Juvenile depression is increasing in frequency (Reference Fombonne, Rutter and SmithFombonne, 1995) and is associated with serious psychosocial impairment, increased risk of suicide and relapse during adolescence (Reference Kovacs, Feinberg and Crouse-NovakKovacs et al, 1984). Long-term follow-up studies have emphasised the increased risk of adult depression (Reference Harrington, Fudge and RutterHarrington et al, 1990; Reference Rao, Ryan and BirmaherRao et al, 1995; Reference Pine, Cohen and GurleyPine et al, 1998; Reference Weissman, Wolk and GoldsteinWeissman et al, 1999a ). However, depression with a prepubertal onset is associated with a lower risk of adult depression and different family and psychosocial correlates compared with adolescent-onset depression (Reference Harrington, Rutter and WeissmanHarrington et al, 1997; Weissman et al, Reference Weissman, Wolk and Goldstein1999a ,Reference Weissman, Wolk and Wickramaratne b ). Moreover, comorbid conduct disorder appears to be associated with different treatment response (Reference Hughes, Sheldon and PreskornHughes et al, 1990), clinical features (Reference Steinhausen and ReitzleSteinhausen & Reitzle, 1996; Reference Simic and FombonneSimic & Fombonne, 2001) and adult outcomes (Reference Harrington, Fudge and RutterHarrington et al, 1991). This longitudinal study investigated further the heterogeneity of juvenile depression and more specifically reassessed the impact of comorbid conduct disorder on adult depressive recurrence.
METHOD
Participants
Patients who attended the child psychiatry department at the Maudsley Hospital, a south London hospital, between 1970 and 1983 were targeted (n=5380). The Maudsley item sheet database was used to select patients for inclusion in the study. From the late 1940s onwards, item sheets completed by mental health professionals (registrars, child psychiatry consultants and others) have been collected and (since 1968) computerised, providing a unique record of socio-demographic and referral data, multi-axial diagnostic formulations and symptom counts on all patients. The subject selection procedure is summarised in Figure 1. The database was searched for subjects presenting symptoms of major depressive disorder (MDD), with or without symptoms of conduct disorder. Several operational definitions were used. First, based on symptom counts, operational definitions of both MDD and conduct disorder were used, consistent with prior studies (see symptom lists below; Reference PearcePearce, 1978; Reference Harrington, Fudge and RutterHarrington et al, 1990). These broad syndromic definitions were devised in order to maximise the sensitivity of the selection process; accordingly, it was expected that a substantial proportion of subjects would subsequently fail to meet strict research diagnostic criteria. In order to meet criteria for the operational definition of depression, subjects had to have a score of 2 (definitely present) for ‘morbid depression, sadness, unhappiness and tearfulness’, associated with two other definite symptoms of depression chosen from a list of nine associated symptoms. For conduct disorder, subjects had to have at least two symptoms with a definite level of severity out of a list of 12 symptoms. Subjects meeting criteria for either depression alone or depression and conduct disorder were included in the next stage. Second, for subjects seen from 1973 onwards, subjects with an ICD—9 Axis I diagnosis suggestive of a depressive disorder (300.4; 309.0; 309.1; 309.4; 311.x; 312.3 and 313.1) were also included (World Health Organization, 1978). Third, subjects with an ICD—9 Axis I diagnosis of conduct disorder (312.0; 312.1; 312.8; 312.9) were also selected if they had a depressive syndrome score of 6 or more calculated by summing the scores for all depressive symptoms. The latter definition differed from the syndromic definition described above by relaxing the requirement of having scores of 2 on depressive symptoms, thereby allowing subjects with low-grade but pervasive depressive symptomatology to be included. Subjects with ‘mental retardation’ (IQ<70) or a pervasive developmental disorder were excluded.
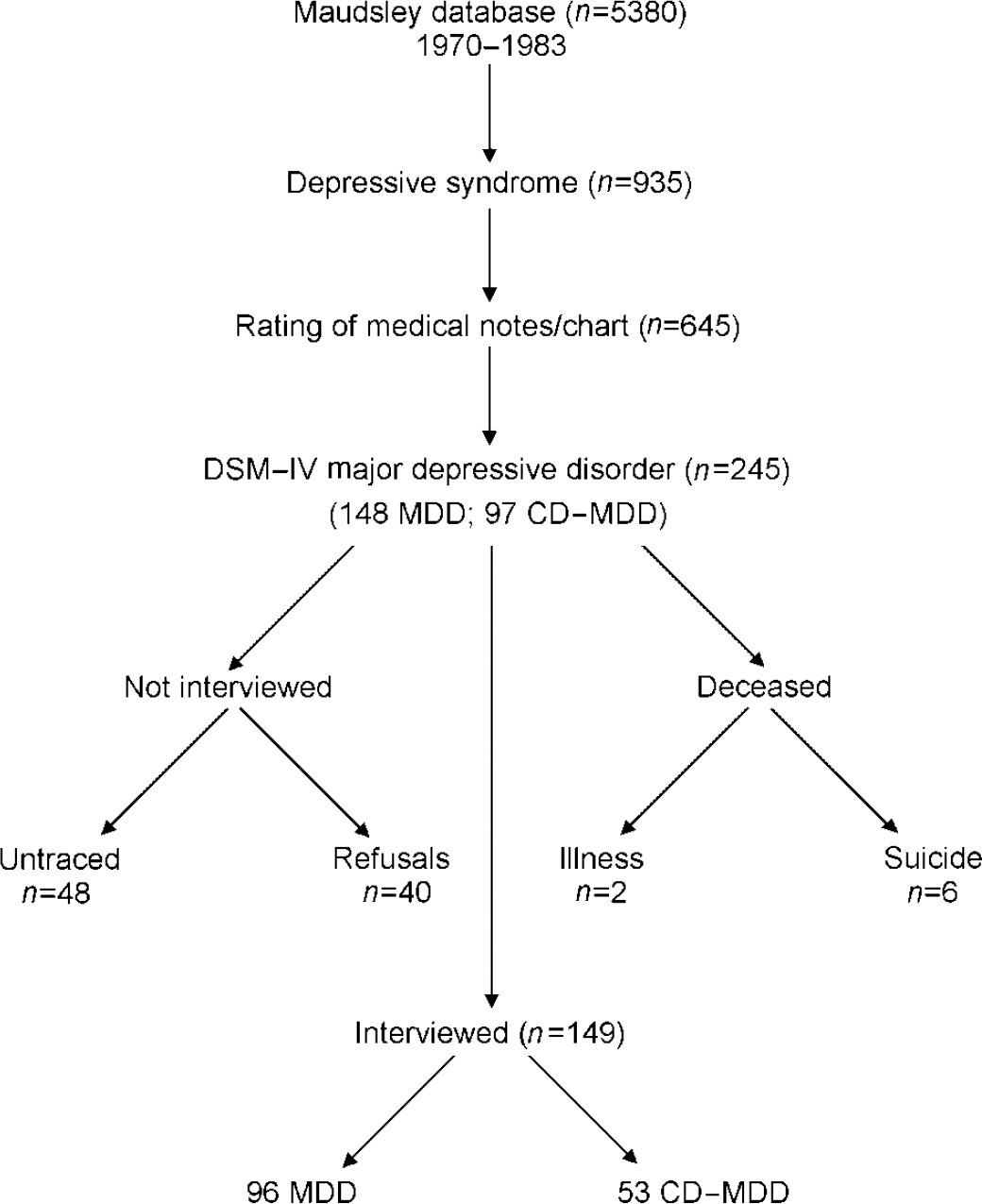
Fig. 1 Participant selection procedure; CD-MDD, major depressive disorder with conduct disorder; MDD, major depressive disorder without conduct disorder.
Of the 935 children selected at this stage, 645 had their medical notes retrieved and rated by an experienced child psychiatrist (see below); 245 children met criteria for MDD either without (n=148) or with (n=97) conduct disorder. These individuals were then traced for follow-up interview. Eight had died during the intervening period, and 48 could not be traced despite repeated attempts. Of the remaining 189 subjects, 40 either refused to be interviewed or repeatedly defaulted on appointments made by interviewers. The remaining 149 individuals were successfully interviewed (Fig. 1).
Measures
Childhood measures
Maudsley item sheet database. After the initial psychiatric assessment of every patient attending the Maudsley Hospital child psychiatry department, a summary sheet containing data on the patient's psychiatric symptoms (0, not present; 1, minimal or dubious; 2, definitely present), psychological, medical and socio-demographic characteristics and family circumstances was systematically completed by medical staff, and these data have been computerised since 1968. Data are available for 52 psychiatric symptoms (12 emotional and 6 somatic; 12 speech, language and motor functioning; 12 conduct symptoms; 7 disturbed relationships; and 3 other). The reliability, internal consistency and validity of item scale scores has been reported elsewhere (Reference Goodman and SimonoffGoodman & Simonoff, 1991; Reference FombonneFombonne, 1998; Reference Moore and FombonneMoore & Fombonne, 1999; Reference Simic and FombonneSimic & Fombonne, 2001).
Symptoms scale scores were created in order to provide more reliable indices of baseline childhood psychopathology. We devised a depression scale score (six items: morbid depression, sadness, unhappiness and tearfulness; suicidal ideas, attempt or threat; school refusal or phobia; abnormally elevated mood; disturbance of eating; disturbance of sleeping; pains of mental origin; α=0.52); an anxiety scale score (six items: morbid anxiety, worrying or panic; situation— or object-specific fears or phobias; ruminations, obsessions, rituals or compulsions; hypochondriasis; depersonalisation or derealisation; conversion hysterical symptoms; α =0.51); an antisocial scale score (eleven items: morbid irritability, screaming, tempers; disobedience; stealing; destructiveness or malicious damage; fire-setting; truancy or staying out late; running away; sexual misbehaviour; fighting, bullying, aggression; violent assault; other antisocial behaviour; α=0.71); an adult relationship scale (three items: overt disturbance of child—mother relationship; overt disturbance of child—father relationship; overt disturbance of relationship with other adults; α=0.65); and a sibling/peer relationship score (two items: overt disturbance of patient-sibling relationship; overt disturbance of relationships with other children; α=0.49). Original ratings (0, 1 and 2) were retained to derive these composite scores and all items contributed only to one scale. In light of its considerable clinical significance, the suicidality item (suicidal ideas, attempt or threat) is used on its own to describe patient status at referral.
The following variables of the database were also used in this set of analyses: pubertal status (prepubertal, pubescent or postpubertal); parent/sibling lifetime history of suicide or psychiatric contact (positive or not); family circumstances of the child (living with both parents v. other situations); brought before the juvenile court at any time (no v. police caution or juvenile court attendance); and social class. All these variables had been recorded with a stable format throughout the study period.
Ratings of medical notes. All the medical, social, educational and psychological data for subjects meeting at least one selection criterion were carefully reviewed by an experienced child psychiatrist and rated using DSM—V diagnostic criteria for MDD and conduct disorder (American Psychiatric Association, 1994). The presence of other comorbid disorders at presentation was separately recorded using ICD—10 clinical guidelines (World Health Organization, 1992). Other data were extracted on an ad hoc questionnaire covering socio-demographic details, referral origin, family psychiatric history, obstetric and birth information, history of any developmental delay or abnormality, physical health, hospital admissions, current weight and height, pubertal status, school attendance and achievement, as well as peer relationships. Psychometric data (mostly from the results on the Wechsler Intelligence Scale for Children (Reference WechslerWechsler, 1974)) were also extracted when present. Family relationships were evaluated from the original psychiatric assessment and reports by other agencies. In addition, components of the psychiatric intervention were noted, including the use of family, individual or other forms of psychotherapy, any prescription of antidepressants and of other drugs either before or after the initial Maudsley assessment, and other interventions. In-patient admissions at the Maudsley and Bethlem Hospitals were recorded.
Adult follow-up measures
Lifetime rates of specific psychiatric disorders were measured using a revised semi-structured version of the Schedule for Affective Disorders and Schizophrenia—Lifetime version (SADS—L; Reference Harrington, Hill and RutterHarrington et al, 1988). Diagnoses were made according to the revisions of the Research Diagnostic Criteria (RDC; Reference Spitzer, Endicott and RobinsSpitzer et al, 1978; Reference Mazure and GershonMazure & Gershon, 1979). Major depression was therefore diagnosed with a 4-week duration and social impairment criteria. Simple phobias with no significant impairment did not count towards a diagnosis of phobic disorder. To improve coverage, dysthymic disorder was coded using DSM—IV criteria, and eating disorders were diagnosed using DSM—III—R criteria (American Psychiatric Association, 1987). Diagnostic hierarchies were removed to allow comorbid patterns between disorders to be fully observed.
Other data were collected on adult social functioning, family psychiatric history, childhood experiences of care and abuse, life events, social support, neuroticism and psychological characteristics, and use of services. Criminal records and death certificates were also available.
Data collection procedures
Participants were located through the Central Register of the National Health Service. A letter of information was sent, followed shortly afterwards by a home visit by one interviewer. Repeated visits were made in the evening or at weekends in order to establish contact with the subject. Most interviews were completed in two sessions of 3-4 hours. A small payment was available for out-of-pocket expenses to facilitate participation.
Data were collected by four female interviewers during the period 1994 to 1999. All had a master's degree or equivalent educational attainment and had prior experience of working with subjects with mental illness. Interviewers were trained to apply the measures through a combination of teaching tapes and videos, role play and pilot interviews. Interviews were audiotaped unless the respondent objected. During fieldwork, joint interviews were performed by a pair of interviewers on several occasions. Interviewers were blind to childhood diagnosis. To maintain blindness during the assessment, all interviews started with the SADS—L focusing on life after the respondent's 17th birthday. After each interview, interviewers wrote detailed vignettes on positive screens of the SADS—L. These vignettes were scored independently by other interviewers and the first author blind to childhood diagnosis. Rating meetings were held regularly and rating discrepancies were resolved by consensus.
Interrater reliability
A subsample of medical notes chosen at random in three groups — subjects with other psychiatric disorders excluded from the study (n=15), subjects with MDD (n=25) and subjects with both conduct disorder and MDD (CD—MDD) (n=19) — were rated blindly by an independent rater. The sample available consisted of 59 subjects (mean age 13.3 years at attendance). The interrater agreement was good for eight depressive symptoms (median κ=0.64) although it was low (κ=0.11) for one symptom (retardation/agitation) with a very low frequency; otherwise, κ coefficients ranged from 0.51 to 0.90 for the seven other symptoms. Agreement was excellent on the overall diagnosis of MDD (κ=0.956). Not surprisingly, agreement for conduct symptoms was better (median κ=0.825), and agreement was also very high on an overall diagnosis of conduct disorder (κ=0.965).
Interrater reliability coefficients for SADS—L ratings of depressive disorders were as follows: major depression, κ=0.78; minor depression, κ =0.52; dysthymic disorders, κ=0.53; and any depressive disorder, κ =0.90. Agreements for other disorders were: Briquet's disorder, κ =0.55; generalised anxiety disorder, κ=0.68; phobic disorder, κ =0.78; obsessive—compulsive disorder, κ=0.48; any anxiety disorder, κ=0.77; bipolar disorders, κ=0.38; any eating disorder, κ =0.78; and excellent (κ>0.80) for all other disorders. Lower values of κ mostly reflected lower base rates for some disorders.
Statistical analyses
Univariate comparisons were performed using the χ2, Fisher's exact and Student's t tests. Reliability was assessed with Cohen's κ coefficient for categorical measures. The effect of comorbid conduct disorder on rates of adult disorders was assessed with logistic regression models controlling for age and gender. To adjust for unequal observation times, Cox proportional hazards models were fitted to the data and relative risks of adult MDD according to childhood comorbidity status were estimated. Survival functions were calculated with the Kaplan—Meier estimator, with age of onset at the first episode of depressive recurrence as the dependent event. Subjects free of any MDD relapse during their adult years were right-censored. Differences between survival functions were examined with the log-rank test. Throughout, a conventional P value of 0.05 was retained as the level of statistical significance.
RESULTS
Interviewed v. non-interviewed subjects
Of the 245 subjects included in the study, 8 (5 men) had died by the time they were traced. Further details on suicidal deaths are provided in a companion paper (Reference Fombonne, Wostear and CooperFombonne et al, 2001, this issue). The rates of completed interviews did not significantly differ between diagnostic groups: 67.5% v. 58.2%; χ 2=1.35, d.f.=1, NS. Excluding untraced subjects, refusal rate was 21.2% (40/189) with no difference between the two diagnostic groups (21.3% v. 20.9%; χ2=0.001, d.f.=1, NS). Differences between interviewed and non-interviewed subjects were investigated on 14 baseline psychiatric measures and demographic characteristics available from the item sheet computerised database; these included gender, age at Maudsley attendance, year of Maudsley attendance, family situation, social class, pubertal status, psychiatric family history, suicidality at presentation, contacts with the juvenile court and the scores on the five item sheet scales. Preliminary analyses did not show differences between non-interviewed and untraced subjects. Accordingly, they were pooled together in a single non-interviewed group.
Within the MDD group, the only difference found indicated a higher proportion of men in the non-interviewed subjects compared with the interviewees (60.0% v. 38.5%; χ2=6.1, d.f.=1, P=0.014); all other comparisons were non-significant. Within the CD—MDD group, the only difference found was for the peer/sibling disturbances scale score, which was slightly higher in the interviewed group than in the non-interviewed subjects (2.38 v. 1.76; t=2.2, d.f.=89, P=0.03). The proportion of men was slightly higher in the non-interviewed group (52.6% v. 41.5%) but not significantly so. Thus, on the whole, there were few differences between baseline characteristics and follow-up interview status in both groups. In particular, levels of depressive symptoms were comparable in both groups and, for the CD—MDD group, levels of conduct symptomatology were also at similar levels according to interview status. Within the CD—MDD group, the rates of combined criminal offences in adulthood were also at roughly similar levels for interviewed and non-interviewed subjects (39.6% v. 52.6%; two-tailed Fisher's exact test, P=0.286); however, the tendency towards higher rates of criminality in non-interviewed subjects was also noticed when more serious offences only were considered (1.9% v. 13.2%; two-tailed Fisher's exact test, P=0.078).
Follow-up sample: childhood data
The sample predominantly comprised patients in their mid-adolescent years, with only 16.1% of subjects under the age of 12 years. Similarly, the proportion of prepubertal children was low (19.7%) compared with that of postpubertal patients (57.7%). There was a marked preponderance of girls in the sample, with no difference between the two groups. However, as reported in other studies, the proportion of males was strongly associated with pubertal status (prepubertal, 75.9%; pubescent, 51.5%; postpubertal, 22.4%; χ 2=28.5, d.f.=2, P<0.001). There was no difference between the groups in terms of social class, year of attendance at the Maudsley or area of residence (Table 1).
Table 1 Socio-demographic characteristics in childhood
| MDD (n=96) | CD-MDD (n=53) | P | |
|---|---|---|---|
| Age in years at Maudsley attendance, mean (s.d.) | 13.8 (1.92) | 14.1 (1.75) | NS |
| Year of attendance, n(%) | |||
| 1970-1973 | 34 (35.4) | 12 (22.6) [UNK] | |
| 1974-1977 | 30 (31.3) | 20 (37.8) [UNK] | NS |
| 1978-1983 | 32 (33.3) | 21 (39.6) [UNK] | |
| Male gender, n(%) | 37 (38.5) | 22 (41.5) | NS |
| Pubertal status, n(%)1 | |||
| Prepubertal | 18 (19.1) | 10 (20.8) [UNK] | |
| Pubescent | 22 (23.4) | 10 (20.8) [UNK] | NS |
| Postpubertal | 54 (57.5) | 28 (58.4) [UNK] | |
| Lives with two parents, n(%) | 67 (69.8) | 24 (45.3) | 0.003 |
| Positive family history, n(%) | 36 (39.1) | 17 (37.8) | NS |
| Social class, n(%)1 | |||
| I-II | 12 (13.5) | 2 (4.9) [UNK] | |
| III non-manual | 19 (21.3) | 7 (17.1) [UNK] | NS |
| III manual | 36 (40.5) | 21 (51.2) [UNK] | |
| IV-V | 22 (24.7) | 11 (26.8) [UNK] | |
| Residence, n(%) | |||
| South London | 55 (57.3) | 34 (64.1) [UNK] | |
| Greater London | 11 (11.5) | 3 (5.7) [UNK] | NS |
| Elsewhere | 30 (31.2) | 16 (30.2) [UNK] |
Item sheet measures showed comparable levels of depressive symptomatology in both groups (Table 2). Anxiety symptom scores were, as expected, significantly higher in the MDD group, while the CD—MDD group displayed significantly higher levels of other disturbances, particularly suicidality. Over half the sample were suicidal at the time of hospital attendance. Broadly similar results with respect to levels of depressive and conduct symptomatology were obtained with blind ratings of the notes. Although there was a significant difference in the average number of depressive symptoms, the magnitude of this difference remained small. Conduct disturbances discriminated between the groups efficiently. In line with anxiety scale scores, categorical diagnoses of comorbid anxiety were found at significantly higher rates in the MDD group. In contrast, attention-deficit hyperactivity disorder and substance misuse or dependence were almost exclusively found in the CD—MDD group.
Table 2 Clinical characteristics in childhood
| MDD (n=96) | CD-MDD (n=53) | P | |
|---|---|---|---|
| Maudsley item sheet | |||
| Depression score, mean (s.d.) | 5.54 (2.13) | 5.64 (1.92) | NS |
| Anxiety score, mean (s.d.) | 3.16 (2.46) | 1.80 (1.97) | 0.001 |
| Conduct score, mean (s.d.) | 1.30 (2.07) | 7.90 (3.55) | 0.001 |
| Suicidal, n(%) | |||
| Minimal | 14 (13.5) | 6 (11.3) [UNK] | 0.013 |
| Definite | 31 (32.3) | 30 (56.6) [UNK] | |
| Adult relationships score, mean (s.d.) | 2.25 (1.64) | 3.85 (1.80) | 0.001 |
| Peer/sibs relationships score, mean (s.d.) | 1.21 (1.27) | 2.38 (1.35) | 0.001 |
| Contact with juvenile court, n(%) | 2 (2.1) | 14 (28.6) | 0.001 |
| Medical notes ratings | |||
| MDD symptoms, mean (s.d.) | 5.52 (0.94) | 5.11 (0.97) | 0.015 |
| Conduct disorder symptoms, mean (s.d.) | 0.10 (0.31) | 4.42 (1.65) | 0.001 |
| Full-scale IQ, mean (s.d.)1 | 105.5 (17.6) | 97.5 (14.8) | 0.031 |
| Comorbid disorders, n(%) | |||
| Separation anxiety | 17 (17.7) | 1 (1.9) | 0.003 |
| Generalised anxiety | 19 (19.8) | 2 (3.8) | 0.006 |
| Any anxiety disorder | 47 (49.0) | 3 (5.7) | 0.001 |
| Attention-deficit hyperactivity disorder | -(0) | 4 (7.6) | 0.015 |
| Substance misuse/dependence | 1 (1.0) | 17 (32.1) | 0.001 |
| Any comorbid disorder | 58 (60.4) | 25 (47.2) | 0.12 |
| Treatment data, n(%) | |||
| Family therapy | 29 (31.2) | 14 (26.4) | 0.54 |
| Parental guidance/counselling | 45 (48.4) | 23 (43.4) | 0.56 |
| Child therapy | 59 (63.4) | 34 (64.2) | 0.93 |
| Tricyclic antidepressant drugs | 45 (48.4) | 16 (30.2) | 0.032 |
| Other psychotropic drugs | 30 (32.3) | 15 (28.3) | 0.62 |
| In-patient admission | 26 (28.0) | 14 (26.4) | 0.84 |
Although IQ data were not available for about two-fifths of the sample, the proportion of subjects with IQ data did not differ importantly across groups (49% v. 34.0%; Fisher's exact test, P=0.087). Consistent with the literature, subjects with CD—MDD had, on average, lower IQs. The strong differences in symptom and diagnostic profiles were not paralleled by differences in treatment data. Diverse therapeutic ingredients and modalities were used during the treatment of the index episode, often in combination, and with generally uniform frequencies across diagnostic groups. Over a quarter of the sample had been admitted for in-patient psychiatric treatment at the Maudsley and Bethlem Hospitals. As admissions before or after attendance at the Maudsley Hospital are not counted, this figure represents an underestimate of the frequency of in-patient treatment in this sample. For the 40 subjects admitted to hospital, the average length of in-patient stay was 275 days (interquartile range 82-430 days), with no difference between the two diagnostic groups (t=0.65, d.f.=38, NS). The only exception was the use of antidepressant medications. Any occurrence of antidepressant prescription either before admission or after initial presentation was counted as positive. Most prescriptions were for tricyclic antidepressants; dosages were either unavailable or not reported consistently over time, precluding further quantitative analysis. Over two-fifths of the sample (41.8%) had received antidepressant drug treatment at one time. A significant difference emerged between the two diagnostic groups, with more antidepressant prescriptions in the MDD group. In so far as such a difference did not apply to other psychotropic drugs, these findings suggest both that antidepressant prescriptions were specifically employed to match the symptomatic presentation and that depressive phenomenology might have been more easily recognised in the non-comorbid group. Electroconvulsive therapy was used in 2% of the sample (2 MDD, 1 CD—MDD).
Adult rates of psychiatric disorders
The vast majority of the sample (84.6%) were in their fourth decade of life, and over half (51%) were 35 years old or more. The mean age at follow-up was 34.6 years (range 25.4-43.5 years, s.d.=4.1). The mean follow-up interval was 20.7 years (range 13.0-27.7 years, s.d.=3.8). There was no difference between the two groups with respect to these two variables.
Adult rates of psychiatric disorders apply from age 17 years onwards (Table 3). As episodes of disorders occurring in childhood or adolescence did not contribute to these figures, these rates are underestimates of ‘true’ lifetime rates. Nevertheless, 86.6% of the sample reported at least one episode of psychopathology over the 21-year follow-up interval. The rate of adult MDD (62.5%) was high in the whole sample, and three-quarters of the respondents had experienced some form of depressive disorder through follow-up. Anxiety disorders (39.6%) were the second most frequent diagnoses with a typically high overlap between subtypes of anxiety disorders. Alcohol disorders were endorsed by nearly a third of the sample (32.2%). The rates of all other psychiatric disorders were lower (<20%). In particular, adult rates of bipolar disorders were only moderately raised compared with general population estimates.
Table 3 Rates of psychiatric disorders through follow-up
| MDD (n=96) | CD—MDD (n=53) | Odds ratio1 | 95% Cl | P | |
|---|---|---|---|---|---|
| Any depression | 74.0 | 77.4 | 1.29 | 0.56-2.96 | 0.55 |
| Major depression | 63.5 | 60.4 | 0.91 | 0.44-1.89 | 0.80 |
| Minor depression | 13.5 | 26.4 | 2.34 | 1.0-5.49 | 0.05 |
| Dysthymic disorder | 9.4 | 15.1 | 1.76 | 0.63-4.89 | 0.28 |
| Bipolar disorders | 5.2 | 3.8 | 0.67 | 0.12-3.69 | 0.64 |
| Any affective disorder | 75.0 | 77.4 | 1.21 | 0.53-2.79 | 0.65 |
| Briquet's disorder | 6.2 | 17.0 | 3.2 | 1.06-9.58 | 0.04 |
| Any anxiety disorder2 | 36.5 | 45.3 | 1.51 | 0.75-3.04 | 0.25 |
| Generalised anxiety | 12.5 | 15.1 | 1.25 | 0.48-3.29 | 0.65 |
| Panic disorder | 12.5 | 22.6 | 2.14 | 0.87-5.27 | 0.10 |
| Phobic disorder | 22.9 | 24.5 | 1.12 | 0.50-2.50 | 0.79 |
| Obsessive—compulsive disorder | 5.2 | 7.5 | 1.51 | 0.39-5.89 | 0.56 |
| Alcoholism | 26.0 | 43.4 | 2.2 | 1.06-4.41 | 0.033 |
| Schizophrenia | 4.2 | 7.5 | 1.9 | 0.45-7.92 | 0.18 |
| Drug misuse and dependence | 1.0 | 28.3 | 40.3 | 5.1-319.2 | 0.0001 |
| Eating disorders | 6.2 | 15.1 | 2.96 | 0.93-9.38 | 0.065 |
| Antisocial personality | 1.0 | 45.3 | 89.4 | 11.2-712.3 | 0.0001 |
| Any adult disorder | 83.3 | 92.5 | 2.63 | 0.81-8.50 | 0.11 |
Systematic comparisons between the two groups were undertaken with logistic regression analyses, adjusting for gender and age at follow-up. The odds ratios provide an estimate of the increase in adult rates of psychiatric disorders attributable to comorbid conduct disorder in childhood. Contrary to one of our main hypotheses, the MDD and CD—MDD groups showed strictly comparable levels of MDD recurrence in adulthood. This held true when the definition of depression was widened to include minor depression and dysthymic disorder. Three-quarters of the subjects in each group had experienced at least one episode or form of affective illness. If anything, there was a trend for the comorbid group to have higher rates of minor forms of affective illness which just reached the level of statistical significance for minor depression. Survival models confirmed the lack of difference in risk of depressive recurrence when comparing the CD—MDD group with the MDD group (relative risk 0.95, 95% CI 0.62-1.46). Figure 2 shows the proportion of subjects in each group remaining free from MDD recurrence from age 17 years up to 43 years. The timing of MDD relapse during the follow-up period was similar in the two groups, with no statistical difference between the two survival curves (log-rank test 0.05, d.f.=1, NS). The median survival times were 30 years (95% CI 26-34) for the MDD group and 30 years (95% CI 22-38) for the CD—MDD group. At the end of the follow-up period, the survival probabilities of remaining free of MDD relapse were similar in the MDD group (0.245) and the CD—MDD group (0.309). Including minor depression in the analysis produced similar results (relative risk 1.06, 95% CI 0.69-1.62). Equally, no difference was found for survival distributions (log-rank test 0.87, d.f.=1, NS). When gender was included as covariate in the proportional hazard models, relative risks were virtually unchanged.
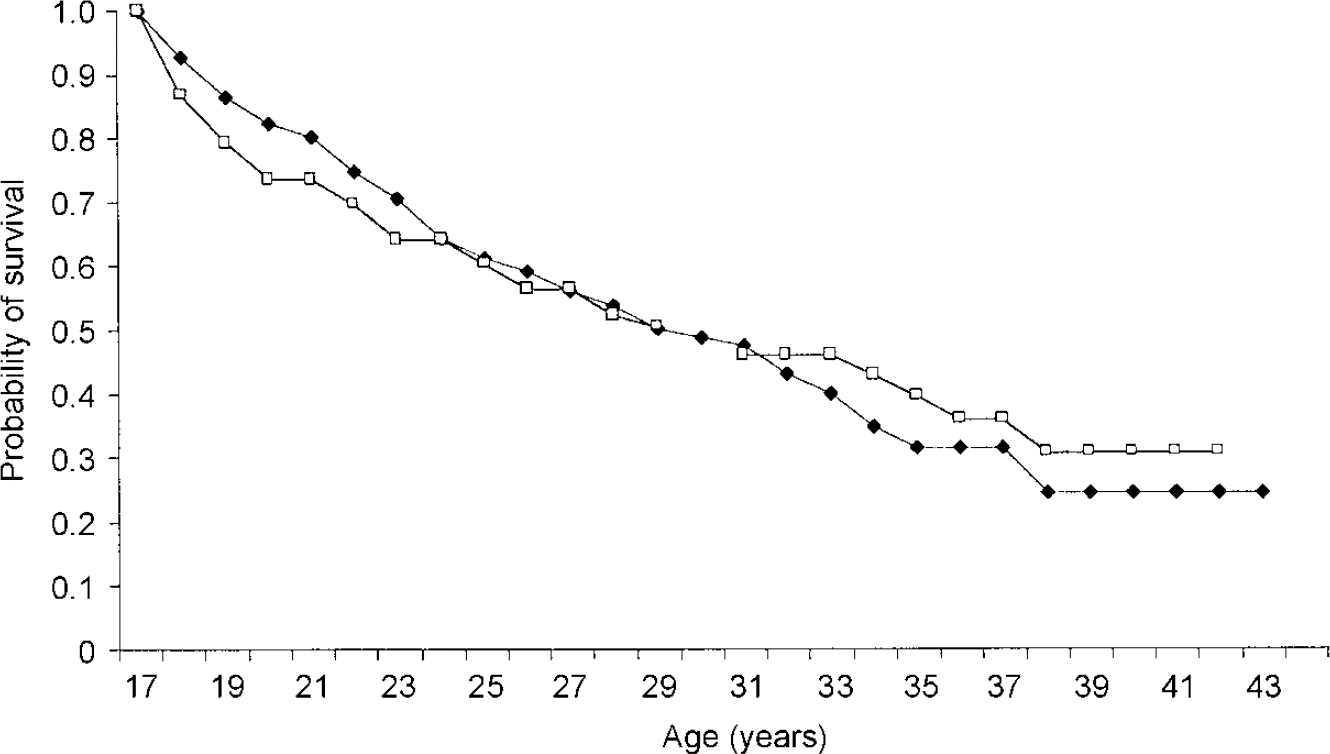
Fig. 2 Survival from major depressive disorder with (□) or without (♦) conduct disorder, by childhood diagnosis: Kaplan—Meier estimation.
With the exception of bipolar and affective disorders, all other psychiatric disorders occurred more frequently in the CD—MDD group than in the MDD group, as shown by odds ratios uniformly higher than unity. This heavy load of adult psychopathology was significantly raised for Briquet's disorder, alcohol disorders, drug misuse and dependence, and antisocial personality.
Women had significantly higher rates of MDD (OR=3.1, 95% CI 1.5-6.3), any depression (OR=3.9, 95% CI 1.8-8.7), panic disorder (OR=3.1, 95% CI 1.1-9.1), phobic disorder (OR=2.8, 95% CI 1.2-6.8), any anxiety disorder (OR=2.5, 95% CI 1.2-5.2) and eating disorders (OR=10.5, 95% CI 1.3-83.8). No significant childhood diagnosis × gender interactions were found, although a trend (P=0.04) was noted for women with CD—MDD to have much higher rates of alcoholic disorders than those with MDD (51.6% v. 20.3%; P=0.004); whereas men in both groups had equal, intermediate-level rates (31.8% v. 35.1%; NS). The same trend applied to rates of drug misuse and dependency, although owing to small cell sizes, power to detect a significant interaction was seriously reduced. Nevertheless, drug misuse and dependency was significantly higher in the CD—MDD group than in the MDD group, both for men (18.2% v. 0%; Fisher's exact test, P=0.016) and women (35.5% v. 1.7%; Fisher's exact test, P<0.001), the levels for women being much higher than those for men.
DISCUSSION
Methodological strengths and weaknesses
Compared with other follow-up studies of juvenile depression, this study had both the largest sample size and the longest follow-up interval. Therefore, most participants would have lived partly through the period at risk for most psychiatric disorders under investigation. Second, attendance at the Maudsley Hospital was typically during the mid-adolescence years, and few subjects were younger than 12 years or prepubertal. Accordingly, this study reflects mostly on the outcome of adolescent rather than child depression. Third, although the catch-up follow-up design precluded direct standardised assessment of patients at presentation, participants were selected according to strict DSM—IV diagnostic criteria following a detailed inspection of their medical charts. Good interrater reliability was demonstrated in this selection procedure, and several correlates of the disorder at presentation, such as age and pubertal status, gender repartition, patterns of comorbid disorders, treatment history and especially the high rate of antidepressant treatment during the index episode, argue strongly for the validity of the diagnostic ascertainment. Fourth, although the sample was selected in a tertiary referral centre, the majority of the sample were local residents at the time of first attendance at the Maudsley Hospital. Furthermore, several patients listed as ‘resident of the Home Counties’ were living in nearby cities in Kent, and could therefore be considered as local residents too, suggesting that the sample was reasonably representative of child psychiatric patients in the 1970s. Fifth, by virtue of study design, the study did not include a non-depression group (either psychiatric or normal controls) or a group with conduct disorder only for comparison, as the focus of the study was on assessing the impact of comorbidity on levels and mechanisms of adult depressive recurrence. Finally, compared with the sample of patients with depression included in a previous follow-up study at the same site (Reference Harrington, Fudge and RutterHarrington et al, 1990), our sample was larger (149 v. 52), older (13.9 years v. 12.9 years) and with lower proportions of prepubertal children (19.7% v. 40%) and males (39.6% v. 58%). Moreover, the matching procedure used in the earlier study led to the inclusion of children with comorbid conduct problems in the depression group, whereas this was not possible in this study.
Depressive recurrence
The recurrence rates of major depression (62.6%) and of any depressive disorder (75.2%) following an episode of childhood major depression are among the highest reported so far. In other studies based on clinical samples, investigators have reported a rate of 49.3% for MDD recurrence in a longitudinal study of adolescents with depression (Reference Weissman, Wolk and GoldsteinWeissman et al, 1999a ), a rate of 69% for MDD and 77% for any affective disorder in a 7-year follow-up of 28 adolescents (Reference Rao, Ryan and BirmaherRao et al, 1995), a rate of 62% for MDD recurrence in the earlier Maudsley follow-up study (Reference Harrington, Fudge and RutterHarrington et al, 1990) and a rate of 64% in another longitudinal study of adolescents with depression (Reference Garber, Kriss and KochGarber et al, 1988). Thus, a consistent picture emerges which emphasises the elevated risk of adult depressive recurrence following first-onset major depression in adolescence. The fact that continuity between adolescent and adult depression is also found in community-based samples (Reference Fleming, Boyle and OffordFleming et al, 1993; Reference Pine, Cohen and GurleyPine et al, 1998) suggests that the findings are not a function of some form of selection bias. Rates of other psychiatric disorders were also very high, pointing to persistent levels of comorbidity in adult depression. Contrary to one of our main hypotheses, however, the presence of a comorbid conduct disorder in childhood was not associated with lower rates of major depression in adult life compared with the non-comorbid group. In fact, the group with comorbid conduct disorder showed an overall higher rate of any affective disorder, with minor depression being more often reported. Survival functions were very similar across the two groups, suggesting that the pattern of relapse over time was closely parallel in both groups and that no difference would have emerged even with a larger sample size. Half the sample in each group had experienced a relapse of major depression by age 30 years, although the risk of recurrence did extend beyond that age. The discrepancies between this study and the previous Maudsley follow-up investigation regarding the impact of comorbid conduct disorder on adult depressive recurrence were examined further. In the previous study, rates of adult depression were lower in the comorbid group although, owing to a small sample size, this difference fell short of statistical significance (Reference Harrington, Fudge and RutterHarrington et al, 1991). Less than half the comorbid sample met RDC criteria for MDD in childhood, whereas this was the case for a higher proportion of subjects (70% v. 46%) in the non-comorbid group. Moreover, within the non-comorbid group, recurrence of MDD in adult life was clearly higher for subjects who met RDC criteria for MDD in childhood (40% v. 13.3%); and the only subject from the comorbid group with adult recurrence had also met RDC criteria for MDD in adulthood (further details available from the author upon request). Unfortunately, small sample sizes limited further exploration of the data. Nevertheless, these trends in the data suggest that a broader and less specific depressive construct was used to include subjects in the previous study, whereas this study relied on narrower diagnostic criteria, possibly leading to differences in patterns of adult depression recurrence.
Other psychiatric outcomes
The comorbid group had increased rates of other disorders, including antisocial personality and substance misuse/dependence disorders. The 45% rate of adult antisocial personality disorder at follow-up in the comorbid group is in line with rates of antisocial personality disorder found in adult follow-up studies of youths with conduct disorder but without depression (Reference Zoccolillo, Pickles and QuintonZoccolillo et al, 1992). Thus, comorbid major depression does not appear to attenuate continuities between juvenile and adult antisocial behaviours. The rate of alcoholic disorders in the non-comorbid group suggests a developmental pathway from juvenile depression to adult alcohol dependence which points to negative and heterotypic long-term psychiatric outcomes. Consistent with earlier studies reporting an association between hysteria and antisocial disorders, both at a family level (Reference Cloninger, Reich and GuzeCloninger et al, 1975) and at individual levels (Reference RobinsRobins, 1966; Reference Cloninger and GuzeCloninger & Guze, 1970), we also found an increased rate of Briquet's disorder in our sample which applied to both genders in the comorbid group. All 15 subjects with Briquet's disorder also met criteria for an affective disorder. In keeping with comorbid patterns observed in adolescence, the rates of alcohol and drug misuse and dependence were high in the comorbid group. The transition to bipolar disorder was, in contrast, relatively rare, with no difference between the two groups. Our findings concur with those from some (Reference Harrington, Fudge and RutterHarrington et al, 1990; Reference McCauley, Myers and MitchellMcCauley et al, 1993; Reference Strober, Lampert and SchmidtStrober et al, 1993; Reference Weissman, Wolk and GoldsteinWeissman et al, 1999a) but not all (Reference Strober and CarlsonStrober & Carlson, 1982; Reference Geller, Fox and ClarkGeller et al, 1994; Reference Kovacs, Akiskal and GatsonisKovacs et al, 1994; Reference Rao, Ryan and BirmaherRao et al, 1995) previous studies. These discrepancies in rates of switching to bipolarity clearly require further investigation. Other adult outcomes are discussed in a companion.
paper (Reference Fombonne, Wostear and CooperFombonne et al, 2001, this issue). While overall levels of recurrence of depression in adult life were similar in both groups, it is plausible that the mechanisms underlying recurrence of depression in adult life in subjects with MDD or CD—MDD are not the same.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
• Adolescent depression is associated with a high risk of depressive relapse extending well into adult life.
-
• Depression occurring in adolescents with conduct problems is associated with equally severe affective and more severe non-affective outcomes.
-
• Women with both antisocial and depressive problems have worse outcomes.
LIMITATIONS
-
• Follow-up interviews could be completed on only 63% of the initial sample although rates of interviews were similar in both groups.
-
• Comparison groups with either conduct disorder only or non-affective psychiatric disorders were not available.
-
• Initial psychiatric assessments were based on medical notes.
Acknowledgements
The authors express their thanks to Olive McKeown, Theresa Pearce, Karen Schepman, Debbie Heavey, Val Hicks and Felicity Whitton for their contribution to the study.








eLetters
No eLetters have been published for this article.