Foot drop due to fibular (peroneal) neuropathy at the knee may be caused by direct trauma, external compression, or structural (intrinsic or extrinsic) mass lesions. We present here an unusual presentation of intraneural ganglion cyst.
A 64-year-old female presented to our clinic for evaluation. She had no significant past medical history, and was able to run 10 km until the time of clinical presentation. The first symptom was a burning and stabbing discomfort in the upper lateral left calf region. She also noted a mild and intermittent foot drop, which was aggravated by walking or jogging. Nerve conduction studies done 6 months later showed partial and non-localized motor and sensory axonal loss in the common fibular nerve territory. Foot drop improved spontaneously with avoidance of strenuous activity.
She presented for reassessment in 18 months after initial onset, reporting that her foot drop had markedly worsened. There was Medical Research Council grade 1/5 weakness of left ankle dorsiflexion and eversion, with sparing of ankle inversion and plantar flexion. There was mild hypoesthesia and allodynia along the left lateral calf and dorsum of the foot. Nerve conduction studies were repeated, showing more severe axonal loss in the deep (motor) and superficial (sensory) branches of the fibular nerve, without conduction slowing across the fibular head. An axonal process in the region of the fibular head was, however, suggested by needle electromyogram findings of active denervation in the tibialis anterior, with sparing of the biceps femoris (short head), tibialis posterior and gastrocnemius muscles.
MRI of the left knee showed a multiloculated and elongated cystic structure along the course of the common fibular nerve at level of the lateral knee margin (Figure 1). This complex structure, with a maximal diameter of 1.2 cm, extended inferiorly over a distance of 4.5 cm and communicated with an additional cluster of cysts within the tibialis anterior muscle. The multiloculated structure was diffusely hypointense on T1 and hyperintense on the fluid sensitive, fat-suppressed proton density (PD) sequences—a signal pattern consistent with fluid/cystic composition. The patient was referred for surgical exploration.
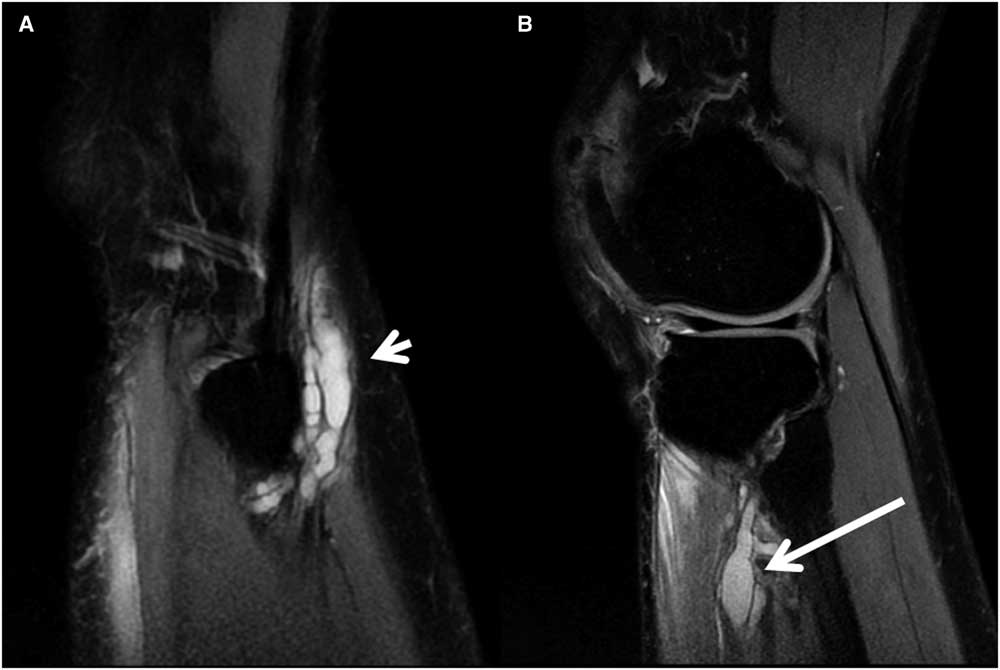
Figure 1 Sagittal MRI images of the left knee (proton density), showing multiloculated intraneural cysts at the following descending levels: (A) common fibular nerve at the fibular head (short arrow) and (B) and deep fibular branch to the tibialis anterior muscle (long arrow).
During surgery, the common fibular nerve was carefully dissected and its articular branch was traced to the level of the joint capsule. The articular nerve branch was severed at the level of the joint, followed by decompression of a cluster of ganglion cysts within the common fibular nerve. Incisions were made over several additional cystic loculations, releasing clear viscous fluid. Histological examination revealed small nerve fascicles surrounded by eosinophilic material without an epithelial lining capsule most in keeping with perifascicular encasement by synovial fluid, and a diagnosis of intraneural ganglion cyst (Figure 2).
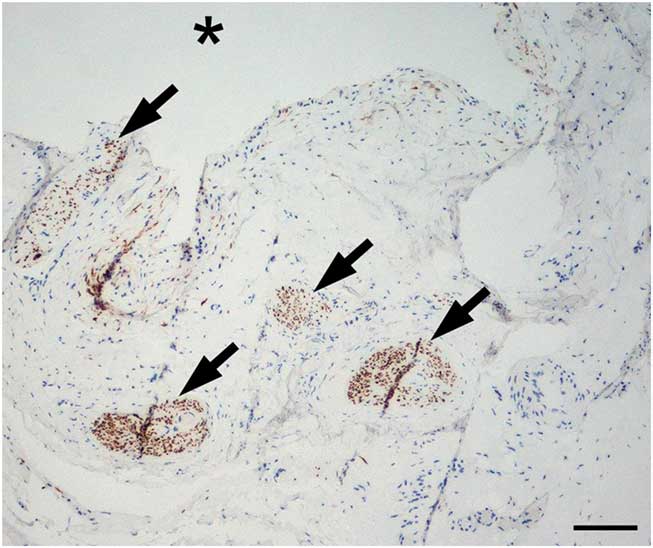
Figure 2 Intraneural ganglion cyst (*represents cavity). Nerve fascicles (arrows) within cyst wall show reduced axon density. Neurofilament 200 kD antibody stain, bar=100 µm.
One year after surgery, the patient had improved to grade 3/5 dorsiflexion paresis, and she reported no pain or sensory loss. She was able to ambulate without a brace and was now able to engage in a slow jog. Repeat MRI studies confirmed complete resection/resorption of the ganglion cysts.
The term intraneural ganglion cyst refers to a perifascicular loculated accumulation of synovial fluid, where an articular branch serves as an anastomotic channel between joint and nerve. In older literature, cases were classified as idiopathic intraneural mucinous or ganglion cysts, thought to reflect an atypical degenerative process. More recent literature, supported by careful intraoperative observation, and high-resolution MRI, has elucidated that a defect in the joint capsule allows extravasation of synovial fluid out of the joint.Reference Spinner, Atkinson and Tiel 1 - Reference Desy, Wang and Elshiekh 4 Intraneural ganglion cysts are uncommon in comparison with extraneural cysts; the most frequent sites of occurrence (by nerve/anatomic location) being the common fibular/knee, ulnar/elbow, tibial/knee, tibial/ankle and ulnar/wrist.
At the knee joint, the process is initiated by degenerative or traumatic lesions of the superior tibiofibular joint, with gradual extrusion of synovial fluid along the articular nerve branch, through a defect in the joint capsule. Gradual elongation of the cyst follows the path of least resistance and is modulated by changes in joint pressure, with gradual dissection around fascicles within the epineurium of the common fibular nerve. From there, spread most commonly occurs downwards to the deep fibular branch (as noted in our case), or superiorly to the distal sciatic and then down the tibial nerve.Reference Spinner, Desy and Amrami 3
Intraneural ganglion cysts must be distinguished from peripheral nerve tumors (schwannomas, neurofibromas, perineuriomas, malignant peripheral nerve sheath tumors), post-traumatic neuromas and large purely extraneural ganglion cysts.
This case demonstrates a unique feature of significant clinical fluctuations before recognition and treatment. Although such fluctuations can be seen in the course of several neuropathic lesions, they could represent the clinical counterpart of the process of episodic, dynamic and fluctuating peroneal and tibial intraneural ganglia formation.Reference Spinner, Amrami and Wolanskyj 5
MRI studies are critical for preoperative diagnosis. Intraneural ganglion cysts appear as tubular or rounded collections that are hyperintense on T2/PD sequences and hypointense on T1.Reference Van den Bergh, Vanhoenacker, De Smet, Huysse and Verstraete 6 , Reference Iverson 7 There should neither be gadolinium enhancement nor a defined capsule. In some cases, the origin of the cyst at the anterior aspect of the proximal tibiofibular joint (the “tail sign”) can be revealed, as well as its horizontal course in the articular branch (the “transverse limb sign”). It may also be possible to document the articular connection via magnetic resonance arthrography.
Knowledge of the pathophysiology has shaped our current management of intraneural ganglion cysts. Simple incision and drainage, or percutaneous aspiration, are associated with high rates of recurrence. Effective therapy requires the identification and disconnection of the relevant articular branch. In addition, consideration must be given to correcting the source of synovial extravasation at the level of the superior tibiofibular joint capsule, particularly in cases of recurrent juxta-articular cyst formation. This may require joint resection, with or without proximal fibulectomy.Reference Spinner, Desy, Rock and Amrami 8 In order to plan and tailor the appropriate surgical intervention, clinicians must be confident in the diagnosis based on history, electrodiagnosis and MRI studies.
Acknowledgment
The authors acknowledge the patients contributing to this research.
Disclosures
All authors do not have anything to disclose. No funding was received for this article.
Statement of Authorship
PB: Data collection, critical review of manuscript; KB: Review of discussion of surgical aspects of diagnosis and management; GJ: Preparation and discussion of neuropathology results; JWC: Critical review of manuscript; JZ: Critical review of manuscript; EBP: Critical review of manuscript; KR: Collection and discussion of neuroradiology data; AB: Literature review, critical review and revisions of manuscript.




