Crossref Citations
This article has been cited by the following publications. This list is generated based on data provided by Crossref.
2022.
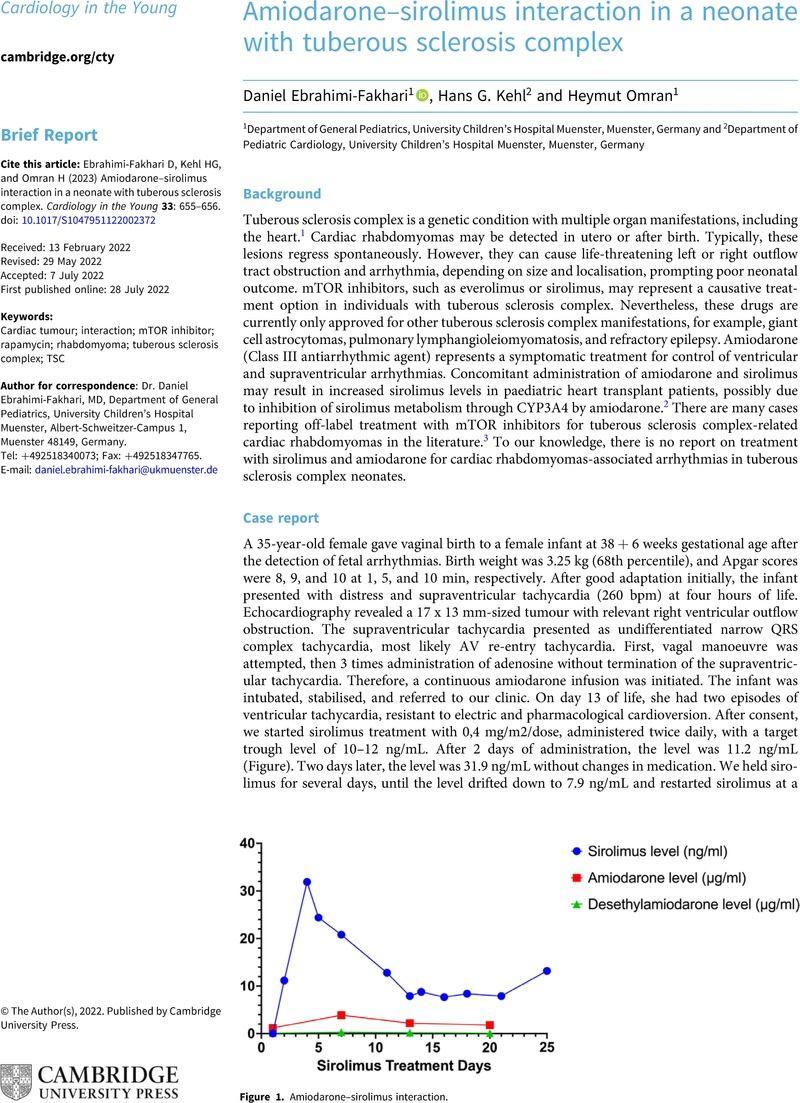
Adenosine/amiodarone/sirolimus.
Reactions Weekly,
Vol. 1921,
Issue. 1,
p.
16.