1.1 Introduction
Global aging is one the most significant challenges we are facing today, although aging trajectories differ from country to country (United Nations [UN], 2017, 2019a). In general, population aging takes a socioeconomic toll on a society, and the subsequent rise in the prevalence of dementia is a serious health burden and difficult social issue most aging countries are now confronted with (Patterson, Reference Patterson2018). Dementia is an emotionally difficult illness not only for the patient but also for family members and caregivers. As the patients lose memory, visuospatial abilities, and other cognitive functions, care often becomes a daunting task. It has been estimated that the worldwide cost of dementia was one trillion U.S. dollars in 2016, and this will likely double in 2030 (Patterson, Reference Patterson2018). Fifty million people, approximately the population of South Korea or Spain, live with dementia around the world, and the number has been projected to triple by 2050.
Since age is the most significant risk factor for dementia, with prevalence significantly increasing after 65 years old (Cummings & Benson, Reference Cummings and Benson1992), countries with faster population-aging trajectories are likely to experience greater challenges in tackling issues concerning dementia. A country is classified as an “aging society” when 7% of its population are over 65 and as an “aged society” when 14% are, and the rate of its population aging is often gauged by the time it took to become an aged society from an aging society. For instance, France took 115 years, the U.S. 69, Spain 45, and Japan 25 to become an aged society from an aging one (Higo & Khan, Reference Higo and Khan2015), but it took only 18 years for South Korea to transform from an aging to an aged society, making it the fastest-aging country in the world (Korean Statistical Information Service [KOSIS], 2021a; Ogawa & Matsukura, Reference Ogawa and Matsukura2007; UN, 2019b). Another measure of population aging, the percentage increase of its population 65 years old and older during a period of time, also illustrates that South Korea would experience a 23% increase from 2019 to 2050, the greatest increase in the world (UN, 2017, 2019b). According to the UN, however, many low- to middle-income countries (i.e., LMICs in Asia and Latin America) are on a similar track, as it has been projected that population aging is growing at a faster pace in these countries than the aged countries in Europe and North America.
In this chapter, the significance of South Korea as a case of interest for understanding global and regional population aging and the associated increasing dementia population is introduced and discussed. A brief history of South Korea, transforming from an agricultural society to a major industrialized nation in less than half a century is introduced, along with major societal changes that would have a major impact on the cognitive aging of older Koreans and their risk for dementia. Earlier studies of cognitive aging of elderly Koreans are introduced, which have demonstrated strong effects of education or literacy on cognitive tests evaluating dementia. Further, the chapter discusses the role of formal education in cognitive development and its moderating effects on neurodegeneration, which would have significant consequences on the prevalence of dementia in older Koreans, especially women. This has important implications on global aging and dementia epidemiology, as well as other health risks associated with rapid modernization, as the current increase in global dementia population is most concentrated in the LMIC countries in Latin America and Asia (Livingston et al., Reference Livingston, Huntley, Sommerlad, Ames, Ballard, Banerjee, Brayne, Burns, Cohen-Mansfield, Cooper, Costafreda, Dias, Fox, Gitlin, Howard, Kales, Kivimäki, Larson, Ogunniyi and Mukadam2020; Patterson et al., Reference Patterson2018).
1.2 From an Agricultural Society to an Industrialized Modern Nation
Today, it is difficult for the younger generation to imagine a post-war Korea with mass poverty, but older Koreans have vivid memories of growing up in small villages scarred by wars and foreign occupation (see Figures 1.1a, 1.1b, 1.1c). The Republic of Korea, better known as South Korea, was established in 1948 amid political turmoil involving foreign interference and clashes of political ideology, resulting in the division of the Korean peninsula into North and South that precipitated the Korean War of 1950–1953. A decade after the war, South Korea initiated the transformation of an age-old agricultural economy heavily reliant on rice farming to a highly industrialized global economy in less than half a century. Sociologist Kyung-Sup Chang characterized the transformation as the “compressed modernization” process of South Korea, and analyzed the sociopolitical, economic, and cultural risks embedded in this rapid transformation (Chang, Reference Chang1999, Reference Chang2010).

Figure 1.1a A family picture taken in Iksan, a small town in Jeollabuk Province, by photographer Joo Myung Duck (1971). It was very common for Korean families to live in a household with three generations, especially in rural villages during the early phase of Korean Economic Development Plan (1962–1996).
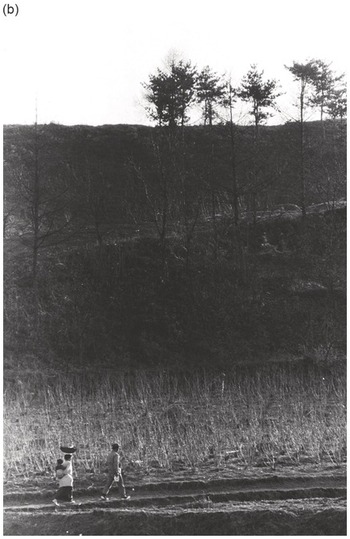
Figure 1.1b A young family walking country lane in Gapyeong, a rural region in Gyeonggi Province, photographed by Joo Myung Duck (1972). Mother is carrying a baby on her back and a basket on her head, following her husband in Gapyeong, a northern rural region.
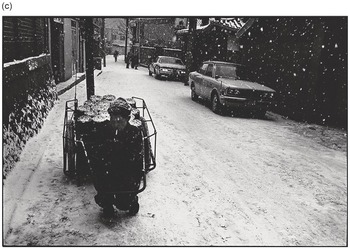
Figure 1.1c A coal-briquette deliverer in Seoul, 1973. In Kang Woon-gu (2008). Chance or Destiny. Paju, Gyeongido: Yeolhwadang.
Historically, Koreans had been mainly rice farmers since the fifth century BC, living in small villages in the Korean peninsula and ruled by monarchs from a number of dynasties until the last one, Chosun, which ended with the Japanese occupation of the peninsula in 1910. Despite the introduction of sporadic industrialization in the early twentieth century by foreign countries and the establishment of a modern republic in 1948, until the early 1960s South Korea remained mostly an agricultural country with a patriarchal infrastructure heavily steeped in Confucianist tradition. After a successful military coup led by Park Jung-Hee in 1961 that overturned the young democracy, the subsequent authoritarian government led by Park and his successors embarked on a very bold economic development plan from 1962 to 1996: the Korean Economic Development Plan (KEDP) (Ko, Reference Ko2007; Park, Reference Park2009). Many agree that the economic overhaul was very effective and efficient in transforming an inert economy into a vibrant one, making Korea an important player in the global market (Park, Reference Park2009; Vogel, Reference Vogel1991). Three decades of planned economic development, however, was something similar to a grand-scale social experiment that resulted in a society with a significant number of tensions and asymmetries in its social fabric (Chang, Reference Chang1999).
1.2.1 Korean Economic Development: Planned and Unintended Outcomes
As the KEDP was implemented to ensure expeditious growth in the economy, Korean society was under perpetual reconstruction. Moreover, because it was planned and assessed by the authoritarian government with very little oversight, the plan was executed in a regimented military style with minimal consideration for civil rights or the psychological well-being of its citizens (Han & Sharp, Reference Han and Sharp1997). Efficiency was perhaps the most important guiding principle to ramp up the economy in a short period of time, practically a generation, partly due to the fact that the authoritarian dictatorship had to earn its legitimacy through economic growth (Jeon, Reference Jeon2019; Kim, Reference Kim1997; Ko, Reference Ko2007). The plan and its execution were very successful in enlarging the Gross National Income (formerly Gross National Product or GNP), jumping from 2.9 billion dollars in 1962 to 608 billion in 1996, a 210-fold increase (World Bank, 2021a), while the Gross Domestic Product per capita increased from $90 in 1962 to $13,398 in 1996 (KOSIS, 2021b). As capital resources to build the economy were extremely scant initially, the industrial infrastructure was built in selected regions and concentrated in selected industries. Businesses, factories, and transportation were built in and around the biggest city and capital, Seoul, with the first highway built to connect Seoul with the biggest port city, Busan. During the KEDP phase, these urban areas enjoyed huge population growth as the major workforce from farming communities flowed from rural areas into industrial cities (Park, Reference Park2009). Further concentration of financial and economic resources was given to a number of big companies or conglomerates that could follow and cooperate with the government’s economic plan focused on an export-driven economy (Kim, Reference Kim1997). Even educational resources were concentrated in the elite or higher education institutions, such as national science and engineering institutes and universities funded by the government and the conglomerates, which were established to educate the future techno-elites who would lead the technology-driven Korean economic development (Jeon, Reference Jeon2019). In comparison, public education at the community level was delegated to private sectors, except the compulsory elementary education that had been established in 1949 (Yang et al., Reference Yang, Gong and Kim2010). The implementation of the economic development plan that concentrated on selected fields and sectors of society for three decades would have a lasting imprint on the social fabric and structure of South Korea, which would create unintended outcomes alongside the successful achievement of economic goals.
Interestingly, birth control policy was an important component of the planned economic development, which, although unintended, would have a significant consequence on the population aging of South Korea due to its aggressive and prolonged implementation. Initially, it was established to curb the post-war baby boom that peaked at six births per woman in 1960 and exacerbated the poverty of post-war Korea. With the success of the population control policy, the birth rate decreased significantly every decade, reaching the replacement rate of two in 1984. Unfortunately, the policy continued until 1996 and a reverse policy encouraging people to have children was introduced only in 2006, although a strong downward trend in the birth rate was already becoming established in Korea and its neighboring region (Chang et al., Reference Chang2010). South Korea’s birth rate dropped below one in 2018, and it is currently the lowest in the world at 0.8 (KOSIS, 2021d; UN, 2019b) and expediting population aging as life expectancy increased at the same time.
With the growing economy, the life expectancy of South Koreans increased as public hygiene improved and health-care systems were built. More specifically, average Koreans lived to just fifty-five years old in 1960; however, in 1969 they lived to over sixty, in 1988 to seventy, and to over eighty years old since 2010 (World Bank, 2021b). It has been reported that reductions in infant mortality, diseases related to infection, and cardiovascular disease were the three major factors that contributed to improving the life expectancy of South Koreans (Yang et al., Reference Yang, Gong and Kim2010), which was partly possible due to the rapid expansion of the health-care system. Since the first introduction of health insurance for workers in large-scale companies with 500 or more employees in 1977, it was expanded to cover all citizens in just twelve years (Lee, Reference Lee2003). The national health insurance system, introduced in 1989, no doubt has improved the overall health and quality of life of Koreans significantly. With the dropping birth rate and increasing life expectancy, however, the South Korean population has been growing older speedily. Considering that the percentage of the population aged sixty-five or older was only 2.9% in 1960, the rapid climb to 7% in 2000, officially becoming an aging country, was a major change in the country’s social demographics in just forty years since the KEDP took off (Kim, Won, et al., Reference Kim, Won, Suh, Kang and Lim2003; National Archives of Korea, 2021). Today, one of the most important population policy agendas of the South Korean government is to address and solve the problem of the so-called “demographic cliff” by moving the birth rate upward in order to slow down population aging (Ministry of Health & Welfare, Republic of Korea, 2021), a policy that has not been successful so far.
Rural areas have been hit the hardest in terms of population loss and aging. As business and industrial hubs were being developed, young workers found service and factory jobs in urban areas. Moreover, young students and sometimes their families moved to cities for secondary and higher education, resulting in a significant migration of the younger population to urban areas. Hence, the population aged rapidly and eventually decreased in small agricultural and fishing villages. Just thirty years after the government-led economic development plan had been implemented, prevalence and clinical studies in South Korea started to find an alarming rate of dementia in the growing older population, especially in the rural areas (Park et al., Reference Park, Ko, Park and Chul-Ho1994; Woo et al., Reference Woo, Lee, Yoo, Kim, Kim and Shin1998).
1.2.2 Education during the Modernization Period
The Republic of Korea started off with an ambitious plan to introduce compulsory primary education in 1948, and this was implemented right before the war in early 1950. The national elementary school system recovered relatively quickly after the war, but it took many years, in fact half a century, to expand compulsory education to secondary level. Considering that modernized industrialization would require an educated workforce, it is somewhat puzzling that a government initiating an ambitious economic development plan did not expand the compulsory education established in 1950 to middle school and beyond as they embarked on the plan. Unfortunately, it remained solely at primary level until 2002, when middle school was included (Yang et al., Reference Yang, Gong and Kim2010). This was partly due to the whole-hearted support of Korean families to educate their children in formal institutions from elementary school to college. For example, the enrollment in primary schools tripled, secondary school enrollment increased more than eight-fold, and higher education by ten times from 1945 to 1960 (Seth, Reference Seth2017), a trend that continued during the latter part of the twentieth century. According to sociologist Kyungsup Chang (Reference Chang2010), the social investment family in Korea, compared to the social investment state in the advanced modern countries in Europe and North America, fertilized the social basis for sustained economic development in Korea. Confucian tradition, manifested as “industrial neo-Confucianism,” has been proposed as the root of the high motivation of Korean families in educating their children, which contributed to the steep increase in the average number of years of education for younger generations. The entrance exam for higher education and elite institutions was characterized as a common cultural tradition in Eastern countries such as South Korea (Vogel, Reference Vogel1991).
Chang (Reference Chang2010), on the other hand, took note of the significant role education had on the new social ordering in post-war Korean society, in which traditional social order based on land ownership had all but vanished (Kim, Reference Kim2016). In the new social order, families strived to educate their children so that they would achieve higher social status, mounting to the famous “education fervor” in modern Korea (Seth, Reference Seth2002). Thanks to the strong motivation and efforts of Korean families to educate the younger generation, the government and businesses were able to get a workforce with higher education without significant investment. Further, the economic development plan from the 1960s relied on low wages to gain competitiveness in exporting goods that required labor-intensive systems, such as in the textile industries (Seth, Reference Seth2017). Therefore, it is hard to deny that the early exponential growth in the Korean economy benefited from the low labor costs of young workers with little formal education and mostly from the rural areas, who would endure harsh working conditions (Chang, Reference Chang1995).
Despite its effectiveness in increasing the average years of education (see Figure 1.2a), formal education supported by the social investment family had serious side effects. Perhaps the most important was that it failed to provide social mobility for socioeconomically disadvantaged citizens, since it depended on fierce competition between individuals and families and was at odds with the fair provision of educational opportunities (Chang, Reference Chang2010). It was especially disadvantageous for girls from rural or poor families wanting to receive secondary level education or beyond, as not only did traditional Confucian social order propel more boys to further their education in cities, but also the girls who remained in small rural villages did not have access to public education beyond elementary school. Many girls left their home villages to work in the cities as teenagers in the early stages of the KEDP, which maintained the significant disparity between the education received by women and men before the twenty-first century (Chang, Reference Chang1995; Sung, Reference Sung2003). As illustrated in Figure 1.2b, the vast majority of women over sixty-five received only primary education or less in 2005, which contrasts with more than half of men who received secondary education or more. The level of secondary and higher education in older women has risen significantly in the past decade, yet more than half of them did not receive secondary education (KOSIS, 2021c). Surprisingly, young women have entered college more frequently than men in the past eight years, as socioeconomics and culture related to family have changed drastically during the compressed modernization period. Still, the fact that a significant gender disparity in formal education has remained among older Koreans has had somber implications for the dementia risk in women.

Figure 1.2a Years of Education of Koreans in age brackets – the number of Koreans who received secondary education or higher has increased dramatically over each decade.

Figure 1.2b Years of education for Korean women and men over 65 years old in 2005 (i) and 2015 (ii), illustrates significant increase in secondary education in older Koreans over a decade.
1.3 Population Aging, Dementia, and Education
Average South Korean women born in 2030 are projected to live into their nineties for the first time in world history (Kontis et al., Reference Kontis, Bennett, Mathers, Li, Foreman and Ezzati2017). Considering that longevity is one of the most sought-after human desires, especially for Koreans, who have suffered war and life-threatening hardship in their modern history, this news merited great celebration in Korea, yet it was met with ambivalence. The increasing socioeconomic burden and health issues associated with population aging caused more apprehension than jubilation. A recent survey by the National Health Insurance found that dementia is the fourth most important health concern among Koreans (Health Insurance Review & Assessment Service, 2016).
Dementia has been generally defined as an acquired syndrome of intellectual impairment produced by brain dysfunction (Cummings & Benson, Reference Cummings and Benson1992), and it is caused by various diseases of the brain. Although memory impairment has been most frequently associated with dementia, the cognitive and behavioral symptoms of dementia vary depending on the brain regions affected by the disease. Most epidemiological studies have shown Alzheimer’s disease to be the most common cause of dementia, followed by vascular diseases or other brain conditions, such as alcoholism-related brain damage, depending on the age, gender, geographical location, and education of the elderly population (Cao et al., Reference Cao, Tan, Xu, Hu, Cao, Dong, Tan and Yu2020; Rizzi et al., Reference Rizzi, Rosset and Roriz-Cruz2014).
Concern over increasing dementia prevalence in South Korea became apparent from the 1990s, when studies began reporting levels higher than the world average of 5% in older Koreans (Ferri et al., Reference Ferri, Prince, Brayne, Brodaty, Fratiglioni, Ganguli, Hall, Hasegawa, Hendrie, Huang, Jorm, Mathers, Menezes, Rimmer and Scazufca2005; Kim et al., Reference Kim, Jeong, Chun and Lee2003; Youn et al., Reference Youn, Lee, Kim and Woo2005), and 10.8% in a rural area in Gyeongbuk province (Park et al., Reference Park, Ko, Park and Chul-Ho1994). Moreover, the numbers were significantly higher than other Asian countries and similar to the more advanced aged countries in Europe and North America. It was particularly noteworthy that dementia prevalence in Taiwan was reported to be 1.7~4.3% (Fuh & Wang, Reference Fuh and Wang2008) from 1980 to 2007. Considering that Taiwan has been comparable to South Korea in terms of its economic development and its history of Japanese occupation in the early twentieth century (Vogel, Reference Vogel1991; World Bank, 2021a), the marked disparity in dementia prevalence between the two countries observed in the early 1990s was puzzling (see Table 1.1 for details). Moreover, until recently, Japan, whose population aging was more advanced, reported lower prevalence than Korea, around 6~7% (Ohara et al., Reference Ohara, Hata, Yoshida, Mukai, Nagata, Iwaki, Kitazono, Kanba, Kiyohara and Ninomiya2017). At first glance, it was not clear why the prevalence of dementia in Korea had risen at an alarming rate since population aging started in the 1990s. On closer inspection, however, the prevalence statistics of older Koreans was striking in that women were two to five times more at risk of developing dementia than men (Kim et al., Reference Kim, Na, Yeon, Kang, Min, Lee, Lee, Lee, Pyo, Park, Kim and Bae1999; Lee et al., Reference Lee, Lee, Ju, Kang Uk Lee, Kim, Jhoo, Yoon, Ha and Woo2002; Park et al., Reference Park, Ko, Park and Chul-Ho1994; Shin et al., Reference Shin, Kim, Yoon, Kim, Yang, Kim, Lee, Kwak and Lee2002; Suh et al., Reference Suh, Kim and Cho2003; Woo et al., Reference Woo, Lee, Yoo, Kim, Kim and Shin1998. See Table 1.2 for details). Although women had been reported to be at increased risk for dementia, especially the Alzheimer’s type, a prevalence of this magnitude had not been reported in countries more advanced in aging, such as the U.S., Japan, and France.
| country | references | year | age | area/sample | sample size | prevalence (adjusted/standardized/estimated prevalence) (%) | |||
|---|---|---|---|---|---|---|---|---|---|
| overall | men | women | |||||||
| U.S. and Canada | U.S. | Folstein et al., Reference Folstein, Bassett, Anthony, Romanoski and Nestadt1991 | 1981 | 65+ | Eastern Baltimore | 923 | (4.5) | (5.2) | (4.0) |
| Koller & Bynum, Reference Koller and Bynum2015 | 2008 | 65+ | Medicare Fee-for-Service beneficiaries | 4,800,000 | 8.5 (8.2) | 6.4 | 9.9 | ||
| Langa et al., Reference Langa, Larson, Crimmins, Faul, Levine, Kabeto and Weir2017 | 2012 | 65+ | HRS* cohort | 10,511 | 8.8 (8.6) | – | – | ||
| Matthews et al., Reference Matthews, Xu, Gaglioti, Holt, Croft, Mack and McGuire2019 | 2014 | 65+ | Medicare Fee-for-Service beneficiaries | 28,027,071 | 11.5 (10.9) | 9.2 (8.6) | 13.3 (12.2) | ||
| Canada | Canadian Study of Health and Aging Working Group, 1994 | 1991–1992 | 65+ | Medicare lists in nine provinces or Enumeration Composite Record in Ontario and Institutions | 10,263 | (8.0) | (6.9) | (8.6) | |
| Public Health Agency of Canada, 2017 | 2013–2014 | 65+ | Canada excluding Saskatchewan | – | 7.1 | 5.6 | 8.3 | ||
| Europe | U.K. | Matthews et al., Reference Matthews, Arthur, Barnes, Bond, Jagger, Robinson and Brayne2013 | 1989–1994 | 65+ | Cambridgeshire, Newcastle, Nottingham | 7,635 | (8.3) | (7.4) | (9.4) |
| 2008–2011 | 65+ | 7,796 | (6.5) | (4.9) | (7.7) | ||||
| Portugal | Nunes et al., Reference Nunes, Silva, Cruz, Roriz, Pais and Silva2010 | 2003–2004 | 55–79 | Sao João da Madeira, Arouca | 1,146 | 2.7 | 3.2 | 2.3 | |
| Gonçalves-Pereira et al., Reference Gonçalves-Pereira, Cardoso, Verdelho, da Silva, De Almeida, Fernandes, Raminhos, Ferri, Prina, Prince and Xavier2017 | 2012–2013 | 65+ | Fernão Ferro, Mora/Cabeção | 1,397 | 3.7 | – | – | ||
| Ruano et al., Reference Ruano, Araújo, Branco, Barreto, Moreira, Pais, Cruz, Lunet and Barros2019 | 2013–2015 | 55+ | Porto | 730 | 1.0 (1.3) | 0.4 | 1.3 | ||
| Spain | Pi et al., Reference Pi, Olivé, Roca and Masana1996 | 1990 | 65+ | Catalunya (La Selva del Camp) | 516 | 14.9 | – | – | |
| Lobo et al., Reference Lobo, Saz, Marcos, Dia, De-la-Camara, Ventura, Montañes, Lobo-Escolar and Aznar2007 | 1994–1996 | 65+ | Zaragoza | 3,715 | 5.9 (3.9) | 3.8 (2.3) | 7.4 (5.0) | ||
| Virués-Ortega et al., Reference Virués‐Ortega, de Pedro‐Cuesta, Vega, Seijo‐Martínez, Saz, Rodríguez, Rodríguez-Laso, Reñé, de las Heras, Mateos, Martínez-Martín, Mahillo-Fernandéz, López-Pousa, Lobo, Reglà, Gascón, García, Fernandéz-Martínez, Boix and del Barrio2011 | 1990–2003 | 75+ | Composite population study (Arosa, Bidasoa, Cantalejo, Gerona, Leganes, NEDICES, PRATICON, Santiago, Toledo, Zaragoza) | 546 | 9.0 (7.5) | 6.8 | 10.3 | ||
| Tola-Arribas et al., Reference Tola-Arribas, Yugueros, Garea, Ortega-Valín, Cerón-Fernández, Fernández-Malvido, San José-Gallegos, González-Touya, Botrán-Velicia, Iglesias-Rodríguez and Díaz-Gómez2013 | 2009 | 65–104 | Valladolid | 2,170 | 8.5 (5.5) | 4.9 | 11.2 | ||
| Italy | Ferini-Strambi et al., Reference Ferini-Strambi, Marcone, Garancini, Danelon, Zamboni, Massussi, Tedesi and Smirne1997 | 1991 | 60+ | Vescovato | 673 | 9.1 (9.8) | – | – | |
| Prencipe et al., Reference Prencipe, Casini, Ferretti, Lattanzio, Fiorelli and Culasso1996 | 1992 | 65+ | Poggio Picenze, Scoppito, Tornimparte | 968 | 8.0 | 7.9 | 8.2 | ||
| Spada et al., Reference Spada, Stella, Calabrese, Bosco, Anello, Guéant-Rodriguez, Romano, Benamghar and Guéant2009 | 2005–2006 | 60–85 | Sicily (San Teodoro) | 280 | 7.1 | – | – | ||
| Greece | Tsolaki et al., Reference Tsolaki, Fountoulakis, Pavlopoulos, Chatzi and Kazis1999 | 1993 | 70+ | Pylea | 380 | 9.6 | 6.3 | 12.1 | |
| Kosmidis et al., Reference Kosmidis, Vlachos, Anastasiou, Yannakoulia, Dardiotis, Hadjigeorgiou, Sakka, Ntanasi and Scarmeas2018 | – | 65+ | Larissa, Maroussi, and nearby towns | 1,792 | 5.0 | 5.6 | 4.6 | ||
| Asia | Japan | Shibayama et al., Reference Shibayama, Kasahara and Kobayashi1986 | 1982 | 65+ | Aichi Prefecture | 3,106 | 5.8 | – | – |
| Okamura et al., Reference Okamura, Ishii, Ishii and Eboshida2013 | 1980–2008 (review) | 60+ | – | – | 2.9–12.5 | – | – | ||
| Ninomiya et al., Reference Ninomiya, Nakaji, Maeda, Yamada, Mimura, Nakashima, Mori, Takebayashi, Ohara, Hata, Kokubo, Uchida, Taki, Kumagai, Yonemoto, Yoshida, Muto, Momozawa, Akiyama and Kiyohara2020 | 2016–2018 | 65+ | Research institutions (Tokyo, Fukuoka, Shimane, Ishikawa, Aomori, Iwate, Kumamoto, Ehime) | 11,410 | 8.5 | 6.6 | 9.8 | ||
| China | Zhang et al., Reference Zhang, Katzman, Salmon, Jin, Cai, Wang, Qu, Grant, Yu, Levy, Klauber and Liu1990 | 1987 | 65+ | Shanghai | 3,888 | (4.6) | (2.0) | (6.6) | |
| Chiu et al., Reference Chiu, Lam, Chi, Leung, Li, Law, Chung, Fung, Kan, Lum, Ng and Lau1998 | 1995 | 65+ | Hong Kong | 1,034 | (4.0) | – | – | ||
| Wu et al., Reference Wu, Ali, Guerchet, Prina, Chan, Prince and Brayne2018 | 1989–2016 (review) | 65+ | Hong Kong | – | 7.2 | – | – | ||
| 60+ | – | – | 5.3 | – | – | ||||
| Wang et al., Reference Wang, Jia, Liang, Li, Qian, Li and Xu2019 | 1985–2018 (review) | 60+ | – | – | 4.9 | 3.8 | 5.6 | ||
| Taiwan | Fuh & Wang, 2008 | 1987–1993 (review) | 65+ | – | 1.7–4.3 | – | – | ||
| Wu et al., Reference Wu, Ali, Guerchet, Prina, Chan, Prince and Brayne2018 | 1989–2016 (review) | 65+ | – | – | 6.0 | – | – | ||
HRS: Health and Retirement Study
Table 1.2 Prevalence of dementia in Korean men and women
| references | year | area | age | sample size | prevalence (adjusted/standardized/estimated prevalence) (%) | ||
|---|---|---|---|---|---|---|---|
| overall | men | women | |||||
| Suh et al., Reference Suh, Kim, Kwak, Kim, Kim, Kim, Kim, Kim, Kim, Kim, Moon, Park, Park, Park, Bae, Seo, Seong, Son, Shin and Kim2021 | 2017 | Nationwide | 65+ | 2,972 | (8.5) | (5.3) | (10.6) |
| Jang et al., Reference Jang, Park, Kim, Lee, Lee and Kim2021 | 2015 | Nationwide | 60+ | 352,869 | 6.7 (5.3) | 4.5 | 8.0 |
| Kim et al., Reference Kim, Han, So, Seo, Kim and Kim2014 | 1990–2013 (review) | – | 65+ | – | 9.2 | 6.8 | 10.7 |
| Kim et al., Reference Kim, Park, Kim, Kim, Kim, Kim, Kim, Moon, Bae, Woo, Ryu, Yoon, Lee, Lee, Lee, Lee, Lee, Lee, Chang and Cho2011 | 2008 | Nationwide | 65+ | 6,141 | 9.2 (8.1) | 8.0 | 9.9 |
| Kim et al., Reference Kim, Jeong, Chun and Lee2003 | 2001 | Busan | 65+ | 1,101 | 7.4 (8.0) | 2.4 (2.7) | 10.5 (10.0) |
| Lee et al., Reference Lee, Lee, Ju, Kang Uk Lee, Kim, Jhoo, Yoon, Ha and Woo2002 | 1999–2000 | Seoul | 65+ | 643 | (8.1) | – | – |
| Park et al., Reference Park, Ko, Park and Chul-Ho1994 | 1990 | Yungil-Gun, Kyungbook | 65+ | 692 | 10.8 | 7.2 | 14.5 |
The socioeconomic status of an individual, especially their years of formal education, has been found to have a major impact on their risk of dementia (Chapko et al., Reference Chapko, McCormack, Black, Staff and Murray2018; Meng & D’Arcy, Reference Meng and D’Arcy2012; Valenzuela & Sachdev, Reference Valenzuela and Sachdev2006). Formal education has been found to be protective against dementia consistently in numerous studies and has been recognized as one of the proxies of cognitive reserve that can moderate the effects of brain damage or degeneration on cognitive functioning (Varangis & Stern, Reference Varangis, Stern, Thomas and Gutchess2020). As demonstrated in Figure 1.2b, many elderly Koreans, especially women, had low education and some were illiterate. Although many of the uneducated women learned to read and write at home or through the adult literacy program, such as Hangul School, later in life, the cognitive development of these older adults cannot be the same as those who were educated during childhood, which would have made a significant difference in the socioeconomic status and cognitive reserve of these women throughout their adult life. Therefore, it could be hypothesized that the high prevalence of dementia in elderly Korean women is largely due to their higher risk of dementia from insufficient formal education. This hypothesis is somewhat consistent with the observed prevalence of dementia and compulsory education history in South Korea and its regional neighbors with similar economic development during the twentieth century. For instance, Taiwan introduced compulsory education, including elementary and middle school education, in 1968 (Ministry of Education, Republic of China, 2021), while Japan added three years of middle school in 1947 to their compulsory primary education, which was established in the early twentieth century. Hence, most older adults who enjoyed longer life expectancy in these two countries during and after industrialization would have had at least nine years of formal education. In comparison, middle school became compulsory in Korea much later, in 2002 (Yang et al., Reference Yang, Gong and Kim2010), and many older Koreans who had been disadvantaged in youth were not able to receive secondary education, most of these being women.
Most of the illiterate and minimally educated Korean women grew up in rural communities steeped in strong patriarchal traditions where women’s education was discouraged, or they may have grown up in families that could not afford education for all their children (Park, Reference Park1993). Therefore, the preventive effect of compulsory secondary education would have been greater in older adults who grew up in small rural villages where the schools were all but absent, compared to those in cities where public middle schools were more accessible. Albeit in hindsight, the number of older Koreans with dementia would have been much lower, especially in women, if compulsory secondary education had been introduced one generation earlier. It should be mentioned, however, that more recent prevalence studies in both Taiwan and Japan found increased prevalence as the life expectancy has continually increased in both countries (Liu et al., Reference Liu, Li, Sun and Hu2019; Ninomiya et al., Reference Ninomiya, Nakaji, Maeda, Yamada, Mimura, Nakashima, Mori, Takebayashi, Ohara, Hata, Kokubo, Uchida, Taki, Kumagai, Yonemoto, Yoshida, Muto, Momozawa, Akiyama and Kiyohara2020; Sun et al., Reference Sun, Lee, Yang, Chen, Lin, Lin, Wang, Tang and Chiu2014).
On the other hand, dementia prevalence has been observed to be relatively high and increasing quickly in the low- and middle-income countries (LMICs), primarily situated in Latin America and South East Asia, which are mostly in the early stage of population aging (Prince et al., Reference Prince, Graham, Brodaty, Rimmer, Varghese, Chiu, Acosta and Scazufca2004, Reference Prince, Bryce, Albanese, Wimo, Ribeiro and Ferri2013). In fact, about two thirds of people with dementia live in LMICs, while most new incidences (71%) are expected to occur in these countries (Prina et al., Reference Prina, Mayston, Wu and Prince2019; World Health Organization, 2017). Global investigations on the risk factors of dementia including the LMICs, where secondary education is mostly not compulsory, found that less education is a risk factor for dementia (Livingston et al., Reference Livingston, Huntley, Sommerlad, Ames, Ballard, Banerjee, Brayne, Burns, Cohen-Mansfield, Cooper, Costafreda, Dias, Fox, Gitlin, Howard, Kales, Kivimäki, Larson, Ogunniyi and Mukadam2020), which is consistent with findings in South Korea.
1.3.1 Education, Cognitive Development, and Dementia Diagnosis
One of the first studies to reveal the cognitive functioning of older Koreans was the first project to establish norms for a dementia screening test in Korea. The Korean version of the Dementia Rating Scale (Chey, Reference Chey1998; Mattis, Reference Mattis1988), a popular test to assess the general cognitive functioning of older adults in North America, was developed and standardized for older Koreans over 55 years old (Chey et al., Reference Chey, Na, Park, Park and Lee1999). It was a small-scale study with 148 community-residing older adults in the Seoul-Gyeonggi region, recruited carefully from diverse districts so that their education and income were representative of the entire area. The normative study demonstrated that on average older Koreans (mean = 125.1, standard deviation [SD] = 9.5) performed significantly lower than their North American counterparts (mean = 137.3, SD = 6.9) and also revealed a greater range of performance. A strong education effect was also found in the Korean sample, in addition to the usual age effect found in the North American elderly population (Chey et al., Reference Chey, Na, Park, Park and Lee1999). These results were consistent with other studies with a wider range of education than the U.S. sample (Schmidt et al., Reference Schmidt, Freidl, Fazekas, Reinhart, Grieshofer, Koch, Eber, Schumacher, Polmin and Lechner1994), and were later replicated with a larger Korean sample (Suk et al., Reference Suk, Chey and Kim2010). In the first study, older Koreans who received higher education performed on par with their North American counterparts (men and women equally), but those who did not finish elementary education performed poorly on the tests. Moreover, men performed significantly better than women on average, but this disparity disappeared when the education effect was removed. Another interesting finding was the wider range of cognitive performance observed in older adults with low education, especially those with no education, with scores ranging from 68 to 140, a range that narrowed as the years of education increased (primary education 98~144; secondary education 110~144; higher education 120~144; Chey et al., Reference Chey1998), which could reflect the “scaffolding effect” of early education on people’s cognitive and brain development (Vygotsky, Reference Vygotsky1978), particularly for children living in environments not conducive to learning and cognitive development. Extremely low scores on cognitive tests were frequently observed in individuals with little formal education, who were often illiterate. Upon interviewing the participant and her family members, however, no significant cognitive or functional decline would be reported among illiterate women. Many of these older adults living in rural areas didn’t know or didn’t care about their addresses, frequently asked in mental state tests, but they were efficient in working at the farm or taking care of the household.
An urgent issue was raised, therefore, concerning the validity of dementia tools or neuropsychological tests developed in North America and Europe when assessing older Koreans with few years of education (Chey et al., Reference Chey1998, Reference Chey, Na, Park, Park and Lee1999, Reference Chey, Kim, Cho and Park2002; Cho et al., Reference Cho, Yang, Kim, Yang, Park and Chey2002). Since the items in dementia tests were matched to cognitive functioning for normal North American adults who had typically finished secondary education, limited performance due to lack of education or illiteracy had not been considered as a possibility when the tests were originally developed. It was a challenge to discriminate between mild dementia from a low cognitive performance due to lack of education (Chey et al., Reference Chey, Na, Tae, Ryoo and Hong2006).
Hence, in-depth investigation of the relationship between mind and brain was necessary not only at an individual but also at the population level. Findings from the Clock Drawing Test (CDT) performance of older adults with little education was a good example of how cautious an evaluator should be when testing older adults with little formal education, and this is especially true for those who are illiterate (Kim & Chey, Reference Kim and Chey2010). Despite involving multiple cognitive functions, the simplicity of CDT earned its popularity as a dementia screening tool in North America. A number of Korean clinicians, therefore, had expected the test to be a short but effective test for dementia screening in older Koreans. Compared to the automatic process of clock reading, it has been found that drawing a clock upon a verbal command with hands consistent with a specific time requires a complex array of neuropsychological functions, such as language comprehension, visuospatial abilities, executive functions, and the representation of a clock and its retrieval (Freedman et al., Reference Freedman, Leach, Kaplan, Winocur, Shulman and Delis1994). Therefore, the rationale of the test was that performance or errors on the CDT would be informative of the older testee’s overall cognitive functioning. Findings from dementia and other neurological patients in North America and Europe supported this assumption (Shulman, Reference Shulman2000).
A study investigating the CDT performance of normal elderly Koreans, however, found significant effects of education in this apparently simple test, most dramatically demonstrated in the illiterate older adults. More specifically, illiterate individuals not only scored very low on the CDT, but also made “conceptual errors,” which is characterized by the absence of the representation of a clock, namely, the conceptualization error (Kim & Chey, Reference Kim and Chey2010), which had been formally regarded as a hallmark of dementia of the Alzheimer’s type (see Figure 1.3). An illiterate elderly individual, however, would commit the error not because she had lost the representation of a clock but because she had never acquired it in her life (see Figure 1.3).

Figure 1.3 Conceptual errors on the Clock Drawing Test of uneducated older adults without dementia (A & B) and patients with dementia of the Alzheimer’s type (C & D).
Concept formation and other higher cognitive functions depend on the integrity of the prefrontal cortex and its connecting brain regions as well as on lengthy formal education (Chey & Park, Reference Chey, Park and Fuji2011). In the study, a number of older women who grew up in rural villages did not know how to tell the time from a clock at home nor read destinations on a bus or street signs throughout their lives (Kim & Chey, Reference Kim and Chey2010). Despite a significant limitation of mental faculty in modernized Korea, illiteracy had been very common in Korea and throughout the world until the nineteenth century. For instance, only 12% of the global population could read and write in 1820 (Roser & Ortiz-Ospina, Reference Roser and Ortiz-Ospina2016).
Most importantly, the clinical validity of the CDT was investigated in the study by comparing the test performance of mild Alzheimer’s dementia patients with those of normal controls. The comparison illustrated that the test performance did not adequately discriminate between the two groups in older adults with less than six years of education (Kim & Chey, Reference Kim and Chey2010). Further, the results showed that nonverbal tests could be as challenging for older adults with low education as the verbal tests. This was consistent with other observations of tests of visuospatial functioning, which were thought to be independent of culture and education. For example, copying and recalling nonverbal material, such as the Rey Complex Figure, proved to be too complicated and difficult for most older Koreans with less than high school education, and the figure stimuli needed to be simplified to be suitable for the population (Kim, Reference Kim2001; Park et al., Reference Park, Kim, Kim and Chey2011).
Despite the numerous challenges involved in developing dementia assessment tools that would be valid and reliable for an elderly population with a wide spectrum of education, a number of screening tools as well as more refined neuropsychological tests were developed in Korea during a short period of time (see for reviews; Chey & Park, Reference Chey, Park and Fuji2011; Kim & Chey, Reference Kim and Chey2016). Most recently, the Korean version of the Harmonized Cognitive Assessment Protocol (K-HCAP; Chey et al., Reference Chey, Lee, Kwak and Lee2022; Lee et al., Reference Lee, Kwak, Lee and Chey2020) has been developed, which can be utilized in international comparison between the Health and Retirement Study and its sister projects around the world (Langa et al., Reference Langa, Ryan, McCammon, Jones, Manly, Levine, Sonnega, Farron and Weir2020; Lee et al., Reference Lee, Banerjee, Khobragade, Angrisani and Dey2019).
1.3.2 Cognitive Aging and Dementia in Older Adults with Low Education
As standardized cognitive tests with age and education norms became available in Korea from the late 1990s, clinicians faced a difficult dilemma of whether to diagnose minimally educated individuals with low cognitive performance (LCP) as cases of mild cognitive impairment (MCI), a possible preclinical stage of dementia that was proposed as a clinical entity that could be prime for treatment (Petersen et al., Reference Petersen, Smith, Waring, Ivnik, Tangalos and Kokmen1999). More specifically, questions were raised whether the community-residing elderly individuals demonstrating a below-normal range of cognitive performance but not meeting dementia diagnosis criteria (Winblad et al., Reference Winblad, Palmer, Kivipelto, Jelic, Fratiglioni, Wahlund, Nordberg, Bäckman, Albert, Almkvist, Arai, Basun, Blennow, de Leon, DeCarli, Erkinjuntti, Giacobini, Graff, Hardy and Petersen2004) should be classified as MCI, which progresses to dementia in approximately 40% of cases (Mitchell & Shiri-Feshki, Reference Mitchell and Shiri-Feshki2009), two to seven times higher than those with normal cognition (Boyle et al., Reference Boyle, Wilson, Aggarwal, Tang and Bennett2006). As neuroimaging technologies advanced to measure neuropathologies in vivo (Mintun et al., Reference Mintun, Larossa, Sheline, Dence, Lee, Mach, Klunk, Mathis, DeKosky and Morris2006), studies found that the neuropathology of Alzheimer’s disease, the main disease to cause dementia, developed much earlier than its clinical symptoms, sometimes more than a decade before (Convit et al., Reference Convit, De Leon, Tarshish, De Santi, Tsui, Rusinek and George1997; Fox et al., Reference Fox, Warrington, Freeborough, Hartikainen, Kennedy, Stevens and Rossor1996; Jack et al., Reference Jack, Knopman, Jagust, Shaw, Aisen, Weiner, Petersen and Trojanowski2010; Kaye et al., Reference Kaye, Swihart, Howieson, Dame, Moore, Karnos, Camicioli, Ball, Oken and Sexton1997; Vemuri et al., Reference Vemuri, Wiste, Weigand, Shaw, Trojanowski, Weiner, Knopman, Petersen and Jack2009; Wolf et al., Reference Wolf, Hensel, Kruggel, Riedel-Heller, Arendt, Wahlund and Gertz2004). Therefore, understanding the nature of the LCP observed in older Koreans with no or minimal formal education became imperative and urgent to improve the diagnostic accuracy in a country where over 70% of adults over sixty-five years old received six or fewer years of formal education (KOSIS, 2006). Utilizing magnetic resonance imaging (MRI)-based volumetry, Chey et al. (Reference Chey, Na, Tae, Ryoo and Hong2006) examined the medial temporal lobe, which typically shows the first signs of atrophy in Alzheimer’s disease in community-residing older adults who have received no more than six years of education. Based on the fact that individuals with MCI show smaller medial temporal structures, such as the entorhinal cortex and the hippocampus (Convit et al., Reference Convit, De Leon, Tarshish, De Santi, Tsui, Rusinek and George1997; Wolf et al., Reference Wolf, Hensel, Kruggel, Riedel-Heller, Arendt, Wahlund and Gertz2004), it was reasoned that if the minimally educated older adults with LCP showed smaller volumes in the entorhinal cortex or hippocampus than those with normal cognitive performance, they are likely to be similar to the MCI cases observed in North America and should be classified as having MCI. Critical for storing information experienced by the individual (i.e., episodic memory), the volumes of these structures were compared in the two groups of older adults with minimal education but who did not show functional decline in everyday life. The study found no significant difference in the two medial temporal lobe structures when corrected with the size of the cranium, which suggested that the memory structures of the LCP did not show more atrophy in the brain regions vulnerable to Alzheimer’s disease, as found in the MCI cases. Moreover, upon one- and three-year follow-up evaluations, the LCP elderly individuals generally improved on the cognitive scores as they familiarized themselves with the paper-and-pencil tests, while the older adults with normal cognitive performance did not show such gains. These findings suggested that the LCP elderly individuals were unlikely to be MCI cases, who should have shown cognitive decline in the following assessment and converted to dementia at the rate of 5–10% annually (Mitchell & Shiri-Feshki, Reference Mitchell and Shiri-Feshki2009).
Whole brain volumes of the LCP older adults measured with the intracranial cavity volume, however, were significantly smaller than those with normal cognitive performance. Though unexpected, the finding was consistent with studies that reported significant correlation between whole brain size and education (Mortimer et al., Reference Mortimer, Snowdon and Markesbery2003) and also intelligence (Pietschnig et al., Reference Pietschnig, Penke, Wicherts, Zeiler and Voracek2015; Willerman et al., Reference Willerman, Schultz, Rutledge and Bigler1991; Witelson et al., Reference Witelson, Beresh and Kigar2006). A later study, utilizing automatic regional volumetry of the whole brain, found that the older adults with LCP had significantly smaller volumes in the bilateral precuneus and prefrontal cortices, both of which are cortical hubs with rich structural connections to associative cortices and regions closely associated with intelligence, self-awareness, and higher cognitive functions (Chey et al., Reference Chey, Kim, Stern, Shin, Byun and Habeck2016).
These findings significantly helped to reduce the ambiguity of interpreting the LCP of community-residing older adults who received little formal education. More specifically, the LCP older adults were not preclinical dementia patients but those who had low overall cognitive capacity throughout their lifetime, mostly due to lack of formal education. Since the two cognitive performance groups were matched in years of education and all participants had received no more than six years of education, it is likely that even informal education had not been available to the LCP individuals. This is consistent with the fact that more than half of them were illiterate, while none of the normal cognitive performance group were.
Although LCP in community-residing older adults with low education does not indicate incipient dementia, smaller whole brain and certain regional volumes could pose a risk for earlier manifestation of dementia in these individuals once neurodegeneration starts in the brain (Mori et al., Reference Mori, Hirono, Yamashita, Imamura, Ikejiri, Ikeda, Kitagaki, Shimomura and Yoneda1997; Wolf et al., Reference Wolf, Hensel, Kruggel, Riedel-Heller, Arendt, Wahlund and Gertz2004). Indeed, after six years of follow-up, older adults with LCP demonstrated more frequent cognitive decline and dementia, despite the fact that their cognitive performance improved in the first three years (Shin, Reference Shin2017; Shin, Chey, & Lee, ‘Is low cognitive performance a risk for dementia in elderly people who lack formal education?’ Unpublished manuscript). As LCP was only observed in older adults with few years of education and often illiterate, these results were consistent with studies that found greater risk of dementia in people with less education and illiteracy (Ashby-Mitchell et al., Reference Ashby-Mitchell, Burns, Shaw and Anstey2017; Norton et al., Reference Norton, Matthews, Barnes, Yaffe and Brayne2014; Rentería et al., Reference Rentería, Vonk, Felix, Avila, Zahodne, Dalchand, Frazer, Martinez, Shouel and Manly2019; Spada et al., Reference Spada, Stella, Calabrese, Bosco, Anello, Guéant-Rodriguez, Romano, Benamghar and Guéant2009). Formal education, a proxy of the cognitive reserve, moderates the clinical manifestation of dementia, delaying it by increasing the reserve capacity of the brain (Stern, Reference Stern2012). Similarly, low cognitive functioning or lower intelligence can also pose a risk for dementia (Russ, Reference Russ2018). Therefore, the risk of dementia for older Koreans would be high as a population, as a significant number of older women received no or minimal education and many had low cognitive functioning throughout their lifetime. More detailed discussions regarding the moderating effects of cognitive reserve, whose proxies include years of education and intelligence, will be discussed in Chapter 5.
1.3.3 Other Modifiable Risks Associated with Compressed Modernization
Rapid societal change can accompany psychological and physical challenges and adversities for its constituents that can be harmful to their brain health. Instability in social positions, unsafe working and living environments that could result in brain injuries and exposure to neurotoxins, and air pollution are modifiable social factors that increase the risk of dementia.
Financial Insecurity and Social Isolation in Late Life
Many older Koreans face economic hardship after retirement, as the introduction of the pension system has been slow and spotty with slim support that is frequently insufficient to support late life. Weak social investment by the state and heavy reliance on families for the care and support of the older generation, amid financial crisis and the emergence of new social paradigms characterized by nuclear families and dense urbanization, have left Koreans very vulnerable in late life (Chang, Reference Chang2018). Traditionally, the eldest son and his family lived with his parents and supported and took care of his parents in late life (mosigi), as he inherited the land or means of living. A family system based on Confucian agricultural society had to go through major change under the compressed modernization process. The migration of children to cities and the rising urban real-estate prices made cohabitating with adult children for support and care very difficult if not impossible for many parents. Moreover, the first financial crisis in the late 1990s, which required IMF intervention, devastated the South Korean economy and drove many companies and families into bankruptcy. Many disadvantaged adult children could not support nor take care of their aging parents as the economy became unfavorable, and the aging parents at the turn of the century found themselves with insecure support or care from their adult children for the first time in Korean history. A majority of aging Koreans were shattered in that they were not prepared financially, socially, or emotionally to be independent in late life. It was possible that they may have invested too heavily in their children’s education, and many were left with little or no financial reserve to support themselves in late life. In fact, the poverty rate of elderly Koreans is around 43.4%, the highest among the Organisation for Economic Co-operation and Development (OECD) member countries and about three times the average of 14.8% (OECD, 2021). But most importantly, this seismic shift in the familial system was accompanied by frequent conflicts and estrangement between family members, accelerating the disintegration of the traditional social fabric of the country.
Today, 35% of older South Koreans report that they have no one to discuss matters with during difficult times, the highest among OECD member countries, whose average is 11.5% (OECD, 2021). Undoubtedly, social isolation among older Koreans stems from disconnection from family members, including their adult children. Being estranged from one’s children has been found to be a particularly significant stressor among older Koreans in studies investigating the role of stress in cognitive decline in community-residing older adults (Lee, Reference Lee2005). Considering the traditional parental expectation towards adult children, this was frequently accompanied by significant grief, depression, and disappointment, which contributed to cognitive decline in many older Koreans (Kwak, Reference Kwak2006; Lee, Reference Lee2005; Park et al., Reference Park, Chey and Kim2014). Especially vulnerable were older adults who moved to the city in their late life for health and financial reasons or those with low education who had weaker social support from neighbors and relatives, whom they could rely on when family members were unavailable.
Although social isolation and loneliness have been a significant social problem in high-income countries, such as Japan, Denmark, and the U.K., it has been recognized as a serious issue in South Korea only recently. Increasingly, social isolation among older citizens is being recognized as a major social issue, as a significant number of older adults have been found dead alone by strangers, referred to as godoksa, meaning solitary death. Various risk factors, such as economic hardship, chronic illness, alcoholism, social isolation, unemployment, estranged family relations, single-person households, and living in an urban area (Kim & Park, Reference Kim and Park2017), have been associated with godoksa or suicide among older Koreans. It is undeniable that these tragedies stem from a rapid disintegration of the family-based social support system that would have provided care and support for older citizens in previous generations. The ironic “individualization of the older adults without the individualism” proposed by Chang (Reference Chang2018, p. 108) aptly characterizes the socially disconnected and lonely plight many older Koreans are confronted with today, especially those with lower socioeconomic standing. The following chapters, especially Chapter 7, review and discuss dementia and other health risks posed by loneliness and social disconnection in late life, while Chapter 12 reviews social programs and policies that are geared to reduce social isolation and its ill-health effects, especially dementia.
High-Risk Environment for Brain Injury and Damage
Considering that traumatic brain injury is a major risk for dementia (Plassman et al., Reference Plassman, Havlik, Steffens, Helms, Newman, Drosdick, Phillips, Gau, Welsh-Bohmer, Burke, Guralnik and Breitner2000; Shively et al., Reference Shively, Scher, Perl and Diaz-Arrastia2012), older Koreans who have experienced a moderate to severe head injury (e.g., in factories, on construction sites, or in vehicular accidents) would be two to four times higher at risk for dementia. Moreover, the risk of dementia increases exponentially with repeated injuries, as the risk increases twofold with a single injury but fourfold for the second injury (Li et al., Reference Li, Li, Li, Zhang, Zhao, Zhu and Tian2017; Schneider et al., Reference Schneider, Selvin, Latour, Turtzo, Coresh, Mosley, Ling and Gottesman2021). Although studies reporting detailed and accurate statistics were not available for traumatic brain injury, the fact that South Korea has maintained high rates of death due to both traffic and industrial accidents until very recently suggests that a history of brain injury would be quite prevalent among older Koreans. It is unfortunate that necessary precautions to prevent major injuries or exposure to toxic chemicals have not been seriously enforced in Korea, partly due to ignorance, but also for the sake of efficiency or productivity. Frequent traffic accidents have endangered the brain health of pedestrians due to automobile-centered traffic regulations in the past. Moreover, construction sites with scant safety precautions have been major sites for falls and injuries, which if not fatal would have resulted in head injuries. Safety regulations have changed in recent years, but the history of brain injuries among older adults remains, and it is likely to have significantly increased the risk of dementia for elderly Koreans.
Korean farmers were not safe from the hazards of industrialization, since they were exposed to pesticides that were introduced extensively from the 1960s when the “new village movement” (saemael undong) began. The pesticides that were imported and distributed widely since the time of the KEDP purported to increase the productivity of the crops significantly, but without adequate precautions concerning the toxicity of the chemicals. Organophosphate pesticide (OPP), one of the most common pesticides around the world, has been found to contain neurotoxins and was banned for residential use in the U.S.A. in 2001. Considering that rice, the major crop in Korea, requires labor-intensive farming, it is likely that rice farmers had been exposed to the chemicals quite heavily in the past when the health risks of the pesticides were unknown to the public. Prolonged exposure to OPP has been found to increase the risk for dementia (Killin et al., Reference Killin, Starr, Shiue and Russ2016), in addition to the increased risks for cardiovascular and respiratory diseases (Hung et al., Reference Hung, Yang, Li, Lin, Chang, Sung and Tai2015; Peiris-John et al., Reference Peiris-John, Ruberu, Wickremasinghe and van-der-Hoek2005) and cancer (Alavanja et al., Reference Alavanja, Hoppin and Kamel2004; Lerro et al., Reference Lerro, Koutros, Andreotti, Friesen, Alavanja, Blair, Hoppin, Sandler, Lubin, Ma, Zhang and Freeman2015). Since the detrimental effects of the pesticides on dementia risks tend to be stronger in less educated people (McDowell et al., Reference McDowell, Hill and Lindsay1994), the increased risk for dementia posed by the OPP should be examined more seriously in rural Korea.
Recently, air pollution and particulate pollutants have been found to be detrimental to brain health and to accelerate neurodegeneration, which appears to increase the risk of dementia (Livingston et al., Reference Livingston, Huntley, Sommerlad, Ames, Ballard, Banerjee, Brayne, Burns, Cohen-Mansfield, Cooper, Costafreda, Dias, Fox, Gitlin, Howard, Kales, Kivimäki, Larson, Ogunniyi and Mukadam2020). In a systematic review of studies from many countries, exposure to fine ambient particulate matter (PM2.5), nitrogen dioxide (NO2), and carbon monoxide, very common air pollutants from traffic exhaust fumes and thermal power generation in South Korea (Wolf et al., Reference Wolf, Emerson, Esty, de Sherbinin and Wendling2022), have been found to be consistently associated with dementia risks (Peters et al., Reference Peters, Ee, Peters, Booth, Mudway and Anstey2019). In recent years, air pollution has become a major health hazard and stressor for South Koreans, as the nation’s air quality ranks 119 among 180 countries and is likely to be a significant risk for dementia in the future.
1.4 Conclusions
Recently, the World Health Organization (2017) announced the “Global action plan on the public health response to dementia 2017–2025.” As global population aging is advancing quickly, the number of people with dementia is increasing rapidly. It is projected to be 75 million in 2030 and 132 million by 2050, compared to 47 million in 2015. Further, about 60% of people with dementia live in LMICs, and most new incidences (71%) are expected to occur in these countries. Rapid aging following compressed modernization and industrialization in South Korea appears to make it the foremost case of the global trend of speedy population aging in LMICs. Although South Korea has been recently categorized as an advanced economy and a high-income country (World Bank, 2021a), its case bears similarity with the more recently aging countries.
South Korea is one of the fastest-aging countries in world history, and its dementia population is growing swiftly. The events were in large part inadvertent results of the expeditious economic development plan and compressed modernization carried out in the latter part of the twentieth century. The government-driven economic development plan that spanned a generation from 1962 to 1996 was extremely successful economically but would have significant side effects, such as rapid population aging and high dementia prevalence. Moreover, the Korean government’s heavy reliance on the family and private sectors for important social investment, such as education and care, inadvertently resulted in disintegration of social support from family that would contribute to the increasing public health problems.
The unintended outcomes of expeditious industrialization have been discussed in terms of population aging. The role of education in cognitive test performance and in preventing dementia during cognitive aging has been illustrated with cognitive and brain aging studies on older Koreans with a wide range of education levels. Further, other modifiable risks of dementia associated with compressed modernization, such as financial insecurity and social isolation in late life, which have not been addressed sufficiently in South Korea, needed mentioning.
The case of South Korea has implications for LMICs, which are now experiencing rapid aging and alarming incidence of dementia. There is an argument for pacing industrialization to ensure social infrastructures do not disintegrate without the introduction of alternative systems so that older adults can be adequately supported in their late life. Further, having policies to establish compulsory secondary education accessible to both girls and boys as well as to protect adults’ brain health from environmental and industrial hazards appear to be important measures to reduce the incidence of dementia in the future.