An estimated 2.4% of United States children, or 1.7 million children, aged 0–17 years have a past or current heart condition.Reference Chen, Riehle-Colarusso, Yeung, Smith and Farr1 Heart conditions may include congenital and acquired heart disease and syndromes affecting the heart. Compared to children without heart conditions, children with heart conditions, particularly those with congenital heart defects (CHDs), need life-long, specialty care.Reference Stout, Daniels and Aboulhosn2 Barriers to healthcare among children with heart conditions may include insufficient health insurance coverage, lack of proximity to healthcare providers with expertise in CHD, and unequal access to healthcare information related to CHD.Reference Jenkins, Botto and Correa3 Racial disparities in health are caused by structural racismReference Churchwell, Elkind and Benjamin4,Reference Williams and Cooper5 – the conglomeration of mutually reinforcing, inequitable systems that reinforce discriminatory beliefs, values, and distributions of resources within a society.Reference Krieger6 Pathways through which structural racism affects health include economic injustice, social deprivation, and inadequate healthcare access and treatment.Reference Bailey, Krieger, Agénor, Graves, Linos and Bassett7
Despite advancements in medical care and increased survival of infants with heart conditions into adulthood, racial disparities in timing of diagnosis,Reference Krishnan, Jacobs and Morris8 lapses in medical care,Reference Jackson, Morack, Harris, DeSalvo, Daniels and Chisolm9 preventive care utilisation,Reference Broughton, Riehle-Colarusso, Nehl, Riser and Farr10 quality of care,Reference Broughton, Riehle-Colarusso, Nehl, Riser and Farr10 and mortalityReference Boneva, Botto, Moore, Yang, Correa and Erickson11–Reference Oster, Strickland and Mahle14 persist. Using Healthy People 2030’s framework of social determinants of health,15 identifying disparities in socio-economic status, education access and quality, and healthcare access and quality may provide insights into ways to improve the survival and overall health of all children with heart conditions. Thus, the objectives of this analysis were to (1) assess differences in socio-economic status, access to healthcare, and healthcare utilisation by presence of a heart condition and (2) assess differences in these outcomes by race/ethnicity among children with heart conditions.
Materials and method
National Survey of Children’s Health
We performed a cross-sectional analysis of caregiver-reported data from the 2016–2019 National Survey of Children’s Health, a population-based survey of the physical and emotional health of non-institutionalized United States children 17 years or younger. Households were randomly sampled from all 50 states and the District of Columbia. Among households identified with children, households with indicators of receipt of Supplemental Security Income or households living in areas of high poverty were sampled first. One child per household was selected. For households with multiple children, children aged 0–5 years and children with special healthcare needs were oversampled at a rate of 60 and 80%, respectively. National Survey of Children’s Health oversamples children aged 0–5 and children with special healthcare needs to produce sufficient subgroup sizes to examine less common outcomes among them. Up to two primary caregivers were surveyed per child. Surveys were offered in Spanish and English in web-based, paper, and telephone-assisted formats. From 2016 to 2019, the weighted overall response rate ranged from 37.4 to 43.1%. Data were weighted to account for non-response bias and to produce population-based estimates.
Measures
All measures were caregiver-reported. Exposures of interest were child’s heart condition status and race/ethnicity. Children were considered to have a heart condition if their caregiver answered “yes” to the following survey question: “Has a doctor or other healthcare provider EVER told you that this child has a heart condition?” Child’s race/ethnicity was combined into the following categories: Hispanic, non-Hispanic White alone, and Non-Hispanic Black or African American alone. Non-Hispanic children of other race/ethnicities or multiple race/ethnicities were excluded due to low sample size among each group. (For non-Hispanic American Indian or Alaska Native, non-Hispanic Asian, non-Hispanic Native Hawaiian and Other Pacific Islander, non-Hispanic other, and non-Hispanic multiracial children, the total n was 15,562 [12.6%, range n = 273–7620] and among heart conditions was 327 [11%, range n = 8–187]) Missing data on race/ethnicity, representing <1% of children, were multiply imputed.
Covariates of interest included child’s age and sex at birth. We grouped child’s age into three categories: 0–6, 7–11, and 12–17 years. Child’s sex at birth was defined as male or female. Missing data on age and sex were multiply imputed. We also examined primary language spoken at home, which was dichotomised as English and a language other than English.
The outcomes of this analysis broadly fall under three social determinants of health: socio-economic status, healthcare access, and healthcare utilisation. For socio-economic status, we examined caregiver’s educational attainment and work status. We categorised educational attainment, based on information from up to two caregivers, as all surveyed caregivers having less than or equal to high school education and at least one having greater than high school education. Similarly, we defined caregiver’s work status as “employed” if at least one caregiver indicated that he/she was employed at least 50 of the past 52 weeks, and “unemployed” if no caregivers were employed for at least 50 of the past 52 weeks.
For healthcare access, we examined child’s insurance type, child’s usual place of care, and whether the caregiver had problems paying for the child’s healthcare in the past 12 months. We dichotomised child’s health insurance type as any private (private only or public and private) and public, other, or no insurance. To determine child’s usual place of care, caregivers were asked “Is there a place you or another caregiver USUALLY take this child when they are sick or you need advice about their health?” and “Where does this child USUALLY go first?…Mark ONE only”. Children whose reported usual place of care was a doctor’s office or clinic/health centre were considered to have a usual place of care. Children who were usually taken to a place other than a doctor’s office or clinic/health centre (e.g. an emergency room) or who had no usual place were considered not to have a usual place of care. The child’s family was considered to have problems paying for healthcare if caregivers responded yes to the following question: “DURING THE PAST 12 MONTHS, did your family have problems paying for any of this child’s medical or healthcare bills?” Caregivers who answered “no” or who paid $0 for their child’s healthcare in the past 12 months, and were therefore not asked the question on problems paying for care, were considered to have no problems paying for care.
For healthcare utilisation, we examined any preventive healthcare visits in the past 12 months, any specialty healthcare visits in the past 12 months, number of hospital emergency room visits in the past 12 months, and unmet need for care. Children who had no healthcare visits in the past 12 months were considered to have no preventive care or emergency room visits. To assess preventive healthcare in the past 12 months, caregivers were asked: “DURING THE PAST 12 MONTHS, how many times did this child visit a doctor, nurse, or other health care professional to receive a PREVENTIVE check-up? … A preventive check-up is when this child was not sick or injured”. We dichotomised this variable as zero and one or more. To assess number of emergency visits, caregivers were asked “DURING THE PAST 12 MONTHS, how many times did this child visit a hospital emergency room?” We defined number of emergency room visits as 0, 1, or 2+ emergency room visits. To measure specialty care, caregivers were asked “DURING THE PAST 12 MONTHS, did this child see a specialist other than a mental health professional? … Specialists are doctors like surgeons, heart doctors, allergy doctors, and others who specialize in one area of health care”. We defined needed specialty care as “Yes” and “No, but this child needed to see a specialist”. Children were considered to have unmet need for care if the parent answered “yes” to the following survey question: “DURING THE PAST 12 MONTHS, was there any time when this child needed health care but it was not received? … Health care includes medical care, dental care, vision care, and mental health services”.
Data analysis
We excluded children missing any variables of interest. Using chi square tests, we compared weighted prevalence of all social determinants of health outcomes, by heart condition status and race/ethnicity. Using the predicted marginal approach to multivariable logistic regression, adjusted for age and sex, we calculated adjusted prevalence ratios and 95% confidence intervals to examine the associations between heart condition status and each dichotomous outcome. For number of hospital emergency room visits, a three-level variable, we used the predicted marginal approach to multinomial logistic regression using a generalised logit link function. We also examined the associations between race/ethnicity and each outcome among children with and without heart conditions, separately. Among children with heart conditions, we examined effect modification in the association between race/ethnicity and outcomes by caregiver work status and educational attainment. As a sensitivity analysis, among children with heart conditions, we dichotomised Hispanic children into two groups: Hispanic children from primarily English-speaking households and Hispanic children from households primarily speaking a language other than English and compared outcomes between each group and non-Hispanic White children.
All analyses were conducted using SAS-callable SUDAAN. All estimates accounted for complex sampling and were weighted for non-response and to produce population-based national estimates. To create population-based estimates, the National Survey of Children’s Health assigns a weight for each child, comprised of the probability of the child’s household being sampled, adjustment for non-response, and adjustments for demographic characteristics of the sampled children relative to the general US population (e.g. state, race, Hispanic ethnicity, sex, and age). More detailed information on sampling and weighting can be found in the National Survey of Children’s Health Methodology Reports.16–19 This analysis was exempt from human patients review due to the de-identified nature of this secondary dataset.
Results
Of the 114,942 children of non-Hispanic White, non-Hispanic Black, or Hispanic race/ethnicity in the 2016–2019 National Survey of Children’s Health, 359 children were excluded for missing information on heart condition status. Of the 2795 children with heart conditions and 111,788 without heart conditions, 163 (5.8%) and 6947 (6.2%), respectively, were excluded for missing data on other study variables. Our analytic sample comprised 104,841 children, 2632 with heart conditions, who were statistically weighted to represent 1.3 million United States children, or 2.2% of all United States children. Among children with heart conditions, children with missing data were more likely to have caregivers with a high school education or less and less likely to have problems paying for care (Supplementary Tables S1).
Non-Hispanic White children represented 65.4% and 58.0% of children with and without heart conditions, respectively (Table 1). Among children with heart conditions, 35.2% were 12–17 years old and 52.0% were male, compared to 34.3% and 51.1%, respectively, among children without heart conditions (p > 0.05 for both). Among children with heart conditions, we observed no differences by race/ethnicity across age and sex strata; however, among children without heart conditions, we found that 37.4% of non-Hispanic Black children were 12–17 years old, compared to 33.8% of non-Hispanic White and Hispanic children, respectively (p < 0.001).
Table 1. Demographic characteristics of children with and without heart conditions, National Survey of Children’s Health 2016–19.

1 Comparing characteristics by race/ethnicity among children with heart conditions.
2 Comparing characteristics by race/ethnicity among children without heart conditions.
3 Comparing characteristics by heart status among all children.
CI = confidence interval.
Comparing children with and without heart conditions
Almost one in five (19.7%) children with heart conditions compared to 23.5% of children without heart conditions did not have a usual place of medical care (p = 0.02; adjusted prevalence ratio [95% confidence interval]: 0.8 [0.7, 1.0]); less than one in ten children with heart conditions (9.9%) compared to 19.8% of children without heart conditions had not received preventive healthcare in the past 12 months (p < 0.001; 0.5 [0.4, 0.6]). However, for 18.0% of children with heart conditions compared to 10.5% of those without heart conditions caregivers reported having problems paying for the child’s medical care (p < 0.001; 1.7 [1.5, 2.0]) (Fig 1). Children with heart conditions were more likely to have one (22.4% versus 15.1%; (1.5 [1.3, 1.7]) and two or more (10.6% versus 4.5%; (2.4 [1.9, 3.0]) emergency room visits in the past 12 months (p < 0.001) and unmet need for healthcare (5.6% versus 2.9%; p < 0.001; 1.9 [1.4, 2.5]). Among children with heart conditions, 2.2% reported needing medical care, 1.9% dental care, 0.9% vision care, 1.8% mental health services, and 1.1% another type of care; 1.8% reported needing two or more types of care. The most frequently reported reasons contributing to children with heart conditions not receiving needed health services were issues related to cost (60.1%), difficulties getting an appointment (54.2%), ineligibility for services (27.5%), services unavailable in their area (24.4%), and transportation (16.3%).
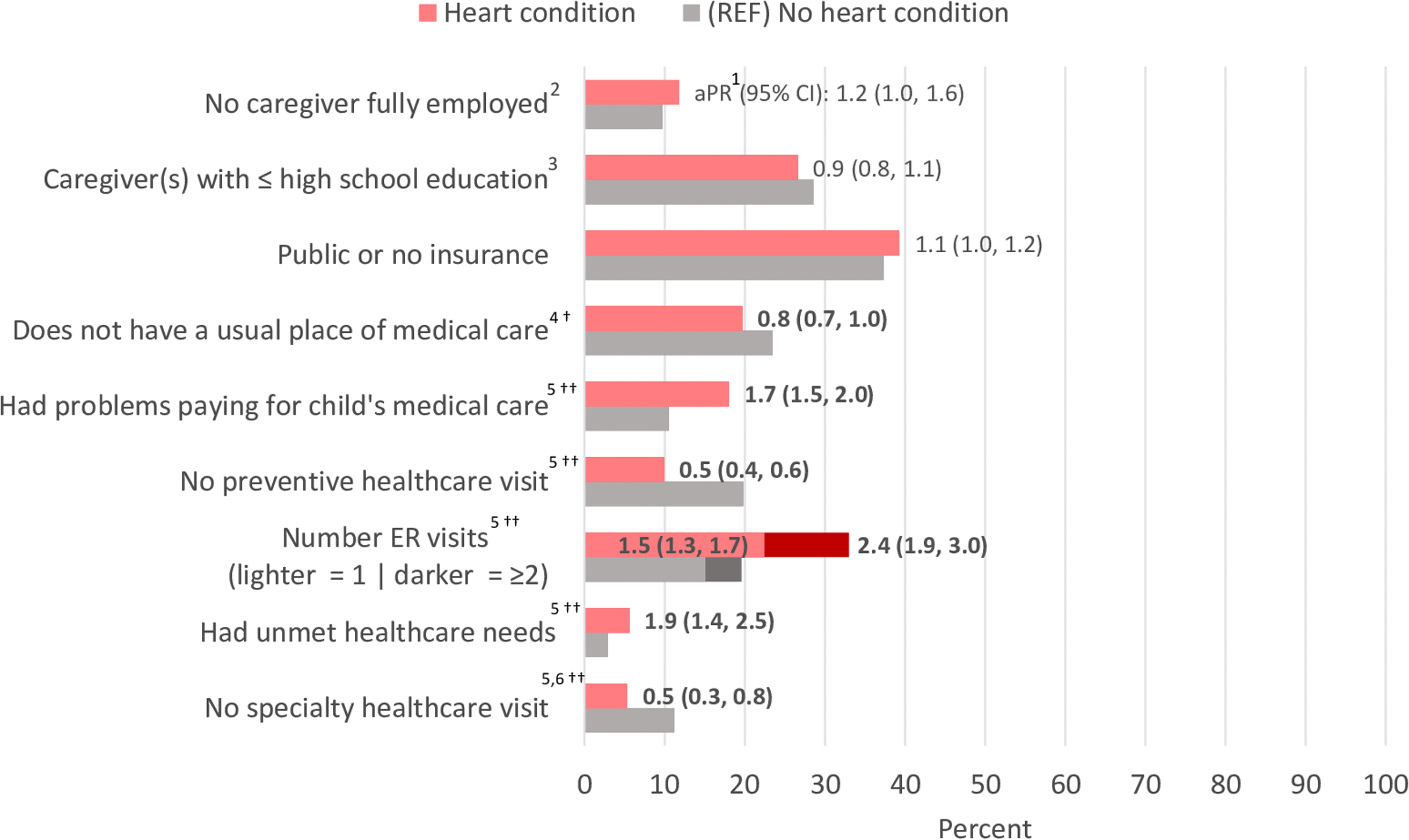
Figure 1. Prevalence and adjusted prevalence ratios of indicators of family socioeconomic status, health care access, and health care utilization among U.S. children with and without heart conditions, National Survey of Children’s Health 2016-19 aPR: adjusted prevalence ratio; CI: confidence interval; ER: emergency room; Bolded aPRs: statistically significant; 1Adjusted for age, sex; 2No caregiver(s) are employed at least 50 of the past 52 weeks; 3All caregiver(s) have a high school education or less; 4Those who did not receive their usual care at a doctor's office received care at a hospital ER or OD, retail store clinic or ‘Minute Clinic,’ school, some other place, or no place; 5in past 12 months; 6Among 1,318 and 19,082 children with and without heart conditions, respectively, who needed a specialty healthcare visit; †=p<0.05; ††=p<0.01.
Among the 1318 children with and 19,082 without heart conditions who needed to see a specialist, 5.3% of children with heart conditions and 11.2% of children without heart conditions did not receive specialty healthcare in the past 12 months (p < 0.001; adjusted prevalence ratio = 0.5 [0.3, 0.8]). We found only 3.2% of children with heart conditions had no insurance; therefore, we combined this category with public or no insurance. We found no difference in caregiver educational attainment and work status, and child’s health insurance type by heart condition status.
Racial/ethnic disparities in outcomes among children with heart conditions
Among children with heart conditions, caregiver employment (p = 0.007) and education (p = 0.048) differed by race/ethnicity. Specifically, among children with heart conditions, Hispanic children, compared with non-Hispanic White children, were more likely to have no caregiver employed at least 50 of the past 52 weeks (15.4% versus 8.0%; 1.9 [1.0, 3.5]) and have caregiver(s) with a high school education or less (33.1% versus 22.7%; adjusted prevalence ratio [95% confidence interval]: 1.5 [1.0, 2.1]). Compared with non-Hispanic White children, non-Hispanic Black children were also more likely to have no caregiver employed at least 50 of the past 52 weeks (24.7% versus 8.0%; 3.2 [1.9, 5.2]) and have caregiver(s) with a high school education or less (35.7% versus 22.7%; 1.6 [1.1, 2.3]) (Fig 2; for exact estimates see supplemental materials).

Figure 2. Adjusted prevalence ratios of indicators of family socioeconomic status, health care access, and health care utilization by race/ethnicity among U.S. children with heart conditions, National Survey of Children’s Health 2016-19 aPRs: adjusted prevalence ratios; CI: confidence interval; ER: emergency room; 1Adjusted for age, sex; 2No caregiver(s) are employed at least 50 of the past 52 weeks; 3All caregiver(s) have a high school education or less; 4Those who did not receive their usual care at a doctor’s office received care at a hospital ER or OD, retail store clinic or ‘Minute Clinic,’ school, some other place, or no place; 5in past 12 months; 6Among 1,318 and 19,082 children with and without heart conditions, respectively, who needed a specialty healthcare visit.
Differences by race/ethnicity among children with heart conditions were also seen for insurance type (p < 0.001) and having a usual place of care (p = 0.001). Specifically, among children with heart conditions, Hispanic compared with non-Hispanic White children were more likely to have public or no insurance (54.8% versus 29.6%; adjusted prevalence ratio = 1.9 [1.5, 2.4]) and no usual place of medical care (26.3% versus 14.5%; 1.8 [1.2, 2.7]). Compared with non-Hispanic White children, non-Hispanic Black children were also more likely to have public or no insurance (62.1% versus 29.6%; 2.1 [1.7, 2.7]) and no usual place of medical care (33.9% versus 14.5%; 2.3 [1.6, 3.4]). Estimates for public insurance did not change substantially when 73 children with no insurance were removed from the model (Hispanic adjusted prevalence ratio = 2.0; non-Hispanic Black adjusted prevalence ratio = 2.3). There were no racial/ethnic disparities in having problems paying for child’s medical care among children with and without heart conditions.
Among children with heart conditions, no racial/ethnic disparities were seen in receipt of preventive or specialty healthcare visits in the past 12 months or unmet need for healthcare in the past 12 months (p > 0.05 for all). However, Hispanic and non-Hispanic Black children, compared with non-Hispanic White children, respectively, were more likely to have ≥ 2 emergency room visits in the past 12 months (14.1%, 18.3% versus 7.8%, p < 0.001; 1.8 [1.0, 3.2] and 2.3 [1.3, 4.3]).
The racial/ethnic disparities seen in socio-economic status and healthcare access among children with heart conditions were also seen among children without heart conditions (Supplementary Tables S2 and S3).
Among 287 children of Hispanic ethnicity with heart conditions and information on language primarily spoken at home, 27.1% primarily spoke a language other than English at home (n = 10 (3.4%) missing data on language spoken at home). Hispanic children from households who primarily spoke a language other than English were more likely than non-Hispanic White children not to have received preventive (21.7% versus 8.8%; 2.5 (1.2, 5.2)) or specialty (16.5% versus 4.0%; 3.9 (1.1, 13.7)) healthcare in the past 12 months, although chi square p-values were not statistically significant, likely due to smaller sample size (p > 0.05). No disparities were seen between Hispanic children from primarily English-speaking households and non-Hispanic White children in not receiving preventive (9.6% versus 8.8%; adjusted prevalence ratio 1.1 (0.5, 2.4)) or specialty (3.5% versus 4.0%; 0.8 (0.2, 2.8)) healthcare in the past 12 months. Associations between Hispanic ethnicity and other outcomes did not differ substantially by language spoken at home.
When limited to children with heart conditions whose caregiver(s) were employed throughout the year, differences by race/ethnicity were seen for emergency room visits (p = 0.006). Specifically, compared to non-Hispanic White children, Hispanic children were 2.4 [1.3, 4.4] times more likely to have ≥2 emergency room visits in the past 12 months (14.8% versus 6.2%). Compared to non-Hispanic White children, non-Hispanic Black children were no more likely to have ≥2 emergency room visits in the past 12 months (6.8% versus 6.2%; 1.0 [0.5, 2.1]). When limited to children with heart conditions who have caregiver(s) with greater than a high school education, differences by race/ethnicity were seen for emergency room visits (p = 0.002) and insurance type (p < 0.001). Specifically, compared to non-Hispanic White children, Hispanic children were 2.8 [1.6, 5.2] times more likely to have ≥2 emergency room visits in the past 12 months (16.4% versus 6.1%) and 2.8 [2.0, 3.8] times more likely to have public or no insurance (46.4% versus 16.9%). Compared to non-Hispanic White children, non-Hispanic Black children were 2.0 [0.9, 4.6] times more likely to have ≥2 emergency room visits in the past 12 months (12.1% versus 6.1%) and 3.1 [2.3, 4.1] times more likely to have public or no insurance (51.4% versus 16.9%).
Discussion
In this analysis of over 2600 United States children with heart conditions, we found that children with heart conditions were more likely than children without heart conditions to have parents reporting problems paying for child’s medical care, unmet needs for healthcare, and need for emergency care. In addition, non-Hispanic Black and Hispanic children with heart conditions were more likely than their non-Hispanic White counterparts to have parents with less education and lower employment, to have public or no health insurance and no usual place of medical care, and to need more emergency care. For Hispanic children, associations were stronger for those from non-English speaking households. These findings show that children with heart conditions may have greater healthcare needs that more commonly go unmet compared to children without heart conditions, and non-Hispanic Black and Hispanic children with heart conditions may experience lower socio-economic status and even greater barriers to healthcare than non-Hispanic White children with heart conditions.
Among children with heart conditions, almost one in five had parents who reported trouble paying for care and over one in 20 had unmet healthcare needs, approximately twice the prevalence of children without heart conditions. Financial stress is prevalent among families of children with CHD, especially families of low socio-economic status or families with children who have severe CHD or special healthcare needs.Reference Ludomirsky, Bucholz and Newburger20,Reference Connor, Kline, Mott, Harris and Jenkins21 Financial difficulty has been associated with delayed care and adverse health outcomes among children with CHD.Reference Ludomirsky, Bucholz and Newburger20,Reference McClung, Glidewell and Farr22 In a nationally representative study of 188 United States families of children with CHD, a quarter who were unable to pay medical bills delayed or never received needed care for their child.Reference Ludomirsky, Bucholz and Newburger20 Delayed care may further result in the need for emergency care.Reference Gurvitz, Valente and Broberg23 In this study, approximately one in five children with heart conditions had visited the emergency room once in the previous 12 months and one in ten had visited two or more times, around two to three times that of children without heart problems, respectively. Among children with heart conditions, reasons for higher emergency room use may be due to the need for urgent cardiac care determined by the family or treating physician. This disparity in emergency room use was most prominent among Hispanic and non-Hispanic Black children with heart conditions among whom one in six and one in seven visited the emergency room two or more times in the preceding 12 months.
This study found further disparities in socio-economic status and healthcare access and utilisation by race and ethnicity among children with heart conditions. Approximately one in three caregivers of non-Hispanic Black and Hispanic children had less than a high school education, compared to one in five caregivers of non-Hispanic White children. Previous studies found associations between caregiver educational attainment and poor outcomes among children with CHD.Reference Kucik, Nembhard and Donohue24–Reference Kucik, Cassell and Alverson28 Recent systematic reviews focused on children with CHD found that low parental education is associated with higher infant mortality, less access to care, increased risk of loss to follow up cardiology care, hospital re-admission, neurodevelopmental problems, and lower quality of life.Reference Best, Vieira, Glinianaia and Rankin29,Reference Davey, Sinha, Lee, Gauthier and Flores30 Caregiver education may also impact health-related knowledge, literacy, and problem-solving skills.Reference Peyvandi, Baer and Moon-Grady31 Caregivers with limited English proficiency may also face additional barriers navigating the healthcare system and accessing quality care.Reference Eneriz-Wiemer, Sanders, Barr and Mendoza32,Reference Gulati and Hur33 Similarly, in this analysis, compared to non-Hispanic White children we found Hispanic children living in primarily non-English speaking households were more likely not to have had a preventive or specialty care visit in the past 12 months.
Additionally, the current study found larger percentages of caregivers of non-Hispanic Black and Hispanic children were unemployed, compared to non-Hispanic White children. Many studies have examined income or federal poverty status, rather than employment, finding racial/ethnic disparities in these measures of monetary resources. They further found associations between monetary resources and poor outcomes related to fetal diagnosis of CHD, CHD prevalence and incidence, infant mortality, post-surgical outcomes, access to care, loss to follow up, and hospital readmission among children with CHD.Reference Davey, Sinha, Lee, Gauthier and Flores30 In this study, we measured socio-economic status through consistency of employment, which is correlated with monetary resources, but also has implications for the child’s health insurance.
We found additional racial and ethnic disparities among children with heart conditions in healthcare access and utilisation, specifically, differences in health insurance and having a usual place of care. Among children with heart conditions, we found approximately half to two-thirds of non-Hispanic Black and Hispanic children only had public, other, or no health insurance and a quarter to a third of non-Hispanic Black and Hispanic children had no usual place of care, approximately twice that of non-Hispanic White children. Our finding is consistent with previous studies showing greater prevalence of public, Medicaid, or no insurance among non-White children compared to White children with CHD.Reference Jackson, Morack, Harris, DeSalvo, Daniels and Chisolm9,Reference Kucik, Cassell and Alverson28,Reference Peyvandi, Baer and Moon-Grady31,Reference Peterson, Catton and Setty34 While public insurance provides healthcare access to children of lower income families and those with special healthcare needs, previous studies have found poorer outcomes among children with public insurance, such as lapses in cardiac care, hospital admission, mortality, number of emergency visits, and in hospital admission or mortality during an emergency room visit.Reference Best, Vieira, Glinianaia and Rankin29,Reference Davey, Sinha, Lee, Gauthier and Flores30,Reference Edelson, Rossano and Griffis35,Reference Skinner and Mayer36 A study of 420,452 paediatric CHD-related emergency department visits, using 2006–2014 data from the nationwide emergency department sample, found two-thirds of CHD-related emergency department visits had government insurance as a primary payer, and that government insurance was a risk factor for inpatient hospital admission.Reference Edelson, Rossano and Griffis35 Racial and ethnic disparities have also been observed in emergency department visits among children with Kawasaki disease,Reference Lo, Gauvreau and Baker37 in mortality among children with cardiomyopathy and myocarditis,Reference Olsen, Tjoeng, Friedland-Little and Chan38 and in treatmentReference Sooy-Mossey, Neufeld and Hughes39 and infant mortalityReference Well, Fenrich and Shmorhun40 among infants with arrhythmias. Additionally, children with heart conditions of Hispanic ethnicity may be less likely than their non-Hispanic White counterparts to have a medical home,Reference Broughton, Riehle-Colarusso, Nehl, Riser and Farr10 and non-White children with CHD fall out of cardiac care earlier than White children.Reference Jackson, Morack, Harris, DeSalvo, Daniels and Chisolm9
Several studies have found associations between race/ethnicity and poor outcomes,Reference Jackson, Morack, Harris, DeSalvo, Daniels and Chisolm9,Reference Broughton, Riehle-Colarusso, Nehl, Riser and Farr10,Reference Lopez, Morris, Sexson Tejtel, Espaillat and Salemi13,Reference Peterson, Catton and Setty34 and social determinants of health and poor outcomes,Reference Ludomirsky, Bucholz and Newburger20–Reference McClung, Glidewell and Farr22,Reference Best, Vieira, Glinianaia and Rankin29,Reference Davey, Sinha, Lee, Gauthier and Flores30,Reference Edelson, Rossano and Griffis35 yet few studies have examined the role of socio-economic indicators as potential mediators of the relationship between race/ethnicity and outcomes among children with CHD.Reference Kucik, Cassell and Alverson28,Reference Peyvandi, Baer and Moon-Grady31 One such study found insurance status and maternal education mediated a quarter to a third of the relationship between Hispanic ethnicity and composite risk of mortality or unexpected hospital re-admissions in the first year of life.Reference Peyvandi, Baer and Moon-Grady31 Among children whose caregivers were employed or who had greater than a high school education, we found associations with ≥2 emergency room visits for Hispanic children strengthened and for non-Hispanic Black children attenuated slightly. While the current study shows associations between race/ethnicity and upstream social determinants of health, further research is needed to untangle the relationship between race/ethnicity, social determinants of health including insurance type and education, and poor outcomes.
The strengths of this analysis are in our use of a nationally representative data source and the large sample size of children with heart conditions. Yet, this study has some limitations. Of note, the National Survey of Children’s Health is caregiver-reported and not otherwise validated. No information is available on what type of heart condition a child may have. Based on a CHD birth prevalence of about 1% Reference Reller, Strickland, Riehle-Colarusso, Mahle and Correa41 and given the 2.2% of children in our data have ever had a heart condition, less than half of children with heart problems in our sample may have CHD. Additionally, we were unable to examine other racial/ethnic groups or multiracial individuals due to low sample size within strata, and heterogeneity in results between these racial/ethnic groups prohibited their grouping. Compared to children included in this study, children missing data were more likely to have caregivers with a high school education or less and less likely to have problems paying for care, which may limit the generalizability of our findings. Our measures for educational attainment and employment status were defined as a composite score of one or more caregivers. Thus, non-Hispanic Black children who are more likely to have one caregiver, rather than two, are necessarily more likely to have a higher percentage of caregivers not employed.Reference Peterson, Catton and Setty34 We were unable to distinguish between preventative primary care and preventative cardiology care in these data. Thus, for children with heart conditions, the prevalence of preventative care may be overestimated. The survey also does not specify the type of specialty care received. Finally, we could not link the upstream social determinants of health we examined to poor outcomes in these data.
Racial and ethnic disparities in social determinants of health, such as socio-economic status and healthcare access, are rooted in structural racismReference Churchwell, Elkind and Benjamin4; therefore, to achieve health equity in CHD, experts in the field have proposed interventions at the individual and population levels, such as diversifying the CHD workforce and implementing policies for lifelong insurance.Reference Lopez, Baker-Smith and Flores42 Additionally, interventions at the clinic and community level studied among other patient populations may have the potential to reduce these disparities. One such intervention is using parent mentors who themselves have children with CHD to facilitate and enhance communication between providers and families of children with CHD,Reference Davey, Sinha, Lee, Gauthier and Flores30 which has been shown to improve outcomes among children with asthmaReference Flores, Bridon and Torres43 and improve insurance rates, healthcare access, and parental satisfaction among uninsured children.Reference Flores, Lin and Walker44 Other researchers have emphasised screening for social determinants of health at all healthcare visits, including specialty healthcare visits,Reference Lopez, Baker-Smith and Flores42 and utilising team-based care, including social workers to assist with barriers to care such as transportation and food insecurity.Reference Arthur, Lucenko, Sharkova, Xing and Mangione-Smith45 Additionally, flags within medical records to identify children facing social complexities (e.g. parent or child mental illness, parent death, parent domestic violence, etc.) could help ensure they receive extra supports as needed.Reference Arthur, Lucenko, Sharkova, Xing and Mangione-Smith45 Other researchers have suggested utilising medical interpreters for families of children with limited English language proficiency and providing community-based visitation programmes for new and pregnant mothers to ensure timely diagnosis of CHD and earlier treatment.Reference Peterson, Catton and Setty34
In this analysis, we found barriers to care for children with heart conditions and racial/ethnic disparities in social determinants of health, such as socio-economic status and healthcare access and utilisation, among children with heart conditions. There is a need to identify families of children with CHD with unmet social or financial needs and to ensure equitable access to care for these children.46–Reference Parker, Garg and Brochier49 More understanding on ways in which social determinants of health, such as those examined in this analysis, modify the associations between race/ethnicity and poor outcomes may be beneficial. Additionally, further evaluation and implementation of successful strategies to improve social determinants of health may help decrease racial/ethnic disparities among children with heart conditions.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1047951122004097
Acknowledgements
This analysis was replicated by Brittany Wright.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.






