Introduction
Unilateral tonsil enlargement is a relatively common presentation to the ENT out-patient clinic. A multi-centre Turkish study of 1784 cases reported the prevalence of unilateral tonsil enlargement in children to be 1.7 per cent.Reference Akcay, Kara, Dagdeviren and Zencir1 For paediatric patients, the clinician's prime concern is ruling out the presence of tonsillar lymphoma. Asymmetry of the palatine tonsils has been reported as the most common symptom of tonsillar lymphoma in the paediatric population.Reference Guimaraes, de Carvalho, Correa and Gusmao2 In the past, even when unilateral tonsil enlargement is asymptomatic, conventional management has included urgent histology tonsillectomy. However, a recent case series and literature review revealed no diagnoses of tonsillar lymphoma after 322 paediatric histology tonsillectomies.Reference Jones, Burnside, McPartland, Markey, Fallon and De3
The National Prospective Tonsillectomy Audit of 2005 reported a 3.5 per cent rate of post-operative haemorrhage.4 Whilst more contemporary surgical techniques such as Coblation® have been associated with a lower incidence of post-operative haemorrhage,Reference Amin, Bhargava, Prentice, Shamil, Walsh and Tweedie5 it is unlikely that such techniques would be widely used in histology tonsillectomy. Therefore, the morbidity from complications such as post-tonsillectomy haemorrhage remains a concern in patients with unilateral tonsil enlargement, especially in the more vulnerable paediatric population.
The investigation and management of unilateral tonsil enlargement in adult patients could perhaps be considered more complex. Where a primary oropharyngeal mucosal malignancy (usually a squamous cell carcinoma (SCC)) is suspected based on clinical examination findings of a discreet mass or a tonsil with an abnormal or ulcerated appearance, a biopsy or tonsillectomy for diagnosis followed by staging imaging is a well-established course of investigation. However, there exists a group of adult patients, presenting with unilateral tonsil enlargement and often no other ‘red flag’ symptoms, with an asymmetric but benign-appearing tonsil. Two British papers were identified describing this population. Addison et al. described 106 cases of adult unilateral tonsil enlargement in the absence of any other suspicious examination findings; no malignant diagnoses were reported following histology tonsillectomy.Reference Addison, Whittaker, Maddox, Pelser and Watts6 However, Oluwasanmi et al. detected 2 cases of tonsillar lymphoma in 68 otherwise asymptomatic patients aged over 16 years with unilateral tonsil enlargement.Reference Oluwasanmi, Wood, Baldwin and Sipaul7
Although a recent Trilogical Society ‘Best Practice’ guideline suggested reserving histology tonsillectomy for unilateral tonsil enlargement cases only when they present with lymphadenopathy, rapid growth or systemic symptoms,Reference Hwang, Kaye, Waxman and Friedman8 anecdotal evidence in the author's region suggests that many patients with uncomplicated benign-appearing unilateral tonsil enlargement are undergoing surgery as a routine investigation.
Most patients scheduled for histology tonsillectomy because of unilateral tonsil enlargement have undergone clinical examination alone. The BrodskyReference Brodsky9 and FriedmanReference Friedman, Tanyeri, La Rosa, Landsberg, Vaidyanathan and Pieri10 scoring systems are validated methods for classifying palatine tonsil size, but these are subjective, and inter-observer variability can occur.Reference Kumar, Valenzuela, Kozak, Ludemann, Moxham and Lea11 In addition, a high proportion of clinically asymmetric tonsils are not significantly different in size once excised.Reference Van Lierop, Prescott, Fagan and Sinclair-Smith12 A question can therefore be raised over the accuracy of clinical examination in diagnosing true unilateral tonsil enlargement.
From the existing body of evidence, it is not clear whether the risk of histology tonsillectomy is justified in order to rule out malignancy in each case of unilateral tonsil enlargement. The authors believe it especially pertinent to examine this risk given the increased number of patients waiting for consultant-led treatment in the UK's National Health Service over the past two years of the coronavirus disease 2019 pandemic.13
Study aims
These were: (1) to establish the number of malignant diagnoses identified by histology tonsillectomy performed for unilateral tonsil enlargement in a South Wales population; (2) to identify any factors in patients’ clinical history or examination associated with a malignant outcome; (3) to establish the rate of haemorrhage following histology tonsillectomy in this population; and (4) to examine the relationship between clinical examination of tonsil asymmetry and excised tonsil volume.
Materials and methods
Ethical considerations
Approval was gained for retrospective data collection from each health organisation as a service evaluation. All data were anonymised from source and stored securely.
Data collection
Histopathology databases were used to identify patients who had undergone histology tonsillectomy. For each case, a retrospective review of electronic notes was performed to record: demographics; documented factors from history-taking and examination by the general practitioner and otolaryngologist, including the side of the subjectively larger tonsil; social risk factors; intra-operative findings; presence or absence of post-operative haemorrhage and subsequent management; final histopathological diagnosis; and size of excised tonsil. The factors considered during the history-taking and examination of patients are summarised in Table 1. A history of ‘rapid enlargement’ was described as enlargement of a tonsil over a period of 12 weeks or less. The ‘B symptoms’ were described as weight loss and/or abnormal fever or sweating.
Table 1. Patient history and clinical examination factors and their relationship to malignant histopathological outcome*
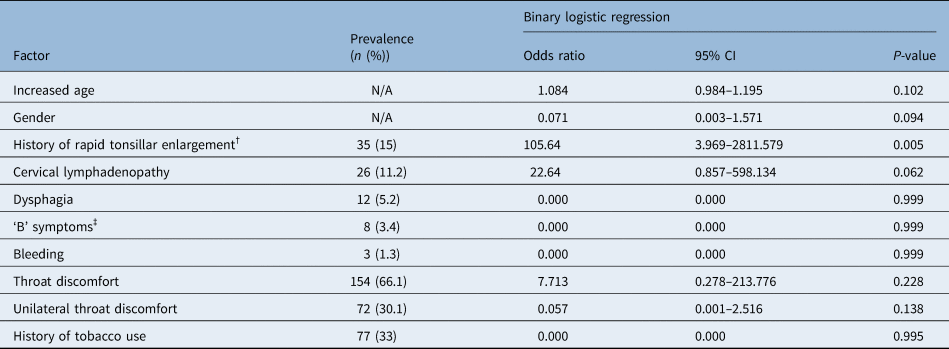
*Determined following histology tonsillectomy for unilateral tonsil enlargement in adult patients (n = 233). †‘Rapid enlargement’ was described as enlargement of a tonsil over a period of 12 weeks or less. ‡Weight loss and/or abnormal fever or sweating. CI = confidence interval; N/A = not applicable
A standardised three-axis measurement had been carried out during histopathological examination of each excised tonsil. These axes were multiplied to calculate estimated tonsil volumes for each case.
Exclusion criteria
The exclusion criteria were designed to ensure that cases were a true reflection of the population with unilateral tonsil enlargement, in the absence of any ‘red flag’ signs of oropharyngeal malignancy or other recognised cause for unilateral tonsil enlargement. Exclusion criteria were: clinical findings suspicious for a malignant lesion (e.g. ulceration or exophytic mass); presence of a discreet lesion not contiguous with the normal lymphoid tissue of the palatine tonsil (e.g. a lesion suspicious for papilloma); excision performed for parapharyngeal or peritonsillar abscess; excision performed as part of an investigation for an unknown primary head and neck cancer; excision performed to investigate a lesion avid on positron emission tomography/computed tomography imaging; and excision performed as a ‘remnant’ tonsillectomy.
Cases were to be included where tonsillectomy had been arranged for another reason (e.g. recurrent tonsillitis or obstructive sleep apnoea (OSA)), but tonsils had been sent for histopathological examination because asymmetry was detected intra-operatively.
Data analysis
Data were analysed using SPSS® statistical software (IBM™, 2019). Binary logistic regression was used to identify factors in patients’ history and clinical examination that were significantly associated with a malignant histopathological outcome. The unpaired t-test was used to assess for differences in the mean estimated tonsil volume between two groups of tonsils: the side considered subjectively larger and the side considered smaller, on initial clinical examination.
Results
Demographics
Over a period from 2017 to 2022, 813 patients underwent histology tonsillectomy across three health organisations. Once exclusion criteria were applied, 323 cases of unilateral tonsil enlargement with no obvious ‘red flag’ signs on examination remained. Ninety paediatric and 233 adult cases were identified. Of the cases, 135 (41.8 per cent) were male and 188 (58.2 per cent) were female. All histology tonsillectomies were arranged because of unilateral tonsil enlargement, but 51 cases (15.8 per cent) had the additional indication of recurrent throat infection and 6 (1.9 per cent) had OSA.
Malignancy
Of the 323 cases, 5 (1.5 per cent) had histopathological evidence of malignant disease: 2 cases of lymphoma, 1 case of tonsillar infiltration of a chronic lymphocytic leukaemia/small lymphocytic lymphoma and 2 cases of oropharyngeal SCC. All patients with malignancy had reported some symptoms in addition to unilateral tonsil enlargement. These cases are summarised in Table 2.
Table 2. Summary of cases with a malignant histopathological diagnosis*

* Determined following histology tonsillectomy for unilateral tonsil enlargement. Pt. no. = patient number; y = years; M = male; F = female
Pre-operative history and examination factors
Information regarding pre-operative history and examination was available for 322 patients (99.7 per cent). Binary logistic regression identified increased age (p = 0.02) and history of rapid tonsil enlargement (p = 0.005) to be significantly associated with malignant histopathological outcome in all cases. Because no malignancy was diagnosed in children in our series, subgroup analysis was performed excluding paediatric patients. In this model, a history of rapid tonsil enlargement (p = 0.005) was shown to be the sole factor significantly associated with malignant histopathological outcome, with an odds ratio of 105.6 (95 per cent confidence interval = 3.97–2811.58).
Size of excised tonsils
Data on the size of excised tonsils were available bilaterally in 300 cases (92.9 per cent). When excised tonsils were grouped into those considered larger and smaller on pre-operative clinical examination, the mean estimated tonsil volume of the ‘larger’ group was found to be significantly greater than that of the ‘smaller’ group (105.3 ± 71.3 cm3 vs 83.3 ± 46.2 cm3; p < 0.0001). The pre-operatively ‘larger’ tonsil was found to have a greater estimated tonsil volume than the ‘smaller’ tonsil in 68 per cent of cases; however, in 29.7 per cent of cases, the ‘smaller’ tonsil had a greater estimated tonsil volume, and in 2.3 per cent the estimated tonsil volumes of the ‘larger’ and ‘smaller’ tonsils were equal.
Post-operative haemorrhage
Thirty-nine out of 323 cases (12.1 per cent) had a documented re-admission with post-tonsillectomy haemorrhage. Eight cases (2.5 per cent) required re-operation, with the remaining post-tonsillectomy bleeds being managed conservatively. There were no other documented cases of major post-operative morbidity or mortality.
Discussion
We present one of the largest published series of histology tonsillectomy for unilateral tonsil enlargement, with data collected from multiple health organisations. Our study had rigorous exclusion criteria, and we were able to analyse the paediatric and adult populations separately.
The study revealed no diagnoses of paediatric lymphoma following 90 histology tonsillectomies in children. This further adds to the pool of cases described by Jones et al.Reference Jones, Burnside, McPartland, Markey, Fallon and De3 demonstrating the extremely low yield of histology tonsillectomy in a paediatric population. Most cases of paediatric tonsillar lymphoma present with a history of rapid enlargement over a period of weeks.Reference Adil, Medina and Cunningham14 It is suggested that, in a paediatric population, this rapid enlargement, along with other ‘red flag’ symptoms such as weight loss, unexplained fever or cervical lymphadenopathy, are used as criteria for histology tonsillectomy, rather than unilateral tonsil enlargement alone.
In the adult population, our series demonstrated 5 cases of malignancy from 233 histology tonsillectomies (2.1 per cent). Whilst a range of histopathological diagnoses were detected (e.g. lymphoma, SCC, chronic lymphocytic leukaemia/small lymphocytic lymphoma), it should be noted that all cases exhibited symptoms in addition to unilateral tonsil enlargement. There were no malignant cases in the 65 adult patients (27.9 per cent) who presented with asymptomatic unilateral tonsil enlargement.
In adults, a documented history of rapid unilateral tonsil enlargement was found to be strongly significantly associated with a malignant histopathological outcome following histology tonsillectomy in our series. This is in keeping with existing knowledge of the presentation of tonsillar lymphoma as a wholeReference Berkowitz and Mahadevan15 and more specifically tonsillar lymphoma in adults, where a history of recent tonsillar enlargement is shown to be a more common presenting symptom than dysphagia, odynophagia or ‘B symptoms’ (i.e. weight loss and/or abnormal fever or sweating).Reference Laskar, Bahl, Muchaden, Nair, Gupta and Bakshi16 However, unilateral tonsil enlargement in the absence of a discreet mass or accompanying pathological cervical lymphadenopathy is not a common presentation of oropharyngeal SCC.Reference Mehanna, Evans, Beasley, Chatterjee, Dilkes and Homer17
Chronic lymphocytic leukaemia/small lymphocytic lymphoma is a rarer histopathological diagnosis following histology tonsillectomy. To our knowledge, there are no previously published reports of chronic lymphocytic leukaemia/small lymphocytic lymphoma presenting as unilateral tonsil enlargement, but reports have been published of chronic lymphocytic leukaemia/small lymphocytic lymphoma presenting with bilateral tonsil enlargement,Reference Duggal, Rana, Vaid, Sood and Kumar Handa18 and indeed chronic lymphocytic leukaemia infiltrating Waldeyer's ring and causing upper airway obstruction.Reference Bersabe, Romain, Ezzell and Renshaw19
We were able to quantitatively calculate estimated tonsil volume for excised tonsils and compare this with documented pre-operative examination findings. This demonstrated that clinicians appeared to be incorrect in identifying unilateral tonsil enlargement in 32 per cent of cases. Using similar methods, Spinou et al.Reference Spinou, Kubba, Konstantinidis and Johnston20 reported that in 15 per cent of cases the subjectively ‘larger’ tonsil was smaller once excised, and in 36 per cent of cases there was no asymmetry present. HarleyReference Harley21 matched unilateral tonsil enlargement cases with ‘symmetrical’ controls and found no significant difference in the degree of asymmetry of excised tonsils. Our large series strengthens an existing smaller body of evidence that suggests the clinical diagnosis of unilateral tonsil enlargement is unreliable.
Our series reports a rate of re-admission with post-tonsillectomy bleeding of 12 per cent. This is significantly greater than the 3.5 per cent reported by the 2005 National Prospective Tonsillectomy Audit,4 but is more in keeping with the 7.9–15.7 per cent reported more recently by a large Swedish longitudinal study.Reference Lundstrom, Stalfors, Ostvoll and Sunnergren22 Evidence that the rates of post-tonsillectomy bleeding and related morbidity may be greater than previously estimated by large-scale audit, especially in the paediatric population,Reference Thompson and Street23 strengthens a recommendation to move away from routine histology tonsillectomy.
In order to avoid the costs and relatively high morbidity associated with histology tonsillectomy, are there any other means of risk-stratifying patients with unilateral tonsil enlargement? Cross-sectional imaging is not often used in unilateral tonsil enlargement cases prior to considering tonsillectomy, but may be appropriate in some cases. The utility of diffusion-weighted magnetic resonance imaging (MRI) has been demonstrated in differentiating normal tonsil tissue from SCC,Reference Bhatia, King, Yeung, Mo, Vlantis and Yu24 but further research is required with regard to the identification of other malignant lesions of the palatine tonsil.
Limitations
The authors acknowledge that although clinical documentation was considered to be rigorous, the assumption that a factor in the patient's history or clinical examination findings is absent if not documented is a possible source of bias.
The relatively low numbers of positive histopathological diagnoses in our adult population limit the interpretation of results of the binary logistic regression performed to identify factors significantly associated with a malignant diagnosis. Estimates in variation of the dependent variable based on the statistical model used ranged from very low to moderately high (Cox and Snell R2 = 0.09; Nagelkerke R2 = 0.605).
Conclusion
This large-scale, multi-centre series of unilateral tonsil enlargement showed no paediatric cases of malignancy diagnosed following histology tonsillectomy. A relatively high rate of post-tonsillectomy bleeding, and a discrepancy between clinical findings and true unilateral tonsil enlargement were demonstrated. The authors recommend avoiding histology tonsillectomy for unilateral tonsil enlargement in the paediatric population unless symptoms are truly progressive or other ‘red flag’ symptoms are present.
• Histology tonsillectomy for unilateral tonsil enlargement results in a low yield in children, but there is less evidence in adults
• In this study, histology tonsillectomies revealed no malignancy in 90 children and led to 5 malignant diagnoses in 233 adults
• All malignant adult cases presented with other symptoms, in addition to unilateral tonsil enlargement
• A history of rapid tonsil enlargement (less than 12 weeks) was associated with a malignant diagnosis
• A clinical diagnosis of unilateral tonsil enlargement was incorrect on histopathological measurement in 32 per cent of cases
• The authors recommend avoiding histology tonsillectomy for asymptomatic unilateral tonsil enlargement; this should be reserved for ‘red flag’ malignancy signs
In the adult population, histology tonsillectomy demonstrated a malignant pathology in 2.1 per cent of unilateral tonsil enlargement cases, but all positive cases had other symptoms. The authors recommend avoiding further investigations in patients with asymptomatic, longstanding unilateral tonsil enlargement. In cases requiring further investigation, diffusion-weighted MRI may be a useful tool to further assess asymmetry or identify a lesion, prior to considering histology tonsillectomy.
Acknowledgements
The authors acknowledge the work of the Otolaryngology/Head and Neck Surgery Departments at Aneurin Bevan University Health Board, Cardiff, and Vale University Health Board and Swansea Bay University Health Board.
Competing interests
None declared.




