 Comorbid Eating Disorders and Obsessive-Compulsive Disorder
Comorbid Eating Disorders and Obsessive-Compulsive Disorder Book contents
- Comorbid Eating Disorders and Obsessive-Compulsive Disorder
- Comorbid Eating Disorders and Obsessive-Compulsive Disorder
- Copyright page
- Contents
- Foreword
- Preface
- Acknowledgments
- Abbreviations
- Part I Overview of the Existing Literature
- Part II Clinical Pitfalls and Treatment Failures
- Part III Evidence-Informed Considerations for Assessment and Treatment
- Part IV Special Topics and Future Considerations
- References
- Index
- References
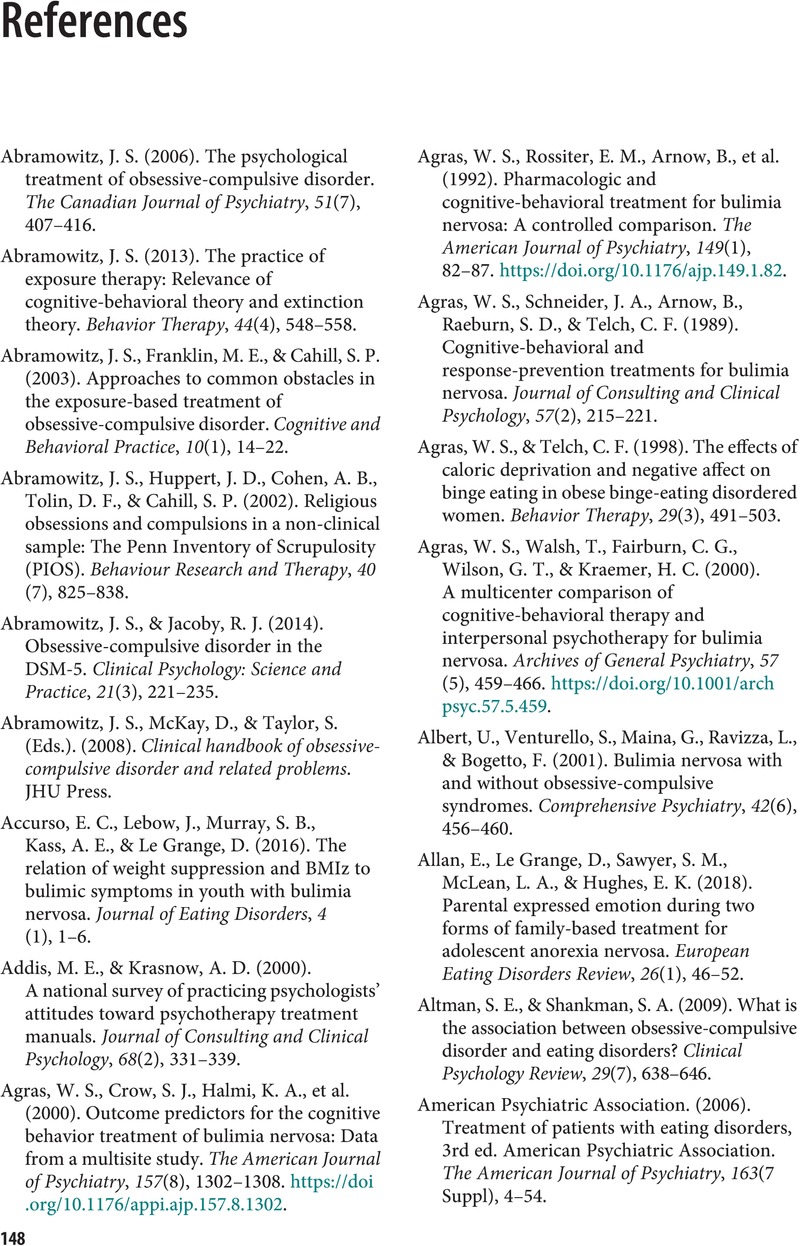
References
Published online by Cambridge University Press: 14 December 2023
- Comorbid Eating Disorders and Obsessive-Compulsive Disorder
- Comorbid Eating Disorders and Obsessive-Compulsive Disorder
- Copyright page
- Contents
- Foreword
- Preface
- Acknowledgments
- Abbreviations
- Part I Overview of the Existing Literature
- Part II Clinical Pitfalls and Treatment Failures
- Part III Evidence-Informed Considerations for Assessment and Treatment
- Part IV Special Topics and Future Considerations
- References
- Index
- References
Summary
- Type
- Chapter
- Information
- Comorbid Eating Disorders and Obsessive-Compulsive DisorderA Clinician's Guide to Challenges in Treatment, pp. 148 - 174Publisher: Cambridge University PressPrint publication year: 2023


