Objectives
The objectives of this chapter are to:
Understand the causes of hypoxaemia.
Understand how much oxygen to give.
Be familiar with devices that enable an increase in the inspired oxygen concentration.
Understand the function and use of the self-inflating bag-mask.
Understand the function and use of the Mapleson C breathing system.
Understand how to monitor oxygenation.
Understand the principle of pre-oxygenation.
Causes of hypoxaemia
The strict definition of hypoxaemia is a partial pressure of oxygen in the arterial blood (PaO2) below normal. For patients with no respiratory pathology, a value of <8 kPa or 60 mmHg (equivalent to an arterial oxygen saturation of approximately 90%) is often used to define hypoxaemia requiring treatment; for patients with chronic obstructive pulmonary disease (COPD), a PaO2 <8 kPa(SpO2 <90%) may be ‘normal’. In nearly all patients hypoxaemia can usually be improved, at least initially, by increasing the inspired oxygen concentration.
Although the cause of hypoxaemia is usually multifactorial, there are several distinct mechanisms:
alveolar hypoventilation;
mismatch between ventilation and perfusion within the lungs;
pulmonary diffusion abnormalities;
reduced inspired oxygen concentration.
Alveolar hypoventilation
If insufficient oxygen enters the alveoli to replace that taken up by the blood, both the alveolar (PAO2) and arterial (PaO2) partial pressure of oxygen decrease. In most patients, increasing the inspired oxygen concentration will restore both. When an adult’s tidal volume decreases below approximately 150 mL there is no ventilation of the alveoli, only the ‘dead space’, which is the volume of the airways that plays no part in gas exchange. No oxygen reaches the alveoli, irrespective of the inspired concentration, and profound hypoxaemia will follow. At this point ventilatory support and supplementary oxygen will be required. Hypoventilation is always accompanied by hypercapnia, as there is an inverse relationship between arterial partial pressure of carbon dioxide (PaCO2) and alveolar ventilation.
Common causes of hypoventilation are as follows:
tongue;
blood;
vomit;
bronchospasm;
oedema (infection, burns, allergy).
Central respiratory depression:
drugs;
alcohol;
central nervous system injury (cerebrovascular event, trauma, etc.);
hypothermia.
Impaired mechanics of ventilation:
pain;
pneumothorax or flail chest;
haemothorax;
pulmonary oedema;
diaphragmatic splinting;
pre-existing lung disease.
Mismatch between ventilation and perfusion within the lungs
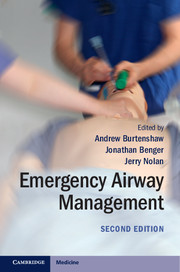
Normally, ventilation of the alveoli (V˙) and perfusion with blood (Q˙) are well matched (V˙/Q˙ = 1), ensuring that haemoglobin in blood leaving the lungs is saturated with oxygen (Figure 2.1). If this process is disturbed (V˙/Q˙ mismatch) regions develop where:
1. Ventilation is less than perfusion (V˙/Q˙<1), resulting in haemoglobin with reduced oxygen content, e.g. pneumothorax, pneumonia.
2. Perfusion is less than ventilation (V˙/Q˙>1). This can be considered wasted ventilation as very little additional oxygen is taken up when haemoglobin is already almost fully saturated (98%), e.g. hypotension, pulmonary embolus.
At its most extreme, some regions of the lung may be perfused but not ventilated (V˙/Q˙ = 0); blood leaving these areas remains ‘venous’, and is often referred to as shunted blood. This is then mixed with oxygenated blood leaving ventilated regions of the lungs. The final oxygen content of blood leaving the lungs is dependent on the relative proportions of blood from these two regions:
Blood perfusing ventilated alveoli leaves with an oxygen content of approximately 20 mL/100 mL blood (assuming a haemoglobin concentration of 150 gL–1).
Blood perfusing unventilated alveoli remains ‘venous’, leaving with an oxygen content of 15 mL/100 mL blood.
The effect of small regions of V˙/Q˙ mismatch can be corrected by increasing the inspired oxygen concentration; however, once more than 30% of the pulmonary blood flow passes through regions where V˙/Q˙<1, hypoxaemia is inevitable, even when breathing 100% oxygen. This is because the oxygen content of the pulmonary blood flowing through regions ventilated with 100% oxygen will increase by only 1 mL/100 mL blood (to produce 21 mL of oxygen per 100 mL blood), and this is insufficient to offset regions of low V˙/Q˙, where the oxygen content will be only 15 mL/100 mL blood.
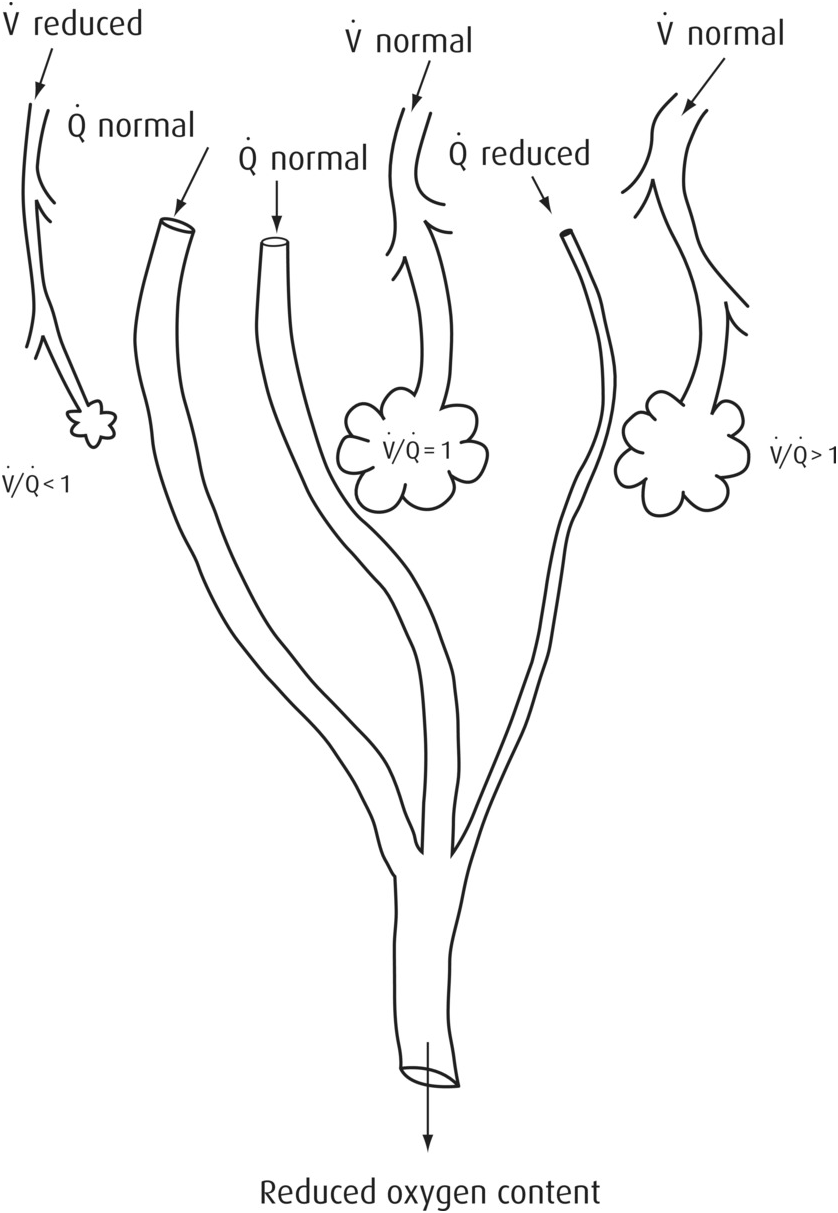
Figure 2.1 Different V˙/Q˙ ratios.
Pulmonary diffusion defects
Any condition that causes thickening of the alveolar membrane (e.g. pulmonary oedema, fibrosing alveolitis) impairs transfer of oxygen into the blood. This is treated first by giving supplementary oxygen to increase the PAO2 (partial pressure of oxygen in the alveoli) and then treating the underlying problem.
How much oxygen?
In the past, oxygen has usually been given on the basis that if some is good, more must be better. It is now recognized that in most circumstances, there is a range of optimal oxygenation and in some conditions (e.g. post-acute myocardial infarction, ischaemic stroke), excess oxygen may be detrimental. In 2008, the British Thoracic Society (BTS) published ‘Guidelines for Emergency Oxygen Use in Adult Patients’. These guidelines recommend that for most acutely ill patients, oxygen should be given to achieve a target saturation of 94–98%, or 88–92% for those at risk of hypercapnic respiratory failure.
Give all critically ill patients (Table 2.1) high-flow oxygen (15 L min–1) until they are stable; then reduce the inspired oxygen concentration to achieve a target saturation of 94–98%. Patients with COPD and other risk factors for hypercapnic respiratory failure who are critically ill are treated similarly, but aim for a saturation of 88–92% once they are stable. When pulse oximetry is unavailable, give high-flow oxygen until definitive treatment is available.
Table 2.1 Critically ill patients
Cardiac arrest or peri-arrest resuscitation
Shock
Sepsis
Near-drowning
Anaphylaxis
Major pulmonary haemorrhage
Major head injury
Carbon monoxide poisoning
Early assessment of gas exchange based on the analysis of an arterial blood sample is essential in all critically ill patients to guide the need for subsequent oxygen therapy or ventilatory support.
Whenever oxygen is given to a patient, it must be prescribed and the target oxygen saturation to be maintained written on the patient’s drug chart.
Devices used for delivery of oxygen
Spontaneous ventilation
Variable-performance devices: masks or nasal cannulae
With these devices, the precise concentration of oxygen inspired by the patient is unknown, because it depends on the patient’s respiratory pattern and the oxygen flow (usually 2–15 L min–1). When breathing through a mask the inspired gas consists of a mixture of:
oxygen flowing into the mask;
oxygen that has accumulated under the mask during the expiratory pause;
alveolar gas exhaled during the previous breath that has collected under the mask;
air entrained during inspiration from the holes in the side of the mask and from leaks between the mask and face.
An example of this type of device is the Hudson mask (Figure 2.2). As a guide, the inspired oxygen concentration will be 25–60% with oxygen flows of 2–15 L min–1. Patients unable to tolerate a facemask, but who can nose breathe, may find either a single foam-tipped catheter or double catheters, placed just inside the vestibule of the nose, more comfortable (Figure 2.3). Lower flows of oxygen are used; 2–4 L min–1 increases the inspired oxygen concentration to 25–40%.

Figure 2.3 Nasal cannulae.
In a critically ill patient breathing spontaneously who requires a higher concentration of oxygen, a Hudson mask with a reservoir (non-rebreathing bag) can be used (Figure 2.4). A one-way valve diverts the oxygen flow into the reservoir during expiration. During inspiration, the contents of the reservoir, along with the high flow of oxygen (12–15 L min –1), ensure minimal entrainment of air, raising the inspired concentration to approximately 80%, providing that the reservoir bag inflates and deflates with each breath. This requires a well-fitting, functioning mask and reservoir, and is often overlooked in clinical practice. An inspired oxygen concentration of 100% can be achieved only by using a close-fitting facemask with an anaesthetic breathing system that includes a reservoir, combined with an oxygen flow of 12–15 L min–1 (see below). Once stable, these patients should have oxygen therapy adjusted as described above.
Fixed-performance devices
These are used to deliver a precise concentration of oxygen, unaffected by the patient’s ventilatory pattern. These devices work on the principle of high-airflow oxygen enrichment (HAFOE). Oxygen is delivered to a Venturi that entrains a much greater, but constant, flow of air (Figure 2.5). The total flow into the mask needs to be as high as 45 L min−1. The high gas flow has two effects: it exceeds the patient’s peak inspiratory flow, reducing entrainment of air, and flushes expiratory gas, reducing rebreathing. These are the devices of choice for patients with known hypercapnic respiratory failure, or who are at risk of this condition.

Figure 2.5 Use of a HAFOE mask delivering (in this case) 40% oxygen.
These devices deliver a fixed concentration for a given flow, and there are several interchangeable Venturis to vary the oxygen concentration (Table 2.2).
The above systems all deliver dry gas to the patient, which may cause crusting or thickening of secretions, difficulty with clearance, and patient discomfort. For prolonged use, a HAFOE system should be used with a humidifier.
Assisted ventilation
Patients whose ventilation is inadequate to maintain oxygenation despite an increase in the inspired oxygen concentration using one of the devices described above, or who are apnoeic, will require oxygenation using a mechanical device. The simplest and most widely used device is the bag-mask (Figure 2.6). An alternative is an anaesthetic breathing system (Figure 2.9).
In selected patients improved oxygenation, as well as ventilatory assistance, can be achieved using either continuous positive airway pressure (CPAP) or non-invasive positive pressure ventilation (NiPPV). These forms of non-invasive ventilatory support are described in Chapter 12.
The bag-mask device
In its simplest form this consists of a self-inflating bag; when squeezed, the contents are delivered to the patient via a non-return valve and facemask. On release, the bag entrains air as it returns to its original shape. Expired air from the patient is prevented from reaching the bag by a one-way valve. In this manner, the patient’s lungs are ventilated with air (21% oxygen). The use of clear, plastic disposable facemasks enable regurgitated stomach contents to be seen sooner and ‘fogging’ of the plastic during exhalation indicates that gas is going into and out of the lungs.
The oxygen concentration in the gas delivered from the bag can be increased in two ways:
1. By connecting a high flow of oxygen (10–15 L min–1) to an inlet port, usually adjacent to the air entrainment valve at the opposite end of the bag to the mask. In this way, when the bag refills, it does so with a mixture of air and oxygen. The oxygen concentration delivered to the patient will depend upon several factors including oxygen flow, rate of ventilation and volume delivered. In the average adult, the concentration is unlikely to exceed 50% (Figure 2.7).
2. In addition to the above, a reservoir can be attached over the air entrainment valve. As the bag is squeezed to ventilate the patient’s lungs, the oxygen flow is diverted and accumulates within the reservoir. As the bag is released it refills from the contents of the reservoir and the oxygen flow, thereby virtually eliminating air entrainment. In this manner, providing the oxygen flow exceeds the minute ventilation of the lungs, close to 100% oxygen can be delivered (Figure 2.8).
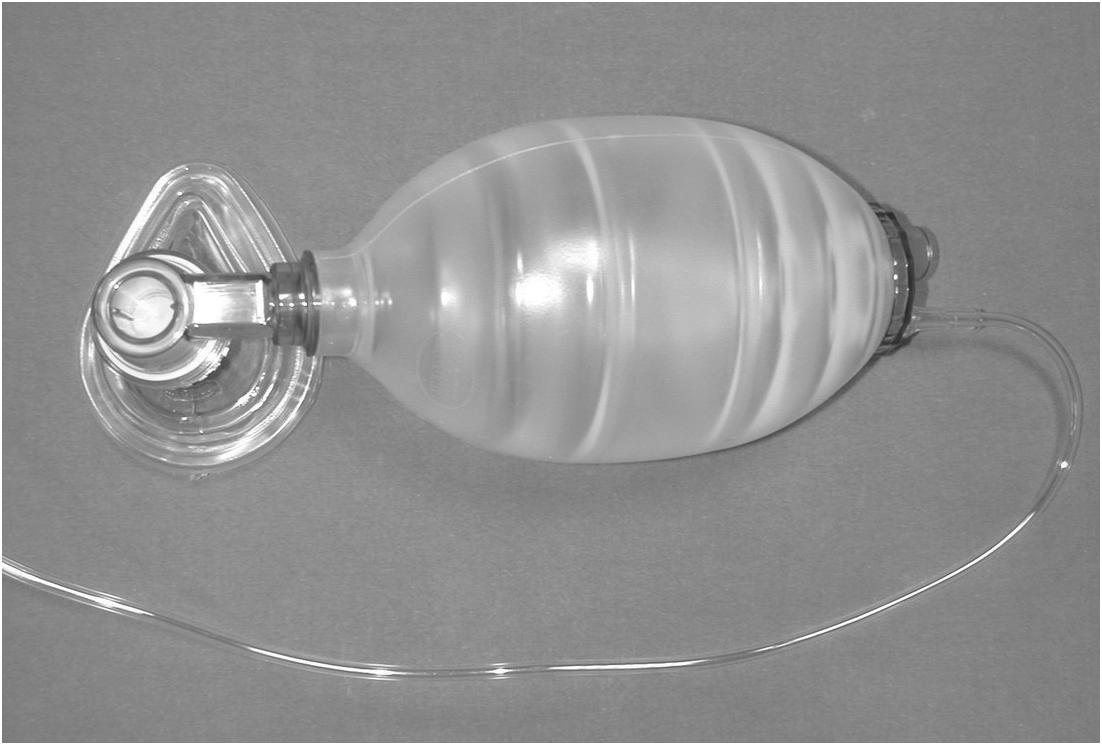
Figure 2.7 Bag-mask with oxygen attached.
Figure 2.8 Bag-mask with oxygen and reservoir.
Oxygen delivery with this device in any configuration is dependent on:
1. The practitioner being able to maintain a good seal between the facemask and the patient’s face, so that there is minimal escape of gas around the mask when the bag is squeezed. This is best achieved by using a two-person technique: one holds the facemask with both hands, while the other squeezes the bag.
2. Avoidance of high pressure and excessive volumes to ventilate the patient’s lungs; these result in gas being forced down the oesophagus and into the stomach. This will reduce ventilation of the lungs and predispose to regurgitation and aspiration.
The commonest reason for requiring high pressures to ventilate the patient’s lungs is failure to maintain a patent airway. This is commonly caused by:
1. Poor airway control: this can often be overcome by using a two-person technique.
2. Foreign material in the airway, e.g. vomit, blood: this must be removed using a safe and effective suction technique.
Although a patient can breathe oxygen spontaneously from a bag-mask device, this is suboptimal because effort is needed to overcome the resistance to inspiratory and expiratory flow. Spontaneously breathing patients should be given oxygen using one of the devices described above, or via an anaesthetic breathing system.
The anaesthetic breathing system
This can be used during both spontaneous and assisted ventilation. Safe use requires an understanding of function, which differs depending on whether the patient is breathing spontaneously or ventilation is assisted.
The most commonly used system in emergency airway management is the Mapleson C breathing system (Figure 2.9). It comprises:
1. An oxygen input, either from the common gas outlet of an anaesthetic machine or a wall-mounted flowmeter.
2. A reservoir bag. This has several functions:
a. It collects the inflowing oxygen during expiration, which is then used to meet the patient’s peak inspiratory flow during spontaneous ventilation.
b. Movement of the bag can be used as an indicator of ventilation.
c. It can be squeezed to deliver oxygen to assist ventilation.
d. If the expiratory valve is closed (or blocked) excess gas accumulates in the bag with minimal increase in airway pressure (a safety feature to protect the patient’s lungs from barotrauma).
3. An adjustable, pressure limiting (APL) valve usually referred to as the expiratory valve. This opens during expiration to enable the escape of exhaled gas (containing carbon dioxide) and prevent its accumulation within the system. This valve also enables the escape of any surplus oxygen flow. The valve can be adjusted manually from fully open (minimal opening pressure) to fully closed (no gas escape is possible through the valve).
4. A connection to a facemask: this is often a short, flexible piece of tubing that may incorporate a bacterial filter.
An important feature of this system is the potential for accumulation of exhaled carbon dioxide within the reservoir bag, which will result in significant hypercapnia. To prevent this, the gas flow must exceed twice the patient’s minute volume. Always use a minimum oxygen flow of 12–15 L min–1.
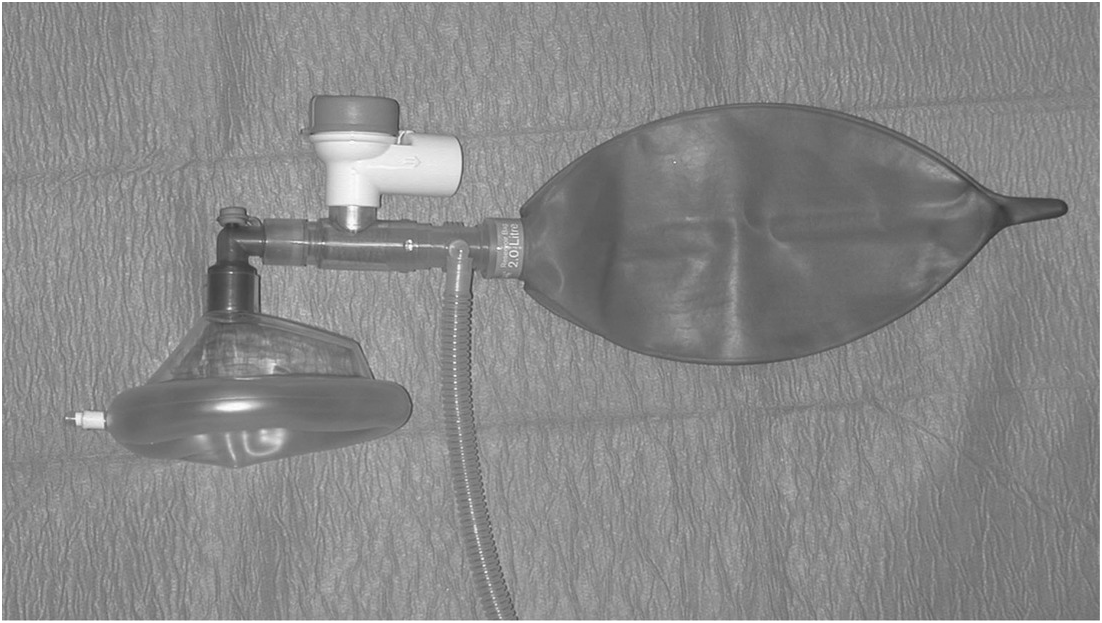
Figure 2.9 Mapleson C anaesthetic breathing system.
Using the Mapleson C breathing system
Spontaneous ventilation The mask is held on the patient’s face with the expiratory valve fully open so that expiration is unimpeded. As the patient breathes in, the negative pressure closes the valve and the bag will collapse slightly. During expiration, the oxygen flow refills the bag and flushes out the exhaled gas containing CO2, resulting in an audible leak of gas via the valve.
Assisted ventilation The mask is held on the patient’s face and the expiratory valve manually adjusted (partially closed) so that sufficient pressure can be generated by squeezing the bag to inflate the lungs (this will often require a second person). Some gas will be heard escaping via the valve. During expiration, the oxygen flow refills the bag and flushes out the exhaled gas containing CO2, resulting in an audible leak of gas via the valve. If the valve is not closed sufficiently during attempted ventilation, the oxygen escapes via the valve rather than entering the patient’s lungs.
Pitfalls when using an anaesthetic breathing system
Spontaneous ventilation
1. Inadequate oxygen flow. Carbon dioxide is not flushed from the system and accumulates in the bag. This leads to rebreathing and the patient will become hypercapnoeic with several adverse effects, e.g. increased cerebral blood flow and intracranial pressure, cardiac arrhythmias.
2. Expiratory valve closed. This prevents expiration, causing an increase in intrathoracic pressure that may have several serious consequences, e.g. increasing intracranial pressure, barotrauma. Gas may also be forced into the stomach and predispose to abdominal splinting and regurgitation. In practice, either an increasing leak develops around the mask or the distending bag should alert the practitioner.
Assisted ventilation
1. Inadequate oxygen flow. It becomes increasingly difficult to provide adequate ventilation as the bag gradually collapses. At this point, the danger is that the expiratory valve is gradually closed to prevent escape of gas and maintain enough volume in the system to squeeze the bag. Although this will apparently enable the patient’s lungs to be ventilated, carbon dioxide is not eliminated and accumulates within the system. The patient becomes rapidly hypercapnoeic, with the problems described above.
Because of the specialist nature of anaesthetic breathing systems, only those with appropriate training should use them.
Monitoring oxygenation
The pulse oximeter
A probe, containing a light-emitting diode (LED) and a photo-detector, is applied across the tip of a digit or earlobe. The LED emits red light alternately at two different wavelengths, in the visible and infrared regions of the electromagnetic spectrum. These are transmitted through the tissues and absorbed to different degrees by oxyhaemoglobin and deoxyhaemoglobin. The intensity of light reaching the photo-detector is converted to an electrical signal. The absorption by the tissues and venous blood is static. This is then subtracted from the beat-to-beat variation in absorption due to arterial blood to display the peripheral arterial oxygen saturation (SpO2), both as a waveform and a digital reading. Pulse oximeters are accurate to ±2% for values in excess of 70%. Below this their accuracy is poorly validated. The waveform can also indicate the heart rate. Alarms are provided for arterial blood saturation and heart rate values. The pulse oximeter therefore gives information about both the circulatory and respiratory systems, and has the advantages of:
providing continuous monitoring of oxygenation at tissue level;
being unaffected by skin pigmentation;
portability (mains or battery powered);
being non-invasive.
There are several important limitations to this device:
Failure to realize the severity of hypoxaemia; because of the shape of the oxyhaemoglobin dissociation curve (Figure 2.10), a saturation of 90% equates to a PaO2 of 8 kPa (60 mmHg).
Unreliable when there is severe vasoconstriction, because of the reduced pulsatile component of the signal.
Provides no indication of the PaCO2; profound hypercapnia is possible with normal oxygen saturations, particularly in the presence of alveolar hypoventilation and a high concentration of inspired oxygen.
Unreliable with certain haemoglobins:
a. when carboxyhaemoglobin is present, it overestimates arterial oxygen saturation (SaO2)
b. when methaemoglobin is present, at saturations greater than 85% it underestimates SaO2.
Progressively under-reads the saturation as the haemoglobin decreases (but is not affected by polycythaemia).
Affected by extraneous light.
Unreliable when there is excessive movement of the patient.
The pulse oximeter is not an indicator of the adequacy of alveolar ventilation.
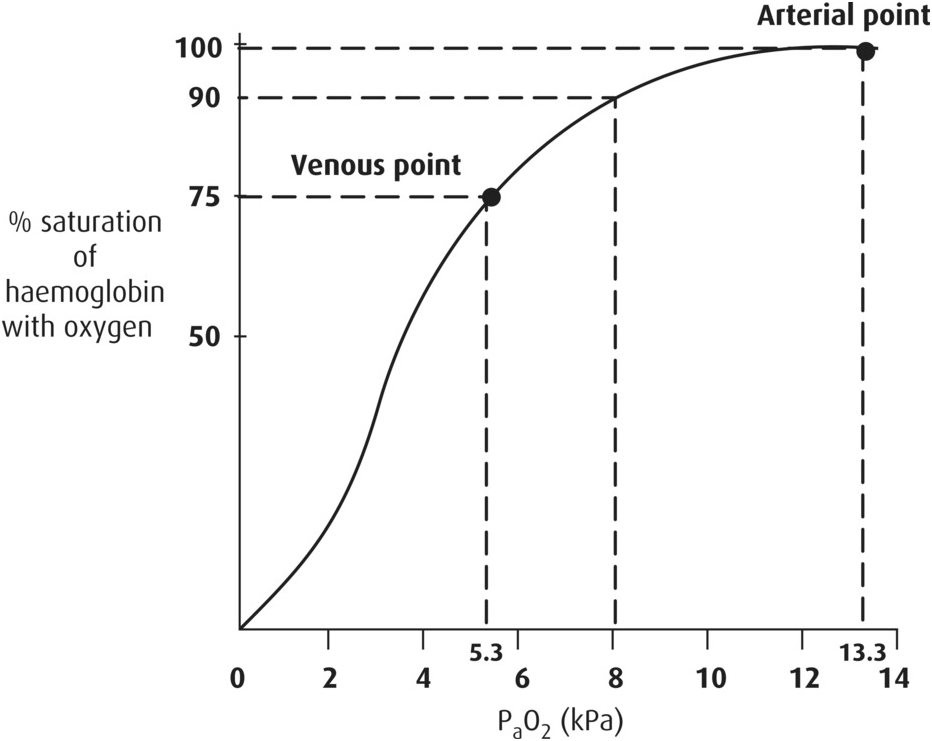
Figure 2.10 The oxygen–haemoglobin dissociation curve. The shape of the oxygen–haemoglobin dissociation curve indicates that the oxygen saturation of blood decreases rapidly below 92%; therefore, when the oxygen saturation displayed on the pulse oximeter decreases to 92%, corrective action is required, and the patient should be reoxygenated immediately.
Arterial blood gas analysis
The analysis of an arterial blood gas sample is essential for assessing the adequacy of oxygenation and ventilation. Information on the interpretation of arterial blood gases can be found in the further reading section.
Pre-oxygenation
Effective pre-oxygenation enables several minutes of apnoea without desaturation of arterial blood, during which tracheal intubation can be achieved. An oxygen reservoir is developed by replacing air (nitrogen) in the lungs (the functional residual capacity) with oxygen, and saturating the blood and tissues. One of the most efficient ways of achieving this is by giving 100% oxygen via a Mapleson C breathing system. A bag-mask device is a less suitable alternative because of the resistance to inspiratory and expiratory flow, and the inability to deliver 100% oxygen. An oxygen mask with a properly functioning reservoir bag delivers approximately 80% oxygen and is an alternative, although less effective, method if an anaesthetic breathing system is not immediately available, or the patient will not tolerate a well-fitting facemask. The efficiency of pre-oxygenation can be further optimized by the use of CPAP, which may be delivered by adjusting the APL valve of the Mapleson C system. This may be of particular benefit for patients with severe lung disease, where use of high-flow continuous positive airway pressure (CPAP) for pre-oxygenation will enable the highest possible arterial blood oxygen saturation to be achieved.
The time for arterial blood to desaturate is related to the effectiveness of the pre-oxygenation phase, the age and weight of the patient, and the patient’s physiological status. In a healthy adult following effective pre-oxygenation, the time for arterial blood to desaturate to 92% may be as long as eight minutes; for a child, this is reduced to four minutes. All these times are reduced in an ill patient, who is usually unable to achieve full pre-oxygenation, especially if ventilation is inadequate (Figure 2.11). Once the saturation reaches 92%, the rate of desaturation accelerates because of the shape of the oxyhaemoglobin dissociation curve (Figure 2.10).
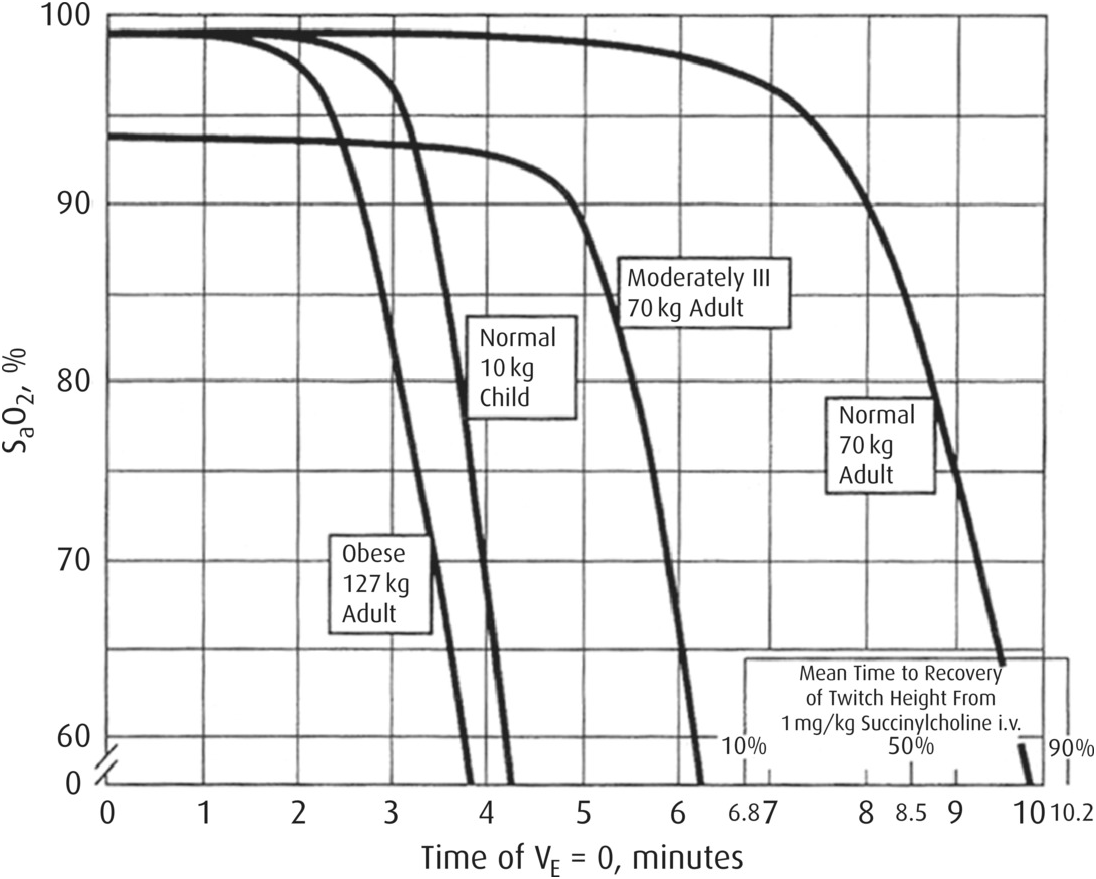
Figure 2.11 Time to desaturation according to a range of patient characteristics. Time to haemoglobin desaturation with initial FAO2=0.87 for various patient circumstances. Note the bars indicating recovery from succinylcholine paralysis at the bottom right of the graph. (From Benumof, J., Dagg, R., Benumof, R. (1997) Critical hemoglobin desaturation will occur before return to an unparalyzed state following 1 mg kg–1 intravenous succinylcholine. Anesthesiology; 87: 979–82, with permission.)
Summary
The commonest causes of hypoxaemia are hypoventilation and ventilation/perfusion mismatch, both of which can be managed initially by increasing the inspired oxygen concentration.
Target oxygen therapy according to the patient’s needs and prescribe appropriately.
A variety of devices are available to deliver oxygen in patients breathing spontaneously or requiring assisted ventilation.
The pulse oximeter provides a useful indication of arterial oxygenation, but not the adequacy of ventilation.
Pre-oxygenation is an important step in preparing for rapid sequence induction, and is achieved best by using an anaesthetic breathing system or, in some cases, CPAP.