The COVID-19 pandemic is a global health crisis confronting humanity today. It is an emerging viral disease caused by a type of Coronavirus named 2019 SARS-Cov-2 which appeared in Wuhan, China in late December 2019. Reference Hajjar, Memish and McIntosh1 There have been previous outbreaks of other coronaviruses, including the Middle East Respiratory Syndrome (MERS-CoV), which emerged from the Arabian Peninsula in 2012 with 858 known deaths, and the Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV) which had caused 800 deaths in China by the end of 2002. Reference Hajjar, Memish and McIntosh1,Reference Kin and Vabret2
As of May 31, 2020, the current COVID-19 pandemic had 6028135 confirmed cases and 368944 deaths in 188 countries, representing a worldwide lethality rate of about 6.12%. America is the most affected continent with 2846391 confirmed cases and 161514 deaths, mainly in the United States, Brazil, Mexico, Canada, and Peru. Europe has 1934991 confirmed cases and 173155 deaths, Asia has 1095786 confirmed cases and 30065 deaths, Oceania has 8639 confirmed cases and 132 deaths, and Africa has 141632 confirmed cases and 4071 deaths. 3
The COVID-19 pandemic affects almost all African countries. As described by the WHO, about 50% of the countries in Africa are experiencing community transmission. 4 With regards to the elements of vulnerability, the mitigation and response capacities of countries faced with this threat, the sub-Saharan African region could be at risk of a public health disaster, given the ever-increasing curve in the number of people infected (100510 cumulative confirmed cases and 2089 deaths). Sub-Saharan Africa is divided into 4 sub-regions: Eastern Africa, Western Africa, Southern Africa, and Central Africa. An integrated analysis of the level of vulnerability to this pandemic with focus on 1 of these sub-regions could make it possible to suggest effective and sustainable approaches to manage the health crisis. This is the reason why this study focused on the Central African sub-region, with the aim of examining its factors of vulnerability to the COVID-19 pandemic in socio-demographic, economic, and health dimensions. The ambition is to extrapolate the observations and recommendations made in Central Africa to other sub-Saharan sub-regions.
Method
Definition of risk and vulnerability
Risk is defined as the probability of the occurrence of an adverse event or hazard. Several different analytical approaches are available in literature, but in general, a risk depends on 2 factors: the hazard and the vulnerability. In its simplest term, a risk measure is given by an equation Reference Sirven5 : Risk = Hazard x Vulnerability.
A hazard is a particular event that is likely to take place. Its potential dimension distinguishes it from disasters that have occurred. It can be natural (biological, geological, hydro-meteorological, climatic, etc.) or anthropic (technological, societal, etc.). The same hazard does not necessarily cause the same effects. In other words, an outbreak in France or Italy will not have the same effects in Burundi or the Central African Republic. Thus, this refers to factors which can be demographic, health-based, socio-economic, administrative, political, or institutional.
These factors imply an emphasis on vulnerability that ranges in scale from the individual to groups of individuals. Reference Sirven5
Vulnerability is therefore determined by the exposure of people as well as their sensitivity to hazards and their capacities to cope with disastrous situations and reduce their impact. Reference Sirven5
Central African sub-region
This sub-region has 11 member states (Angola, Burundi, Cameroon, Central African Republic, Congo, Gabon, Equatorial Guinea, Democratic Republic of Congo, Rwanda, São Tomé and Príncipe, and Chad), grouped under the name of the Economic Community of Central African States (ECCAS), with an area of 6640600 km2 for a population estimated at around 187.2 million inhabitants. 6
Data sources and information
In this study, the indicators used came from the databases of the World Bank (WB), the United Nations Development Program (UNDP), and the World Health Organization (WHO). 7–11 Information on the evolution of this pandemic in terms of number of confirmed cases and deaths in the world and in respective countries was collected on the web-based continuous compilation of COVID-19 data by the European Centre for Disease Prevention and Control (ECDC). 3 Current data from the scientific literature on the novel coronavirus involved has been searched on PubMed (National Library of Medicine, Bethesda, MD), Google Scholar (Google Inc, Mountain View, CA), and the WHO website.
Demographic, health, and socio-economic indicators have made it possible to describe the vulnerability of the Central African sub-region and its countries to COVID-19. Literature data on COVID-19, the number of COVID-19 tests administered, the number of confirmed cases and deaths worldwide (and in Central Europe, North America, China, and sub-Saharan regions) were used to describe the magnitude of the hazard, which in this context is biological.
Selection criteria and quality control of data and indicators
The study period was from December 31st, 2019 to May 31st, 2020; that is to say 05 months after the start of the pandemic. The demographic indicators chosen were the average age of the population, their life expectancy, and the proportion of people aged 65 and over. The health indicators used were the number of hospital beds per 1000 inhabitants, the number of doctors per 1000 inhabitants, the number of nurses and midwives per 1000 inhabitants, the gross mortality, and indicators of morbidity including national prevalence of certain chronic diseases such as HIV/AIDS, obesity, diabetes, and cancer. The socio-economic indicators used were the Gross Domestic Product (GDP), unemployment rate, percentage of the population living on less than 1.9 USD per day, percentage of non-agricultural informal employment, percentage of literacy of over 15-year-olds, and the 2018 ranking of countries according to the Human Development Index (HDI) of the UNDP.
Statistical data analysis
We have ensured the quality and validity of the data collected. These data were grouped and categorized on a Microsoft Excel 2007 spreadsheet (Microsoft Corp, Redmond, WA). The means of the indicators and sometimes their totals have been calculated to describe vulnerability and the epidemic situation at the sub-regional level.
Results and discussions
The COVID-19 pandemic, a biological hazard
The COVID-19 pandemic is due to a novel coronavirus which has been named Sars-Cov-2. It is an emerging zoonosis. Although its animal origin is not precise enough, the pangolin, the snake, and the turtle are suspected due to the interaction between their cell surface protein angiotensin-converting enzyme 2 (ACE 2) with a protein from the 2019-Sars-Cov-2 virus.
The origin of the crossing of the species barrier, the passage from animal to human, raises a lot of debate. Reference Liu, Xiao and Wei12 In-depth studies on forest and domestic fauna and production chains in the Central African sub-region must be carried out on the circulation of coronaviruses in animals and reservoirs. This virus has a great tropism for the cells of the upper and lower respiratory mucous membranes in which it multiplies. The COVID-19 incubation period ranges from 2 to 14 days. Reference Linton, Kobayashi and Yang13 Apart from asymptomatic carriers who represent 1.2% of patients, 14 the most frequent symptoms are fever, cough, difficulty in breathing, fatigue, muscle pain, and more rarely, gastrointestinal signs. Thus, the clinical picture can range from a common flu-like syndrome to severe respiratory distress that can progress to multiple organ failure. Reference Guan, Ni and Hu15,Reference Rothan and Byrareddy16
Sars-Cov-2 is characterized by its great contagiousness, which explains the rapid increase in the number of cases worldwide. Till date 6028135 confirmed cases have been reported in 188 countries in just 5 months, approximately 200 times the number of cases observed during the Ebola epidemic between 2014 and 2016 in West Africa. 3,17 The Ebola virus is mainly transmitted by contact with the patient’s body fluids, 17 while COVID-19 is transmitted from 1 person to another by air through droplets, personal contact, and contamination of objects. Reference Rothan and Byrareddy16 Cases of COVID-19 transmission by asymptomatic and pre-symptomatic patients have been reported by some authors, Reference Bai, Yao and Wei18,Reference Rothe, Schunk and Sothmann19 as well as few cases of reactivation of the virus after recovery. Reference Ye, Pan and Pan20 The evidence for reinfection in recovered patients is not yet clarified at this date. Reference Omer, Malani and del Rio21
The virulence of Sars-cov-2 has already caused more than 368944 deaths in the world in just 5 months, the overall lethality rate is 6.12%, varying from 1 country to another according to local resilience capacities. This number of deaths in just 5 months represents more than 33 times the number of deaths observed with the Ebola outbreak that lasted from 2014 to 2016 in West Africa, which had a much greater lethality rate of 39.5%. 3,17 This difference is explained by the high number of cases of COVID-19.
Another important characteristic of this virus is its resistance, as droplets, particularly those emitted during sneezing can be projected up to 2 to 4 meters and the virus can persist there for up to 45 minutes depending on the conditions of temperature and pressure. Its survival on surfaces, which is limited to a few minutes on the skin, can continue for up to 12 hours on clothing and 5 days on paper, metal, and plastic. SARS-CoV-2 is sensitive to ultraviolet rays and heat and can be inactivated by lipid solvents including ether (75%), ethanol, chlorine-containing disinfectant, peroxyacetic acid, and chloroform (except for chlorhexidine). Reference Kampf, Todt and Pfaender22
Despite the previous data on other coronaviruses like MERS-CoV Reference Altamimi and Ahmed23 and the spread which seems to be slower in sub-Saharan Africa than in Europe, North America, and a part of Asia, the seasonality of cases and slower transmission in warmer climates is highly contested. All this is with respect to the ongoing situation in Southern US, India, Indonesia. 3 Nevertheless, such biological and epidemiological characteristics make the SARS-Cov-2 coronavirus a threat to all humanity. The statistical features of the COVID-19 pandemic seem to present the same trend in the 5 African sub-regions with 2157 deaths/48454 cumulative cases in Northern Africa, 686 deaths/33029 cumulative cases in Southern Africa, 266 deaths/15589 cumulative cases in Eastern Africa, 740 deaths/35555 cumulative cases in Western Africa, and 397 deaths/16337 cumulative cases in Central Africa (Map 1).
The virus is already significantly present in 11 Central African Countries where the first cases had been progressively reported since February 2020 (Map 1, Map 2, Figure 2 and Table 1).

Figure 1. Map 1.
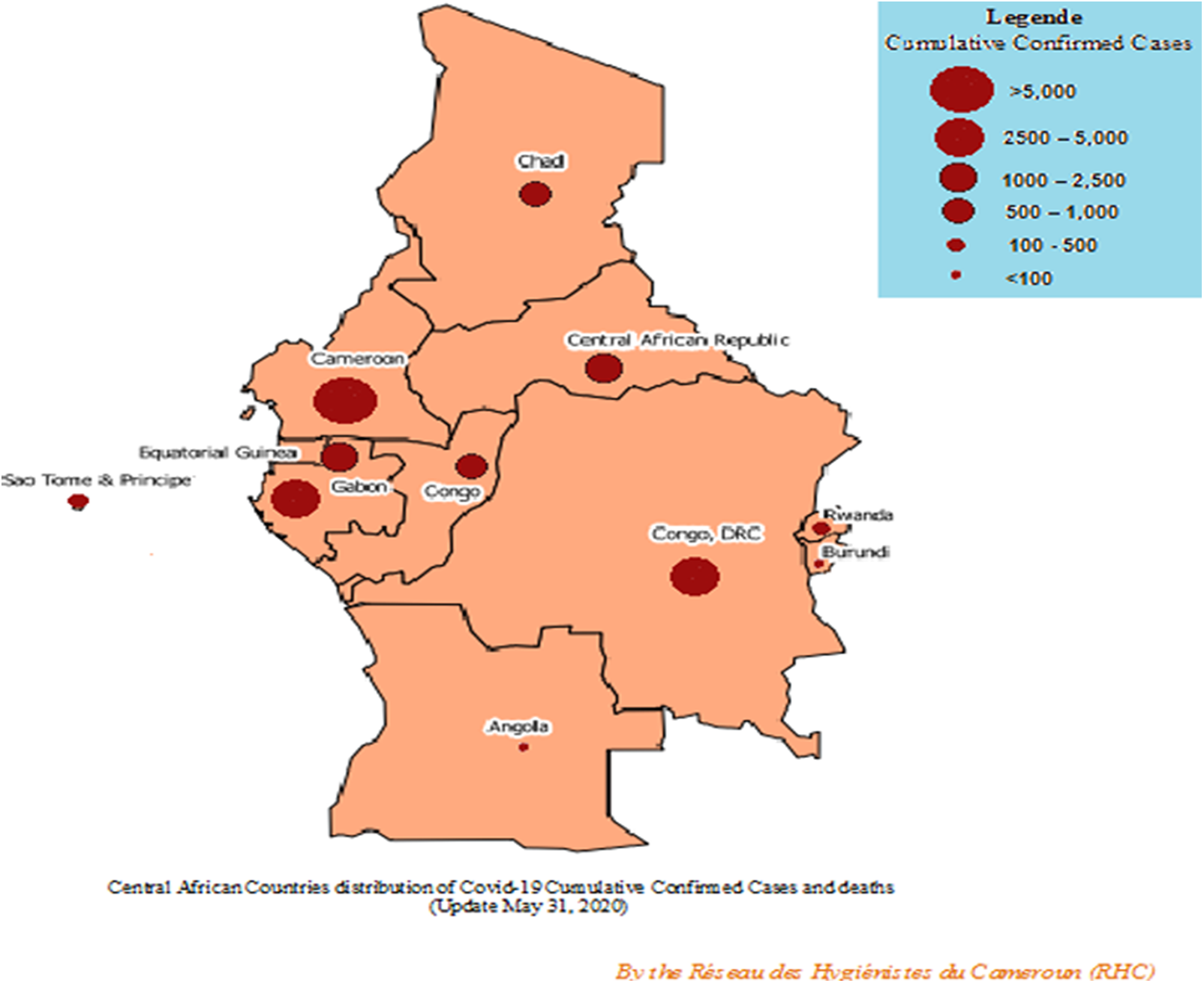
Figure 2. Map 2.

Figure 3. The weekly evolution of the number of cumulative confirmed cases and deaths in the Central African sub-region (Updated May 31, 2020).
Table 1. Distribution of the number of cases and deaths of COVID-19 in Central African States (Updated May 31, 2020)

Table 2. Demographic characteristics of Central African States

Demographic and health vulnerability
The age pyramid of sub-Saharan African Countries is known for its parasol shape, characterized by high birth and mortality rates. Reference Chevallier and Le Golf25 Table 2 shows that the average age of the populations of the Central African sub-region is 17.81 years, with a minimum of 16 years in Chad, and a maximum of 20.7 years in the Congo, versus 43.1, 37, and 36.7 in Europe, Central Europe, and China respectively. In 2018, the proportion of people aged 65 years and above varied from 2 to 4% versus 18%, 16%, and 11% in Central Europe, North America, and China respectively. These demographic data show sub-Saharan African populations to be younger. The effect of age structure on COVID-19 lethality has been underlined in worldwide, European, Asian, and North American COVID-19 statistics. It was therefore observed that the lethality of COVID-19 was much higher in elderly people than in other age groups. In Italy, for example, 84.6% of deaths due to COVID-19 were made up of people aged 70 and over, 10.9% aged between 60 to 69, 4.2% from 40 to 49, 0.3% from 30 at 39, and 0% under 30. Reference Mahase26,27 According to those demographic and COVID-19 statistics, the age structure of the population could be linked to the low lethality rate and the high number of recoveries observed in the Central African sub-region.
The gender-related vulnerability to COVID-19 should be well studied in the African context. UN Women underlined that paying attention to the needs and leadership of women could strengthen the response to COVID-19. 28 The evidence from China suggests that the number of men who died from COVID-19 is 2.4 times higher than that of women (70.3 vs. 29.7%, P = 0.016). Reference Jin, Bai and He29 Several births have been reported in central African countries among women infected with COVID-19, but no evidence has been published providing details. The African literature on the transmission of COVID-19 from mother to child, obstetric prevention, clinical presentation in the newborn, management, and prognosis must be strengthened for a better response in these vulnerable groups. Chinese studies showed that pregnancy and childbirth did not aggravate the course of symptoms or CT-scan features of COVID-19 pneumonia. Reference Liu, Li and Wu30 According to the CDC, the transmission of SARS-CoV-2 to neonates could occur during the postnatal period when neonates are exposed to mothers, visitors, or healthcare personnel with COVID-19. There is poor evidence about possible intrapartum, peripartum, or vertical transmission. Even though information on clinical presentation and disease severity among neonates is limited, data from case reports and small case series suggest that infants may be at higher risk for severe illness from COVID-19 compared to older children. 31
Our results showed that the gross mortality is 8.6 per 1000 inhabitants in Central African sub-region, with extremes of 5 to 13 per 1000 inhabitants, depending on the country. Life expectancy in this sub-region is 61.09 years, with a minimum of 52 years in Central African Republic (CAR) and a maximum of 70 years in São Tomé and Príncipe versus 77 years in Central Europe, 79 years in North America, and 77 in China (Table 3). These large differences are connected to the high mortality and morbidity of other diseases in the Central African sub-region (Table 5). Indeed, observations made in developed countries have revealed greater lethality of COVID-19 in people with certain co-morbidities. Reference Phua, Weng and Ling32 According to the WHO data, the HIV prevalence of the Central African sub-region is 2.6%, with a minimum of 0.7 in São Tomé and Príncipe and a maximum of 7.1 in Equatorial Guinea. The prevalence of diabetes is 5.4% in Central African sub-region, with a minimum of 2.4 in São Tomé and Príncipe and a maximum of 6 in Central African Republic, Democratic Republic of the Congo, Congo, Chad, Equatorial Guinea, Gabon, and Cameroon. A total of 239469 cases of cancers were reported in the Central African sub-region in 2020 (Table 3). In addition, the endemic malaria, malnutrition, poverty, and underdevelopment constitute a vicious circle, Reference Fillol, Cournil and Cames33 with characteristics of slow-onset disasters to which are added the current problem. All these diseases are likely to weaken the health situation of the populations of the Central African sub-region and contribute to greater lethality of COVID-19.
Table 3. Morbidity and mortality indicators of Central African States

The high gross mortality observed in the Central African sub-region is also favored by the low epidemic-response capacity of the health infrastructure and human resources. Indeed, our results show that the number of hospital beds per 1000 inhabitants in the Central African sub-region is 1.7 with a minimum of 0.4 in Chad and a maximum of 6.3 in Gabon (Table 4) versus 6.4, 2.9, and 4.2 in Central Europe, North America, and China respectively. The number of doctors per 1000 inhabitants is 0.2 with a minimum of 0.04 in Chad and a maximum 0.4 in Gabon and Equatorial Guinea (Table 4) versus 3.1, 2.6, and 2.0 in Central Europe, North America, and China respectively. The number of nurses and midwives per 1000 inhabitants is 1.1 with a minimum of 0.4 in Chad and a maximum of 2.6 in Gabon and Equatorial Guinea (Table 4) versus 7.2, 14.1, and 2.7 in Central Europe, North America, and China. 7 It has been observed in Italy that 12% of COVID-19 patients received before March 12, 2020 required intensive care. Many developed countries like Italy and France which are renowned for their state-of-the-art health infrastructure and human resources were overwhelmed by the enormous influx of COVID-19 patients. Reference Phua, Weng and Ling32 This comparative analysis gives an idea of the need for Central African countries to urgently improve their intensive care services for a better response to this health crisis. Thus, additional studies must be carried out to assess the intensive care infrastructure quantitatively and qualitatively in Central African countries.
Table 4. Some health care indicators

Elsewhere, we found that there were some countries like Burundi and Angola which have to date performed a very low number of COVID-19 tests per 1 million inhabitants, 24 and 305 respectively (Table 1). Furthermore, as highlighted by the WHO, the sub-Saharan region seems to have the lowest rate of COVID-19 testing. This is the cause of the fear of a possible ‘silent epidemic’ in this region if its leaders do not prioritize coronavirus testing. According to the WHO, during the Ebola outbreak in West Africa from 2014 to 2016, apart from the 11000 reported deaths due to Ebola infection, another 10000 people died from common diseases. 17 This means that the management of other usual pathologies remains a significant public health burden during this pandemic. This may weaken the national and sub-regional responses during this health crisis due to the COVID-19 pandemic and vice-versa. It is therefore evident that the absence of universal health coverage in all the countries of Central African sub-region except for Gabon could have a negative impact on gross mortality in this period. 34 Obviously, the existence of another ongoing outbreak could further increase vulnerability to the COVID-19 pandemic. This is the case of the Democratic Republic of the Congo, which is going through its 9th Ebola epidemic since August 2018, in the provinces of Ituri and North Kivu. The WHO declared it a public health emergency of international scope in July 2019. 17 The last cases of this outbreak were reported on April 16, 2020 and resulted in 3458 confirmed cases and 2277 deaths. 35 It can also be hoped that the experience of these communities that faced a previous major outbreak can contribute to improved resilience to future outbreaks. In the same way, the Congo and Gabon have also each encountered 4 Ebola outbreaks between 1994 and 2005. Reference Berliner36 As described in Table 4, most Central African Countries have experienced Cholera outbreaks. Reference Ali, Nelson and Lopez37 However, each of these countries has encountered at least 1 other deadly outbreak such as yellow fever, measles, necrotizing fasciitis, Marburg virus, Meningitis. 38–43 An intergovernmental collaboration framework at the sub-regional level could be a means for sharing such epidemiological experiences for better capacity-building.
Social, financial, and economic vulnerability
According to Table 3, the Gross Domestic Product (GDP) in the Central African sub-region is 23.43 billion USD with a minimum of 2.54 billion USD in Central Africa Republic and a maximum of 95.34 billion USD in Angola. Given that the West Africa Ebola outbreak weakened the economies of Liberia, Sierra Leone, and Guinea, 44 this should be enough reason to anticipate an economic crisis during this COVID-19 pandemic and its recovery phase. It appears that, apart from Gabon and Congo, 9 of the 11 countries in the Central African sub-region are among the bottom 50 in the World Bank Poverty Ranking according to the Human Development Index. Furthermore, 45.49% of the population of the Central African sub-region live with less than 1.9 USD/day with a minimum of 3.4% USD in Gabon and a maximum of 76.8% in Equatorial Guinea. The unemployment rate is 6.53% with a minimum of 1% in Rwanda and a maximum of 20% in Gabon. Additionally, 80.8% of the populations of Central African sub-region rely on the informal non-agricultural sector for survival, with a maximum of 96% in Democratic Republic of the Congo (Table 5). Accordingly, certain response strategies like confinement, quarantine, and rapid strengthening of the health infrastructures, which have proven very effective against COVID-19 in China would be difficult to implement in most of these countries if there is no substantial financial support put in place. Reference Zunyou and Jennifer45 Some of the countries in this sub-region have recently started de-confinement and the reopening of borders, schools and bars despite the significant and continuous increase in the number of cases and deaths.
Table 5. Socio-economic characteristics of the Central African states

GDP, Gross Domestic Product; HDI, Human Development Index.
The adult literacy rate is 70% in the Central African sub-region, with a minimum of 22% in Chad and a maximum of 94% in Equatorial Guinea (Table 5). The Ebola epidemic in West Africa has demonstrated the value of community engagement in the response to outbreaks. Reference Mamadou Mbaye, Kone and Kâ46 It is obvious that in the current situation of the COVID-19 pandemic, a low literacy rate in a country, associated with misinformation and belief in conspiracy theories, can have a significant impact on the involvement of communities in the response. This was in fact 1 of the factors behind the persistence of community transmission of Ebola virus infection in West Africa from 2014 to 2016. Reference Waldispuehl47 Raising awareness and implementing proper communication are crucial parameters to take into consideration during this pandemic.
Conflicts are known for their ability to weaken a country’s institutions and economy, and the Central African Sub-region is not an exception. Reference Jean-Paul, Jean-Claude and Stéphane48,Reference Hugon49 This sub-region has experienced several armed conflicts in recent decades. The Democratic Republic of the Congo has been plagued by repeated wars for several decades. This country has been confronted since 2004 by the conflict in North Kivu, which has been compounded by an Ebola outbreak in the same area. For the last 3 years, Cameroon has been facing an internal conflict in its 2 Anglophone regions, and in the far North, for more than 10 years Chad has been involved in the war against the Boko Haram. Central African Republic (CAR) is still recovering from its civil war, which lasted between 2013 and 2017. Furthermore, many countries in this region are faced with corruption and embezzlement of public funds that could sabotage the sustainable and effective implementation of a resilience strategy to this health crisis. 50 The overcrowding noted in most prisons and detention centers in Central African countries can make them epicenters of COVID-19 if strategies of decongestion and barrier measures are not implemented. 51
Conclusion
This paper presents, among other things, evidence that Central African countries can derive benefits from the age structure of their young population against COVID-19. Nevertheless, the high morbidity due to other diseases associated with the low epidemic response capacity of the health infrastructure and human resources can worsen the lethality of this pandemic. The population of the third age, which represents only 3% of the population and those of people with co-morbidities could have more deaths and severe cases. The lower lethality of COVID-19 in young people without co-morbidities with possible asymptomatic cases, and the low rate of COVID-testing noticed in sub-Saharan countries can increase the exposure of the elderly. This leads us to evoke the paradigm of, ‘the young person who involuntarily exposes his old parents.’ The rapid dissemination of Sars-Cov-2 observed in Europe, Asia, and America compared to the slow spread paradoxically observed in Africa should raise questions for subsequent studies either in the environmental, climatic, or socio-cultural dimensions. But if it was only an illusion, as the WHO noticed the fewest diagnosed cases of the virus in Africa, there could be a silent progression in the number of cases and deaths. The early retirement of lockdown restrictions introduced in certain sub-Saharan countries despite the continuous increase in the number of cases and deaths could worsen the situation. Economic indicators, in particular the percentage of the population working in the informal sector and the percentage of those living on less than US $1.9/day show that control strategies such as general confinement and rapid strengthening of the health infrastructures which have remarkably been effective in China are not realistic in most sub-Saharan countries. Those observations made in this study in the Central African Sub-region could be easily extrapolated to other sub-Saharan sub-regions, as they seem to have the same epidemiological, socio-demographic, and economic profiles with Central Africa. In these Subregions, where a large proportion of the population lives in poverty, conflicts, and humanitarian crises, questions of prevention standards could appear superfluous. It appears that Central African countries need financial and logistical support for sustainable and effective responses to the COVID-19 pandemic. Such a hazard should become a pretext for African development. Administrative, political, or institutional vulnerabilities should also be analyzed with the aim of completing this study, as well as an integrated and in-depth analysis of the capacities of the sub-region countries.
Author contributions
Tazemda Kuitsouc GB: conception, design, data collection, data analysis and writing; Dominique Kuitsouc: conception and writing; Ingrid Djuikoue C: analysis and writing; Nwaha Makon AS: writing and editing; Tagne Kamga C: writing and editing; Kuitsouc Domkam R: analysis and writing; Keubou Kuematsa C: writing and editing; Belefeh G Nkafu: writing and editing; Tuono Romaric: writing; Man-Koumba Soumahoro: writing; Tchokonte Nana V: writing and editing; Kaptue N Lazare+: writing; Tambo Ernest: conception, analysis, and writing; Ndebia Eugene J: Writing and editing.
Funding statement
The study was supported by the ‘Réseau des Hygiénistes du Cameroun (RHC).’
Conflicts of interest
The authors have not declared any conflicts of interest.










