Although healthy cooking programmes for youth have demonstrated positive impacts on food preferences and dietary behaviours(Reference Cunningham-Sabo and Lohse1–Reference Hersch, Perdue and Ambroz3), their influence on measures beyond nutrition, such as quality of life and emotional well-being, is unknown. Preliminary research among adults suggests that positive psychosocial changes frequently occur during culinary programmes focused on developing cooking skills, and these changes may not be entirely attributable to nutrition(Reference Farmer, Touchton-Leonard and Ross4,Reference Iacovou, Pattieson and Truby5) . While the specific pathways in which cooking interventions influence psychosocial outcomes are uncertain(Reference Farmer, Touchton-Leonard and Ross4), evidence suggests that improvements in social interaction(Reference Iacovou, Pattieson and Truby5), executive functioning(Reference Provencher, Demers and Gelinas6,Reference Tchanturia, Lounes and Holttum7) and cooking self-efficacy(Reference Garcia, Reardon and McDonald8) are likely to be important contributors. Considering initial findings related to the psychosocial benefits of culinary interventions for adults(Reference Farmer, Touchton-Leonard and Ross4), an investigation of the influence of youth-focused cooking programmes on emotional health of children is warranted.
Mental health difficulties have increased among children and adolescents over the past several decades(Reference Kyu, Pinho and Wagner9), with the implementation of effective prevention and early intervention strategies for youth now national priority focus areas(Reference Whitney and Peterson10). In 2016, reports indicated that approximately 7·7 million US children under 18 years of age had at least one diagnosed mental health disorder, including depression, anxiety or attention-deficit and hyperactivity disorder, and approximately half of these children never received treatment from a mental health professional(Reference Whitney and Peterson10). In Flint, Michigan, a low-income urban area that continues to struggle with a population-wide lead-in-water public health crisis(Reference Hanna-Attisha, LaChance and Sadler11), there are heightened concerns about behavioural health impacts on children exposed to contaminated water(Reference Fortenberry, Reynolds and Burrer12–Reference Hanna-Attisha and Kuehn14). In addition to the deleterious effects of lead toxicity on developmental and biological processes among children(Reference Silbergeld15), previous reports have shown higher levels of stress, anxiety and depression among those exposed to human-induced emergencies(Reference Fortenberry, Reynolds and Burrer12,Reference Palinkas, Petterson and Russell16,Reference Lima, Pai and Santacruz17) . Because mental health issues frequently begin during childhood or adolescence(Reference Khalid, Williams and Reynolds18–Reference Avison20), there is an urgent need to develop scalable prevention strategies that reach children and adolescents, particularly those at highest risk, to address not only physical health but also emotional well-being.
Consistent evidence indicates that diet and nutrition play an important role in the prevention of certain mental health conditions among youth(Reference Khalid, Williams and Reynolds18,Reference Wu, Zhuang and Li21,Reference O’Neil, Quirk and Housden22) . More specifically, a healthy diet, characterised by high intakes of fruits, vegetables and whole grains, has been associated with better emotional health and quality of life among children and adolescents(Reference Khalid, Williams and Reynolds18,Reference Wu, Zhuang and Li21) , while unhealthy dietary patterns, characterised by a ‘Western’ diet high in processed meats, saturated fats and refined grains, have been associated with poorer mental health(Reference O’Neil, Quirk and Housden22). Beyond dietary factors, one recent study determined that better self-reported cooking ability was associated with lower levels of depression and fewer emotional difficulties among adolescents, suggesting that learning to cook could foster development of important life skills that encourage adolescents to contribute positively to their families(Reference Utter, Denny and Lucassen23). Together, this evidence suggests that cooking programmes, designed to improve dietary behaviours and cooking skills of youth, could positively influence quality of life and psychosocial health of participants. However, these specific outcomes have not been explored among children and adolescents(Reference Farmer, Touchton-Leonard and Ross4). Health-related quality of life (HRQoL) is a multidimensional concept with domains related to overall well-being as well as physical, mental, emotional and social functioning(24,Reference Varni, Burwinkle and Seid25) . Although the measure does not reflect the level of mental distress or depression an individual experiences, it is an important outcome that addresses the impact of health status on quality of life.
Flint Kids Cook, a healthy cooking programme for youth, was created in October 2017 amid concerns about child nutrition during a lead-in-water public health crisis in Flint, Michigan, USA. In direct response to caregiver requests for child-focused cooking programmes(Reference Saxe-Custack, Lofton and Hanna-Attisha26), a team of local chefs, registered dietitians and researchers developed Flint Kids Cook. This intervention was grounded in social cognitive theory, which explains behaviour changes based on interactions between one’s personal and environmental systems(Reference Bandura27–Reference Montgomery29). Flint Kids Cook focused on improving child knowledge, skills and self-efficacy for cooking healthy foods through interactive nutrition education and food preparation activities. Caregiver support and access to healthy foods were also a programme focus, achieved through take-home educational materials, recipes and child-friendly cooking utensils(Reference Nixon, Moore and Douthwaite30). The programme was facilitated by a credentialed chef who, with a registered dietitian’s assistance, taught classes inside a farmers’ market commercial kitchen. The current study had two aims. The first aim was to examine changes in HRQoL among youth who participated in Flint Kids Cook. The second aim was to examine the association between changes in HRQoL and changes in cooking self-efficacy, attitude towards cooking (ATC) and dietary intake.
Methods
Study design
This pre-post research study surveyed participants in Flint Kids Cook, a 6-week healthy cooking programme for children and adolescents at a local farmers’ market, at baseline and programme exit.
Study setting and recruitment
Flint, Michigan, is an industrial city with approximately 100 000 residents. The birthplace of General Motors, Flint, fell into an extreme economic recession following the decline of the American automobile industry(Reference DeWitt31). Similar to many low-income cities throughout the USA, Flint lacks resources and nutritional options(Reference Saxe-Custack, Lofton and Hanna-Attisha26,Reference Saxe-Custack, Lofton and Hanna-Attisha32–Reference Mayfield, Carolan and Weatherspoon34) . Approximately 58 % of children live in poverty in Flint(35) (poverty level for a household of four in 2018 was a household income of $25 100(36)). The community continues to struggle with an unsafe drinking water crisis that has negatively impacted the physical and emotional well-being of children living in this low-income, urban area(Reference Hanna-Attisha, LaChance and Sadler11,Reference Fortenberry, Reynolds and Burrer12,Reference Zahran, McElmurry and Sadler37) . Children were recruited into the programme through posters and pamphlets at local paediatric offices and partnering community sites and were eligible to participate if they (1) were 8–18 years of age, (2) spoke English and (3) had not participated in a prior session. Although residency in Flint was not a requirement to participate, the majority of children who enrolled reported living at a Flint address. Registration and cooking incentives were provided free of charge.
Intervention
Flint Kids Cook, conducted in a farmers’ market commercial kitchen, included nine total hours of instruction over six consecutive weeks (one session per week). During this introductory-level class, the chef taught students proper techniques for chopping and slicing, measuring and mixing ingredients, as well as sautéing, roasting and baking. Recipes and curriculum content were guided by the US Department of Agriculture’s (USDA’s) MyPlate, with each 90-min session dedicated to a specific food group (Table 1)(Reference Post, Haven and Maniscalco38). Students worked in small teams to prepare two dishes that represented the food group discussed in class and were encouraged to practice at home with a ‘homework bag’ that was distributed at the conclusion of each of three classes (1, 3 and 5). The reusable bag contained a recipe and ingredients, as well as a feedback sheet to share their experiences with food preparation at home. Feedback sheets were returned to class facilitators at the start of subsequent sessions (i.e. 2, 4 and 6). The last session in the 6-week series featured a celebratory family dinner prepared by students. While caregivers did not actively participate in the classes, they were invited to watch sessions through a window outside the farmers’ market kitchen.
Table 1 Flint Kids Cook lessons, topics and activities

Process evaluation was utilised for formative purposes to understand the extent to which Flint Kids Cook was delivered as designed (fidelity), incorporated the appropriate content and number of lessons (dose delivered), and reached intended participants (reach). To assess fidelity and dose, several unannounced site observations were video-recorded and reviewed by researchers. To ensure that the programme was reaching the target audience, enrolment in each 6-week session required that at least 60 % of participants lived at a Flint address. Attendance sheets as well as participant feedback sheets were completed at the conclusion of each of six sessions.
Data collection
Health-related quality of life
Pediatric Quality of Life Inventory Child Self-Report was used to measure HRQoL(Reference Varni and Limbers39). The survey instrument consists of twenty-three total items with three summary scores as well as four multidimensional scales (physical functioning, emotional functioning, social functioning and school functioning) that show adequate reliability and validity, with internal consistency reliability for the total scale score (total HRQoL summary score; alpha = 0·88 child), physical health summary score (alpha = 0·80 child) and psychosocial health summary score (alpha = 0·83 child) acceptable for group comparisons(Reference Varni, Seid and Kurtin40). A 4·4-point change in total scale score for the child self-report is considered clinically meaningful(Reference Varni, Burwinkle and Seid25). One previous study explored the use of PedsQL Generic Core Scales as a measure of paediatric population health. In the study, authors determined that 1 sd below the population mean was a meaningful cut-off point for at-risk status for impaired HRQoL relative to the population sample(Reference Varni, Burwinkle and Seid25). For the child self-report, the total scale score cut-off point was 69·7. The authors further explained that children with newly diagnosed cancer on treatment self-report a total scale score of 68·9, while children with rheumatic conditions self-report a total scale score of 72·1. Therefore, scores approximating 1 sd below the population mean represent total scale scores similar to children with a severe chronic health condition(Reference Varni, Burwinkle and Seid25).
In the current study, baseline and exit measures of HRQoL were assessed through child self-report immediately prior to the first session and at the conclusion of the final session. On each occasion, children and adolescents completed the self-administered survey after a facilitator introduced it to the class. Facilitators were available to assist younger children as needed. Survey items such as ‘It’s hard for me to walk more than one block’ assessed physical functioning; items such as ‘I feel afraid or scared’ assessed emotional functioning; items such as ‘I have trouble getting along with other kids’ assessed social functioning; and items such as ‘It’s hard to pay attention in class’ assessed school functioning. Response options (‘Never’, ‘Almost Never’, ‘Sometimes’, ‘Often’ and ‘Almost Always’) were reverse-scored and linearly transformed to a 0–100 scale, with higher scores indicating better HRQoL. To create scale scores, the mean was computed as the sum of the items over the number of items answered.
Cooking self-efficacy and attitude towards cooking
Cooking self-efficacy, which refers to a child’s judgement over their capability to prepare various foods, is important for behaviour change(Reference Bandura27), while ATC demonstrates the child’s overall desire to cook. These variables are central to social cognitive theory and have been used in prior studies to evaluate the effectiveness of cooking and nutrition programmes for children(Reference Cunningham-Sabo and Lohse2,Reference Lohse and Cunningham-Sabo41) . Baseline and exit measures of cooking self-efficacy and ATC were assessed through child self-report immediately prior to the first session and at the conclusion of the final session using a validity-tested 8-item self-efficacy and 6-item ATC survey. This survey previously demonstrated internal consistency and test–retest reliability such that individual test–retest scores were significantly correlated (P < 0·001); r = 0·80 (self-efficacy) and 0·82 (ATC)(Reference Lohse, Cunningham-Sabo and Walters42). In the current study, children and adolescents completed the self-administered survey after a facilitator introduced it to the class. Facilitators were available to assist younger children as needed. Eight survey items such as ‘I can cut food’ and ‘I can follow recipe directions’ measured cooking self-efficacy with the following response options: ‘YES!,’ ‘Yes,’ ‘No,’ ‘NO!’ and ‘Not Sure’(Reference Lohse, Cunningham-Sabo and Walters42). Scores related to cooking self-efficacy ranged from 8 to 40, with lower scores denoting greater self-efficacy. Six survey items describing activities such as ‘measuring ingredients’ and ‘making food with family’ measured ATC with the responses ‘Really Like,’ ‘Kind of Like,’ ‘Don’t Like,’ ‘Really Don’t Like’ and ‘Not Sure’(Reference Lohse, Cunningham-Sabo and Walters42). Scores related to ATC ranged from 6 to 30, with lower scores indicating a more positive attitude.
Dietary intake
Dietary data from children were collected via the Block Kids Food Screener, which has demonstrated good relative validity for children and adolescents(Reference Hunsberger, O’Malley and Block43). The 41-item assessment examined frequency and quantity of foods and beverages consumed during the previous week and was administered by a class facilitator before the first class was initiated and again at the conclusion of the final class. On each occasion, children and adolescents completed the self-administered survey after a facilitator introduced it to the class. Facilitators were available to assist younger children as needed. Guided by previous literature that has demonstrated an association between quality of life and certain dietary factors among children and adolescents(Reference Khalid, Williams and Reynolds18,Reference Wu, Zhuang and Li21,Reference O’Neil, Quirk and Housden22) , we measured this association with regard to several key dietary variables (i.e. whole fruits, fruit juices, vegetables, whole grains, saturated fats and added sugars). Block Online Analysis System provided nutrient estimates and number of servings by food groups. These data were used to determine participants’ mean daily intake of total fruits, fruit juices, vegetables, whole grains, saturated fats and added sugars.
Data analysis
Paired sample t-tests were used to examine change in HRQoL, cooking self-efficacy, ATC and dietary measures from baseline to programme exit. Pearson’s correlations examined associations between change in HRQoL summary scores from baseline to programme exit and change in mean daily intake of key dietary factors, change in cooking self-efficacy and change in ATC. Similarly, Pearson’s correlations examined associations between change in psychosocial health summary scores from baseline to programme exit and change in mean daily intake of key dietary factors, change in cooking self-efficacy and change in ATC. Change was calculated by subtracting programme exit scores from baseline scores. Independent sample t-tests were used to compare change in HRQoL by key participant characteristics. Statistical Package for the Social Sciences (version 25, IBM Corp.) was used to manage and analyse data with significance set at P < 0·05. Children were permitted to skip questions on the surveys and may not have been in attendance on the first or last day of class, when baseline and exit measures were completed (a few children absent from class those days did complete surveys over the phone); thus, for each analysis, children were included when all relevant data were available and excluded when data were missing. The current project was deemed exempt by the institutional review board approval from Michigan State University.
Results
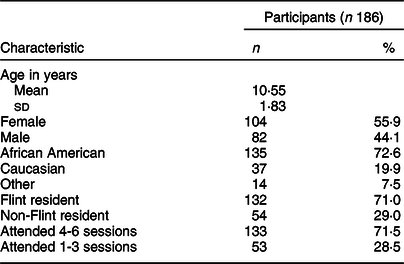
Among the 186 children who participated in Flint Kids Cook from October 2017 to February 2020 (mean age 10·55 ± 1·83 years; range 8–15 years), the majority were African American (72·6 %), Flint residents (71·0 %) and female (55·9 %). Most children (71·5 %) attended at least four of six total sessions (Table 2); however, some had lower attendance. Caregivers noted transportation challenges as well as competing activities/schedules as reasons for lower attendance. There were no differences between children who attended four or more classes and those who attended three or fewer in terms of gender (P = 0·655), age (P = 0·572) or city of residence (P = 0·054); however, there was a difference in ethnicity, with 65·2 % of African American participants, 86·5 % of Caucasian participants and 92·3 % of participants who did not identify as African American or Caucasian attending four or more classes (P = 0·009). Additionally, there was no difference in age (P = 0·150), ethnicity (P = 0·945), residence (P = 0·086) or gender (P = 0·770) between those children who completed at least one of the assessments and those children who did not complete any of the assessments.
Table 2 Characteristics of children and adolescents who participated in Flint Kids Cook from October 2017 to February 2020
Health-related quality of life
A total of 129 children completed the Pediatric Quality of Life Inventory at baseline and programme exit. As shown in Table 3, improvements (P < 0·001) were observed in mean HRQoL summary score from baseline (77·22 ± 14·27) to programme exit (81·62 ± 14·43). Mean psychosocial health summary scores also improved significantly (P = 0·001) from baseline (74·68 ± 15·68) to programme exit (79·04 ± 16·46). Similarly, significant improvements were observed in each of four multidimensional scales: physical (P = 0·016), emotional (P = 0·002), social (P = 0·037) and school functioning (P = 0·002). Furthermore, the change in HRQoL summary score from baseline to programme exit did not differ significantly based on gender (P = 0·628), ethnicity (P = 0·203), age category (P = 0·321) or city of residence (P = 0·874). In a multiple regression model, ethnicity, age and gender were not significant predictors for change in HRQoL summary score (P = 0·216) or for change in psychosocial health summary score (P = 0·173). Additionally, there was no correlation between number of sessions attended and the primary outcomes of HRQoL summary score and psychosocial health summary score (r = –0·074 and r = –0·003, respectively).
Table 3 Assessment of Flint Kids Cook from October 2017 to February 2020
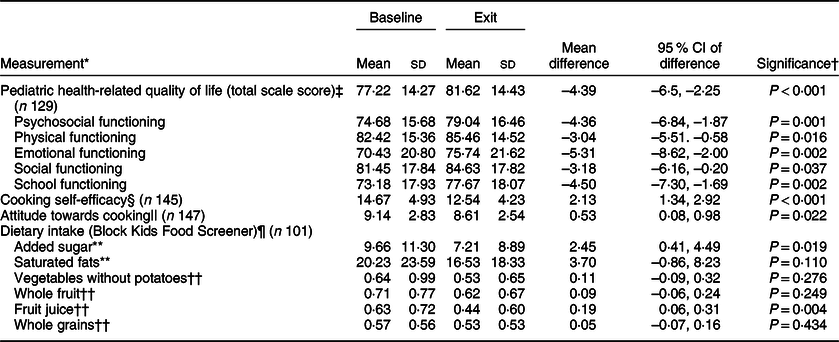
* Children and adolescents completed self-administered surveys after a facilitator introduced them to the class. Facilitators were available to assist younger children as needed. Children were also permitted to skip items and may not have been in attendance on the first or last day of class, when baseline and exit measures were completed; thus, for each analysis, children were included when all relevant data were available and excluded when data were missing.
† P < 0.05 is considered statistically significant.
‡ Paediatric health-related quality of life was measured using the Pediatric Quality of Life Inventory: Child Self-Report consisting of 23 items that use a scale with five Likert response options, ‘never’, ‘almost never’, ‘sometimes’, ‘often’ and always’, corresponding to scores of 100, 75, 50, 25 and 0, respectively. This evaluation tool is reverse-scored and linearly transformed, with a higher score (scale of 0 to 100) indicating better health-related quality of life.
§ Cooking skills were measured with five multiple choice response options (YES!, Yes, No, NO! and Not Sure; scored as 1, 2, 4, 5 and 3, respectively). These responses were provided for each of eight cooking skills survey items. Possible scores ranged from 8 to 40 with lower scores indicating greater self-efficacy in relation to cooking skills.
|| Attitude towards cooking was assessed by five multiple choice response options (Really Like, Kind of Like, Don’t Like, Really Don’t Like and Not Sure; scored as 1, 2, 4, 5 and 3, respectively). These responses were provided for each of six cooking attitude survey items. Possible scores ranged from 6 to 30 with lower scores indicating a more positive attitude towards cooking.
¶ Dietary intake was measured using a Block FFQ consisting of forty-one food items with the selected frequency ‘none last week’, ‘1 day last week’, ‘2 days last week’, ‘3–4 days last week’, ‘5–6 days last week’ and ‘every day last week’.
** Measured in grams.
†† Measured in servings.
Cooking self-efficacy and attitude towards cooking
Among the children who completed cooking-specific assessments, significant improvements were observed in mean cooking self-efficacy scores (P < 0·001) as well as mean ATC scores (P = 0·022) (Table 3). We further examined the relationship between change in HRQoL summary scores and change in cooking self-efficacy and ATC. There was a significant correlation between change in HRQoL summary score and change in ATC (r = –0·194, P = 0·025) as well as change in cooking self-efficacy (r = –0·234, P = 0·008). Additionally, change in cooking self-efficacy was significantly correlated with change in psychosocial health summary score (r = –0·273, P = 0·002).
Dietary intake
Mean daily intake of added sugars decreased significantly (P = 0·019) from baseline (9·66 ± 11·30) to programme exit (7·21 ± 8·89). Similarly, mean daily intake of fruit juices decreased significantly (P = 0·004) from baseline (0·63 ± 0·72) to programme exit (0·44 ± 0·60). Changes in other key dietary factors were not significant (Table 3).
To determine whether changes in dietary intake were related to changes in HRQoL summary scores, we examined correlations of change in HRQoL to change in mean daily intake of key dietary factors (fruits, vegetables, whole grains, saturated fats and added sugars). Change in HRQoL summary score was not correlated with change in mean daily intake of whole fruits (r = 0·035, P = 0·727), fruit juices (r = 0·082, P = 0·417), vegetables (r = 0·096, P = 0·343), whole grains (r = 0·045, P = 0·657), saturated fats (r = 0·121, P = 0·232) or added sugars (r = 0·133, P = 0·188). Similarly, change in psychosocial health summary score was not correlated with key dietary factors.
Discussion
To the knowledge of the authors, this study is the first to report significant improvements in HRQoL among children and adolescents who participated in a healthy cooking programme. Central to our findings were modest but clinically meaningful increases in quality of life and psychosocial health summary scores(Reference Varni, Burwinkle and Seid25) as well as each of four multidimensional scales, including physical, social, emotional and school functioning. These significant improvements occurred over a period of 6 weeks and were consistent across gender, age and ethnicity. Findings suggest that Flint Kids Cook positively influenced quality of life among participating children and adolescents, most of whom were African American and residents of a low-income, urban community in the midst of a public health crisis. Although previous research has not assessed changes in quality of life and psychosocial health of children who participated in healthy cooking programmes, findings support earlier evidence demonstrating psychosocial benefits of culinary interventions for adults(Reference Farmer, Touchton-Leonard and Ross4). In addition to a sense of accomplishment upon learning new skills, the previous studies with adults noted the importance of socialisation and working in teams(Reference Farmer, Touchton-Leonard and Ross4), factors that may also have played a role in improving HRQoL among participants in the current study.
Similar to previous healthy cooking programmes among youth(Reference Cunningham-Sabo and Lohse2,Reference Jarpe-Ratner, Folkens and Sharma44–Reference Muzaffar, Metcalfe and Fiese46) , participants in Flint Kids Cook reported improvements in cooking self-efficacy. Moreover, changes in quality of life and psychosocial health of young participants were associated with changes in cooking self-efficacy. According to social cognitive theory, knowledge of health risks and benefits creates a precondition for change, but beliefs of self-efficacy (i.e. one’s judgement over their capability to change(Reference Bandura27)) are needed to overcome barriers to adopting and maintaining healthy lifestyles(Reference Bandura28). Although the specific pathway is unclear, earlier studies among adults have suggested that improving cooking self-efficacy may be a means to improve self-esteem by affecting intrapersonal barriers to healthy living(Reference Farmer, Touchton-Leonard and Ross4). Interestingly, psychosocial changes that occurred in the current study were not associated with changes in diet or nutrition but instead were related to notable improvements in cooking self-efficacy.
The current study suggests that the benefits of healthy cooking interventions for youth may extend beyond diet and nutrition. Previous research has similarly demonstrated the mental health benefits of youth gardens(Reference Lam, Romses and Renwick47,Reference Carney, Hamada and Rdesinski48) , with one recent study indicating that youth associate feelings of relaxation with gardening, growing food and cooking(Reference Lam, Romses and Renwick47). Earlier research has also determined that self-reported cooking ability is positively associated with better family connections, greater mental well-being and lower levels of self-reported depression among adolescents(Reference Utter, Denny and Lucassen23). Cooking programmes for children may provide an opportunity for ‘hands-on’ experiences that may be practiced at home, surrounded by family. With evidence indicating that frequent family meals are inversely associated with alcohol and substance use, violent behaviour, and feelings of depression or thoughts of suicide among adolescents(Reference Harrison, Norris and Obeid49,Reference Skeer and Ballard50) , it is reasonable to assume that culinary programmes for children and adolescents may influence emotional well-being. Accordingly, cooking programme objectives for youth should include not only improvements in key dietary variables but also improvements in quality of life and psychosocial health with regular assessment of these important outcome measures among young participants.
Previous evidence indicates that there are associations between healthy dietary patterns and better mental health among children(Reference Khalid, Williams and Reynolds18,Reference Wu, Zhuang and Li21) . Furthermore, the relationship between poor diet quality and mental health concerns in youth, including depression, anxiety and attention deficit and hyperactivity disorder, has been well documented(Reference Wu, Zhuang and Li21). However, the results of the current study demonstrated that improvements in quality of life and psychosocial health of participants were not associated with changes in dietary behaviours, which included reductions in mean daily intake of added sugars and fruit juices. This important result, which supports previous studies that have assessed psychosocial benefits of culinary programmes for adults(Reference Farmer, Touchton-Leonard and Ross4,Reference Chen, Lee and Chang51) , suggests that cooking programmes for youth are likely to foster positive changes that may be unrelated to diet and nutrition. This particular finding is noteworthy considering that traditional assessments of cooking programmes for children tend to evaluate their success based largely upon nutrition-related outcomes(Reference Hersch, Perdue and Ambroz3,Reference Muzaffar, Metcalfe and Fiese46,Reference Jacob, Motard-Belanger and Provencher52) . The current study suggests that cooking programmes for youth may provide important psychosocial benefits to children and adolescents even in the absence of comprehensive dietary improvements.
In addition to the lack of a control group, there were limitations of the current study. Our sample was small and specific to one low-income, urban community. As a result, findings may not be generalisable. It is important to note, however, that although we did not have a measure or proxy for socioeconomic status, Flint Kids Cook is located in a community where the majority of children are living in poverty, suggesting that other low-income communities may benefit similarly from such programmes. We did not assess prior cooking experience, which may have influenced participant responses. Additionally, the accuracy of the Block Kids Food Screener may be limited by recall bias, but a trained research assistant was consistently available to children when completing this instrument in an effort to minimise this particular study limitation. Although multiple regression modelling does not indicate that age, gender or ethnicity are predictors for change in HRQoL summary scores or for change in psychosocial health summary scores, we recognise that we are limited by our sample size and the group sizes in these characteristics.
Strengths of this study include the use of validated tools to measure HRQoL, cooking self-efficacy, ATC and dietary intake. While there was no follow-up beyond programme end to determine whether findings would persist, this study provides an important first look at improved HRQoL among children and adolescents who participated in a healthy cooking programme. Access to the programme was also critically important. In 2014, the Flint Farmers’ Market relocated to the downtown area as an intentional effort to increase the percentage of people coming by bus from the city’s poorest neighbourhoods for general groceries(Reference Sadler53). The thoughtful introduction of Flint Kids Cook at the downtown farmers’ market site was a deliberate effort to facilitate easy access to the programme. Future studies exploring participant and caregiver opinions of the programme will provide insight into the factors contributing to the increases in HRQoL, cooking self-efficacy and ATC, as well as opportunities for improvement. We encourage similar programmes in other low-income, urban settings to consider incorporating methods to capture baseline and exit measures from children with lower attendance in an effort to specifically examine the dose–response relationship.
Conclusions
Given the rise in mental health difficulties among young people over the past several decades(Reference Kyu, Pinho and Wagner9), there is an urgent need to design innovative public health programmes that broadly reach children and adolescents to support both physical and psychosocial health, especially in low-income settings where such interventions may be most beneficial. The current study demonstrates the positive impact of a scalable healthy cooking programme on quality of life and psychosocial health of youth. Flint Kids Cook could be modelled in similar low-resource communities.
Acknowledgements
Acknowledgements: The authors would like to thank Chef Sean Gartland for recipe development and facilitation of Flint Kids Cook as well as Sarah Egan and Mallory Goldsworthy for nutrition instruction and support. Financial support: This project was supported by Michigan Health Endowment Fund (R-1710-141906); and Flint H2O project (The Michigan Health Endowment Fund and Flint H2O project had no role in the design, analysis or writing of this article). Conflict of interest: None. Authorship: A.S.-C. conceived the study, study design and analysis; led analysis of the data; and led all writing and drafting of the manuscript. J.L. contributed significantly to data analysis, interpretation of results and drafting of the manuscript. M.H.-A. assisted in conceptualisation of the study and the drafting and revising of the manuscript. C.D. participated in data collection and drafting and revising of the manuscript. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the Michigan State University Institutional Review Board. Written informed consent was obtained from all subjects.






