The new type of virus seen (SARS-CoV-2) in the Hubei region of China in December 2019 was named Coronavirus-19 disease (COVID-19).Reference Baloch, Baloch and Zheng1 This disease not only affected the whole of China due to its high contagiousness in a short period of one month but also spread rapidly to many different countries, and the World Health Organization (WHO) reported on March 11, 2020, that the world was facing a serious problem.Reference Iuliano, Chang, Patel, Threlkel, Kniss and Reich2 The virus, which caused severe morbidity and mortality, caused severe health problems such as respiratory tract infection, pneumonia, kidney failure, heart attack, and even multiple organ failure. WHO declared the epidemic as a pandemic.Reference Erol, Kayıkçıoğlu and Kılıçkap3, Reference Zhang, Dong and Liu4 This decision created global concern and fear. For this reason, many restrictive measures have been taken by governments worldwide, including curfews that affect daily life, and many organizations have been canceled.Reference Hellewell, Abbott and Gimma5-Reference Zhen, Li and Li7
Following the declaration of the pandemic, individuals’ physical behavior has been restricted within the framework of the measures taken by countries. As a result of these restrictions, individuals face health problems that may develop due to inactivity (e.g., weight gain, cardiorespiratory problems). In addition, restricting social life along with an inactive life can cause mental problems.Reference Gupta, Grover and Basu8, Reference Richter, Ferraz‐Rodrigues and Schilling9 The COVID-19 outbreak and its pandemic nature have caused widespread anxiety and fear. Inevitably, the feelings of anxiety, fear, and uncertainty about the future caused by the pandemic process will have negative effects on human psychology. These anxieties also change the quality of life by causing fatigue and sleep problems.Reference Fazeli, Zeidi and Lin10, Reference Dana, Nodeh and Salehian11
People have gone through a difficult process due to contracting the virus, experiencing losses due to COVID-19, and continuing uncertainty about the future and the present. Its effects continue today. It appears that there are significant relationships between university students contracting COVID-19 after the pandemic, the fear of losing a family member, and an increase in intolerance of uncertainty.Reference Duman12 COVID-19 phobia significantly increases socialization anxiety, especially among university students.Reference Heumann, Helmer and Busse13 Anxiety, depression, sleep quality, and physical activity level may also be related.Reference Puccinelli, da Costa and Seffrin14 As a result, staying active and maintaining an exercise routine is important to maintain mental and physical health during the COVID-19 pandemic.Reference Zhao, Wang and Wang15
COVID-19, which limits life in many areas to reduce transmission, has also caused restrictions in education, causing schools worldwide to be unable to provide face-to-face education for a long time.Reference Gopal, Singh and Aggarwal16 This has increased the use of digital platforms and social media applications in education and affected students’ academic performance.Reference Ghosh, Khatun and Khanam17 In this regard, this study aimed to evaluate the association of university students’ COVID-19 phobia, pain, quality of life and sleep, physical activity, and fatigue levels on students’ achievement.
Methods
This study was planned and carried out as a cross-sectional study. All students studying at Eastern Mediterranean University Faculty of Health Sciences between the ages of 18-25 were included in the study. Questionnaires prepared via Google Forms were sent to 1011 students via Microsoft Teams (MS Teams), which is used as a distance education tool. Individuals who had internet problems did not complete all questionnaires.Individuals who had musculoskeletal, neurological, or respiratory problems that would affect their physical activity level were excluded from the study. The authors claim that all procedures used in this study adhere to the Helsinki Declaration and the ethical standards of relevant national and institutional committees on human experimentation. This study was approved by the Eastern Mediterranean University Research and Publication Ethics Board with the decision numbered SBF00-2021-0016. The students were informed about the study before the study, and their informed consent was obtained. All data were collected between November 2021 and February 2022.
Individuals’ age, height, weight, body mass ındex (BMI), gender, smoking and alcohol usage, work status, and grade point average (GPA) during the distance education period were questioned. It was questioned whether the person had caught the COVID-19disease, whether COVID-19had caused any damage, the physical activity status during the pandemic process, and the effects of the pandemic process on the individual’s daily life.
Assessment of Pain
Pain felt in the last week was evaluated using the Pain Quality Assessment Scale (PQAS). The scale, whose Turkish validity and reliability were determined by Şahin et al., consisted of 20 questions evaluating pain severity and quality, including “deep” and “superficial” pain. On a Likert-type scale ranging from 1 to 10, 0 indicates “none” for the specified complaint, and “10” indicates “the most unbearable, most severe” pain for the specified complaint. The lowest score on the scale can be 20, and the highest score can be 200. As the score increases, the pain intensity increases. Internal validity assessed by Cronbach alpha was obtained between 0.730-0.930.Reference Jensen, Gammaitoni and Olaleye18, Reference Şahin, Bodur and Salli19
Assessment of Fatigue
The fatigue severity of the participants was evaluated using the Fatigue Severity Scale (FSS), which consists of 9 items. Each FSS item consists of statements that are scored on a seven-point Likert-type scale ranging from 1 (“strongly disagree”) to 7 (“strongly agree”). Higher scores indicate increased fatigue. The Turkish validation of the Fatigue Severity Scale was found to be valid and reliable (ICC > 0.80).Reference Ferentinos, Kontaxakis and Havaki-Kontaxaki20, Reference Armutlu, Korkmaz and Keser21
Assessment of Distance Education Satisfaction
Perceived ease of use and perceived usefulness dimensions in the technology acceptance model of student satisfaction in distance education were evaluated with the Online Learning Systems Acceptance Scale (OLSAS).Reference Durnali, Orakçi and Toraman22 The scale, consisting of 6 items, is designed as a 7-point Likert type. The lowest score that can be obtained from the scale is 6, and the highest score is 42. The scale was developed and adapted by Ilgaz, and its reliability coefficient is 0.80- 0.96.Reference Özkanan and Erdoğan23
Assessment of Coronavirus-19 Phobia
The participants’ phobia levels towards COVID-19 were evaluated with the COVID-19 Phobia (CP19-S) Scale. This scale was developed to examine the effects of phobia on the somatic, social, economic, and psychological sub-dimensions. It consists of 20 items and 4 factors. CP19-S, rated on a 5-point Likert type ranging from “strongly disagree” to “strongly agree,” is evaluated according to the extent to which people agree with the statements stated in the items in the past week. The total score is between 20-100 points, and high scores indicate a high level of sub-dimensions and general coronaphobia. The Turkish validity and reliability of the scale was conducted by Arpacı et al., and the Cronbach Alpha value was found to be 0.92, and the reliability coefficient was 0.94.Reference Arpaci, Karataş and Baloğlu24, Reference Akarsu, Akgüllü and Şengül25
Assessment of Physical Activity Level
Weekly physical activity level was assessed using the International Physical Activity Questionnaire Short Form (IPAQ-SF). It consists of 7 questions that provide information about time spent walking, moderate and vigorous activities, and time spent sitting. The sum of duration (minutes) and frequency (days) of walking, moderate and vigorous activity is used when calculating the total score. A score is obtained by multiplying the metabolic equivalent of task (MET) value corresponding to duration, frequency, and basal metabolic rate (Walking 3.3 MET, moderate physical activity 4 MET, vigorous physical activity 8 MET) as “MET-min/week.” Total scores be classified according to low, medium, or high physical activity level. The Turkish version of the IPAQ short forms was found reliable and valid by Saglam et al.Reference Cihan, Bozdag and Var26, Reference Saglam, Arikan and Savci27
Assessment of Sleep Quality
Jenkins Sleep Scale (JSS) was used to evaluate subjective sleep quality. It includes 4 items in the last 4 weeks: (a) difficulty in initiating sleep, (b) awakening during the night, (c) awakening during sleep with difficulty in maintaining sleep, and (d) awakening exhausted in the morning despite having slept as usual. Rating is done on a 6-point Likert scale (not at all = 0, 1–3 days = 1, 4–7 days = 2, 8–14 days = 3, 15–21 days = 4, and 22–28 days = 5).Reference Ornat, Martínez-Dearth and Chedraui28 The score that can be obtained from the scale varies between 0 and 20, with higher scores indicating more disturbed sleep. The Cronbach’s alpha of the JSS was 0.862, and Turkish validity and reliability were determined by Duruöz et al.Reference Duruöz, Erdem and Gencer29
Assessment of Quality of Life
Participants’ quality of life was evaluated with Short Form-36 (SF-36). It is a self-assessment tool consisting of 36 items that provide evaluation under eight domains: (1) physical functioning, social functioning, emotional role, physical role, bodily pain, vitality, mental health, and general health perception. Scores changed from 0 to 100 for each domain separately. The high scores that the quality of life increases positively. The reliability and validity studies for the Turkish version of SF-36 were performed by Kocyigit et al. Cronbach’s alpha value of the eight domains varies between 0.73–0.76.Reference Ware and Sherbourne30, Reference Kocyigit, Aydemir and Fisek31
Statistical Analysis
Data were analyzed with SPSS 26 and AMOS 26. The significance level was taken as .05. Continuous variables were shown as mean (X) and standard deviation (SD), while categorical variables were shown as frequency (n) and percentage (%). While the relationship between continuous variables was calculated with the Pearson correlation coefficient, the relationship between the categorical variables was calculated with the Spearman correlation coefficient. The correlation coefficient was interpreted as a 0.00-0.29: weak or low; 0.30-0.49: medium; 0.50- 1.0: high or strong relationship.Reference Shahriari32 To evaluate the effects of age, BMI, gender, living place, smoking, alcohol usage, employment status, presence of disease in the family, COVID-19 status, and staying home time, PQAS, FSS, JSS, IPAQ, C19P-S, SF-36, and OLSAS on student achievement (GPA), multiple regression analysis with backward selection method was performed. Variance inflation factor (VIF) was used to control multicollinearity. In addition, Path Analysis was performed to evaluate the direct and indirect effects of scale scores on achievement (Figure 1).

Figure 1 Path analysis chart.
Results
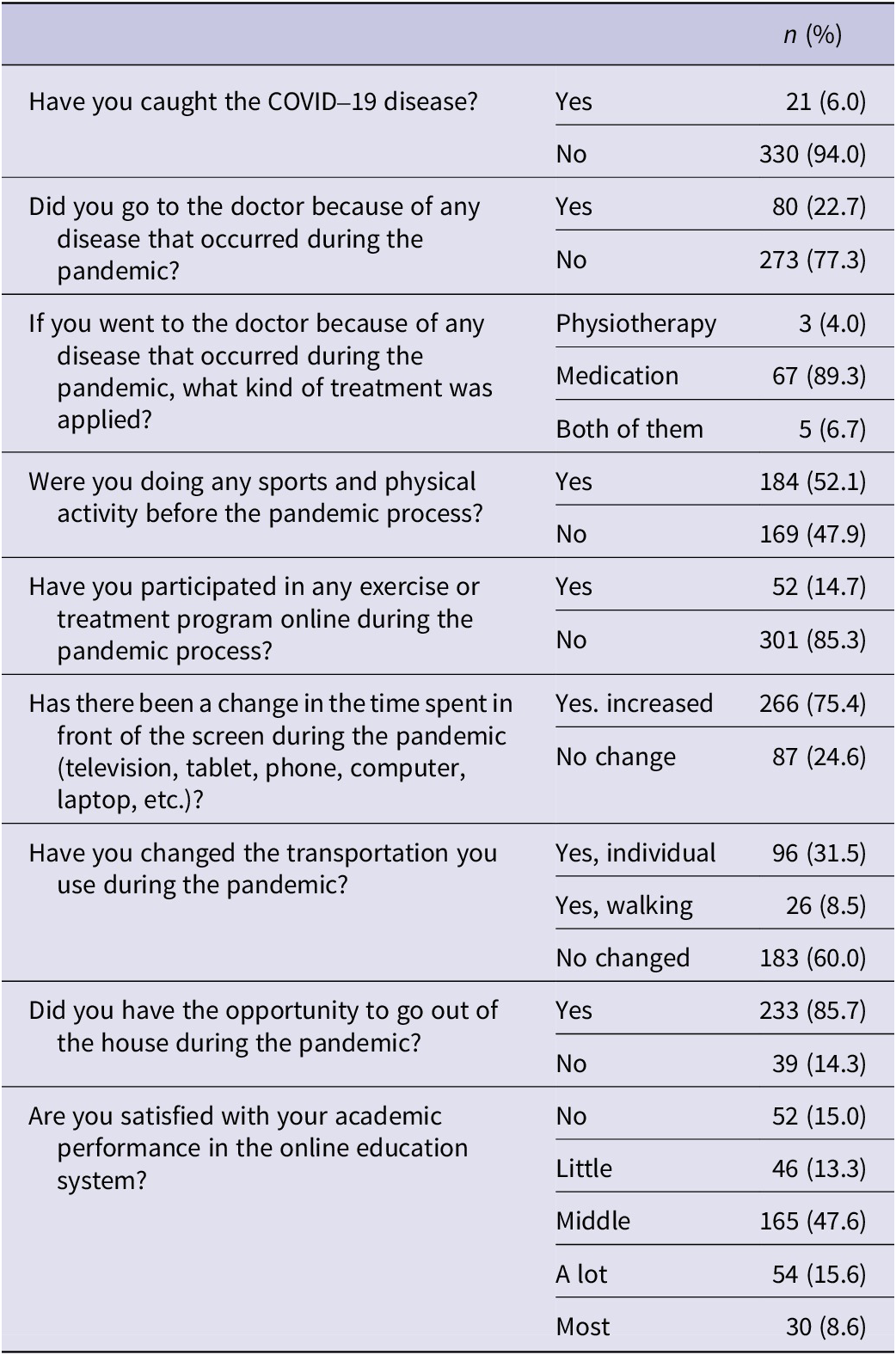
As a result, 151 students who met the exclusion criteria, 207 students who did not fill out the forms completely, and 300 students who did not respond to the Google form link sent via Microsoft Teams were excluded from the study. Thus, the study was completed with 353 participants. The mean age, height, weight, BMI, and GPA values of them were 21 ± 2 years, 171± 10 cm, 67 ± 16 kg, 22.89 ± 4.02 kg/cm2, and 2.73 ± 0.568 respectively. Of the participants, 39.7% were male and 60.3% female, 29.5% consumed cigarettes, and 36.5% consumed alcohol. Information and changes related to alcohol consumption, working, and disease status are also included in Table 1. In addition, the answers given by asking questions related to weight loss, physical activity change, mask usage, transportation, and academic performance satisfaction during the pandemic are given in Table 2.
Table 1. Clinical characteristics of the participants

* Calculated over the consumers. BMI: Body Mass Index; GPA: Grade Point Average; n: Count; %: Percentage; X: Mean; SD: Standard Deviation
Table 2. Participant information related to the pandemic process
While a weak negative correlation was found between the GPA score and BMI (r = −0.200; P = 0.003), a weak positive correlation was found between the GPA score and cigarette usage (r = 0.194; P = 0.004), alcohol usage (r = 0.178; p = 0.008), studying status (r = 0.152; P = 0.024), and SF-36 social function (r = 0.189; P = 0.005). Our constructed model was significant in the multiple linear regression (F = 5.025; P<0.001). The determination coefficient related to the model was 19.2%. In addition, age (B = 0.045; t = 2.075; P = 0.040), BMI (B = -0.200; t = 2.974; P = 0.004), SF-36 physical (B = 0.128; t = 2.701; p = 0.008), SF-36 psychological (B = 0.057; t = -2.549; p = 0.012) and SF-36 social variables (B = 0.189; t = 2.401; P = 0.018) were found statistically significant (Table 3).
Table 3. The results of Correlation and Multiple Linear Regression Analysis for GPA

R 2 = 0.192; F (P) = 5.025 (< 0.001) BMI: Body Mass Index; FSS: Fatigue Severity Scale; C19P-S: COVID-19 Phobia Scale; IPAQ: International Physical Activity Questionnaire; PQAS: Pain Quality Assessment Scale; OLSAS: Online Learning Systems Acceptance Scale; JSS: Jenkins Sleep Scale; SF-36: Short Form-36; B: Unstandardized regression coefficient; β: Standardized regression coefficient.
* < 0.05;
** < 0.001;
a Pearson Correlation Coefficient;
b Spearman Correlation Coefficient.
Since the scale scores are related to each other, path analysis was performed to determine the indirect effects on other variables besides their direct effects on success (Figure 1). Increased COVID-19 phobia decreased sleep quality (B = 0.042; P = 0.010), physical role in quality of life (B = 0.239. P = 0.048), and pain in quality of life (B = 0.163. P = 0.038) parameters while increasing fatigue (B = 0.151; P<.001) and distance learning efficiency (B = 0.105. P = 0.002). An increase in sleep quality increases fatigue severity (B = 0.478; P<0.001) and pain quality score (B = 1.103; P<0.001), while an increase in fatigue severity decreases physical activity (B = 21.597; P = 0.006) quality (B = 0.529; P<0.001). While physical activity increased energy (B = 0.001; P = 0.027) and psychological parameters of quality of life (B = 0.001, P = 0.037), the increase in pain quality decreased the psychological parameter (B = 0.091; P = 0.043). The psychological (B = -0.005; P = 0.032) and social scores (B = 0.004; P<0.001) of quality of life were also effective on the GPA. While the increase in the psychology score decreases the success average, the increase in the social score increases the success average (Table 4).
Table 4. Path coefficients of the recursive model

SE: Standard Error; CR: Critical Ratio; B: Unstandardized regression coefficient; β: Standardized regression coefficient; BMI: Body Mass Index; FSS: Fatigue Severity Scale; C19P-S: COVID-19 Phobia Scale; IPAQ: International Physical Activity Questionnaire; PQAS: Pain Quality Assessment Scale; OLSAS: Online Learning Systems Acceptance Scale; JSS: Jenkins Sleep Scale; SF-36: Short Form-36; GPA: Grade Point Average.
* < 0.05;
** < 0.001.
Discussion
This study investigated the achievement of university students and the factors associated with it while battling with the COVID-19 pandemic and during distance education. It was determined that the level of student achievement during the pandemic process was related to age, BMI, and the physical, psychological, and social aspects of quality of life. In addition, it was determined that the increasing COVID-19 phobia worsened the quality of sleep, affected the physical role and pain parameters that would affect the quality of life, and increased fatigue and distance education satisfaction.
The fear of death during the pandemic caused more protective behavior in young adults compared to the elderly population, and therefore they remained in social isolation for a longer period.Reference Pasion, Paiva and Fernandes33 Vella et al. reported that age plays a role in academic success in web-based courses, especially since younger students are less prepared in terms of self-discipline and motivation, which can increase student performance and retention in the virtual academic environment.Reference Vella, Turesky and Hebert34 In this study, the protective behaviors shown by university students in distance education during the pandemic caused isolation, which led to an increase in the importance and motivation given to distance education, causing them to achieve better academic achievement, especially as they got older. In case of any disease that will cause social isolation in the future, it should be aimed to raise awareness among students of all ages about distance education and keep their achievement level high.
While 52.1% of the university students who participated in our study were doing physical activity before the pandemic, only 14.7% were seen exercising during the isolation period. In particular, it was stated that 75.4% of these people spent more time sitting at home. The literature has shown that there is a negative relationship between physical activity and BMI.Reference Hemmingsson and Ekelund35, Reference So, Swearingin and Robbins36 The decreased level of physical activity during the pandemic also poses a risk factor for increased BMI. In the meta-analysis conducted by He et al., similar to our study results, it was found that there was a weak negative correlation between BMI and academic achievement.Reference He, Chen and Fan37 Increasing BMI may decrease the success level of university students. For this reason, postural exercises should be recommended to students between classes, especially during distance education. In our study, it was also observed that fatigue increased with COVID-19phobia. Decreased physical activity level also causes fatigue.Reference Güneş and Demirer38 Distance education to increase physical activity should also be targeted and motivated to reduce students’ fatigue during the pandemic.
The rapid spread of the coronavirus and the immediate measures taken in response to the COVID-19 pandemic have negatively affected the quality of life of individuals of different ages by causing changes in their performance regarding healthy lifestyles. According to the World Health Organization, quality of life is defined as “the individual’s perception of his or her position in life, within the cultural context and value system he or she lives in, and concerning his or her goals, expectations, parameters and social relations.”39 Individuals infected with COVID-19disease may experience various symptoms, especially fever, cough, shortness of breath, muscle pain, sore throat, headache, chest pain, and abdominal pain.Reference Weng, Su and Wang40 Although only 6% of the participants in our study caughtCOVID-19, 85.3% did not engage in physical activity, and 75.4% were found to have increased the time they spent in front of the screen. The lifestyle changes of individuals due to COVID phobia and/or post-COVID-19 disease, quality of life is affected especially by physical role and pain domains, and the level of success decreases with the worsening quality of life.
Improvements in academic achievement due to increased social relations are a highly important issue.Reference Olivier, Archambault and De Clercq41 Social support means meeting psychological needs through communication, and its importance for achievement is frequently stated in the literature. This theory is emphasized as “self-determination theory.”Reference Ryan and Deci42 Previous studies have shown that family, friends, instructors, and similar support resources provide positive relationships with students’ well-being and achievement.Reference Kiuru, Wang and Salmela-Aro43, Reference Tomás, Gutiérrez and Pastor44 It has also been found that the decrease in social relations during the pandemic negatively affects students’ achievement.Reference Stang-Rabrig, Vogel and Forciniti45 Our study reached similar results to the literature and showed that the improvement of the social domain of the quality of life contributes to the improvement of academic achievement.
Emotional or behavioral reactions are demonstrated during the COVID-19 pandemic. Psychiatric disorders such as intolerance toward uncertainty, perceived vulnerability to disease, anxiety tendency, depression, and post-traumatic stress disorder occur. Individuals with COVID-19 phobia begin to think that they are infected with the disease by misinterpreting their physical condition due to health anxiety. COVID-19phobia also causes significant impairment in daily life functionality, with fear of contracting the virus causing COVID-19, leading to significant anxiety, increased reassurance and safety-seeking behaviors, and avoidance of public places and situations. Berdida et al. stated that as anxiety related to COVID-19 increases, quality of life decreases for nursing students.Reference Berdida and Grande46 Keener et al. found that students’ intense workload in online courses, changing course expectations, financial difficulties, and concerns about the impact of distance learning on their grades affected them, especially psychologically.Reference Keener, Hall and Wang47 This study observed that COVID-19 phobia changed the effectiveness of distance learning, and achievement was also affected by the quality of life. It is suggested that academic success and quality of life are related, that even in face-to-face education, the student provides most of the active learning with pre-learning and post-learning activities, and that projects/homework should also be given to increase the student’s autonomy and participation.Reference Spivey, Stallworth and Olivier48 To increase the level of success of the students and reduce the stress they experience in distance education, apart from different educational techniques, it should be aimed to increase academic success by making instructors more tolerant in giving grades, ensuring that students attach more importance to education by taking into account their changing social lives, and increasing the options of taking/not passing courses.
In this study, which was conducted during the period of curfew and social isolation after the COVID-19 epidemic, collecting information using social networks to comply with social distance principles is the strength of our study, but it also has some limitations. First of all, using the self-administered questionnaire may have affected the students’ answers due to their changing living conditions, COVID-19 phobia, and changing mental states after social isolation. Secondly, the differences in the participants’ living opportunities and economic conditions may have affected their understanding of quality of life. Although this study was planned to be carried out in different universities, it was limited only to single university because education was suspended due to the pandemic, and there is no distance education model in other universities in our country. Based on the results and limitations of this study, it is recommended that future studies be conducted in the form of a multi-cohort study, including distance education programs that increase physical activity and achievement levels for students by physiotherapists, and interviews via phone video call, if possible, to reduce the bias of online assessments.
Conclusion
In preparing for future disasters such as earthquakes and infectious diseases, it is necessary to analyze and take appropriate measures to improve students’ academic achievement, physical activity level, and quality of life. Distance education, theuse of which increased during the COVID-19 pandemic, continues today. This study aimed to examine students’ academic achievement and related factors and found that age, BMI, and physical, psychological, and social domains of quality of life are associated with distance education’s achievement level.
Acknowledgments
We thank the participants for their willingness to participate in this study.
Author contribution
The study was conceptualized and supervised by the primary investigator OD, and designed by all the authors. OD, BK, and EC collected all data and contributed to data analysis, processing, interpretation, and drafting of the manuscript. The literature search was conducted by OD and EA. The original manuscript was written by OD, EM, EA, and BK. The final manuscript was critically reviewed by OD and finally approved by all the authors.
Competing interest
None declared.







