BACKGROUND
Post-event debriefing, recommended by the American Heart Association (AHA),Reference Bhanji, Donoghue and Wolff 1 provides an opportunity for the team to reflect and learn from their performance. We define post-event debriefing as facilitated inter-professional team reflection after a clinical event that focuses on improving both system and team performance. Despite guidelines on how to implement a clinical debriefing programReference Kessler, Cheng and Mullan 2 , Reference Sawyer, Loren and Halamek 3 and evidence that debriefing is associated with improved patient care,Reference Wolfe, Zebuhr and Topjian 4 published literature suggests that debriefing is rare after critical emergency department (ED) events and resuscitations.Reference Theophilos, Magyar and Babl 5
Time constraints, unrelenting care demands, and lack of available, appropriately trained facilitators are barriers to a consistent clinical debriefing.Reference Sandhu, Eppich and Mikrogianakis 6 Data suggest that physicians facilitate 70% to 90% of real-event debriefings,Reference Theophilos, Magyar and Babl 5 - Reference Mullan, Wuestner and Kerr 8 but ED care demands impact physician availability. Although able to participate in a short debriefing as a team member, the physician’s ability to regularly facilitate debriefings may be impacted by the extra time needed to coordinate a debriefing. This compromises the feasibility and sustainability of physician-led debriefing programs. To address this issue, we explored the use of charge nurses as the designated group responsible for facilitating clinical debriefings.
PURPOSE
The purpose of this project was to develop a feasible and sustainable charge–nurse-facilitated clinical debriefing program across Calgary area adult EDs.
Before the INFO process was implemented, no specific group was responsible for facilitating debriefings in Calgary EDs. When debriefings did occur, they were facilitated by the physician team leader; however, time pressures and the invariable backlog of waiting patients limited physician ability to facilitate debriefings.
We recognized that ED charge nurses have clinical knowledge, operational awareness, and an understanding of team roles and expertise within their departments. They usually observe resuscitations but are not allocated a specific role, so are more situationally aware and ideally suited to facilitate post-event debriefings. When resuscitations end, ED nurses and physicians normally return immediately to other patient care responsibilities and become immersed in clinical work, but charge nurses do not have specific patient assignments, allowing them to prioritize the clinical debriefing process.
The Calgary ED charge nurse group expressed a willingness to take on responsibility for clinical debriefing in the ED, and agreed that facilitating INFO sessions was within their scope of practice. Designating this to our charge nurses allowed us to focus training on a small, specific group who then assumed an ongoing oversight of the debriefing process.
DESCRIPTION OF THE INNOVATION
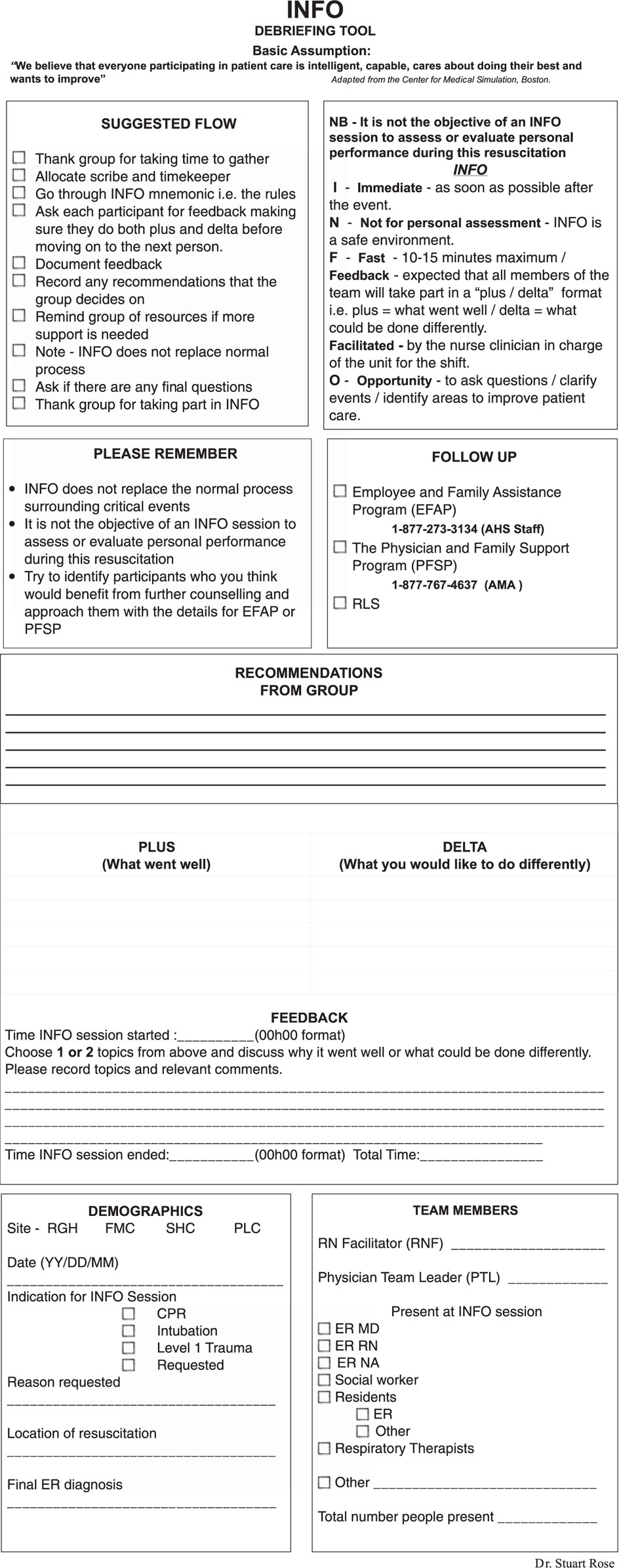
Based on successful principles in healthcare and other industries,Reference Tannenbaum and Cerasoli 9 we developed a clinical debriefing intervention called INFO (immediate, not for personal assessment, fast facilitated feedback, and opportunity to ask questions). INFO implementation was a stepwise process. Firstly, a debriefing tool was developed to specifically support the novice debriefer (Figure 1). AHA guidelines provide examples of several debriefing tools.Reference Association 10 These tools and, in particular, the DISCERN tool, were referenced in developing a draft version of the tool.Reference Mullan, Wuestner and Kerr 8 , Reference Association 10 Modifications included the provision of a structured suggested format, the use of a pre-briefing script, and setting the climate for the debriefing by establishing psychological safety. Scripted statements were used to make the debriefing tool more supportive for the novice and encourage a safe environment for debriefing.
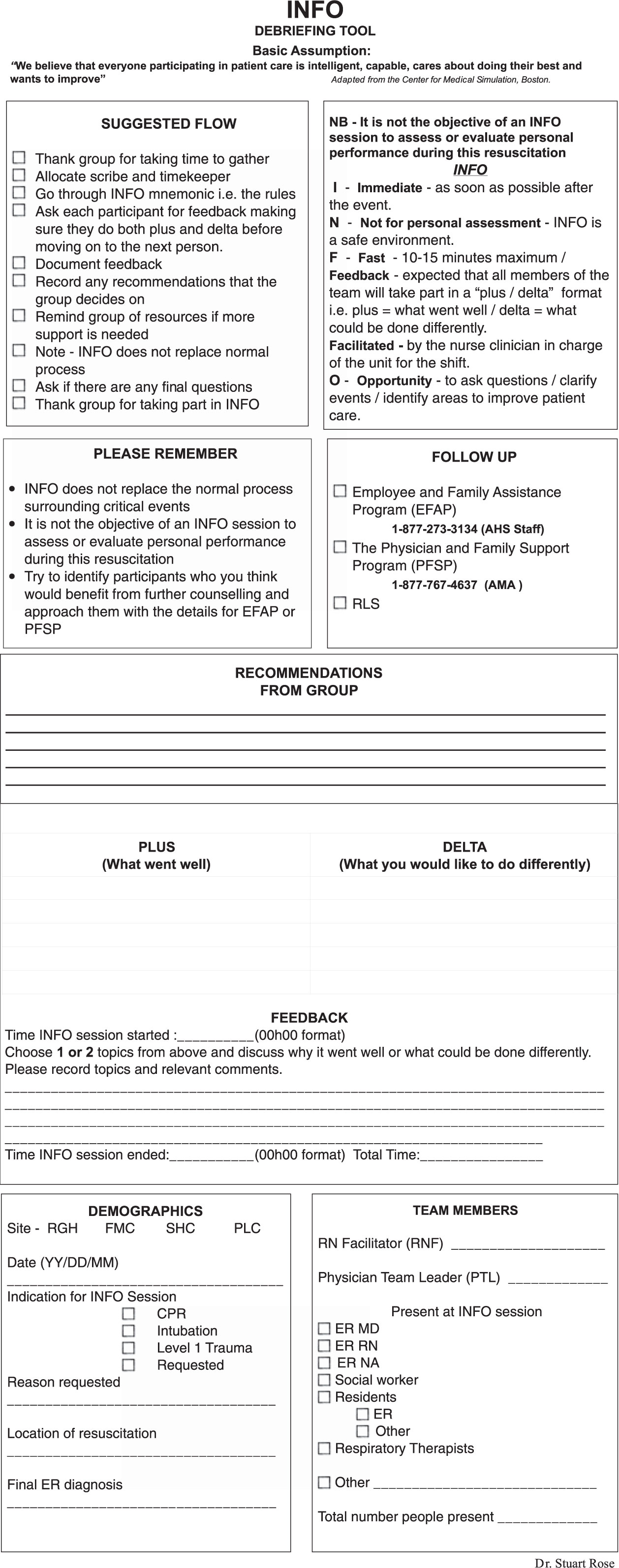
Figure 1 INFO clinical debriefing tool.
The second step was achieving inter-professional engagement and support, which involved a front-end needs assessment, engagement of key stakeholder groups (especially physicians and nurses), encouragement of their involvement in tool development, incorporation of their feedback as appropriate, and the identification of physician and nursing champions.
The third step was a 4-hour “Teach the Teacher” (T3) workshop aimed at the nursing champion and nurse educators. T3 graduates assumed the role of faculty for teaching the INFO Basics workshop, which allowed us to train our charge nurse groups and build facilitator training capacity.
In the fourth step, the 2-hour INFO Basics workshop focused on the INFO tool and provided feedback on the charge nurses’ performances in simulated INFO debriefings. After the completion of this workshop, the ED staff are approved to conduct debriefings.
As soon as INFO was rolled out in the ED, a regular discussion was held with the INFO charge nurses, nurses, physicians, and other staff members to assess the impact of the debriefing process. Addressing participant recommendations for improvement was important to promote investment in future INFO debriefings and in addressing patient care and potential safety issues.
Now operating as a voluntary process initiated by on-duty staff, 254 inter-professional ED INFO clinical debriefing sessions have taken place from March 2016 to September 2017. Sessions have a median duration of 10 minutes and have involved over 1,300 staff. Recommendations arising from the INFO sessions have been implemented into clinical practice (Table 1).
Table 1 Changes to clinical practice as suggested by completed INFO debriefings

CPR=cardiopulmonary resuscitation; EMS=emergency medical services; HSCE = high stakes clinical events; PPE=personal protective equipment.
DISCUSSION
The INFO clinical debriefing process described here is novel and adds to current literature on clinical debriefing in two important ways. Firstly, INFO addresses one of the most common barriers to regular debriefing – a lack of skilled facilitatorsReference Sandhu, Eppich and Mikrogianakis 6 – and it has proven to be a simple and effective way of building debriefing capacity in our departments. Further, it reduces the focus on physician-led debriefing and shifts leadership accountability to other team members, providing leadership opportunity for non-physicians and validating the concept of a team approach to patient care and quality improvement. Any member of the team can request an INFO debriefing, but designating responsibility to the identifiable charge nurse group has led to regular clinical debriefings in Calgary EDs. Using a structured debriefing process promotes the culture of teamwork and feedback that has resulted in various recommendations for change to clinical practice across Calgary area adult EDs.
SUMMARY
The INFO clinical debriefing process addresses two significant barriers to regular ED clinical debriefing: a lack of trained facilitators and the focus on physician-led debriefing. Our experience shows that a charge–nurse-facilitated debriefing is feasible, can be successfully implemented in diverse EDs, and can be performed by relatively inexperienced debriefers. A structured approach has resulted in regular debriefings, which have become a routine part of improving team management of high stakes or unexpected clinical events in Calgary EDs.
Acknowledgements: We thank Dr. Grant Innes and Dr. Andrew McRae for their contributions in editing and revising this paper. We also thank the many people who have made suggestions and given feedback on the INFO process. In particular, we acknowledge the contributions of Dr. Aaron Johnston and Dr. Vince Grant in improving the INFO process.
Competing interests: None declared.