Introduction
Tourette syndrome (TS) is a childhood-onset neurodevelopmental disorder characterized by the presence of motor and phonic tics.Reference Jankovic 1 TS is the most common cause of chronic tics. A 2007 National Survey of Children’s Health estimated a prevalence of 3.0 per 1000 among children aged 6 to 17 years in the U.S. 2 Pooled data from epidemiological studies estimated that between 4 and 8 per 1000 school-age children have TS.Reference Scahill, Specht and Page 3 In a systematic review and meta-analysis of 21 population-based prevalence studies, the pooled TS population prevalence estimate was 0.52%.Reference Scharf, Miller, Gauvin, Alabiso, Mathews and Ben-Shlomo 4 These studies consistently show a higher prevalence of TS in males with a 3-4:1 ratio compared to females. Tics have a typical age at onset between 4 and 8 years and show increased frequency and severity until age 10 to 12 when a peak in tic severity is observed; this period is typically followed by a decline in tic severity during adolescence and adulthood.Reference Groth 5 However, how this occurs in boys and girls has been largely unexplored. A recent European multicenter study revealed a sex dimorphism in patients with TS, with males showing more severe symptoms than females during the early years within TS evolution; however, females had a progressively greater symptom severity with aging compared with males.Reference Garcia-Delgar, Servera and Coffey 6 There is less information on sex differences in patients with chronic motor/vocal tic disorderReference Scahill, Specht and Page 3; if symptom severity progresses more in females, a larger proportion of these patients may eventually fulfill the diagnosis of TS compared with their male counterparts. Sex differences in gray and white matter volume, as well as brain connectivity, have been demonstrated with anatomical and functional neuroimaging studies in patients with TS.Reference Robertson, Eapen and Singer 7 Notwithstanding these sex biases, there are still few studies focusing on the clinical dimorphism of TS between sexes.
Patients with TS frequently present with comorbid neuropsychiatry conditions with a lifetime prevalence of 85.7%.Reference Hirschtritt, Lee and Pauls 8 Among comorbid neuropsychiatric conditions, attention-deficit/hyperactivity disorder (ADHD) and obsessive–compulsive disorder (OCD) are the most frequently recognized.Reference Hirschtritt, Lee and Pauls 8 Comorbid disorders are important to be recognized as they influence overall presentation of TS.Reference Santangelo, Pauls, Goldstein, Faraone, Tsuang and Leckman 9 -Reference Huisman-van Dijk, Matthijssen, Stockmann, Fritz and Cath 12 Despite this high prevalence, there is a dearth of information about sex dimorphism in the frequency of comorbid ADHD and OCD in males and females with TS. Recent multicenter studies have shown that males with TS have a higher prevalence of comorbid ADHD, oppositional defiant or conduct disorders, whereas females have a higher prevalence of OCD, anxiety and eating disorders.Reference Garcia-Delgar, Servera and Coffey 6 , Reference Hirschtritt, Lee and Pauls 8
In this study, we aimed to compare the frequency, phenomenology, body distribution, complexity, and severity of tics in males and females with TS of various ages. Additionally, we explored the frequency of ADHD and OCD in patients with both sexes with TS. We hypothesize that there is a clinical dimorphism between males and females with TS. Identifying such differences may be helpful to predict evolution and detect comorbidities earlier in these patients. We use the term “sex” rather than “gender” according to the American Institute of Medicine recommendation as previously reviewedReference Meoni, Macerollo and Moro 13 , Reference Baizabal-Carvallo and Jankovic 14 despite prior reports, including ours, using the term “gender.”Reference Baizabal-Carvallo and Jankovic 14
Patients and Methods
We performed a detailed analysis of video recordings and clinical records of consecutive patients diagnosed with TS. We included patients with TS and persistent (or chronic) motor/vocal tic disorder diagnosed and evaluated by movement disorders experts in a tertiary care referral center, at the Department of Neurology of Baylor College of Medicine in Houston, Texas. We used the clinical criteria according to the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5). 15 We excluded patients considered to have secondary tic disorders related to cranial trauma, stroke, toxins (ie, carbon monoxide), infectious (ie, encephalitis), para-infectious (Sydenham disease), and inherited disorders (ie, Huntington disease, tuberous sclerosis, Wilson’s disease) or drug-induced tics. Patients with tics having an evolution shorter than 12 consecutive months (ie, provisional tic disorder, according to DSM-5) were included if no secondary or a drug-induced cause was identified. Emerging evidence supports the notion that chronic and provisional tic disorders are part of the TS spectrum and the latter rarely transitory.Reference Kim, Greene and Bihun 16 , Reference Claudio-Campos, Stevens and Koo 17 We eliminated patients with incomplete clinical information, unclear diagnosis, or those who withdrew consent.
We classified tics according to the complexity and distribution of the movements. Simple motor tics were defined as contractions involving one group of muscles, causing brief, jerk-like movements.Reference Jankovic 1 Complex motor tics were defined as more coordinated sequence of movements, including copropraxia. Simple phonic tics were considered in case of emission of basic, nonmeaningful noises such as sniffing, grunting, squeaking, throat-clearing, sucking, coughing, or burping sounds; whereas complex motor tics included linguistically meaningful utterances and verbalizations, including coprolalia, echolalia (repetition of someone else words or phrases) and palilalia (repetition of one’s own words or phrases).Reference Jankovic and Kurlan 18 Tic severity was determined by blinded assessments of video recordings to the evaluation at the clinic. Tic severity was based on the Global Severity Ratings and Rush Video-Based Tic Rating Scale, as described previously.Reference Goetz, Pappert, Louis, Raman and Leurgans 19 , Reference Sambrani, Jakubovski and Müller-Vahl 20 We considered the following categories, 0: None; 1: very mild (tics rarely observed on video); 2: mild (tics are noticeable but not disruptive); 3: medium (tics are frequent but mildly disruptive); 4: marked (tics are frequent and moderately disruptive); 5: severe (tics are very frequent and moderately disruptive); and 6: very severe (tics are very frequent and extremely disruptive). As tics have a waxing and waning course, and not all tics may be present at the time of examination, we also assessed retrospectively the severity of tics by reviewing the patient’s clinical history. Accordingly, patients were divided into three categories: (a) mild: tics are focalized or infrequent causing minor or no disruption at work, school, or daily living activities; (b) moderate: tics are frequent and extensively distributed causing some disruption at work, school or daily living activities; and (c) severe: tics are frequent causing severe disruption at work, school or daily living activities. Additionally, we identified the number of different phonic tics per patient on video recordings.
We assessed the frequency of comorbid ADHD and OCD according to the DSM-5 criteria. 15 The diagnosis of ADHD was based on the presence of either disruptive inattention and/or disruptive hyperactivity/impulsivity for at least 6 months. Whereas the presence of time-consuming, distressful, obsessions, compulsions, or both was consistent with OCD. 15 Diagnoses were carried out during clinical encounters and retrospectively obtained from medical charts. Patients provided signed written informed consent, approved by the Baylor College of Medicine Institutional Review Board for Human Research for videotaping and publishing in a scientific journal.
Statistics
We summarized data in means ± standard deviations and percentages. The nonparametric, Mann Whitney U test was used to compare means between males and females. The chi-square (χ 2) test or Fisher’s exact test, along with odds ratios (OR) and confidence intervals (CI) at 95% were used to compare proportions between sexes. All statistical evaluations were performed using SPSS version 22, a P-value < .05 was considered significant. For the purpose of analysis, we stratified patients into two age groups: patients younger than 18-years of age: “young” group; and patients 18-years-old or older: “old” group. This threshold was chosen as TS usually shows a peak of severity before age 18.Reference Groth 5 We used a multiple logistic regression, using a conditional backwards method to assess the effect of statistically significant independent variables on the dependent variable: “sex.” Variables statistically significant or with a statistical trend for significance (P < .10) were included for entering as independent variables in the binary multivariate regression. Variables with P ≥ .10 were eliminated from the final model. The Hosmer–Lemeshow test was used to assess the goodness of fit for the logistic regression model, a P-value < .05 was considered poor fit. We assessed for statistical interactions between significant independent variables in the general multivariate model.
Results
We studied 213 patients presenting for evaluation of a tic disorder. Twelve patients were excluded or eliminated from the study (Figure 1). A total of 201 patients were included in the analysis.

Figure 1. Cohort attrition.
There were 156 males (77.6%) and 45 females (22.4%), M:F ratio: 3.5:1. When assessing the whole cohort, no differences were observed in age at onset, age at evaluation; frequency, distribution, and complexity of tic phenomenology and the severity of the tic disorder between sexes. However, male patients had a higher frequency of ADHD (OR: 3.07, C.I. 95%: 1.42-6.65; P = .003); male patients also showed a statistical trend for higher frequency of eye rolling tics (P = .098) (Table 1).
Table 1. Summary of Sex Differences in All Patients with Tourette syndrome
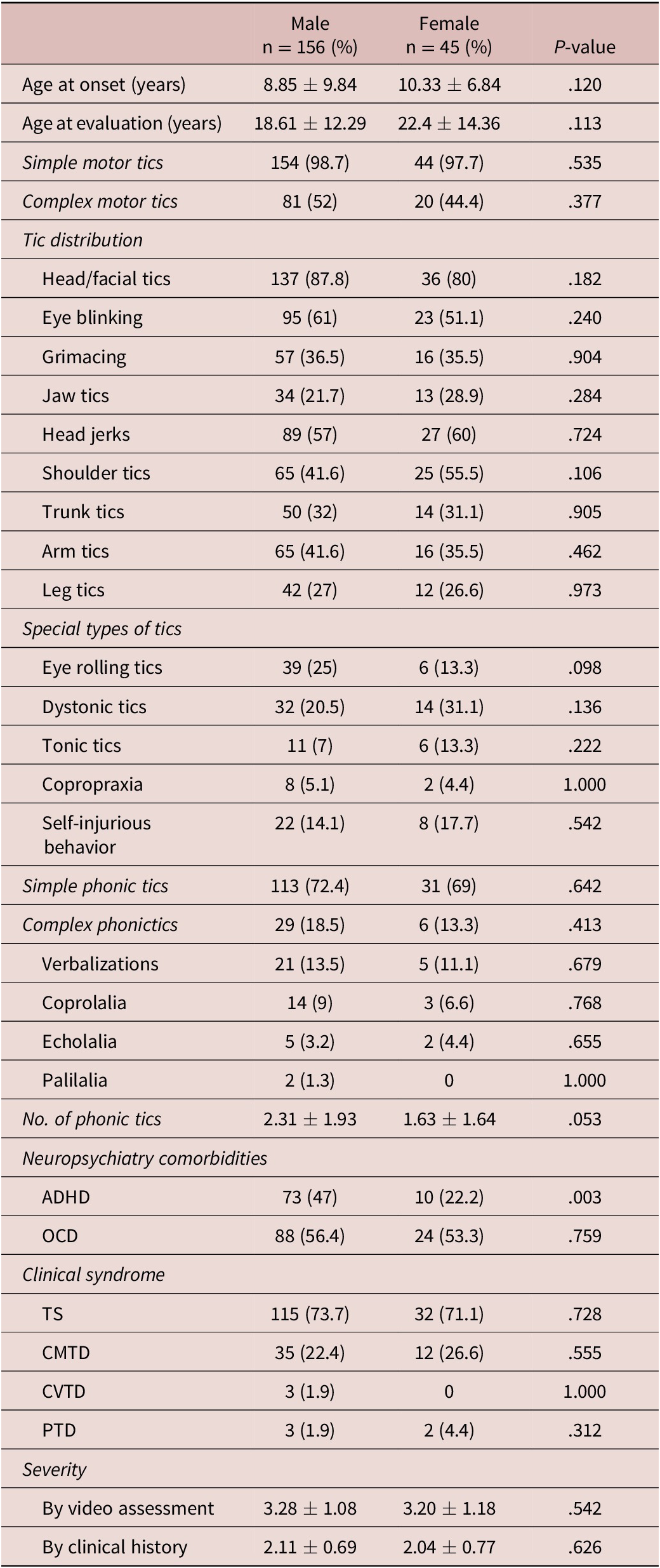
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; CMTD, chronic motor tic disorder; CVTD, chronic vocal tic disorder; OCD, obsessive–compulsive disorder; PTD, provisional tic disorder; TS, Tourette syndrome.
When assessing patients younger than 18-years old, “young” age group (total: n = 118, males, n = 95, females, n = 23). Males showed a higher frequency of eye-blinking (OR: 3.36, C.I. 95%: 1.29-8.74, P = .010) and complex motor tics (OR: 3.42, C.I. 95%: 1.24-9.45; P = .014) than females (Figure 2); with a statistical trend for a higher frequency of eye-rolling tics in males (OR 3.95, C.I. 95%: 0.86-18.1, P = .059) compared with females. Males also seemed to have a younger age at onset than females 5.9 vs 7.5 years (P = .083) and still showed a higher frequency of ADHD in this “young” age group (OR 4.95, C.I. 95%: 1.69-14.4, P = .003) (Table 2). Variables from the “young” group fulfilling the criteria in the bivariate analysis were entered in the multivariate logistic regression analysis. The following variables were included in the final equation: complex tics (exp B = 3.312, C.I. 95%: 1.05-10.99, P = .049), ADHD (exp B = −4.11, C.I. 95%: 1.18-14.25, P = .026) and age at onset (exp B = 1.18, C.I. 95%: 0.98-1.42, P = .072). No interactions were observed between complex tics and ADHD (P = .406), age at onset and ADHD (P = .651) or complex tics and age at onset (P = .829). Moreover, we did not find interactions between OCD and complex motor tics (P = .634). The regression model showed an appropriate goodness of fit (P = .696).
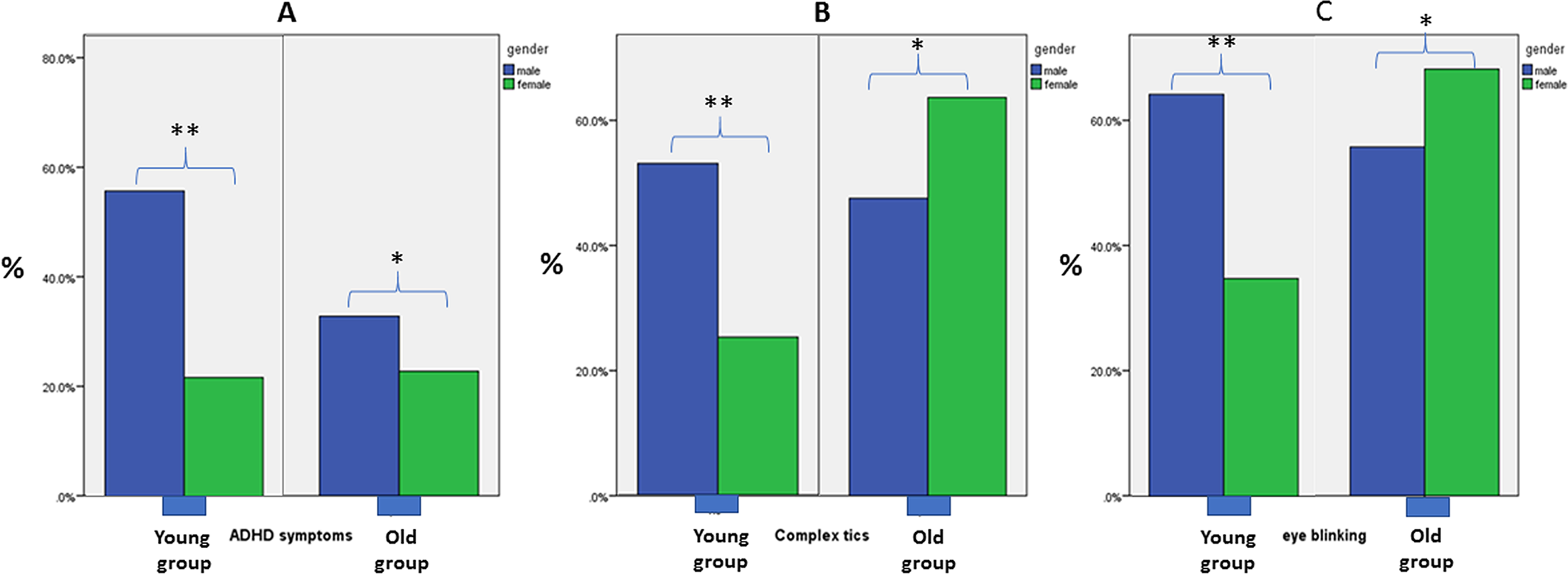
Figure 2. (A) Frequency of attention-deficit/hyperactivity disorder (ADHD), (B) complex motor tics, and (C) eye-blinking tics in males and females considering the “young” and “old” groups. **P < .05; * P nonsignificant.
Table 2. Summary of Sex Differences in Patients with Tourette syndrome in Patients < 18 Years-Old, “Younger Group”
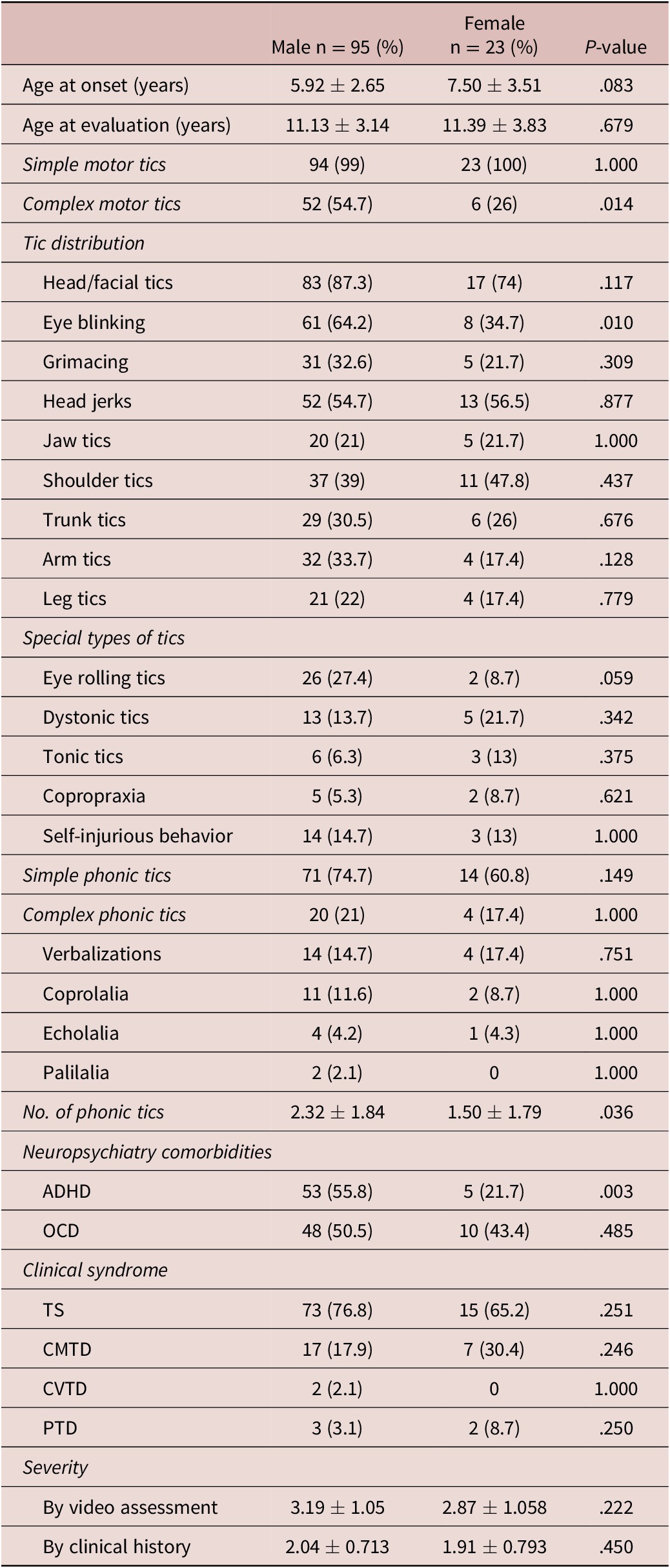
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; CMTD, chronic motor tic disorder; CVTD, chronic vocal tic disorder; OCD, obsessive–compulsive disorder; PTD, provisional tic disorder; TS, Tourette syndrome.
Patients aged 18-years or older, were underrepresented (total: n = 83, males, n = 61, females, n = 22) compared to “young” patients. We did not observe sex differences in clinical, comorbid and demographic variables in this group (Supplementary Table S1). Variables such as frequency of ADHD, complex motor tics and eye blinking, showing a statistical difference in the young group, were no longer significant when comparing sexes in the old group (Figure 2). These effects were related to a decrease in ADHD frequency in males and an increase in the frequency of complex and eye-blinking tics in females in the old group (Figure 2). Multivariate analysis was not conducted for this age group, as no variable had a statistically significant result.
Intrasex comparison of groups showed that females older than 18 years had a higher frequency of complex motor tics (P = .011), eye blinking (P = .025), grimacing (P = .048), and arm tics (P = .009) with a trend for higher severity by video assessment (P = .078) than their young counterparts (Supplementary Table S2). Whereas males had a decrease in the proportion of patients with ADHD (P = .005) but an increase in dystonic (P = .008) and arm tics (P = .012) (Supplementary Table S3).
Discussion
In this study, we compared the clinical profile of male and female patients with TS. Except for ADHD and the number of phonic tics, the age at onset and clinical presentation were similar between sexes when considering the entire cohort. However, after stratification by age at examination, differences were observed in the younger group of patients. Some tics were more common in male patients younger than 18 years of age, such as eye-blinking, and complex motor tics, but these differences were lost in older patients, suggesting that either such manifestations predominate in male children and teenagers overall or they appear earlier in male patients. The latter hypothesis is suggested by the observation that the percentage of eye-blinking in female patients increased from 34.7% to 68.2% and complex motor tics increased from 26% to 63.6%, when comparing patients in the “young” vs the “old” group (Figure 2); while those frequencies remained relatively stable in males (Table 2 and Supplementary Material). The increased percentage in the frequency of complex tics would be expected to result in a higher severity of TS in older female patients. This, indeed, was observed in our study, as the tic severity increased from 2.87 to 3.55 in females when comparing the “young” vs the “old” groups. Our study also suggests that male patients with TS younger than 18 years have more conspicuous pattern of tics compared with females, as they show complex motor tics more frequently: 54.7% vs 26% (P = .014), respectively. However, after 18 years of age, females showed a visible increase in the frequency of complex motor tics (63.6%). Similar observations were made in another study where a greater likelihood of tic worsening, tic severity, and expansion of body tic distribution was observed during adulthood in female patients with TS.Reference Martino, Cavanna, Robertson and Orth 21 Moreover, a European multicenter study including 709 patients with TS (23.3% females) reported similar findings.Reference Garcia-Delgar, Servera and Coffey 6 This study also found that male participants ≤12 years had greater compulsions than females, but a rise in compulsions was observed in females with aging.Reference Garcia-Delgar, Servera and Coffey 6 Moreover, compulsions were more strongly correlated with ADHD symptoms in males than in females in young patients with TS in another study.Reference Schulte, Hawelka and Pletzer 22 This observation fits into the picture of more common complex motor tics in young males with TS. Compulsions and complex motor tics have been considered within the same phenomenology spectrum.Reference Wolff, Luehr and Sender 23
In summary, evidence suggests that males with TS present with greater complexity and severity of tics during childhood and adolescence; however, females show increased tic complexity and severity with aging. It is unclear whether this occurs in patients with chronic motor tics only; however, as phonic tics can be viewed as motor tics that involve the nasal, laryngeal or respiratory muscles, it is likely that these patients evolve similarly.
We also found a higher frequency of number of phonic tics per patient in males from the young group (P = .036). This difference was lost in the “old” group. Although we did not find differences in complex tics, another study showed a higher frequency of coprolalia, palilalia in males, consistent with other clinical reports.Reference Sambrani, Jakubovski and Müller-Vahl 20 Further studies should also clarify whether differences in severity and clinical course of phonic tics exist between sexes.
A previous study showed that the diagnosis of TS is made at later age in females than males.Reference Santangelo, Pauls, Goldstein, Faraone, Tsuang and Leckman 9 In our study, the age at onset and age at presentation was overall similar between sexes; however, a trend for a younger age at onset in male patients was observed in the “young” group: 5.92 vs 7.5 years (P = .083). A younger age at onset in males may contribute to the earlier appearance in life of some types of tics, such as complex tics. However, it is unclear whether eye-blinking or complex motor tics have an earlier appearance related to the onset of motor tics, as we did not record the age at onset of all types of tics, a task with frequent recall bias. We report a frequency of eye movement tics ranging from 50% to 61%, contrasting with another study, which reported a lifetime prevalence of eye movement tics of 78.3%.Reference Martino, Cavanna, Robertson and Orth 24 A difference explained by the assessment method: questionnaires to assess the lifetime prevalence vs video-recording assessment.
A statistical trend for a greater frequency of eyerolling tics in males was observed in the “young” group (P = .059). A sex-related lower ocular fixation capacity in males may potentially contribute to such difference. Recent studies in healthy individuals have shown sex-related differences in eye movements, including shorter ocular fixation in males than females.Reference Mercer Moss, Baddeley and Canagarajah 25 , Reference Schulte, Hawelka and Pletzer 26 Ocular fixation duration has shown an inverse correlation with testosterone levels, particularly in women.Reference Schulte, Hawelka and Pletzer 26 Whether sex-hormones levels can influence ocular fixation and/or increase the probability of ocular deviation is a hypothesis worth testing.
Although disturbance in dopaminergic transmission is a major biochemical abnormality in patients with TS, disturbance of cortico–striato–pallido–thalamic–cortical networks and the relatively unique role of the insula are considered central in the pathophysiology of TS.Reference Wolff, Luehr and Sender 27 , Reference Jackson, Loayza, Crighton, Sigurdsson, Dyke and Jackson 28 Structural dimorphism involving cortical gray and subcortical white matter has been reported between boys and girls with TS.Reference Eliot, Ahmed, Khan and Patel 29 Overall, boys seem to have thinner frontal cortical areas and decreased corpus callosum volume compared with girls.Reference Wolff, Luehr and Sender 27 , Reference Baumgardner, Singer and Denckla 30 -Reference Zimmerman, Abrams, Giuliano, Denckla and Singer 33 Interestingly, patients suffering ADHD without TS have shown thinner corpus callosum in anterior, but more in posterior callosal sections.Reference Luders, Narr and Hamilton 34 It has been hypothesized that a smaller number of corpus callosum fibers may affect interhemispheric communication channels necessary to sustain attention and motor control.Reference Luders, Narr and Hamilton 34 Additionally, adult female patients (mean age about 30 years-old) with TS had increased connectivity between subcortical structures striatum, thalamus, and several cortical areas such as temporal, lateral orbito-frontal, and primary sensory-motor cortices compared to adult males with TS in a single study.Reference Worbe, Marrakchi-Kacem and Lecomte 35 Patients with OCD also seem to have increased connectivity within the executive control network, but decreased within the default and sensorimotor networks.Reference Cui, Ou and Chen 36 It is possible that increased brain connectivity, particularly in the executive network, also relates to complex motor tics, this would fit current clinical and neuroimaging observations. However, how distinct changes in brain connectivity occur between sexes in patients with TS and how they modify with aging should be further clarified.
In this study, male patients showed a higher prevalence of ADHD, particularly in the “young” group. ADHD is a neurodevelopmental disorder with a 3:1 ratio favoring a higher frequency in males, particularly at an early age.Reference Andersen and Teicher 37 , Reference Jankovic, Gelineau-Kattner and Davidson 38 The clinical manifestations of ADHD have been related to decreased function of dopamine and norepinephrine in fronto-striatal circuits.Reference Pinares-Garcia, Stratikopoulos, Zagato, Loke and Lee 39 The dynamic changes in the density of dopaminergic receptors may also play a role in the clinical expression of ADHD; explaining its diverse prevalence at different ages. Studies in animal models have shown that male rats have a higher peak in D2 receptor densities in the central nervous system during adolescence (144 ± 26%) compared with female rats (31 ± 7%). However, about 55% of D2 dopaminergic receptors are eventually down-expressed from the brain of male rats during adulthood, balancing the absolute density of dopamine receptors between sexes.Reference Andersen and Teicher 37 , Reference Andersen, Rutstein, Benzo, Hostetter and Teicher 40 This profile in dopamine receptor densities mirrors what we observed in this study: a higher frequency of ADHD in children and teenage male patients with TS; but no difference in patients 18-years-old or older. Further studies should also focus on defining the type of ADHD in patients with TS: predominantly inattentive, predominantly hyperactive–impulsive and combined, as well as specific comorbidities between sexes with TS.Reference Weiss, Worling and Wasdell 41 , Reference Levy, Hay, Bennett and McStephen 42
The prognosis of TS has been assessed in few prospective studies.Reference Hassan and Cavanna 43 Improvement in tic severity is reported in the majority of patients during adulthood with complete remission occurring in between 10% and 44% of cases.Reference Hassan and Cavanna 43 However, few studies have prospectively assessed whether a sex dimorphism exists in the clinical course and prognosis of TS. One study reported that males have more improvement than females with aging.Reference Burd, Kerbeshian, Barth, Klug, Avery and Benz 44 Although our study is not a prospective one, we found that females in the old group had a trend for greater tic severity than females from the young group; whereas tic severity was similar in males between age groups. Tic severity, premonitory sensations, and family history of TS have been identified as childhood predictors of poorer quality of life in adulthood in patients with TS.Reference Cavanna, David, Orth and Robertson 45 It has also been reported that female sex predicts better response to haloperidol,Reference Garris and Quigg 46 although whether females patients with TS respond differently to medications than males is an important topic that requires further studies.
Our study has limitations. Patients were enrolled from a tertiary care center, and likely represent the higher end within the spectrum severity of TS. Moreover, the number of females included is rather low; further studies should include a higher number of females. Our study is retrospective, a prospective study assessing the age at onset of different types of tics would be necessary to compare the evolution of TS between sexes. Inclusion of clinical scales to contrast the clinical profile of ADHD and OCD between males and females is desirable for further prospective studies.
In conclusion, a dimorphism in the clinical presentation of TS was observed between sexes with males showing an early greater ADHD comorbidity and appearance of complex motor tics; however, females showed a later increase of complex motor tics. Such differences may represent complex and distinct sex-related changes in dopamine receptor expression, morphological and functional variations during central nervous system maturation.
Supplementary Materials
To view supplementary material for this article, please visit http://doi.org/10.1017/S1092852922000074.
Author Contributions
J.F.B.-C. gathered the data, conceptualized, and wrote the first draft of the manuscript. J.J. gathered the data, conceptualized, and reviewed the manuscript.
Disclosure
The authors do not have any competing interests to disclose.






