A 2-day-old male was admitted to the emergency room with signs of cardiogenic shock. Initial echocardiogram diagnosed a type B interrupted aortic arch, ventricular septal defect, atrial septal defect, and patent ductus arteriosus, pre-surgical CT or MRI was not performed. At 10 days of age, as haemodynamic conditions improved, at the surgery, the ductal tissue was resected, and a longitudinal incision was made in the distal part of the aorta, the anastomosis of the descending aorta was performed using an aortic advancement technique, and the left subclavian artery was ligated and sectioned with closure of septal defects. The surgical note described a left aortic arch with the interruption after the origin of the left common carotid artery and left subclavian artery originating from the descending thoracic aorta. Intra-operative echocardiogram reported a small residual ventricular septal defect, mild tricuspid regurgitation, moderate pulmonary regurgitation, and aortic arch without obstruction.
During his stay in the cardiovascular ICU healthcare-associated pneumonia was diagnosed by radiography and respiratory deterioration; however, the patient never presented fever or systemic inflammatory response indicators.
All laboratory results and cultures were reported as normal. The patient was successfully extubated on the fifth day post-surgery, and 16 days after that he was discharged from the cardiovascular care unit to the neonatal ICU; in this period, the patient was diagnosed with atrial tachycardia, and the FISH study confirmed 22q11.2 microdeletion syndrome. Twenty days after surgery, he was discharged from the hospital.
He gradually improved, and a post-surgical echocardiogram at 60 days of age showed an image suggestive of pseudoaneurysm in the ascending aorta. After performing a cardiac CT (Fig. 1) and MRI (Figs. 2 and 3), a giant aneurysm at the site of surgical anastomosis was diagnosed extending towards the ascending and descending aorta. It was considered that the possible origin of the lesion could be due to an alteration in the collagen of the vessel wall or surgical issues during the anastomosis that led to aortic wall degeneration and aneurysmal dilation.Reference Ghosh 1 The patient presented rapid neurological deterioration requiring orotracheal intubation secondary to a cerebrovascular ischaemic event with lesions in the right frontal and temporal lobes. Subsequently, the patient continued with progressive clinical deterioration and died at 2 months 28 days of life. No post-mortem study was performed.

Figure 1. Cardiac CT 60 days after aortic arch advancement surgery. Double-oblique coronal and sagittal views of the aortic root, showing a giant aneurysm extending from the ascending aorta to the aortic isthmus.

Figure 2. Cardiac MRI cine images in left ventricle three-chamber view and double-oblique sagittal view showing true aneurysm of the aortic arch sparing the descending thoracic aorta.
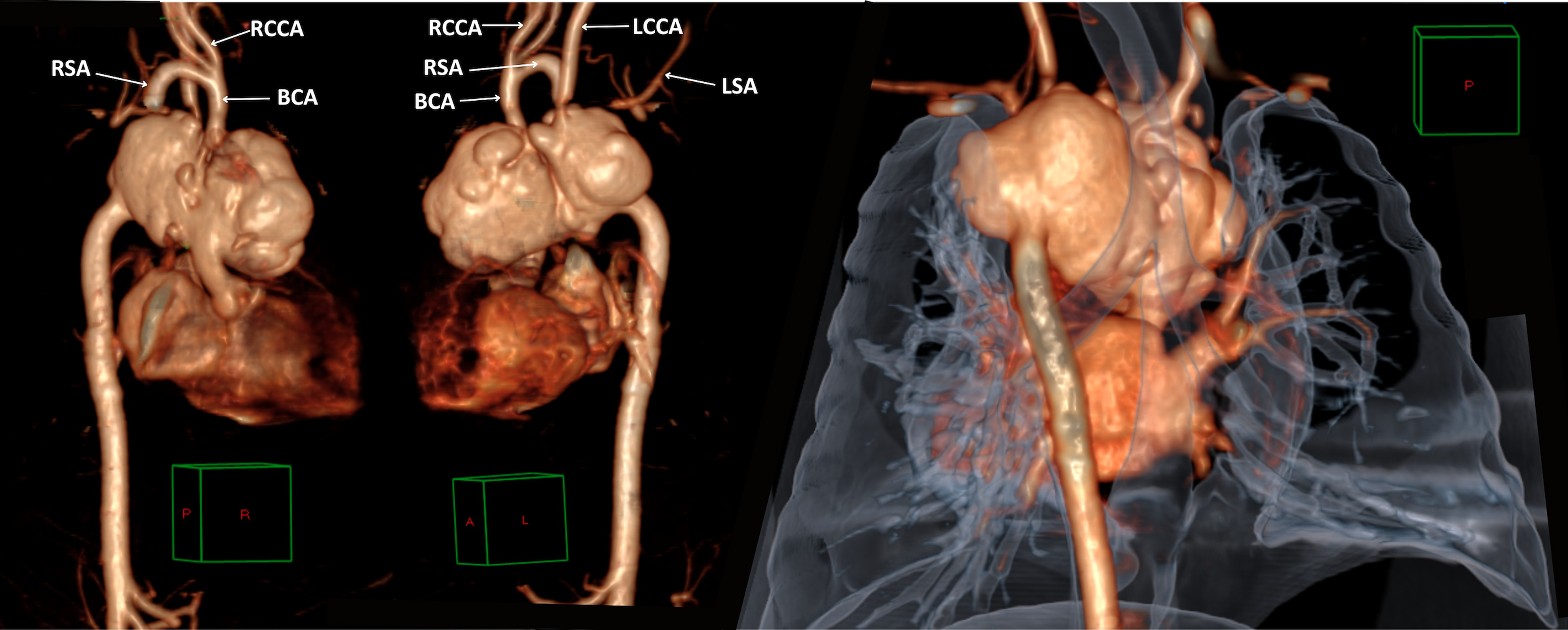
Figure 3. 3D volume-rendering reconstruction images in anterior and posterior views showing giant aortic aneurysm with right tracheal deviation, and the left subclavian artery was surgically ligated. BCA = brachiocephalic artery; RCCA/ LCCA = right/left common carotid artery; RSA/LSA = right/left subclavian artery.
Acknowledgements
None.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Competing interests
None.






