Introduction
Over the past decades, changes in demand for care led to reconsiderations and redistributions of tasks and responsibilities in the primary care workforce across Europe. Primary care practices adapted to the changed patterns of morbidity and patients’ increasingly complex health care needs by, for example, expanding the services offered and the skill mix of health care workers involved (Van Schalkwyk et al., Reference Van Schalkwyk, Bourek, Kringos, Siciliani, Barry, De Maeseneer and McKee2020). European primary care services particularly expanded in the area of (chronic) disease management (Schäfer et al., Reference Schäfer, Boerma, Spreeuwenberg, Schellevis and Groenewegen2016). The adaptations are also visible in the workforce composition of primary care practices, which is increasingly made up of multidisciplinary teams, rather than individual general practitioners (GPs) only (Groenewegen et al., Reference Groenewegen, Heinemann, Greẞ and Schäfer2015). Such teams enable the redistribution or delegation of tasks to professional support functions. Drivers of these developments were not only changes in the demand for health care, but also the need for increased efficiency, cost containment and difficulties in many countries to attract and retain GPs. Ageing GP populations in Europe and a lack of newly trained GPs have resulted in shortages, particularly in rural areas (Groenewegen et al., Reference Groenewegen, Bosmans, Boerma and Spreeuwenberg2020).
In this article, we describe and explain the extent of task shifting between GPs and nurses and support personnel in 34 countries. We define task shifting as the reallocation and redistribution of tasks and the sharing of roles among health professions and different groups of health professionals (WHO, 2006; EC, 2019). The number and diversity of staff present in a practice or health centre determines the options for task shifting but may also be a result of this process. In a strictly single-handed GP practice (i.e. without any supporting staff), for example, possibilities for task shifting are absent.
Occupational titles (and the related professional education) strongly differ between countries (Hewko et al., Reference Hewko, Cooper, Huynh, Spiwek, Carleton, Reid and Cummings2015; Kroezen et al., Reference Kroezen, Schäfer, Sermeus, Hansen and Batenburg2018; Schäfer et al., Reference Schäfer, Kroezen, Hansen, Sermeus, Aszalos and Batenburg2018). Therefore, it is easier to identify and label functions carried out in practices than to allocate occupational titles to those executing them. In primary care, assistants are usually called practice assistants or practice secretaries. Nurses in primary care practices may have the occupational title of practice nurse, which does not necessarily imply they are registered nurses. In some countries, nurses working in primary care may functionally be equivalent to practice secretaries or assistants in other countries. Throughout this article, we will use the term ‘practice assistant/nurse’ and this includes practice secretaries as well.
There is a broad range of tasks that can be shifted to practice assistants/nurses, including routine checks (e.g. blood pressure measurement, health assessments), prescribing drugs and referring patients, more technical procedures (e.g. wound care, removing sutures) and health promotion activities (e.g. patient education on quitting smoking) (Vail et al., Reference Vail, Bosley, Petrova and Dale2011; Maier and Aiken, Reference Maier and Aiken2016). Previous studies found that for curative services shifted from GPs to nurses, there was no difference in the quality of care provided (Laurant et al., Reference Laurant, Reeves, Hermens, Braspenning, Grol and Sibbald2007; Martinez-Gonzalez et al., Reference Martinez-Gonzalez, Tandjung, Djalali and Rosemann2015; Lovink et al., Reference Lovink, Persoon, Koopmans, Van Vught, Schoonhoven and Laurant2017; Laurant et al., Reference Laurant, van der Biezen, Wijers, Watananirun, Kontopantelis and van Vught2018). However, less is known about task shifting from doctors to nurses in the area of prevention and health education (Laurant et al., Reference Laurant, van der Biezen, Wijers, Watananirun, Kontopantelis and van Vught2018).
Some countries have a much longer tradition of task shifting than others. In the UK and The Netherlands, task shifting to practice assistants/nurses in primary care started as early as the 1980s (Van Tuyl et al., Reference Van Tuyl, Vis, Bosmans, Friele and Batenburg2020), while in other countries, like Belgium (Groenewegen et al., Reference Groenewegen, Heinemann, Greẞ and Schäfer2015) the dominance of small single-handed GP practices has hampered task shifting. More in general, barriers and facilitators may be sought in the degree of acceptance of task shifting among patients as well as healthcare professionals, in the organisation and resources of the practices and in regulation and other conditions at country or health system level (Maier and Aiken, Reference Maier and Aiken2016; Maier et al., Reference Maier, Aiken and Busse2017; van der Biezen et al., Reference Van der Biezen, Derckx, Wensing and Laurant2017; Nuttall, Reference Nuttall2018; Karimi-Shahanjarini et al., Reference Karimi-Shahanjarini, Shakibazadeh, Rashidian, Hajimiri, Glenton, Noyes, Lewin, Laurant and Colvin2019). Therefore, we expect to find a large variation in task shifting between the countries included in our study.
In this article, we report on a secondary analysis of the QUALICOPC study, involving a survey among GPs in 34 (mainly) European countries, conducted in 2012. We will first describe the extent of task shifting in these countries. Next, to understand potential barriers and facilitators to task shifting, we will analyse the associations between the extent of task shifting and a number of characteristics of the GPs, their practices and the health care systems in which they operate.
Hypotheses
Based on theories on readiness for change in general (Weiner, Reference Weiner2009) and on studies on barriers to implementation of task shifting in particular (Niezen and Mathijssen, Reference Niezen and Mathijssen2014; Karimi-Shahanjarini et al., Reference Karimi-Shahanjarini, Shakibazadeh, Rashidian, Hajimiri, Glenton, Noyes, Lewin, Laurant and Colvin2019), we developed a number of hypotheses on relationships, which are not necessarily causal. We expect that readiness for task shifting is influenced at the following three levels:
-
- level 1: the individual GPs and other professionals involved (e.g. their commitment; efficacy in bringing about task shifting),
-
- level 2: the practices they work in (e.g. experienced urgency of change in skill mix, available resources in the practice),
-
- level 3: the country or health system (e.g. urgency of task shifting as experienced at policy level; resources made available for this change; adaptation of costing of skill-mix changes).
Influences at different levels may independently increase or decrease the readiness for task shifting, but are also expected to influence each other. Commitment of care providers, for instance, may be impacted by the experienced urgency of change, and their ability to bring about change depends on the resources available in the primary care practice (Weiner, Reference Weiner2009).
Likewise, potential barriers and facilitators for task shifting can be identified at these three levels:
-
- level 1: individual GPs and practice assistants/nurses (e.g. their views on professional boundaries; knowledge and capabilities),
-
- level 2: the practice environment (e.g. patients’ preferences for a care provider, their acceptance of receiving care from practice assistants/nurses, their knowledge about and trust in practice assistants/nurses‘ work),
-
- level 3: the country and health system context (e.g. degree of policy support for task shifting; financial incentives; legal barriers for task shifting; positioning of professional associations; local or regional labour market shortages).
To identify the barriers at patient, GP and practice level, multi-level data is needed at the professional and practice level. For level 3 barriers, data is needed at the health system or country level influencing policies and policy options. As described below, the QUALICOPC study provides the required multi-level data to analyse the impact of these barriers in an integrative manner.
We will test the following hypotheses:
At the level of GPs:
-
- More innovative GPs have shifted more tasks to practice assistants/nurses.
-
Task shifting can be considered an innovation in the work organisation of general practices. We assume that younger GPs are more willing and capable to adopt innovations in their practices, as shown in the literature about the uptake of electronic health records (EHRs) (Xierali et al., Reference Xierali, Phillips, Green, Bazemore and Puffer2013). Following this line of reasoning, it is expected that GPs, who are more innovative in the use of information technology and systems in their practice, are more inclined to adopt task shifting.
-
-
- Part-time working GPs have shifted more tasks to practice assistants/nurses.
-
GPs working part-time are assumed to put more effort in maintaining continuity of care (Karimi-Shahanjarini et al., Reference Karimi-Shahanjarini, Shakibazadeh, Rashidian, Hajimiri, Glenton, Noyes, Lewin, Laurant and Colvin2019). Working part-time is a challenge to continuity because GPs are not always available for their patients during usual office hours. To maintain continuity of care during periods of absence, targeted efforts are needed to shift specific care tasks either to other GPs or to supporting staff. As female GPs more frequently work part-time (Van Hassel, Reference Van Hassel2020), we expect female GPs to have shifted more tasks to practice assistants/nurses than male GPs.
-
At the level of practices:
-
- Task shifting by GPs to practice assistants/nurses occurs to a larger extent in GP practices with more supporting staff.
-
Availability of staff enables task shifting; in the absence of support staff, it is not possible. So, the availability of supporting staff is a condition for task shifting. But still, given available supporting staff, we expect variation in the level of task shifting, as shifting requires teamwork (Van Tuyl et al., Reference Van Tuyl, Vis, Bosmans, Friele and Batenburg2020).
-
-
- Task shifting by GPs to practice assistants/nurses will occur to a larger extent in GP practices with a patient population with higher demands for care and more complex care needs.
-
Following Niezen and Mathijssen (Reference Niezen and Mathijssen2014), we expect that practices with relatively many patients that have more complex care needs (e.g. elderly), and practices located in rural areas (e.g. with ageing population or in under-served areas) or inner cities (with problems of deprivation) are faced with relatively higher workloads and will use task shifting to cope with these conditions.
-
At the level of countries/health systems:
-
- Task shifting by GPs to practice assistants/nurses will occur to a larger extent in countries where institutional facilitators outweigh barriers for task shifting
-
Task shifting can be strongly influenced by legal and regulatory barriers and facilitators (Van Schalkwyk et al., Reference Van Schalkwyk, Bourek, Kringos, Siciliani, Barry, De Maeseneer and McKee2020). In the Czech Republic, for example, GPs are required to employ a nurse, while in The Netherlands the costs of employing a practice nurse are formally reimbursed (Van Tuyl et al., Reference Van Tuyl, Vis, Bosmans, Friele and Batenburg2020).
-
-
- Task shifting by GPs to practice assistants/nurses will occur to a larger extent in countries with strongly ageing populations and/or lower or decreasing numbers of GPs per capita.
-
In such countries, policy makers may feel more urgency to promote task shifting, which will drive the employment of practice assistants/nurses and task shifting within practices.
-
-
- Task shifting by GPs to practice assistants/nurses will occur to a lesser extent in countries where professional boundaries between GPs and supporting and nursing staff are relatively strict.
-
Professional boundaries are particularly important in strongly organized occupations, such as medical doctors (Abbott, Reference Abbott1988). Shared views on professional boundaries may overrule GPs’ individual attitudes and willingness to shift tasks as well as popular trust in the capabilities of practice assistants/nurses to take on tasks (Van Tuyl et al., Reference Van Tuyl, Vis, Bosmans, Friele and Batenburg2020). As the guards of professional boundaries, professional associations have a keen interest in task-shifting issues (see Kroezen et al., Reference Kroezen, van Dijk, Groenewegen and Francke2011).
-
-
- Task shifting by GPs to practice assistants/nurses will occur to a larger extent in countries where professionalisation of practice assistants/nurses is more advanced.
-
As a counterforce to the position of medical associations, professional associations of practice assistants/nurses have a role in the promotion of task shifting. The more professionalised practice assistants/nurses are, the more task shifting will occur in primary care. Indicators for the professionalisation of practice nurses/assistants are, for example, the establishment of a professional association and education of practice assistants/nurses (Kroezen et al., Reference Kroezen, Schäfer, Sermeus, Hansen and Batenburg2018; Van Tuyl et al., Reference Van Tuyl, Vis, Bosmans, Friele and Batenburg2020).
-
Data and methods
The QUALICOPC study
Data were collected between 2011 and 2013 from approximately 7200 GPs in 31 European countries (EU 26 - except France -, and Iceland, Norway, North Macedonia, Turkey, Switzerland and England) and three non-European countries (Canada, New Zealand and Australia). In each country, a sample of around 220 GPs completed a questionnaire, except for small countries (Cyprus, Iceland, Luxembourg and Malta) where this was around 75. In most countries, a random sample of GPs was invited to participate. In countries without a national sampling frame, alternatives were sought as close as possible to a random sample. Only one GP per practice participated in the study. The participation rates varied from less than 10% in Austria and Belgium to over 70 % in Malta and Spain, with an average of 30% (Groenewegen et al., Reference Groenewegen, Greẞ and Schäfer2016).
Details of the study design and the development of the questionnaire can be found elsewhere (Schäfer et al., Reference Schäfer, Boerma, Kringos, De Maeseneer, Gress, Heinemann, Rotar-Pavlic, Seghieri, Svab, Van den Berg, Vainieri, Westert, Willems and Groenewegen2011; Reference Schäfer, Boerma, Kringos, De Ryck, Gress, Heinemann, Murante, Rotar-Pavlic, Schellevis, Seghieri, Van den Berg, Westert, Willems and Groenewegen2013). Ethical review was conducted in accordance with the legal requirements in each country (Rotar Pavlic et al., Reference Rotar Pavlic, Sever, Klemenc-Ketis and Svab2015).
Measures
Dependent variable
The degree of task shifting was measured through a sum score of GPs’ responses to the following questions on four different tasks: ‘Does your practice nurse or assistant independently provide: (1) Immunisation; (2) Health promotion; (3) Routine checks of chronically ill patients; (4) Minor procedures?’ Answering options were: ‘yes’ (counted as 1), and ‘no’ or ‘not applicable (no nurse in my practice)’ (counted as 0). Therefore, the composite score ranges between 0 and 4. We combined the categories ‘no’ and ‘not applicable’ (having no nurse or assistant to delegate tasks amounts to the same as not delegating these tasks).
Independent variables at GP practice level
-
- Innovativeness
As a first indicator for innovativeness, we used the number of EHRs applications used by GPs (De Rosis and Seghieri, Reference De Rosis and Seghieri2015). In the survey, GPs could select the following options (multiple answers possible): ‘Not applicable (I don’t use a computer)’; Making appointments; Issuing invoices; Issuing medicine prescriptions; Keeping records of consultations; Sending referral letters to medical specialists; Searching medical information on the Internet; Storing diagnostic test results; Sending prescriptions to the pharmacy. The answers were combined into a sum score, ranging from 0 (no computer use) to 8 (applying all EHR applications listed). Besides, as a second proxy for innovativeness, we used GPs’ age, assuming that younger GPs are more trained and familiar with using EHR applications.
-
- Part-time working
We do not have a direct measure of GPs’ part-time working status. Instead we used the GPs reported weekly workhours and added the average in a country as an offset in the statistical analysis.
-
- Availability of staff
Availability of staff at GP practice level was measured through two variables: availability of support and nursing staff (yes/no – receptionist/assistant, practice nurse, home care nurse or nurse practitioner); and other professionals (yes/no – other professionals in the practice).
-
- Practice location and population
Information on the practice location was derived from the answer to the question: How would you characterise the place where you are currently practising? (possible answers: big (inner)city, suburbs, (small) town, mixed urban-rural, rural). The practice composition was measured as the estimated proportion of elderly people; people from ethnic minorities and deprived people (possible answers: above average, average, below average).
Independent variables at country level:
-
- Institutional environment
In the absence of direct information to operationalise barriers or facilitators in the institutional environment of primary care practices, we assume that the institutional environment is more facilitating when it is more usual to have support staff in the practice. We therefore aggregated the number of practices without receptionist/assistant, practice nurse, home care nurse or nurse practitioner to country level.
-
- Demand for and supply of primary care
For demand and supply of primary care, we used the following three indicators. Firstly, population ageing, that is, the increase in the percentage of the population over 65 years old between 1993 and 2012 retrieved from World Bank data (Source: http://databank.worldbank.org/data/home.-aspx-
Secondly, GP shortages were derived from the PHAMEU framework (Primary Health Care Activity Monitor for Europe; Kringos et al., Reference Kringos, Boerma, Bourgueil, Cartier, Hasvold, Hutchinson, Lember, Oleszczyk, Rotar Pavlic, Svab, Tedeschi, Wilson, Windak, Dedeu and Wilm2010): Do (regional or national) shortages exist of GPs according to usual national norms? (No shortage = 3; Shortage in some regions = 2; Nation-wide shortage = 1; no info for Ireland and Luxemburg).
Finally, the ageing of GPs was measured by the percentage of GPs over 60 years of age (aggregated from the QUALICOPC data).
-
- Professional boundaries between GPs and supporting and nursing staff
As a proxy indicator for professional boundaries, we used data on whether nurses have prescription rights in a country. Using data from Kroezen et al. (Reference Kroezen, van Dijk, Groenewegen and Francke2011) and Maier (Reference Maier2019), we classified countries into three categories: 1 = no prescription rights (Austria, Belgium, Bulgaria, Czech Republic, Germany, Greece, Hungary, Iceland, Italy, Latvia, Lithuania, Luxemburg, Malta, North Macedonia, Portugal, Rumania, Slovakia, Slovenia, Turkey); 2 = prescription rights introduced after 2010 (Cyprus, Estonia, Netherlands, Poland, Spain and in one Canton in Switzerland); 3 = prescription rights granted up to 2010 (Australia, Canada, Denmark, Finland, Ireland, New Zealand, Norway, Sweden, UK). The category ‘prescription rights introduced after 2010’ was added because the introduction of nurse prescribing is a lengthy process (Maier, Reference Maier2019) and it is likely that in these countries professional boundaries between nurses and doctors were already under debate in the preceding years.
- Professionalisation of practice assistants/nurses: a scale consisting of the following indicators derived from the PHAMEU database (Kringos et al., Reference Kringos, Boerma, Bourgueil, Cartier, Hasvold, Hutchinson, Lember, Oleszczyk, Rotar Pavlic, Svab, Tedeschi, Wilson, Windak, Dedeu and Wilm2010):
-
- Is there professional training specifically for district or community nurses? (Yes/no)
-
- Is there professional training specifically for PC/GP practice nurses? (Yes/no)
-
- Do national associations or organizations of PC nurses exist in this country? (Yes/no)
-
- Is a professional journal on PC nursing being published in this country? (Yes/no).
Statistical analysis
The analysis was done using multi-level analysis to account for the nested structure of the data (Leyland and Groenewegen, Reference Leyland and Groenewegen2020). We used the random effects (variances) at GP and country level to describe the clustering of task shifting by GPs. The country-level variances were used to construct a caterpillar plot to show the differences between countries on the task-shifting scale. The GP, practice and country variables were included in a multi-level linear regression analysis with the scale value as dependent variable.
For the GP and practice characteristics, we used list-wise deletion of missing values. As the number of countries is relatively small for statistical analysis, we included country-level variables one at a time. We use P < 0.05 as the boundary value for statistical significance.
The modelling strategy consists of the following steps:
-
1. empty model to calculate the clustering of the dependent variable within GP practices and countries;
-
2. adding GP and practice variables and average number of working hours per country;
-
3. average number of working hours dropped and country variables (one-by-one) added.
Analyses were performed in MLwiN, version 2.30.
Ethical approval
Ethical approval for the QUALICOPC study was acquired in accordance with the legal requirements in each country (De Rosis and Seghieri, Reference De Rosis and Seghieri2015).
Results
Descriptive data on the independent variables are provided in Supplementary Table 1. We distinguish between variables measured at the GP and practice level and variables measured at the country level. Across, all practices and countries, the average number of EHR applications used for clinical purposes was 6 on a scale from 0 to 8. The average age of GPs was 50 years. On average, they worked 40 h per week. Most GPs had nurses/practice assistants or secretaries as support staff and in 11% of the practices also other professionals were active. Nearly one-third of the practices were located in cities. The GPs reported mainly an average share of elderly and socially deprived people in their practice and a lower than average share of people from ethnic minorities.
For variables measured at the country level, in one-fifth of the countries, there was no shortage of GPs. The average percentage of GPs of 60 years and over was 17. In more than half of the countries, nurses had no prescribing rights at the time of the survey and the scale for professionalisation averaged 7.2 on a scale from 4 to 12.
Figure 1 shows the distribution of the task-shifting scale for the 34 countries in the study. The frequency distributions of the separate items of the scale are in Supplementary Tables 2–5. Countries differ in the occurrence of task shifting from GPs to nurses and/or assistants Task shifting is most common in England, FYR Macedonia and Sweden, while Switzerland, Austria and Bulgaria are in the lower end of the distribution. The large variation between countries are also reflected in the Intra Class Correlation which is 21% (Table 1).
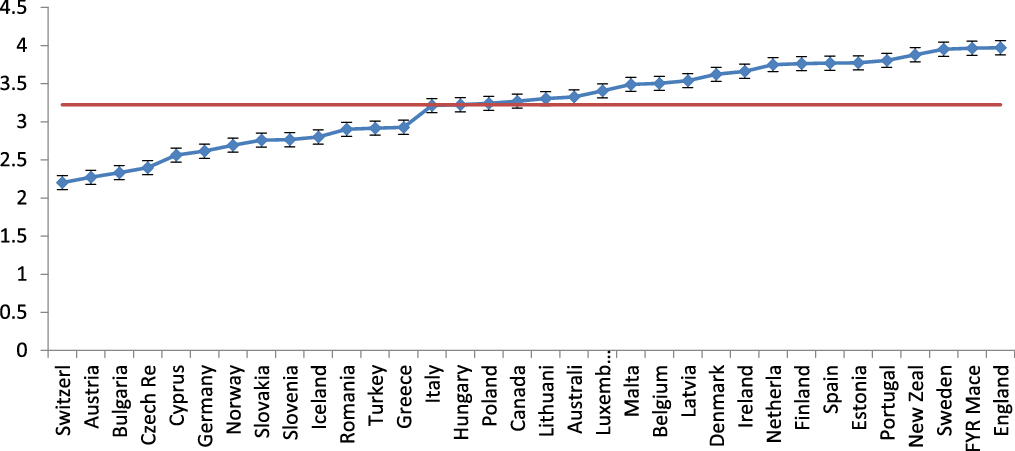
Figure 1. Task shifting scale by country (based on empty model).
Table 1. Linear multilevel regression analysis of task shifting in general practice (N countries = 34; nGPs = 6,257)

* P < 0.05; ** P < 0.01.
a Coefficients of GP/practice level variables and random effects taken from model 3 with the professionalisation scale as an independent variable at country level.
b No information for Ireland, Luxembourg, Canada.
c No information for Malta.
With respect to the GP and practice variables, only the use of EHR applications and the age of the GPs are significantly related to task shifting (Table 1). GPs that use more different EHR applications, have shifted more tasks to nurses and/or assistants, the same applies for older GPs. The GP and practice variables explain very little of the variance in task shifting at the level of GPs.
Regarding the country variables, nurse prescribing and professionalisation of primary care nursing are positively related to task shifting by GPs. The latter of the two shows the strongest relationship and explains 21% of the country variation in task shifting by GPs (100 − [country variance in model 2 with nurse prescribing, divided by the country variance in the empty model] × 100).
Discussion
In 2012, task shifting in primary care to nurses/assistants was very common in the 34 countries included in our study. The extent of task shifting by GPs differs between countries with England on the high end of the distribution and Switzerland on the low end. We tested a number of hypotheses related to GP, practice and country characteristics. Three hypotheses were confirmed. First, GPs that use more EHR applications in their practice more often shifted tasks to nurses or assistants. We used a computer to use as an indicator for innovativeness. Second, in countries where nurses have prescribing rights, GPs have shifted tasks to nurses/assistants to a greater extent. We have used this as an indicator for less strict professional boundaries. Finally, in countries that score higher on a scale for professionalisation of primary care nurses, task shifting by GPs is also more prevalent. Our other hypotheses were all refuted. Hence, it appears that increasing (complexity of) demand for care and (expected future) lack of GPs are not related to task shifting. Remarkable is the fact that older GPs, contrary to our hypothesis, have shifted task to a larger extent than younger GPs.
Our first confirmed hypothesis related to innovativeness (Greenhalgh et al., Reference Greenhalgh, Robert, Macfarlane, Bate and Kyriakidou2004). The use of computers in practice for more different purposes indicates the readiness of GPs and their practices to implement innovations. However, our reasoning that younger GPs are more open to innovations, was apparently not correct, as it is not related to the extent of task shifting. A possible explanation may be that older GPs have more insight into the competences of their support staff (who perhaps are also older and more experienced) to take over tasks. Where shifting of particular tasks to practice assistants/nurses is not formally allowed, it is possible that older GPs yet take more liberty to delegate tasks informally. Another explanation may be that older, more experienced GPs increasingly shift their own tasks towards management of their practice, hence shifting tasks related to patient care in the direction of other support staff. However, these explanations should be tested independently. In sum, our analysis suggests that the extent of task shifting is related to innovativeness at GP level and to professional boundaries between nurses and doctors and professionalisation of practice nurses at the country level.
The two confirmed hypotheses about professional boundaries and professionalisation of practice assistants/nurses relate to the system character of the position of different health care professions and their mutual relations (Abbott, Reference Abbott1988). This shows that task shifting should not be considered in isolation and that it is sensitive to the context. It is part of broader processes of inter-professional domain setting, which are intertwined with the educational system and the development of mutual trust between doctors, practice assistants/nurses and patients (Frenk et al., Reference Frenk, Chen, Bhutta, Cohen, Crisp, Evans, Fineberg, Garcia, Ke, Kelley, Kistnasamy, Meleis, Naylor, Pablos-Mendez, Reddy, Scrimshaw, Sepulveda, Serwadda and Zurayk2010). Consequently, although the initiative of task shifting will often be within practices, our study shows the importance of a facilitating environment at a system level. We used nurse prescribing rights as an indicator for debates on professional boundaries. Admittedly, these debates do not necessarily lead to less strict boundaries (as we formulated in our hypothesis), but may also lead to new, strict boundaries. In our view, the debate about prescription rights of nurses in itself indicates that change is possible and as such this makes for an environment in which task shifting will be seen as an option. It should be added that nurse prescribing is a form of task shifting; however, we are convinced that we can still use it as part of the explanation of task shifting in general practice, because nurse prescribing tends to be introduced in the hospital context first.
At health system level, cost containment may also have played a role in policies that support shift tasks from GPs to nurses and support personnel. However, there is hardly any information about national policies regarding task shifting, but we know that the value of teamwork and the optimal team skill mix are considered important policy issues in many countries (Van Schalkwyk et al., Reference Van Schalkwyk, Bourek, Kringos, Siciliani, Barry, De Maeseneer and McKee2020). Related to this, we did not have information about the education and skills of practice nurses/assistants employed in the practices in our survey. Most likely, these differ between and within countries. From a quality of care perspective, an additional question is how practice nurses/assistants perform the tasks that have been shifted to them and how this differs between GP practices. Systematic reviews have shown that the quality of care performed by nurses is at least as good as care from GPs (Laurant et al., 2007; Reference Laurant, van der Biezen, Wijers, Watananirun, Kontopantelis and van Vught2018; Lovink et al., Reference Lovink, Persoon, Koopmans, Van Vught, Schoonhoven and Laurant2017; Martinez-Gonzalez et al., Reference Martinez-Gonzalez, Tandjung, Djalali and Rosemann2015).
Our hypotheses concerning the role of increasing (complexity of) demand for care and (expected future) lack of GPs on task shifting were not confirmed. Yet, these developments have further progressed in many countries, with a strong impact on the workload and availability of GPs for which task shifting can be among the solutions. This makes an insight into barriers and facilitators to task shifting important to pave the way for new initiatives to unfold. Task shifting from GPs to nursing and support staff can be considered as one of the first emerging forms of task shifting. However, also other professionals play increasingly important roles in the strengthening of primary care organisation. Several countries invested in task shifting from GPs to pharmacists. In Canada, New Zealand, the USA and the UK, pharmacists have to prescribe rights with varying levels of responsibilities. In the Netherlands, experiments with pharmacists as clinical care provider in primary health care teams and employees within a GP practice show promising results in terms of improved safety and effectiveness of pharmacotherapy in primary care, including a reduced risk of medication-related hospitalisations compared to usual care (Sloeserwij et al., Reference Sloeserwij, Hazen, Zwart, Leendertse, Poldervaart, de Bont, de Gier, Bouvy and de Wit2019).
Our analysis and the data that we used have a number of strengths and limitations, some of which were already mentioned. We have data from a large number of countries, 34. This makes a statistical analysis at both GP/practice and country/health system level possible. We applied state of the art statistical analysis that takes the hierarchical character of the data into account. The response rates for the QUALICOPC study differed, but averaged around 30%. The samples were as much as possible random samples, but this was not attainable in all countries. We expect that this bias was not strong as the sample distribution by age and sex of GPs was close to the national distribution (Groenewegen et al., Reference Groenewegen, Greẞ and Schäfer2016). However, as in any survey study, there may be non-response bias. Social desirability might have influenced some of the answers, in particular at the positive extreme of the distribution of the scale for task shifting. Such as in the FYR Macedonia, where other information shows only a minor role for nurses in GP practices (WHO, 2019).
We performed a secondary analysis of existing data, not specifically designed to study task shifting. Consequently, the measurements were quite general. A further limitation is that the data are by now somewhat old. This is particularly relevant for the descriptive value of the study, but our hypothesis testing is less sensitive to this. If our data collection would be repeated as of now, we expect to see effects of different changes over time. For example, there is increased acceptance of task shifting by the population, e.g. in Germany (Jedro et al., Reference Jedro, Holmberg, Tille, Widmann, Schneider, Stumm, Döpfmer, Kuhlmey and Schnitzer2020). Computer use in primary care practices will have increased even further. Prescribing rights of nurses are more prevalent today than at the time of data collection, but we used the formalisation of such prescribing rights in more recent times as an indicator for the debate about professional boundaries which was likely going on when data was collected. We have no data on changes in the aspects of professionalisation of practice nurses/assistants.
Finally, it should be emphasised that the associations we found cannot be considered as causal associations. Inter-professional relations have a system character and complex feedbacks (Abbot, Reference Abbott1988). An implication of the importance of the system level is that there are no easy recipes for introducing task shifting from GPs to practice assistants/nurses in countries where this is not yet prevalent. Simply transferring an innovation from one health care system to another often does not work (Nolte and Groenewegen, Reference Nolte and Groenewegen2021). Finally, the absence of information on education, skills and competences, and the quality of task performance has limited the scope of our study.
Conclusions
Task shifting by GPs to practice assistants/nurses can be an answer to current challenges in primary care. The extent of task shifting in a country strongly benefits from a facilitating national context. Within countries, task shifting is more prevalent in practices with an innovating attitude and among older GPs. Given the importance of the subject of task shifting, we recommend an assessment of changes in this area in the countries studied in a new survey.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1463423621000657
Acknowledgements
The authors thank their partners in the QUALICOPC project; J De Maeseneer, J Detollenaere, L Hanssens, S Willems (Belgium); S Greß, S Heinemann (Germany); G Capitani, S De Rosis, AM Murante, S Nuti, C Seghieri, M Vainieri (Italy); D Kringos, T Van Loenen (the Netherlands); D Rotar Pavlič, I Švab (Slovenia). The authors thank the coordinators of the data collection in each country: L Jorm, I McRae (Australia); K Hoffmann, M Maier (Austria); P Salchev (Bulgaria); W Wodchis, W Hogg (Canada); G Samoutis (Cyprus); B Seifert, N Šrámková (Czech Republic); J Reinholdt Jensen, P Vedsted (Denmark); M Lember, K Põlluste (Estonia); E Kosunen (Finland); C Lionis (Greece); I Rurik (Hungary); J Heimisdóttir, O Thorgeirsson (Iceland); C Collins (Ireland); G Ticmane (Latvia); S Macinskas (Lithuania); M Aubart, J Leners, R Stein (Luxembourg); G Bezzina, P Sciortino (Malta); T Ashton, R McNeill (New Zealand); T Bjerve Eide, H Melbye (Norway); M Oleszczyk, A Windak (Poland); L Pisco (Portugal), D Farcasanu (Romania); E Jurgova (Slovakia); T Dedeu (Spain); C Björkelund, T Faresjö (Sweden); T Bisschoff, N Senn (Switzerland); K Stavric (The former Yugoslav Republic of Macedonia); M Akman (Turkey); C Sirdifield, N Siriwardena (United Kingdom).
Financial support
This article is based on data from the QUALICOPC (Quality and Costs of Primary Care in Europe) project, co-funded by the European Commission under the Seventh Framework Programme (FP7/2007-2013) under grant agreement 242141. For this secondary analysis, no separate funding was received.
Conflict of interest
None
Ethical standards
Ethical review was conducted in accordance with the legal requirements in each country.





