference Stogdill33,Reference Wood34 Over the course of the last century, the focus shifted to characteristics commonly possessed by leaders (known as trait theory), and how leaders acted (behavioural theory). Contingency theory, which emerged in the 1950s, moved the focus to the relationship between leaders, their actions, and the organisational and wider contexts in which they operate.Reference Kumar35 Since the 2000s, research has increasingly addressed how leadership accommodates complexity within teams, organisations, and the wider system.Reference Belrhiti, Giralt and Marchal36,Reference Plsek and Wilson37 That is, individuals, groups, or organisations within a given setting may hold different and sometimes competing priorities, even when they are working towards a shared goal of improving quality and safety of care.
Researchers have also drawn a distinction between leadership strategies: ‘transactional’ strategies involve use of rewards and punishment to motivate, whereas ‘transformational’ strategies involve use of charisma, challenge, and individual focus to win others’ trust and emotional buy-in to drive improvements.Reference Hartley and Benington38 Further, there has been a shift in perception from leader as commander to leader as engager, where leaders stimulate more collective approaches to leading on improvement.Reference Reichenpfader, Carlfjord and Nilsen39
Understanding of who it is that leads has also changed over time. At micro-service level, different staff groups have traditionally held different leadership responsibilities. For example, doctors tended to hold greater autonomy to influence practice and guide improvement than nurses.Reference Øvretveit40 But with the development of new public management in the 1980s, power shifted from professionals to managers as boards came to set priorities and facilitate improvement.Reference Ferlie and Aldag24 This seminal change was initially prompted by the Griffiths review into NHS management (1983), which reported that the NHS was unclear on objectives, performance, and quality, with little sense of who was in charge.Reference Griffiths41–Reference Gorsky43 However, there is now growing recognition of the value of having a strong clinical voice in senior management.Reference Vindrola-Padros44,Reference Jones, Pomeroy and Robert45 This has led to development of ‘hybrid’ leaders who combine clinical and managerial roles and so may influence improvement both formally and informally.Reference Waring46,Reference Currie, Burgess and Hayton47
There have also been attempts to move beyond models of heroic individuals to consider models of shared leadership.Reference Øvretveit40,Reference Currie and Lockett48 ‘Distributed’, ‘shared’, or ‘collective’ leadership proposes that leadership does not sit with one individual; rather, it encompasses anyone in an organisation or system who has a role in leading or managing activity – this includes middle management and frontline staff.Reference Currie and Lockett48–Reference Best, Greenhalgh and Lewis51 There is some evidence that high-performing healthcare organisations and clinical teams are more likely to feature aspects of shared leadership, while also retaining clear strategic direction from the top.Reference Baker52,Reference Aufegger, Shariq, Bicknell, Ashrafian and Darzi53 However, as we discuss later (Section 5.1), the effectiveness of distributed leadership may be influenced by context; for example, there are likely to be particular challenges when attempting to implement distributed leadership across complex systems that cover multiple organisations and sectors.Reference Currie and Lockett48,Reference Currie and Spyridonidis54
4 Approaches in Action
In this section, we present evidence on how governance and leadership influence quality and safety. While we discuss evidence on governance and leadership separately, the two issues are closely intertwined. Section 4.1 describes how aspects of governance influence quality and safety. Sections 4.2 and 4.3 explore how board governance helps improve quality and safety, and the relationship between performance measurement, performance management, and regulation. Section 4.4 discusses leadership’s contributions to quality and safety at macro, meso, and micro levels. Sections 4.5 and 4.6 illustrate these relationships in terms of leading major system change and how team leadership influences quality and safety.
4.1 How Does Governance Influence Quality and Safety?
The challenge of steering organisations and individuals to improve quality and safety can be framed in a number of ways.Reference Aufegger, Shariq, Bicknell, Ashrafian and Darzi53 For example, agency theory suggests the task is to develop systems and processes that manage individuals’ self-interest,Reference Aufegger, Shariq, Bicknell, Ashrafian and Darzi53–Reference Bennington56 whereas stewardship theory assumes individuals are all working towards the same goal and that the task of governance is more facilitative.Reference Aufegger, Shariq, Bicknell, Ashrafian and Darzi53,Reference Bennington56,Reference Eeckloo, Delesie and Vleugels57 But whatever the conceptual model, governance typically involves setting strategy, ensuring accountability, and fostering an appropriate culture,Reference Bennington56,Reference Chambers, Harvey, Mannion, Bond and Marshall58 as outlined below.
4.1.1 Setting Strategy
Setting a long-term strategy refers to an overarching plan that describes how the organisation’s values and priorities are to be achieved. It is important that strategy is linked to clear and measurable quality goals. National policies or standards at system level typically frame the context in which healthcare organisations operate and the priorities they seek to achieve.Reference Fulop and Ramsay11,Reference Thiel, Winter and Büchner59 Closer to the front line, organisational strategies for quality set the tone for staff and teams, while also framing the objectives against which performance is measured (e.g. see Section 4.2 on contributions of board governance to quality and safety).Reference Ferlie, Baeza, Addicott and Mistry12,Reference Bolden50,Reference Currie and Spyridonidis54,Reference Chambers, Harvey, Mannion, Bond and Marshall58–Reference Ramsay, Fulop, Fresko and Rubenstein60
4.1.2 Ensuring Accountability
Effective systems of accountability – monitoring and measuring performance, perhaps linked to meaningful incentives – are critical elements of governance of a quality strategy. At the macro level, such systems are visible in national regulation and inspection processes.Reference Fulop and Ramsay11,Reference Hartley20 Within organisations, boards may develop and implement local audit and clinical governance processes.Reference Gorsky43,Reference Bolden50,Reference Thiel, Winter and Büchner59,Reference Dixon-Woods, Baker and Charles61–Reference Mannion, Davies and Freeman64
4.1.3 Fostering Culture
Shaping culture (the ‘shared aspects of organisational life’Reference Mannion, Freeman, Millar and Davies65) has a vital part to play in ensuring that long-term strategies and systems of accountability can work most effectively. Cultures that explicitly prioritise characteristic features of high-quality care delivery (for example, commitment to improvement, patient experience, engagement, and teamwork) are thought to support better care.Reference Bolden50,Reference Thiel, Winter and Büchner59,Reference Parand, Dopson, Renz and Vincent66 However, a review of the evidence cautions that conventional assessments of organisational culture are often too simplistic, since organisations are often home to a multitude of cultures at the micro level. Further, the interrelationships between organisational culture and improving quality and safety are likely to be complex; for example, culture may influence different improvement activities differently, and the culture itself might be shaped by how an organisation delivers on quality.Reference Mannion, Freeman, Millar and Davies65 Further discussion of some of the issues relating to culture can be found in the Element on making culture change happen.Reference Mannion, Dixon-Woods, Brown and Marjanovic4
4.2 How Board-Level Governance Can Contribute to Improving Quality and Safety
We have already identified three important governance roles for boards: setting strategy, ensuring accountability, and fostering culture. In this section, we discuss how boards enact their governance roles to support delivery of high-quality, safe care, presenting evidence on how boards interact with both the organisations they govern and their wider context.Reference Jones, Pomeroy and Robert45,Reference Chambers, Harvey and Mannion55,Reference Ramsay, Fulop, Fresko and Rubenstein60,Reference Mannion, Davies and Freeman64,Reference Millar, Mannion, Freeman and Davies69,Reference Martin, Aveling and Campbell70
‘Board governance’ refers to the systems and processes used by senior leadership in healthcare organisations to support delivery of key organisational priorities, including high-quality, safe care.Reference Jones, Pomeroy and Robert45,Reference Chambers, Harvey and Mannion55,Reference Ramsay, Fulop, Fresko and Rubenstein60 Boards are accountable for the quality and safety of care in the organisations they lead.Reference Jones, Pomeroy and Robert45,Reference Chambers, Harvey and Mannion55,Reference Ramsay, Fulop, Fresko and Rubenstein60,Reference Freeman, Millar, Mannion and Davies71 But these are not boards’ only priorities; others include, for example, resource management, finances, innovation, population health, workforce, and equality and diversity. To govern effectively, boards must achieve an appropriate balance between all these priorities.Reference Ramsay, Fulop, Fresko and Rubenstein60,Reference Ramsay, Fulop, Fresko and Rubenstein72
What boards do and how they do it is important to the quality and safety of care that their organisations provide.Reference Brown, Dickinson and Kelaher1,Reference Jones, Pomeroy and Robert45,Reference Chambers, Harvey and Mannion55,Reference Tsai, Jha and Gawande73 Evidence from the USA and the UK suggests that boards tend to perform better on quality and safety if they make quality a strategic priority, dedicate time to discussing quality in board meetings, and establish dedicated quality committees.Reference Baker52,Reference Ramsay, Fulop, Fresko and Rubenstein60,Reference Martin, Aveling and Campbell70,Reference Jha and Epstein74,Reference Jha and Epstein75 In the following sections, we discuss some of the ways in which boards can strengthen their focus on quality.
4.2.1 Using Strategy to Drive Quality
A key role of boards is to set the strategy for the organisation they lead. Quality should be at the heart of this strategy.Reference Ramsay, Fulop, Fresko and Rubenstein60,Reference Ramsay, Fulop, Fresko and Rubenstein72 Research on boards in Australia has identified the importance of translating broad strategic statements into specific, meaningful quality objectives, since, in the absence of such statements, board members and staff struggled to discuss progress on improvement.Reference Brown76
An analysis of the approaches used by English boards to enable quality improvement (QI) used an evidence-based measure that reflected the degree to which boards prioritise, understand, engage with, and support QI – referred to as QI ‘maturity’. This study indicated the importance of both the amount of time dedicated to quality and its focus. Boards of organisations with high QI maturity spent the bulk of their time discussing quality and prioritising issues that had been escalated by the quality committee, trusting the wider governance structure to identify the issues that required attention.Reference Jones, Pomeroy and Robert45
4.2.2 Engaging Stakeholders at All Levels to Build Cultures that Prioritise Quality
Boards that are effective at leading improvement achieve it by engaging stakeholders at macro, meso, and micro levels (reflecting their accountability to different levels of the system) and translating this engagement into strategic priorities.Reference Bate, Mendel and Robert77–Reference Baker, MacIntosh-Murray and Porcellato79 Such boards seek to manage their wider environment – including regulators, payer organisations (commonly described as commissioners in the English NHS), and fellow provider organisations – in order to support region-wide responses to quality challenges. Equally, they may engage with local stakeholders to build cultures that are supportive of improvement, patient engagement, and teamwork.Reference Baker52,Reference Ramsay, Fulop, Fresko and Rubenstein60,Reference Nembhard, Cherian and Bradley80–Reference Damschroder, Aron and Keith82 For example, boards of the organisations judged to have high QI maturity were found to engage actively with stakeholders, including clinicians and patient groups, so that different stakeholders could help shape organisational priorities for quality.Reference Jones, Pomeroy and Robert45
4.2.3 Using Data to Ensure Accountability and Drive Improvement
Boards that are successful in focusing on quality make use of data to drive improvement, rather than just for external assurance.Reference Jones, Pomeroy and Robert45,Reference Dixon-Woods, Baker and Charles61 They do this by clearly defining what is meant by quality and endorsing its associated measures. They create and regularly review a quality monitoring framework, analyse performance against benchmarks over time to identify areas of improvement, and assess progress on areas of concern.Reference Brown, Dickinson and Kelaher1,Reference Jones, Pomeroy and Robert45 Drawing on a combination of hard quantitative data on performance and soft data (e.g. discussions with clinicians or patients, or walk-arounds by senior management) has been found to help boards understand the realities of quality and safety on the ground and to help make a compelling case for improvement.Reference Jones, Pomeroy and Robert45,Reference Mannion, Davies and Freeman64,Reference Tsai, Jha and Gawande73,Reference Dixon-Woods, McNicol and Martin83,Reference Martin, McKee and Dixon-Woods84
4.2.4 Communication and Information to Support Understanding and Prioritisation of Quality
Effective communication about quality at board level – for example, presenting clear narratives on quality while being open to questioning and challenge – can help offer board members the space to reflect on the reasons for any quality and safety issues, and potential solutions.Reference Brown85 Also important is the capacity to use, interpret, and act on available data. Boards of Australian organisations with low engagement with quality described themselves as ‘drowning in data’,Reference Jones, Pomeroy and Robert45 while English boards with low QI maturity received data that made it ‘hard to see the wood from the trees’.Reference Brown85 Boards with high QI maturity, on the other hand, outlined the use of benchmarks linked directly with improvement prioritiesReference Jones, Pomeroy and Robert45 and managers created a logical narrative through the data, thereby facilitating rapid understanding and better engagement from board members.Reference Brown85 Boards with high QI maturity highlighted the advantages of effective challenge (e.g. questioning assumptions behind analyses and actions) in creating a wider understanding of quality issues across the board.Reference Jones, Pomeroy and Robert45,Reference Brown85 They also set in place communication systems that aimed to support shared understanding of quality issues across departments and professions at every level.Reference Jones, Pomeroy and Robert45,78,Reference Curry, Spatz and Cherlin86
4.2.5 What Helps Boards Govern for Quality?
Boards can be helped to carry out their governance roles by ensuring they have the appropriate membership and that board members continue to develop their capabilities in relation to quality. Board membership needs to be sufficiently large and sufficiently diverse to provide the necessary expertise to govern complex healthcare organisations.Reference Ramsay, Fulop, Fresko and Rubenstein60,Reference Mannion, Davies and Freeman64 For instance, research on healthcare organisations in the UK, USA, and elsewhere suggests that a higher proportion of doctors on boards has been associated with better performance on quality ratings and patient outcomes.Reference Veronesi, Kirkpatrick and Vallascas87–Reference Sarto, Veronesi and Kirkpatrick89 This may be because clinicians offer greater understanding of quality and safety, and communicate more effectively with clinical staff.Reference Millar, Mannion, Freeman and Davies69,Reference Veronesi, Kirkpatrick and Vallascas87,Reference Sarto and Veronesi88 However, how these clinicians behave also matters: boards with high QI maturity included clinicians who were assertive and vocal on matters of quality; less mature organisations had fewer such members.Reference Jones, Pomeroy and Robert45 The balance of executive management and non-executive (lay) members is also important.Reference Ramsay, Fulop, Fresko and Rubenstein72 Non-executives, ideally with expertise in quality and safety, provide a valuable perspective in scrutinising performance – challenging senior management on quality and safety and how they are balanced against other organisational priorities.Reference Chambers, Harvey and Mannion55
Boards that address quality effectively prioritise learning and development.Reference Nembhard, Cherian and Bradley80,Reference Burnett, Mendel and Nunes81,Reference Dixon-Woods, McNicol and Martin83,Reference Braithwaite90 They learn from external examples of good practice to drive initial improvement, then analyse local problem-solving to develop tailored improvement strategies.Reference Jones, Pomeroy and Robert45,Reference Nembhard, Cherian and Bradley80 Members of these boards are also more likely to have undergone formal QI training – for example, on what quality means and relevant improvement techniques, including investigation (e.g. root cause analysis) and improvement approaches (e.g. plan-do-study-act cycles).Reference Jones, Pomeroy and Robert45 Board-level improvement tools can support the development of effective organisational QI strategies and at a relatively low cost, but support from senior board members is necessary for such interventions to have optimal impact.Reference Barbosa, Jones and Pomeroy91
4.3 The Role of Performance Measurement and Performance Management in Improving Quality and Safety
In this section, we discuss how performance measurement and performance management have been used in an effort to strengthen accountability for healthcare quality and safety.Reference Ferlie, Baeza, Addicott and Mistry12,Reference Mannion and Braithwaite92–Reference Bevan and Hood94 Internationally, demand for accountability for healthcare quality and safety is growing.Reference Busse, Klazinga, Panteli and Quentin95 Performance measurement (judging how a service performs against targets) has increased in prominence as a tool of accountability in health and other sectors since the late 1970s, with the first national performance indicators implemented in the NHS in 1983.Reference Pollitt96 Alongside this, performance management (the techniques and approaches used to create or shape performance) has also become more prominent.Reference Pollitt96
Performance measurement and performance management differ in important ways. Measurement involves collecting and comparing data on how organisations are doing – for instance, in complying with quality standards (e.g. in a national audit) or on delivery of outcomes (e.g. infection or mortality rates). By contrast, performance management entails an active response to measurement of how organisations are doing in order to drive improved performance.Reference Lebas97 For instance, many health systems, including in the USA (Medicare), the EU, and the UK, incentivise provision of high-quality, safe care.Reference Brown, Dickinson and Kelaher1,Reference Busse, Klazinga, Panteli and Quentin95
We now discuss how different aspects of performance measurement and management influence quality and safety, and some associated pitfalls.
4.3.1 Performance Measurement
Performance measures may help communicate priorities, while targets seek to define what constitutes good and bad levels of performance on a given measure.Reference Bevan and Hood94,Reference Pollitt96 Targets may support significant improvements in processes associated with quality of care. For instance, the introduction of national targets and monitoring for healthcare-associated infection (such as methicillin-resistant Staphylococcus aureus [MRSA] and Clostridium difficile) was associated with an increase in hospitals’ governance and improvement activity on this issue.Reference Ramsay, Magnusson and Fulop98 Similarly, national thresholds for time taken to see patients were associated with pronounced reductions in patient waiting times.Reference Boyne and Chen99,Reference Kelman and Friedman100
However, targets can have several downsides. They may lead to box-ticking, where staff do enough to achieve the target in ways that do not reflect its spirit. For example, in response to a 5-minute waiting-time target intended to encourage rapid patient triage in emergency rooms, hospitals introduced ‘hello nurses’ who greeted patients quickly but did little else. So the target was met but without achieving the intended benefit.Reference Mannion and Braithwaite92 A further potential downside in target-driven regimes is that what is measured becomes what matters. This may mean that important but harder-to-measure aspects of care (such as the humanity of care) are overlooked.
Sometimes target-setting may thwart the goals it is intended to serve or cause confusion of purpose. For example, error reporting has an important role to play in understanding patient safety, but the message it presents is complex, as a higher number of reported errors may reflect a stronger focus on patient safety.Reference Reason101–Reference Braithwaite, Westbrook, Travaglia and Hughes103 This challenge can be observed in the context of medication errors, which are substantially under-reported; this makes it difficult to set a target to reduce error, which in turn may have contributed to reduced focus on governing this important safety issue.Reference Ramsay, Magnusson and Fulop98
The range of techniques used to assess performance is wide, and each can have positive and negative effects: there is no single right answer. For example, self-measurement – where an organisation or service measures and reports its own performance – can be performed rapidly but runs the risk of ‘fiddling’ the figures (distorting or even falsifying data).Reference Mannion and Braithwaite92,Reference Pollitt96
4.3.2 Responses to Performance Management
Responses to performance management are mixed. For example, publishing performance data and incentivising performance through financial penalties or rewards (as described in Box 1) can help to drive improvements in quality and safety.Reference Campanella, Vukovic and Parente104 But they can also have unintended consequences. One consequence of performance management is that it can reduce the ‘slack’ – the space to think and act – available to boards, thereby limiting their capacity to develop their improvement strategies.Reference Jones, Pomeroy and Robert105 Other examples include reduced appetite to take on high-risk casesReference Behrendt and Groene106,Reference Williams, Modgil, Drake and Keeley107 and increased risk of gaming targets, such as ratchet effects, where services seek to improve only slightly on the previous year’s performance (e.g. on waiting times), permitting a perception of ongoing progress at the expense of the patients who might benefit from larger and more immediate improvements in quality.Reference Mannion and Braithwaite92,Reference Bevan and Hood94,Reference Pollitt96
Box 1 Financial incentives for performance
The relationship between financial incentives and performance has been explored in several studies. Research on hospitals in north-west England found that while pay for performance was associated with initial reductions in patient mortality,Reference Sutton, Nikolova and Boaden108 this effect was not sustained long term.Reference Kristensen, Meacock and Turner109 Research on US hospitals has also indicated no significant effect of financial incentives on patient mortality,Reference Jha, Joynt, Orav and Epstein110 and research on payment for performance in primary care in England has reported similarly limited effect on quality and outcomes of care.Reference Ryan, Krinsky, Kontopantelis and Doran111,Reference Harrison, Dusheiko and Sutton112 A review of qualitative research on primary care in England suggests that while pay for performance activity fitted well with clinicians’ desire for personal success, it clashed with their prioritisation of self-direction, benevolence, and creativity; the review recommended that gaining clinicians’ acceptance of any definition of ‘high-quality care’ would be key to achieving greater engagement with such schemes.Reference Khan, Rudoler, McDiarmid and Peckham113
4.4 How Does Leadership Influence Quality and Safety?
Given that its goals include influencing and mobilising, leadership has the potential to encourage and facilitate improvement (and the cultures associated with improvement) at every level.
At the macro level, leadership sets the tone for a whole system, framing national and regional priorities, driving engagement in systems of accountability, and encouraging intraregional initiatives and interregional learning.Reference Hartley20,Reference Hartley, Sancino, Bennister and Resodihardjo114
At the meso level, leadership (e.g. boards) defines the vision for an organisation and engages local staff in improvement activity, while also reaching out to external organisations to shape region-wide endeavours.Reference Øvretveit40,Reference Baker52,Reference Bennington56,Reference Ramsay, Fulop, Fresko and Rubenstein60,Reference Parand, Dopson, Renz and Vincent66
And at the micro level, frontline leadership helps ensure clinical teams work together to improve quality and safety, while responding to rapid changes in circumstance.Reference Øvretveit40,Reference Aufegger, Shariq, Bicknell, Ashrafian and Darzi53,Reference Braithwaite90
Effective leadership for quality and safety requires clear understanding of priorities, both in terms of external drivers and local issues. In order to be able to identify such issues and the appropriate responses, research suggests that leaders will benefit not only from expertise and experience in improving quality and safety,Reference Alderwick, Charles, Jones and Warburton115,Reference McKean and Snyderman116 but also the humility to recognise that change might be needed in one’s own services.Reference Vindrola-Padros44,Reference McKean and Snyderman116,Reference Kool and van Dierendonck117
Providing clarity about goals and priorities – defining and stating the purpose of action and change – is important for communicating why improvement is necessary.Reference Hartley20,Reference Øvretveit40,Reference Kempster, Jackson and Conroy118,Reference Künzle, Kolbe and Grote119 Doing so consistently and clearly may help people to understand the desirability of the prioritised action and behaviours.Reference Øvretveit40,Reference Alderwick, Charles, Jones and Warburton115,Reference McKean and Snyderman116,Reference Künzle, Kolbe and Grote119,Reference Donovan, Salmon and Lenné120
Being able to engage and enable others is a key element of leadership for quality and safety. Bringing about improvement requires commitment across a wide range of stakeholders, some of whom might not accept that change is required. Leaders therefore need to embody integrity and fairness, and take a consistent approach in order to inspire commitment to improvement. It is similarly important that both leaders and those they are leading have the capabilities and capacity to participate in such activities.Reference Øvretveit40,Reference Jones, Pomeroy and Robert45,Reference Parand, Dopson, Renz and Vincent66,Reference Braithwaite90,Reference Alderwick, Charles, Jones and Warburton115,Reference Kool and van Dierendonck117,Reference Künzle, Kolbe and Grote119
Though ‘heroic’ leadership is a discredited approach, leaders’ personal characteristics and capabilities may play a role in how effective they are at influencing others. The evidence identifies experience, technical expertise, extraversion, and conscientiousness as important characteristics.Reference Caldwell, Dixon and Floyd121 Political skill and awareness are also increasingly seen as important facilitators of leading improvement.Reference Hartley20,Reference Hartley, Sancino, Bennister and Resodihardjo114 How a leader relates to and is seen by teams is critical. The perceived status of different professional groups matters, too. Evidence from health and care settings shows that staff prefer to be led by a fellow professional, placing trust in their expertise and understanding. However, it is those from ‘higher status’ professions, such as doctors, who tend to gain leadership roles.Reference Currie and Lockett48,Reference Currie and Spyridonidis54 Traditional hierarchies in healthcare settings can make it harder for leaders from professions that have tended to be denied high status, such as nursing, to be seen as legitimate leaders.
4.5 Understanding How Leadership Influences Major System Change
In this section, we discuss how leadership influences major system change, including reorganisation of specialist care across multiple healthcare organisations at regional level.Reference Kumar35 Major system change has been linked with better care and outcomes (e.g. improvements in mortality or length of hospital stay).Reference Ramsay, Morris and Hoffman122–Reference Moran, Lecky and Bouamra127 But such change is complex, often taking many years and substantial effort to plan and implement, and it requires sustained collaboration with multiple stakeholders in contrasting situations and with conflicting priorities.Reference Best, Greenhalgh and Lewis51 System change may be controversial, prompting resistance from local leaders, clinicians, and the wider public.
As we discuss, different forms of leadership play important roles in delivering major system change, addressing both the challenges of complex change and associated resistance. Bottom-up clinical leadership can help to ensure suitably designed systems that are supported by the people who will deliver them; top-down, region-wide leadership can encourage relevant stakeholders not to withdraw from discussions in the change process. Some of the key approaches that can contribute to the success of major system change are outlined below.
4.5.1 Engaging and Collaborating with the Right Stakeholders
Leading major system change relies on engaging and working in collaboration with the right stakeholders. As major system change commonly addresses a whole patient pathway across a region, multiple different groups may contribute in different ways. For example, clinicians – including primary care, hospital specialist services, and ambulance services – are vital to ensuring services deliver appropriate care and that patients are transferred reliably.Reference Vindrola-Padros, Ramsay and Perry128–Reference Turner, Ramsay and Perry130 Major system change is also unlikely to happen unless it has backing in terms of resources and governance from payer organisations (commissioning organisations in the context of the English NHS) and senior hospital management.Reference Turner, Ramsay and Perry130 Further, major system change should reflect the needs of patients and the public; this means engaging them and their representatives, including charities and politicians. Common examples of engagement activities include consultation (e.g. through distributing public surveys about proposals and holding open meetings where members of the public may raise questions or concerns) or involving stakeholders in planning and oversight groups.Reference McKevitt, Ramsay and Perry131
Given that these different stakeholders may have competing priorities, a key leadership challenge is keeping stakeholders on board throughout the change process – from the initial agreement to change, through planning and implementation, to ongoing sustainability of the new system. A common challenge to major system change relates to concerns about the loss of local services or activity; this may come from clinicians, healthcare organisations, or local communities.
4.5.2 Combining Top-Down and Bottom-Up Approaches
Box 2 details two examples of the reorganisation of stroke services in London and Greater Manchester that provide an interesting exploration of top-down and bottom-up leadership approaches.
Box 2 Top-down and bottom-up leadership approaches in a major system change of stroke services
London’s major system change of stroke services combined top-down and bottom-up leadership. Change was led by the London Strategic Health Authority (top-down), which worked with clinical leaders (stroke and ambulance services) across the region to design the new system. Strong clinical (bottom-up) leadership shaped the objectives and design of the new services and undertook a substantial public consultation exercise. Combining top-down authority with bottom-up clinical engagement resulted in system-wide ownership of the changes, which helped to overcome local resistance to the proposals.Reference Turner, Ramsay and Perry130,Reference Fraser, Baeza and Boaz132
In contrast, Greater Manchester’s changes were mainly bottom-up, led by the local stroke network. The network was highly effective at bringing stakeholders on board. However, they hit difficulties when some local services threatened to withdraw from the change process upon learning that they might lose activity under the proposed changes. To keep these organisations on board, the network adapted the service model by altering the eligibility criteria for treatment in a specialist unit. This meant that all hospitals continued to treat some stroke patients. But although local hospitals stayed engaged, the less radical service model did not lead to significant improvements in care delivery and outcomes, as had been achieved through London’s changes.Reference Morris, Hunter and Ramsay124,Reference Fulop, Ramsay and Hunter125,Reference Turner, Ramsay and Perry130
In the absence of region-wide authority, other leadership approaches have been observed. For example, Greater Manchester centralised their stroke services further in 2015, following a long period of delay. One factor that made a difference was the introduction of top-down leadership through the launch of a region-wide board in late 2014. The new board included leaders of clinical commissioning groupsFootnote * and hospitals, and the board drove rapid system-wide agreement of changes, completed in spring 2015. This new system resulted in significant improvements in care and outcomes across the region.Reference Morris, Ramsay and Boaden123,Reference Fulop, Ramsay and Hunter125
4.5.3 Leading Implementation of a Provider Network
Provider networks – where provider organisations (e.g. NHS acute trusts) collaborate formally to deliver a particular care pathway – are another option for delivering major system change.Reference Provan and Kenis25 An example of successful leadership in implementing a provider network, London Cancer, is described in Box 3.
Box 3 Establishing a provider network to implement a major system change of specialist cancer surgical services
London Cancer, a network of provider organisations, was established to implement a major system change of specialist cancer surgical services across a geographical footprint covering a population of 3.2 million.Reference Vindrola-Padros, Ramsay and Perry128
Research on the network’s implementation of a major system change for urological and oesophagogastric cancers identified several processes that supported delivery of change. These included:
a consistent core leadership team (made up of senior clinicians with enhanced leadership skills)
sharing responsibility with clinicians and managers across different levels of the system (facilitated by experienced network managers)
engaging actively with key stakeholders.
Consistent core leadership: the chief medical officer (a clinician from a separate, non-surgical specialty) and the network board (chaired by a cancer survivor and made up of experts based outside London) led the programme. Local clinicians and managers felt the chief medical officer and network board offered strong, objective leadership, which helped enable support for the changes.
Sharing responsibility at multiple levels: for each clinical pathway that was to be centralised, a pathway lead working within that specialty was appointed. Pathway leads chaired committees whose membership comprised other local clinicians operating within that clinical pathway. Together, they were responsible for leading development and delivery of the new services, which in turn enabled greater ownership of the proposed changes within local services.
Engaging stakeholders: cancer survivors (and patient representative groups) were directly involved in governance at every level of the programme, including as members of the overall programme board and cancer pathway-specific boards. This approach improved patient engagement and facilitated wider public involvement. In addition, when new payer organisations were established (see Box 2), leaders of London Cancer engaged with them actively. This helped to ensure that the major system change process underwent appropriate scrutiny and was supported by payer organisations and providers across the local system.Reference Vindrola-Padros, Ramsay and Perry128
One critique of the leadership approaches used in major system change argues that leaders may use clinical arguments politically to sideline the voice of local (clinical and public) stakeholders who are against change.Reference Fraser, Stewart and Jones133 Equally, such critiques may underplay the extent to which this resistance is driven by professional and organisational vested interests, which may not coincide with the interests of patients and the public; an important example of this is the (understandable) desire of clinicians and managers to resist changes that might disadvantage their own services (e.g. through loss of specialist activity resulting in fewer training opportunities and loss of attractiveness to medical trainees).Reference Fulop, Ramsay and Hunter125,Reference Turner, Ramsay and Perry130,Reference Fulop, Ramsay and Vindrola-Padros134,Reference Black, Wood and Ramsay135
4.6 How Does Team Leadership Influence Quality and Safety?
Delivering safe, high-quality care relies on effective collaboration between highly specialised professionals.Reference Aufegger, Shariq, Bicknell, Ashrafian and Darzi53,Reference Smith, Fowler-Davis, Nancarrow, Ariss and Enderby136,Reference Lyubovnikova, West, Salas, Tannenbaum, Cohen and Latham137 Effective teamwork is associated with better performance on quality and safety,Reference Smith, Fowler-Davis, Nancarrow, Ariss and Enderby136–Reference West and Lyubovnikova138 including lower mortality, fewer patient safety incidents, and better staff well-being and retention.Reference Smith, Fowler-Davis, Nancarrow, Ariss and Enderby136,Reference Lyubovnikova, West, Dawson and Carter139–Reference West, Almo-Metcalfe and Dawson141 In contrast, teams that do not work well together are less likely to deliver high-quality care.Reference Dixon-Woods, Baker and Charles61,Reference Lyubovnikova, West, Salas, Tannenbaum, Cohen and Latham137,Reference Lyubovnikova, West, Dawson and Carter139 In this section, we outline how leadership works at team or micro level.Reference Austin, Demski and Callender142
Effective teams tend to have shared quality objectives; they have inclusive approaches to decision-making, information sharing, conflict management, and learning, with an underlying engaging and supportive team leadership.Reference West, Lyubovnikova, Eckert and Denis68,Reference Lyubovnikova, West, Salas, Tannenbaum, Cohen and Latham137,Reference Lyubovnikova, West, Dawson and Carter139 Leadership is frequently identified as central to fostering team cultures and behaviours that support high-quality, safe care.Reference Aufegger, Shariq, Bicknell, Ashrafian and Darzi53,Reference Smith, Fowler-Davis, Nancarrow, Ariss and Enderby136,Reference Lyubovnikova, West, Salas, Tannenbaum, Cohen and Latham137 This includes the creation of psychological safety, whereby team members feel that they can raise questions or share concerns or fears with their colleagues. (Further discussion of psychological safety can be found in the Element on workplace conditions.Reference Maben, Ball, Edmondson, Dixon-Woods, Brown and Marjanovic143)
One useful way of thinking about team leadership is to consider its focus – first on the people in the team, and second on the tasks to be achievedReference Smith and Fowler Davis144 – as discussed in the next two sections.
4.6.1 Person-Focused Leadership
Person-focused leadership involves engaging and inspiring team members to work together. To do this, leaders communicate both their vision for quality and their confidence that the team can achieve it. Leading by example – for instance, demonstrating consistent commitment to high standards – may encourage a shared approach to delivering care.Reference Smith and Fowler Davis144
Enabling shared leadership, where responsibility is distributed across team members in line with their (professional or patient-specific) expertise, is thought to be associated with more effective decision-making.Reference Aufegger, Shariq, Bicknell, Ashrafian and Darzi53,Reference Smith, Fowler-Davis, Nancarrow, Ariss and Enderby136,Reference Smith and Fowler Davis144 By focusing on team members individually, understanding their aspirations, and providing constructive feedback, leaders are able to make staff feel valued, confident, and more part of the team (see Box 4).Reference Smith and Fowler Davis144
Box 4 Person-focused team leadership in community-based care
Research on integrated community-based health and social care teams in England has shown that team leadership approaches may make important differences to how teams operate and deliver high-quality care.Reference Smith, Fowler-Davis, Nancarrow, Ariss and Enderby136,Reference Smith and Fowler Davis144 These teams developed through a national initiative (the NHS vanguard programme)Reference Warwick-Giles and Checkland145 that sought to integrate health and social care in the community and reduce pressures on hospital services.
The research drew on a review of the literature and qualitative research with staff based in 10 community interprofessional teams. In particular, staff discussed how person-focused aspects of team leadership contributed to effective teamwork and service-user outcomes. Several important examples are set out below.
Motivating the team: team leaders who maintained a positive attitude, communicating confidence in the team’s abilities to deliver on its vision and objectives, were seen as more able to sustain team morale during difficult periods.
Walking the talk: setting high standards and being seen to embody these consistently, and demonstrating authority if required, were viewed as important in building team members’ confidence in their ability to deliver on their goals.
Collaborative learning and improvement: team members reported the value of prioritising improvement of their service and being enabled to work together to agree objectives for or approaches to change. Creating safe spaces where staff could raise concerns and propose solutions was seen as important for developing plans that fitted the context and were owned by team members.
Considering individuals: recognising and working with individual needs was seen as key to developing the team overall while ensuring its individual members felt valued. Examples of this included team leaders viewing each team member as an individual, providing constructive feedback, and tailoring development to reflect personal aspirations while also complementing the team’s objectives.
Empowering staff: sharing responsibility – for example, for decision-making – across the team was reported as being important for developing teamwork. At the same time, by providing advice or assuming responsibility for higher risk actions, team leaders supported the autonomy of individual staff (‘letting us get on with it’) and enabled staff to deal with problems directly.
Team building and maintenance: a team approach was taken in both day-to-day activities (e.g. by managing group dynamics to ensure all voices were heard, or creating clear and consistent boundaries for team member roles) and formal and informal team exercises (e.g. team-based development activities or social events).
Emotional intelligence: staff referred to the importance of empathy, communication, and openness to help staff feel valued and understood and to promote healthy communication across the team.
Supporting the team in discussing, learning, and collaborating around quality appears to result in better problem-solving and a stronger sense of team membership and common goals.Reference Smith, Fowler-Davis, Nancarrow, Ariss and Enderby136,Reference Smith and Fowler Davis144 This is supported further by creating a clear sense of team identity and purpose.Reference Smith, Fowler-Davis, Nancarrow, Ariss and Enderby136,Reference Smith and Fowler Davis144 For example, research on mental health teams has indicated the importance of having team leaders who can chair team meetings effectively. When team leaders were able to create a space for the team to agree key care decisions, share ideas, and work through disagreements constructively, this set the tone for the team.Reference West, Almo-Metcalfe and Dawson141
The task of team leadership may become more complex when teams cover more than one profession or sector. Staff in integrated teams reflected that health and social care have different leadership cultures: social care is less hierarchical than healthcare and has more formalised mechanisms of support for staff.Reference Smith and Fowler Davis144
4.6.2 Task-Focused Leadership
Task-focused leadership relates to the processes by which team goals are achieved. Having a shared sense of objectives, responsibilities, and delivery helps to ensure that all team members are working to achieve the same quality goals; and, as goals become clearer, so does team effectiveness.Reference McKean and Snyderman116,Reference Smith, Fowler-Davis, Nancarrow, Ariss and Enderby136,Reference Lyubovnikova, West, Salas, Tannenbaum, Cohen and Latham137,Reference Smith and Fowler Davis144 Next, building expertise (e.g. by addressing gaps in knowledge or skills and enabling access to training) increases the team’s capabilities to deliver high-quality care.Reference McKean and Snyderman116,Reference Smith, Fowler-Davis, Nancarrow, Ariss and Enderby136,Reference Smith and Fowler Davis144 Then, leading beyond the team, in order to promote it with stakeholders within and beyond the organisation, can improve access to shared resources (e.g. diagnostics) and help to build wider networks across local systems.Reference McKean and Snyderman116,Reference Smith, Fowler-Davis, Nancarrow, Ariss and Enderby136,Reference Smith and Fowler Davis144,Reference Edmondson and Harvey146
Underlying these processes are team leaders’ personal qualities: in addition to expertise and focus on quality and innovation,Reference Smith, Fowler-Davis, Nancarrow, Ariss and Enderby136 they bring enthusiasm, empathy, emotional intelligence, and communication skills.Reference Smith, Fowler-Davis, Nancarrow, Ariss and Enderby136,Reference Smith and Fowler Davis144 Staff in integrated community teams highlighted the importance of a team leader who could ‘walk the talk’ and act as a role model for other members of the team, and they emphasised the importance of leaders who maintained a positive, constructive approach during difficult times.Reference Smith and Fowler Davis144
5 Critiques of Governance and Leadership
5.1 Navigating the Complex Challenges of Governance and Leadership
There is probably no single best way to govern or lead for improving quality and safety. The examples explored in this Element show that the effects of governance and leadership are strongly influenced by context at the macro, meso, and micro levels. Contingency theory suggests that different styles of governance may work better depending on circumstances. For example, inward-focused organisations (those that focus mainly on internal processes) may achieve greater staff commitment, while outward-looking organisations (those that prioritise the wider context, including neighbouring organisations, regulators, and policy-makers) might engage more effectively with external regimes.Reference Mannion and Davies67 Important influences include policy priorities and organisational challenges – factors that should not be seen in isolation but understood, rather, as highly interrelated.Reference Hartley20,Reference Øvretveit40,Reference McKean and Snyderman116,Reference Donovan, Salmon and Lenné120,Reference Øvretveit147–Reference Fulop and Robert149
Earlier, we highlighted a number of unintended consequences of some approaches to governance, including the risks of reduced capacity to balance long-term and short-term priorities, reduced creativity in central policy-making (Section 3.2), and downsides associated with target-driven regimes (Section 4.3). We also showed that adapting approaches to healthcare governance from those used elsewhere – for example, importing thinking, structures, and processes from the business sector (Section 3.2) to inform new public management – is not straightforward. The question of stakeholders illustrates some of these complexities: while governance in the business sector relates to shareholders, the main stakeholder in a public health system could be said to be society in all its guises.Reference Ferlie, Baeza, Addicott and Mistry12,Reference Ferlie and Aldag24,Reference Ramsay, Fulop, Fresko and Rubenstein60,Reference Chambers62 As a result, there are active debates about how to ensure democratic, public accountabilityReference Ferlie, Baeza, Addicott and Mistry12,Reference Ferlie and Aldag24 and how best to involve the public in making decisions about major changes to the organisation of care.Reference McKevitt, Ramsay and Perry131,Reference Fraser, Baeza and Boaz132 Closer to the micro level, the example of root cause analysis, a technique originally used to investigate incidents in industrial settings, further illustrates some of the challenges of transferring learning into healthcare. In industrial settings, root cause analysis operates as a learning technique and prioritises the avoidance of blame. In healthcare settings, however, root cause analysis may take on additional functions of establishing responsibility for an incident and extending organisational surveillance and control; this in turn reduces the envisaged learning benefits.Reference Nicolini, Waring and Mengis150
Similarly, though considerable efforts have been made to improve approaches to regulation (Box 5), research on the CQC’s influence on performance describes how regulators may be feared by the organisations they regulate.Reference Smithson, Richardson and Roberts151 Fearfulness can prompt organisations to become closed and defensive, which in turn limits the effectiveness of regulatory activity. NHS England’s special measures regime for improving quality (which operated from 2014 to 2021, when it was replaced with the Recovery Support Programme)156 provides a recent illustration of the potential impact of macro-level performance management on organisations.Reference Vindrola-Padros44 Under this regime, organisations rated by the CQC as ‘inadequate’ on leadership and other qualities entered special measures for quality, a process that included an offer of external support and oversight to improve quality.Reference Vindrola-Padros44,Reference Smithson, Richardson and Roberts151 Organisations also required support to mitigate the emotional cost and stigma associated with being placed in special measures. Further, improving performance from a low starting point required substantial additional resources, both in terms of the time required to make change (2–3 years) and sustainable funding for long enough to result in improved performance.Reference Vindrola-Padros44
Box 5 Development of the CQC’s inspection approach
In 2013, the CQC introduced a new approach to inspection, which included more precisely targeted care standards and extended site visits conducted by larger, more expert teams.Reference Smithson, Richardson and Roberts151 Research on this approach described the important relationship between inspectors and local staff: inspectors needed to be sufficiently skilled and experienced to be perceived as credible and sufficiently consistent to be trusted; local teams needed to be willing to discuss improvement openly. A key challenge identified for inspectors was the need to build a close and supportive relationship with healthcare teams, while also maintaining sufficient objectivity.Reference Smithson, Richardson and Roberts151
In 2014, the CQC extended its inspection approach to dig further into leadership of organisationsReference Steward152 and, in so doing, suggested that the priorities of a ‘well-led’ organisation should be:
setting a clear vision for the organisation
having clear governance and accountability processes
fostering a culture that is transparent and quality-focused
engaging with both staff and patients
learning and finding new ways to improve.
From 2021, following experiences of the COVID-19 pandemic, the CQC adapted their approach to inspection further.153,Reference Rayner154 On-site service inspections would no longer be conducted routinely; instead, they would happen only when there was a clear need for them, for instance when there were clear signs of a change in quality of care, or where necessary information was unavailable. In support of this more risk-based approach, CQC emphasised the importance of both hard and soft intelligence, including enhanced routine data monitoring, and strengthened communication with services and members of the wider community. From 2022, CQC began a staged introduction of a new single assessment framework.155 This aimed to simplify the regulation process and to link assessment more closely to stakeholder priorities, guided by new quality statements (‘We statements’), shaped by public expectations of services.
None of this is to say that regulation and governance are bad things, but it does emphasise the need for optimised design and execution. According to Smithson et al., a constructive, quality-focused relationship between regulators and those regulated is more likely to result in positive experiences of regulation and improvements in healthcare quality.Reference Smithson, Richardson and Roberts151 Considering regulation as a ‘social process’ means that both regulators and those regulated may contribute to more productive interactions, characterised by longstanding relationships, openness, mutual trust and respect, shared values and agreed ways of working, opportunities to interact informally, and experienced and respected inspectors who possess the interpersonal skills to conduct inspection with consistency and fairness.Reference Smithson, Richardson and Roberts151
The challenges of leadership are similarly complex. Whether leading at board levelReference Jones, Pomeroy and Robert45,Reference McKean and Snyderman116 or within a clinical team,Reference Künzle, Kolbe and Grote119 effective leadership relies in part on assessing and responding to present and oncoming shifts in context. Making sense of these complex and dynamic changes in context is likely to play an important part in effective leadership for quality.Reference Hartley20 Of course, that requires the right approach to leadership. As discussed earlier (Section 3.3), much thinking on leadership has traditionally drawn on what are now fairly outdated understandings of how leadership works – for instance, the focus on heroic models, which contrasts with the reality that achieving high-quality care is likely to rely on more collective efforts. Since the early 2000s, there has been a shift to seeing distributed leadership as an effective way to encourage creative innovations at the frontline.Reference Currie and Lockett48–Reference Bolden50,Reference Braithwaite90,Reference Barnett and Weidenfeller157 But distributed leadership (where leadership is spread though different levels of an organisation or system) is not in itself a panacea: while effective healthcare does rely on drawing together expertise from a range of disciplines,Reference Aufegger, Shariq, Bicknell, Ashrafian and Darzi53,Reference Smith, Fowler-Davis, Nancarrow, Ariss and Enderby136,Reference Lyubovnikova, West, Salas, Tannenbaum, Cohen and Latham137 researchers have also noted that managerial and professional hierarchies may simultaneously work against attempts to share leadership.Reference Currie and Lockett48,Reference Currie and Spyridonidis54
Governance and leadership across sectors can be particularly challenging when leadership is also shared – with a risk that such distributed leadership becomes fractured in practice.Reference Currie and Lockett48 Frontline staff and local leaders may have a clear view of how to deliver high-quality care within their own team, but their views may be influenced by a desire to protect their services from change. As illustrated by the two examples of stroke service reorganisation (see Box 2), these vested interests may have to be challenged to improve care quality.Reference Fulop and Ramsay11,Reference Jones, Pomeroy and Robert45,Reference Dixon-Woods, McNicol and Martin83
Accelerated by the COVID-19 pandemic, recent thinking has proposed ‘the need for public sector transformations to support the robust governance of turbulence’.Reference Ansell, Sørensen and Torfing158 It is argued that many traditional approaches to governance are not fit to address turbulent, disruptive challenges, especially in an era of rapid technological advances where information and other resources may be transferred quickly across the world, and where the nature of problems to be addressed is unclear. Discussions of governance during this period,Reference Ansell, Sørensen and Torfing158 supported by a literature review of public service responses to the turbulence prompted by COVID-19,Reference Scognamiglio, Sancino, Caló, Jacklin‐Jarvis and Rees159 suggest that robustness can be achieved through agile network governance, where public organisations meet new challenges creatively in close partnership with the private sector and wider society. This work identifies seven strategies that characterise governance for turbulence:Reference Scognamiglio, Sancino, Caló, Jacklin‐Jarvis and Rees159
scalability – where resources may be increased or decreased to support responses to immediate and changing demands
prototyping – iterative development of innovative solutions, based on evaluation of rapid feedback
modularisation – where multiple solutions are developed in parallel to address separate components of a developing situation
bounded autonomy – building local and regional ownership of a strategy, drawing together system leaders, service providers, and members of the public
bricolage – making creative and adaptive use of available resources to fashion a response when no tailored response exists
strategic polyvalence – where solutions are designed so that they might serve multiple strategic purposes
voluntary compliance – importantly, evidence on responses to COVID-19 suggested that robustness of governance responses to turbulence rely on co-creation between public organisations and consenting members of the public.
Important priorities for governing in turbulent times include active engagement with frontline staff and external experts, a willingness to work with incomplete or uncertain data, distribution of responsibility to actors best suited to an emerging problem, willingness to experiment and an acceptance of the risk of associate failure, and enhanced communication with all stakeholders.Reference Ansell, Sørensen and Torfing158
5.2 Gaps in the Evidence
Some clear gaps and challenges in the evidence remain. Although much has been written about how governance and leadership could or should work, we are still learning about their relationship with quality and safety. In particular, much remains to be understood about which aspects of governance and leadership result in better quality, how they exert that influence, and under which circumstances. In part, this relates to a number of limitations in how we think about governance and leadership, and how their relationship with quality and safety has been analysed to date.
First, there are some important challenges in relation to how governance and leadership are defined and understood. As outlined in Section 3.1, different definitions of both concepts have emerged, raising questions about the extent to which research is addressing the same thing. Examples of such difficulties include terms like ‘leadership’ and ‘management’ being used interchangeably,Reference Reichenpfader, Carlfjord and Nilsen39 and supposedly contrasting leadership approaches being applied in very similar ways in practice.Reference Donovan, Salmon and Lenné120
Second, there are limitations in terms of the type of evidence that has been generated. The overall quality of the evidence base for the impact of governance and leadership on performance has been questioned.Reference Currie and Lockett48 Further, in many cases the direction of the relationship may be uncertain; for example, high performance might enable certain governance or leadership approaches, rather than be the result of them. While some researchers propose that randomised controlled trials (RCTs) are required to better understand the impact of governance and leadership on aspects of quality and safety,Reference Mintz and Stoller160 RCT-type evidence is unlikely to be appropriate for understanding many of the phenomena presented here. This is because many of the factors that RCTs seek to control for (e.g. organisational context and interactions with it) in fact play a pivotal role in how governance and leadership work in practice. Excluding these factors limits the value of such analyses.Reference Marchal, Westhorp and Wong161 Some research has shown associations between certain approaches to governance and leadership and performance on quality,Reference Jha and Epstein74,Reference Jha and Epstein75,Reference Veronesi, Kirkpatrick and Vallascas87 and other research acknowledges how different approaches play out in different contexts.Reference West, Lyubovnikova, Eckert and Denis68
Studies that account for the integral role of context are likely to provide many useful lessons about how governance and leadership contribute to quality and safety – for example, approaches making use of qualitative and quantitative methods, process evaluations, and in-depth ethnographic studies are likely to be valuable.Reference Moore, Audrey and Barker162–Reference Fletcher, Jamal and Moore164 Longitudinal, theory-driven research of this kind can help open up this black box to explain how governance and leadership influence quality and safety. We have highlighted several examples of such research in this Element, but more are needed; given the powerful influence of context there is a clear need for further research to be conducted in a range of settings. As research funders continue to prioritise such work, we anticipate that understanding of these complex relationships will continue to grow over the coming years.
6 Conclusions
This Element has analysed how governance and leadership shape and influence organisation and delivery of healthcare quality and safety at macro, meso, and micro levels of the system. Governance and leadership may contribute both to significant improvements and major failures in delivering high-quality, safe care, so it is important to get them right. We have described conditions that might help to ensure that performance measures, targets, and regulatory activities support rather than hinder organisations in improving quality (e.g. aligned targets, sufficient organisational capacity). We have outlined behaviours that may help boards focus more effectively on improving quality (e.g. prioritisation of quality, focused discussions informed by a range of hard and soft data, engaging stakeholders both within and beyond the organisation). We have also set out how different leadership approaches contribute to delivering major system change (e.g. how combining top-down authority and bottom-up clinical leadership can help sustain stakeholder participation and challenge local vested interests). Finally, we have shown how person-centred and team-centred leadership may influence the ways in which teams work together to deliver high-quality, safe care (e.g. effective chairing of meetings may support a greater shared sense of purpose, while engaging with and valuing team members as individuals may help build psychological safety). Box 6 provides a summary of the lessons that can be drawn from the evidence.
Box 6 Lessons on how governance and leadership influence quality and safety at macro, meso, and micro levels
At Macro Level (National)
Incentives (e.g. targets, payments) can encourage implementation and sustainability of change, but they may also have unintended consequences (e.g. gaming targets). Those who manage, deliver, and use services therefore need to contribute to the development of the objectives associated with these incentives to ensure buy-in.
Interventions to support struggling organisations may support improvements in quality but may also introduce significant practical and emotional burdens. Resources are needed to ensure that organisations have the skills and capacity to develop and deliver an improvement strategy.
At Meso Level (Systems and Organisations)
Quality and safety need to be a central priority for board activity. That means inclusion on agendas, creating systems to support understanding of quality, and dedicating resources to build expertise in quality.
To build a compelling case for improving quality, board and divisional leaders should draw on a range of both hard data and soft data (e.g. patient narratives). A central challenge is to then engage key stakeholder groups (including staff, patients, and carers) to build a shared understanding of quality and a culture that is supportive of quality. For example, this can be achieved by leaders attending stakeholder events, inviting stakeholders to board meetings, and visiting various care settings.
Board development and self-assessment tools (e.g. on QI maturity) may help boards to adopt processes that are more effective in addressing quality and, in turn, develop more successful organisational improvement strategies.
Boards may also look beyond their own organisation – for example, learning from improvement approaches used in neighbouring organisations, or by contributing to system-wide improvement activities.
Implementing system-level improvements is complex and may be facilitated by combining top-down and bottom-up leadership approaches.
At Micro Level (Clinical Teams)
Person-centred leadership includes focusing on team members’ individual needs and aspirations, and providing constructive feedback and development opportunities. Such actions may improve the team’s overall skill mix and help to ensure that team members feel valued, thereby increasing their sense of belonging and ownership of team priorities.
Taking a task-centred approach may also support quality. Creating shared objectives and responsibility for quality across the team is central to shaping a culture that is supportive of improvement. Using established team processes (e.g. routine discussions of clinical cases, team away-days, training or coaching sessions) to facilitate decision-making, learning, and collaboration around quality and safety can help to achieve this. It may also enhance team members’ psychological safety, thereby encouraging open discussions about improvement and increasing innovation. However, achieving or maintaining a shared culture across teams may become more challenging as membership becomes more diverse and complex.
7 Further Reading
Defining Governance and Leadership
Davies et al.Reference Davies, Anand and Artigas19 – a review that describes the history and mechanisms of different modes of governance.
Ferlie et al.Reference Lynn, Heinrich and Hill18 – an overview of thinking about macro, meso, and micro levels in health systems.
Hartley and BeningtonReference Hartley and Benington38 – an overview of approaches to leadership in healthcare.
ØvretveitReference Øvretveit40 – a review of how governance and leadership influence quality.
Influencing Improvement through Governance and Leadership
BraithwaiteReference Braithwaite90 – an analysis of factors influencing QI.
Fulop and RamsayReference Fulop and Ramsay11 – an analysis of how organisations influence quality and safety.
McKean and SnydermanReference McKean and Snyderman116 – a review of leadership’s influence on safety, drawing on healthcare and other sectors.
Mannion and DaviesReference Mannion and Davies67 – an analysis of the influence of context and culture on quality in care, with a focus on governance.
Performance Measurement and Management
PollittReference Pollitt96 – a literature review of performance management over the past 40 years.
Mannion and BraithwaiteReference Mannion and Braithwaite92 – a review identifying the pitfalls of performance measurement in the English NHS.
Smithson et al.Reference Smithson, Richardson and Roberts151 – an evaluation of the CQC’s approach to inspecting health and social care providers.
Leadership of Major System Change
Best et al.Reference Best, Greenhalgh and Lewis51 – a literature review describing factors influencing large system transformation, including leadership.
Turner et al.Reference Turner, Ramsay and Perry130 – a qualitative analysis of leadership approaches used in a major system change of acute stroke services in London and Greater Manchester.
Vindrola-Padros et al.Reference Vindrola-Padros, Ramsay and Perry128 – a qualitative analysis of leadership approaches used by a provider network in implementing a major system change of specialist cancer surgical services.
Fraser et al.Reference Fraser, Stewart and Jones133 – an editorial drawing on research evidence, presenting a critique of approaches to leading major system change.
Board Governance
Chambers et al.Reference Chambers, Harvey and Mannion55,Reference Chambers, Smith and Proudlove165 – a literature reviewReference Chambers, Harvey and Mannion55 and qualitative studyReference Chambers, Smith and Proudlove165 of board governance, including membership and dynamics.
Jones et al.Reference Jones, Pomeroy and Robert45 – a mixed-methods study of how boards operate in healthcare organisations with high and low QI maturity.
Team Leadership
Aufegger et al.Reference Aufegger, Shariq, Bicknell, Ashrafian and Darzi53 – a review of the literature on how shared leadership might contribute to effectiveness of clinical team management.
Smith et al.Reference Smith and Fowler Davis144 – an article drawing together a review of the evidence and qualitative research on the contribution of leadership to teamwork and effectiveness in community health and social care teams.
Both authors contributed to conceptualisation of this Element, the selection and interpretation of evidence presented, and drafting of the Element at all stages of its development. Both authors have approved the final version, and agree to be accountable for all aspects of the work in ensuring that questions related to its accuracy or integrity are appropriately investigated and resolved.
Conflicts of Interest
Naomi J. Fulop is a non-executive director on the board of Whittington Health NHS Trust.
Acknowledgements
We thank the peer reviewers and editorial team for their insightful comments and recommendations to improve the Element. A list of peer reviewers is published at www.cambridge.org/IQ-peer-reviewers. Naomi J. Fulop is a National Institute for Health Research (NIHR) Senior Investigator. The views and opinions expressed in this Element are those of the authors and do not necessarily reflect those of the NIHR, NHS, or the Department of Health and Social Care.
Funding
This Element was funded by THIS Institute (The Healthcare Improvement Studies Institute, www.thisinstitute.cam.ac.uk). THIS Institute is strengthening the evidence base for improving the quality and safety of healthcare. THIS Institute is supported by a grant to the University of Cambridge from the Health Foundation – an independent charity committed to bringing about better health and healthcare for people in the UK.
About the Authors
Naomi J. Fulop is Professor of Health Care Organisation and Management in the Department of Applied Health Research, University College London. Her research interests are at the interface between health policy and delivering, managing, and organising healthcare services.
Angus I. G. Ramsay is Principal Research Fellow in the Department of Applied Health Research, University College London. He is interested in using mixed-method evaluation approaches to understand how organisational factors influence efforts to improve quality of care and patient outcomes.
Creative Commons License
The online version of this work is published under a Creative Commons licence called CC-BY-NC-ND 4.0 (https://creativecommons.org/licenses/by-nc-nd/4.0). It means that you’re free to reuse this work. In fact, we encourage it. We just ask that you acknowledge THIS Institute as the creator, you don’t distribute a modified version without our permission, and you don’t sell it or use it for any activity that generates revenue without our permission. Ultimately, we want our work to have impact. So if you’ve got a use in mind but you’re not sure it’s allowed, just ask us at [email protected].
The printed version is subject to statutory exceptions and to the provisions of relevant licensing agreements, so you will need written permission from Cambridge University Press to reproduce any part of it.
All versions of this work may contain content reproduced under licence from third parties. You must obtain permission to reproduce this content from these third parties directly.
Editors-in-Chief
THIS Institute (The Healthcare Improvement Studies Institute)
Mary is Director of THIS Institute and is the Health Foundation Professor of Healthcare Improvement Studies in the Department of Public Health and Primary Care at the University of Cambridge. Mary leads a programme of research focused on healthcare improvement, healthcare ethics, and methodological innovation in studying healthcare.
THIS Institute (The Healthcare Improvement Studies Institute)
Graham is Director of Research at THIS Institute, leading applied research programmes and contributing to the institute’s strategy and development. His research interests are in the organisation and delivery of healthcare, and particularly the role of professionals, managers, and patients and the public in efforts at organisational change.
Executive Editor
THIS Institute (The Healthcare Improvement Studies Institute)
Katrina is Communications Manager at THIS Institute, providing editorial expertise to maximise the impact of THIS Institute’s research findings. She managed the project to produce the series.
Editorial Team
RAND Europe
Sonja is Director of RAND Europe’s healthcare innovation, industry, and policy research. Her work provides decision-makers with evidence and insights to support innovation and improvement in healthcare systems, and to support the translation of innovation into societal benefits for healthcare services and population health.
RAND Europe
Tom is Head of Evaluation at RAND Europe and President of the European Evaluation Society, leading evaluations and applied research focused on the key challenges facing health services. His current health portfolio includes evaluations of the innovation landscape, quality improvement, communities of practice, patient flow, and service transformation.
THIS Institute (The Healthcare Improvement Studies Institute)
Ellen supported the production of the series during 2020–21.
About the Series
The past decade has seen enormous growth in both activity and research on improvement in healthcare. This series offers a comprehensive and authoritative set of overviews of the different improvement approaches available, exploring the thinking behind them, examining evidence for each approach, and identifying areas of debate.