Introduction
Caregiving of children diagnosed with autism spectrum disorder (ASD) is challenging due to the heterogeneous and chronic nature of autism, and broad range of possible co-occurring conditions (Vohra et al., Reference Vohra, Madhavan, Sambamoorthi and St Peter2014). Lack of the child's communication and socialization skills, low ability for self-caring in daily routines, and societal barriers such as inadequate school system services to address needs and lack of other support resources may challenge families raising a child with ASD (Ho et al., Reference Ho, Fergus and Perry2018). Due to the multifaceted nature of the disorder and lack of evidence-based treatment options, parents of autistic children are in a persistent search for services from multiple sources and specialists to address the needs of their children (An et al., Reference An, Kanderzhanova, Akhmetova, Foster and Chan2020; Srinivasan et al., Reference Srinivasan, Ekbladh, Freedman and Bhat2021).
Population-based studies from the US showed that despite greater utilization of services, caregivers of children with ASD were more likely to report difficulties in accessing child healthcare services and have more unmet family support needs as compared to caregivers of children with other developmental disabilities or typically developing children (Vohra et al., Reference Vohra, Madhavan, Sambamoorthi and St Peter2014; Srinivasan et al., Reference Srinivasan, Ekbladh, Freedman and Bhat2021). Previous research from low and middle-income countries on children with ASD found challenges related to primary caregivers' needs for family support, accessibility for services and well-trained specialists, public awareness and understanding of autism, inclusive education system and social acceptance of children with ASD (Bilgin and Kucuk, Reference Bilgin and Kucuk2010; Divan et al., Reference Divan, Vajaratkar, Desai, Strik-Lievers and Patel2012; Tilahun et al., Reference Tilahun, Hanlon, Fekadu, Tekola, Baheretibeb and Hoekstra2016; Gobrial, Reference Gobrial2018; Shorey et al., Reference Shorey, Ng, Haugan and Law2020). Emotional burden on parents due to the child's disorder and parental mental health were identified as unmet needs by studies conducted in both high and lower resourced settings (Divan et al., Reference Divan, Vajaratkar, Desai, Strik-Lievers and Patel2012; Lushin and O'Brien, Reference Lushin and O'Brien2016; Tilahun et al., Reference Tilahun, Hanlon, Fekadu, Tekola, Baheretibeb and Hoekstra2016; Papadopoulos, Reference Papadopoulos2021).
Extensive research has found that parents of children with ASD often experience elevated levels of stress, depression and anxiety, as compared to parents of typically developing children (Hodge et al., Reference Hodge, Hoffman and Sweeney2011; Bitsika et al., Reference Bitsika, Sharpley and Bell2013; Wang et al., Reference Wang, Hu, Wang, Qin, Xia, Sun, Wu and Wang2013; Lai et al., Reference Lai, Goh, Oei and Sung2015; Al-Farsi et al., Reference Al-Farsi, Al-Farsi, Al-Sharbati and Al-Adawi2016; Padden and James, Reference Padden and James2017). Though the majority of studies investigating parental stress due to having a child with ASD were conducted in Western or European contexts (Hayes and Watson, Reference Hayes and Watson2013; Barroso et al., Reference Barroso, Mendez, Graziano and Bagner2018), similar findings from systematic reviews of studies in Southeast Asia (Ilias et al., Reference Ilias, Cornish, Kummar, Park and Golden2018) and Arab countries (Alkhateeb et al., Reference Alkhateeb, Hadidi and Mounzer2022) also show increased stress levels for parents and other adverse impacts on their mental health.
Kazakhstan is a post-Soviet upper-middle income country located in Central Asia (World Bank, 2022). With a total population of 19 million, children aged from 0 to 17 years constitute about 32% of Kazakhstani population (Bureau of National Statistics Agency for Strategic Planning and Reform, Republic of Kazakhstan, 2022). Officially the estimated prevalence of ASD is 2.6 per 100 000 children in Kazakhstan (Perfilyeva et al., Reference Perfilyeva, Bespalova, Skvortsova, Surdeanu, Garshin, Perfilyeva, Khamdiyeva, Bekmanov and Djansugurova2019), which is lower than prevalence found in most countries worldwide. The low rates of diagnosis have been linked to gaps in medical training and lack of expertise among professionals (Somerton et al., Reference Somerton, Stolyarova and Khanin2022) and low public awareness and social stigma attached to ASD in Kazakhstan (An et al., Reference An, Chan and Kaukenova2018, Reference An, Kanderzhanova, Akhmetova, Foster and Chan2020). Public services for children with autism in Kazakhstan are in the early stages of gradual development. During the last two decades, governmental regulations were introduced to increase detection, treatment, and provision of social services for children with special needs (An et al., Reference An, Chan and Kaukenova2018). Recently, the government of Kazakhstan introduced a road map for advancing healthcare provisions for ASD children for 2019–2020, committing to improve the quality of life of both children with autism and their families through early diagnosis, rehabilitation, inclusive education and social integration (An et al., Reference An, Kanderzhanova, Akhmetova, Foster and Chan2020). Educational and recreational facilities, and community-based non-profit organizations have shaped most of the infrastructure for care provisions for autistic children (An et al., Reference An, Chan and Kaukenova2018; Somerton et al., Reference Somerton, Stolyarova and Khanin2022). In recent years a substantial upsurge in the number of registered children with autism has been observed, increasing from 77 in 2003 to approximately 2000 in 2007 (An et al., Reference An, Chan and Kaukenova2018; National Centre for Correctional Pedagogy), and to nearly 4887 in 2021 (Republican Scientific and Practical Center for Mental Health, reported by national media). Despite this apparent upsurge in numbers, there has been a sparsity of research in autism in Kazakhstan. To the authors' knowledge, limited qualitative and mixed-methods studies have explored the experiences of parents raising a child with ASD (An et al., Reference An, Chan and Kaukenova2018, Reference An, Kanderzhanova, Akhmetova, Foster and Chan2020) and knowledge and beliefs of health specialists involved in diagnosis of children with autism (Somerton et al., Reference Somerton, Stolyarova and Khanin2022). The qualitative study by An et al. (Reference An, Chan and Kaukenova2018), investigating parental perspectives on support and services for children with autism in Kazakhstan, found challenges and unmet needs related to early diagnosis, and availability of trained specialists, financial support, multidisciplinary team of specialists, inclusive education, and acceptance of autistic children by society. However, the mental health of parents with autistic children was not directly addressed.
Increased caregiver stress or depression has been shown to decrease parenting abilities (Cummings and Davis, Reference Cummings and Davies1994), which can in turn negatively impact the child's physical and mental health (Olfson et al., Reference Olfson, Marcus, Druss, Alan Pincus and Weissman2003; Lushin and O'Brien, Reference Lushin and O'Brien2016). Researchers found that parenting stress was inversely associated with successful outcomes of early learning processes of autistic children (Osborne et al., Reference Osborne, McHugh, Saunders and Reed2008) and was strongly directly associated with the development of depressive symptoms and deterioration of the quality of life in parents of children with high-functioning pervasive developmental disorders (Suzumura, Reference Suzumura2015). A large-scale cohort study conducted by Fairthorne et al. (Reference Fairthorne, Hammond, Bourke, Jacoby and Leonard2014) showed that caregivers of children with ASD had higher risk of death and experienced substantially poorer survivorship.
Factors related to the child with ASD and parents, and social level factors were found to be predictors of the psychological burden for caregivers of children with ASD. Increased severity of autism symptoms (Ekas and Whitman, Reference Ekas and Whitman2010; Picardi et al., Reference Picardi, Gigantesco, Tarolla, Stoppioni, Cerbo, Cremonte, Alessandri, Lega and Nardocci2018), number of co-occurring conditions (Zablotsky et al., Reference Zablotsky, Bradshaw and Stuart2013) and children's emotional and behavioral problems (Estes et al., Reference Estes, Olson, Sullivan, Greenson, Winter, Dawson and Munson2013; Falk et al., Reference Falk, Norris and Quinn2014; Zhou et al., Reference Zhou, Liu, Xiong and Xu2019) were found to be predictors of stress, anxiety and depression among caregivers of children with ASD. Parental perceived limit-setting ability, satisfaction with parenting, mothers' age (Falk et al., Reference Falk, Norris and Quinn2014), self-stigma (Werner and Shulman, Reference Werner and Shulman2013; Chan and Lam, Reference Chan and Lam2018) and poor coping strategies (Whitehead et al., Reference Whitehead, Dorstyn and Ward2015) were also found to be associated with depression among parents. Father's age (Falk et al., Reference Falk, Norris and Quinn2014) and financial strain were predictors of higher parental stress levels (Zablotsky et al., Reference Zablotsky, Bradshaw and Stuart2013; Falk et al., Reference Falk, Norris and Quinn2014; Ilias et al., Reference Ilias, Cornish, Kummar, Park and Golden2018). Poor quality interactions within the extended family and absence of children's schooling were also associated with higher parental stress (Derguy et al., Reference Derguy, M'Bailara, Michel, Roux and Bouvard2016). Public stigma due to autism was associated with depression and anxiety (Gray, Reference Gray2002; Chan and Lam, Reference Chan and Lam2017).
Some studies found that not all caregivers of children with ASD experience increased stress levels and elevated depression and anxiety symptoms. Some families display traits of resilience, such as family hardiness, which was inversely associated with depression (Weiss, Reference Weiss2002). Perceived social support (Ekas et al., Reference Ekas, Lickenbrock and Whitman2010; Weiss et al., Reference Weiss, Robinson, Fung, Tint, Chalmers and Lunsky2013; Zablotsky et al., Reference Zablotsky, Bradshaw and Stuart2013; Whitehead et al., Reference Whitehead, Dorstyn and Ward2015; Drogomyretska et al., Reference Drogomyretska, Fox and Colbert2020), psychological resilience (Bitsika et al., Reference Bitsika, Sharpley and Bell2013), religious beliefs (Ilias et al., Reference Ilias, Cornish, Kummar, Park and Golden2018), effective coping skills (Zablotsky et al., Reference Zablotsky, Bradshaw and Stuart2013) and participation in parental support groups (Kerr and McIntosh, Reference Kerr and McIntosh2000) may play a role in protecting parental mental health and wellbeing of caregivers of autistic children.
While a considerable amount of research investigates risk factors for psychological distress among caregivers of children with ASD, the focus of research on the experiences of parents in the upper-middle income Central Asian country of Kazakhstan is lacking. Furthermore, though a large part of previous research has globally shown that parent and autistic child demographics and behavioral characteristics are associated with psychological distress among caregivers of children with autism, a sparsity of studies have investigated the impact of caregivers' unmet needs on psychological burden. Our study addresses this gap by introducing a more comprehensive list of potential risk and protective factors for the evaluation of their associations with psychological distress.
The aims of our study were to (1) determine the prevalence of stress, anxiety, and depressive symptoms among parents of children with ASD, and to (2) examine the associations of a more comprehensive range of potential risk and protective factors associated with these outcomes, including sociodemographic characteristics of parents and autistic children, unmet needs of social support and acceptance by society, financial support, and use of various treatment and behavioral interventions. Findings of our study will provide insights into factors associated with psychological distress in parents of autistic children in the Central Asian region, an under-researched area. Findings of this study can provide a foundation to raise public awareness of the unmet psychological needs of parents raising children with ASD, and provide evidence to inform the planning of more effective policy and family focused interventions.
Methods
Study setting and sample
Our study participants consisted of 146 parents of autistic children. Recruitment of study participants to this cross-sectional survey was conducted by convenience sampling from various places in Astana city, the capital of Kazakhstan, at the awareness-raising event on the International Autism Day, the Public Association of Parents of Children with Autism ‘ORDA’, and the National Children's Rehabilitation Center, which provides services for children with ASD countrywide. Data collection was conducted during the months April to December 2018. Participants met the following inclusion criteria: parents having at least one autistic child and could communicate in Russian or Kazakh language(s). All participants were asked for an oral consent and were not asked to sign a written informed consent form, due a reluctance to sign forms as a result of the legacy of the Soviet Union. An information letter as part of the oral consent process was provided to communicate objectives, risks and benefits with participation in this study, as well as covering the rights of participants and responsibilities of the researcher. After providing oral informed consent, parents completed an anonymous paper-based survey. This survey was administered to participants who provided consent at convenient private spaces at the ‘ORDA’ Center and at the National Children's Rehabilitation Center. The study was approved by the Ethical Committee of the Corporate Fund ‘University Medical Center’ (IRB №: 6/04092018).
Instruments
The parent self-administered survey comprised of 59 questions inquiring about the sociodemographic characteristics of parents and their autistic children, parental needs with regards to autism care, membership in parental support groups, and two standardized scales to assess parental mental health and perceived social support.
The survey was administered in two languages, Kazakh and Russian. The original English version of the standardized scales were translated into Kazakh language by our multilingual research team members, and were culturally adapted to ensure validity and reliability of the tool, following the guidelines for cross-cultural adaptation of self-report measures (Beaton et al., Reference Beaton, Bombardier, Guillemin and Ferraz2000). We used a Russian version of the standardized scales that was validated by previous researchers. The survey was pretested and corrected for clarity and understanding among a small sample of parents of autistic children; pre-test surveys were excluded from analysis.
Depression anxiety stress scale (DASS-21)
The DASS-21 is an internationally-validated tool used to assess the mental health of an individual based on negative emotional states of depression, anxiety and stress experience over the past week (Lovibond and Lovibond, Reference Lovibond and Lovibond1995). The DASS is 21-item questionnaire divided into three sub-scales, each containing seven questions. The Depression subscale assesses hopelessness, devaluation of life, self-abasement, lack of interest, and inertia. The Anxiety subscale evaluates panic attacks, skeletal muscle effects, and subjective experience of anxious affect. The Stress subscale assesses levels of chronic difficulty in relaxing, nervous arousal, and being easily upset, irritable and impatient. Each question is measured on a four-point Likert scale ranging from 0 (‘did not apply to me at all’) to 3 (‘applied to me very much’). Overall score is calculated by summing the scores of each emotional state sub-scale, then categorized into none, mild, moderate, severe-and-extremely severe symptoms of depression, anxiety, or stress. The DASS-21 showed good internal reliability in previous studies, with Cronbach's α of 0.835, 0.737 and 0.761 for depression, anxiety and stress subscales in one study (Le et al., Reference Le, Tran, Holton, Nguyen, Wolfe and Fisher2017). For the current study, we translated and culturally adapted the scale in the Kazakh language. We also utilized the Russian version of the DASS-21, which was validated by the National Centre in HIV Epidemiology and Clinical Research in Sydney Australia as part of an international trial (Psychology Foundation of Australia, 2018). In our sample, Cronbach's α for the overall scale was 0.936 and 0.942 for Kazakh and Russian versions, respectively.
Multidimensional Scale of Perceived Social Support
The Multidimensional Scale of Perception of Social Support was developed by Zimet et al., in 1988, with the Russian language version previously being tested in a study by Kuznetsov et al. (Reference Kuznetsov, Pushkarev and Yaroslavskaya2015). The Scale is a short self-report measure that assesses subjective perceptions of social support, which is composed of 12 items rated on a 7-point Likert scale, ranging from 1 for ‘absolutely disagree’ to 7 for ‘absolutely agree’. Based on the pre-test of the questionnaire, for the current study the response scale was reduced up to 5 points to improve the understanding and acceptability of the scale. Thus, the summed total score ranges from 12 to 60, where the higher score indicates more social support. The scale assesses effectiveness and adequacy of social support in three dimensions - ‘family’, ‘friends’, and ‘significant other’. The scale is considered by Zimet et al. (Reference Zimet, Dahlem, Zimet and Farley1988) as a psychometric probe with good reliability (Cronbach's α = 0.88), adequate factor and construct validity, and simple for examination and a time-saving tool. In our sample Cronbach's α was 0.926 and 0.954 for Kazakh and Russian language versions, respectively.
The sociodemographic section of the questionnaire collected information about parental age, gender, education, marital status, number of children, family income, employment status, place of residence, and financial and instrumental care support (10 questions). This section also included questions concerning the autistic child's age, gender, and diagnosis, the specialists who informed parents about ASD for the first time, living arrangements for the child, co-occurring chronic conditions, educational attainment (home-based/caregiver, mixture of classes, regular education classroom, and special educational classroom), and use of various treatment interventions (eight questions).
A question on treatment interventions received in the past year included Applied Behavior Analysis (ABA) therapy, academic classes (sessions with specialists, such as speech therapist and psychologist), occupational therapy, physical therapy (e.g. usage of light, heat, ultrasound, electrical impulses) and social skills interventions. Parents were asked if they participated in parental support organizations (one item). A few open-ended explorative questions about perceived benefits and barriers for participation in support groups were asked additionally.
Parents' perceived needs fulfillment was assessed by seven items, inquiring about early diagnosis, availability of trained specialists, financial support, inclusive education, acceptance by society, support of parental organizations, and multidisciplinary team of specialists. The research team created this measure based on findings of the previous qualitative study by An et al., Reference An, Chan and Kaukenova2018, which identified the most salient unmet needs of parents of autistic children in Kazakhstan. The extent of perceived fulfillment of needs was measured using following scale: ‘fully met’ = 1, ‘partially met’ = 2, ‘unmet’ = 3 and ‘extremely unmet’ = 4. Each item on this scale was analyzed as a separate categorical variable.
Data analysis
Descriptive statistics were calculated to characterize the study sample using percentages for categorical variables, and means and standard deviations for continuous variables. χ2 analysis was performed to test statistical significance of categorical variables, with Fisher's exact test (two-tailed) substituted when assumption of expected small cell size was not met. The differences for continuous independent variables between groups were assessed by the Student's t test, with ANOVA utilized when more than two groups were to be compared. Multivariate linear regression analyses were performed to explore the associations of parental mental health status with independent variables, where three separate models were constructed for depression, anxiety, and stress. Due to limited sample size the p value of 0.25 in bivariate analysis was selected for inclusion of variables into final models, after which backward stepwise selection was performed to determine models. Mean differences and 95% confidence intervals were chosen as measures of association between independent and outcome variables. Statistical significance was set at α = 0.05. All statistical analyses were completed using STATA Software version 15.1.
Results
Socio-demographic and children's illness-related characteristics
Frequency distributions of socio-demographic characteristics of parents and their children with autism, as well as children's illness-related characteristics, are presented in Table 1.
Table 1. Descriptive characteristics of parents and children with autism spectrum disorder (ASD) (n = 146)
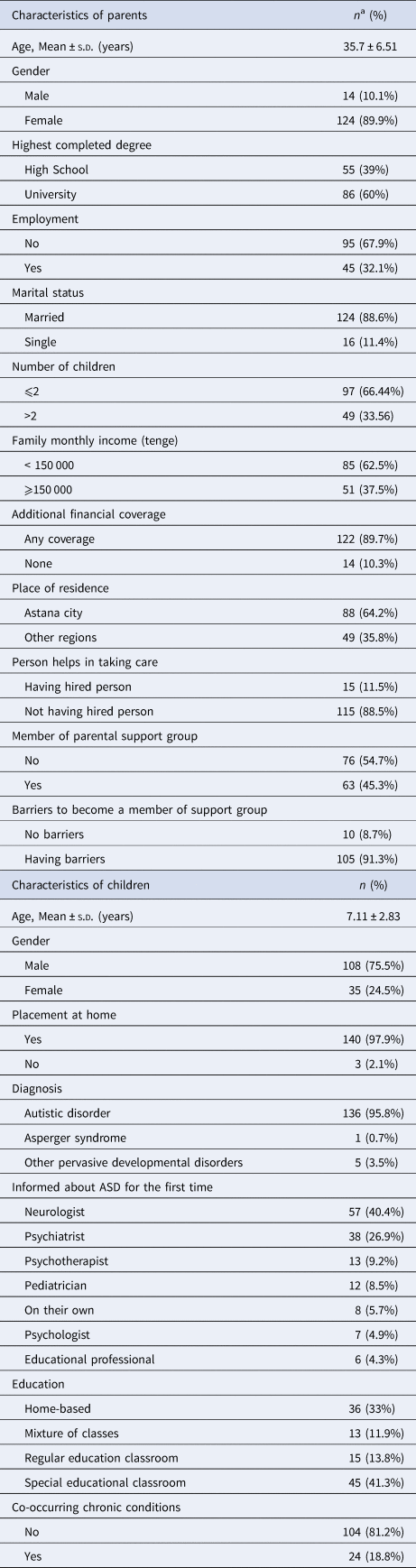
a Total counts and percentages may vary because of missing values.
Women constituted a significant proportion of the respondents (89.9%) with overall mean age of 35.69 years (s.d. ± 6.51). Almost nine-out-of-ten respondents were married (88.6%), and over half of these parents held university degrees (60.0%) and were residents of Astana city (64.2%). Around two thirds of them were not employed (67.9%), with monthly family income of less than 150000 tenge (~ 390 USD, 62.5%).
A total of 75.5% of parents reported that they were raising a boy with autism and that the mean age of their children was 7.11 years (s.d. ± 2.83). A total of 95.8% of respondents indicated that their child has Autistic Disorder, with 3.5% indicating other pervasive developmental disorders (3.5%) and 0.7% indicating Asperger Syndrome. Nearly 19% stated that their child had at least one other co-occurring chronic condition such as epilepsy, allergy, impaired or loss of hearing, and congenital malformation. A total of 40.4% of parents were first informed about their child's diagnosis by a neurologist and 26.9% by a psychiatrist. A total of 95.8% of children with ASD were living at home and 33% stayed at home to receive interventions. A total of 11.9% attending a mixture of classes and the remaining children attended special or regular educational classrooms, 41.3% and 13.8%, respectively.
Membership in support groups, received interventions and needs of parents
A total of 45.3% of respondents were members of support groups for parents with autistic children (Table 1). Out of all respondents, 73.3% indicated that barriers exist that hinder becoming a member of parental support groups, such as lack of information on the support groups and travel distance to support group meetings.
Frequency distributions of treatments and behavioral interventions are provided in Table 4. A majority of children with autistic disorder were engaged in academic classes (82.9%), 39.7% received occupational therapy and 36.3% received social skills interventions. About one quarter (26.0%) of the respondents' children had access to ABA and the same percentage (26.0%) had access to physical therapy. The need for inclusive education was the most frequently reported unmet-or-extremely-unmet need as compared to other needs, accounting for 42.5% and 24.7% of respondents, respectively (Table 5). Approximately a third of caregivers mentioned early diagnosis (31.5%), financial support (31.5%) and acceptance by society (33.3%) as unaddressed needs. While a substantial percentage of respondents identified early diagnosis and acceptance by society as extremely-unmet needs (8.8% and 11.0%, respectively), unmet financial support need was reported by a higher 19.3% of respondents. In addition, comparatively fewer respondents were unsatisfied by the level of availability of trained specialists (24.03%), support from parental organizations (27.59%), and multidisciplinary team of specialists (20.00%). Just over one-tenth of respondents had hired a person to assist in caring for the child with ASD (11.5%). The majority received additional financial coverage for their children's needs and services (89.71%); in most cases, these were governmental pension and governmental special social service funds.
Stress, anxiety and depression: prevalence and associations
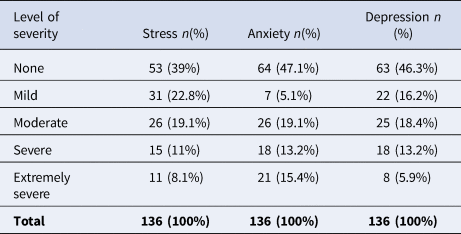
A total of 136 complete responses were analyzed to calculate scores for outcome variables. Overall, the combined prevalence for mild to extremely severe levels of stress, anxiety and depression were 61, 52.9, and 53.7%, respectively (Table 2).
Table 2. Stress, anxiety, and depression among parents of children with ASD
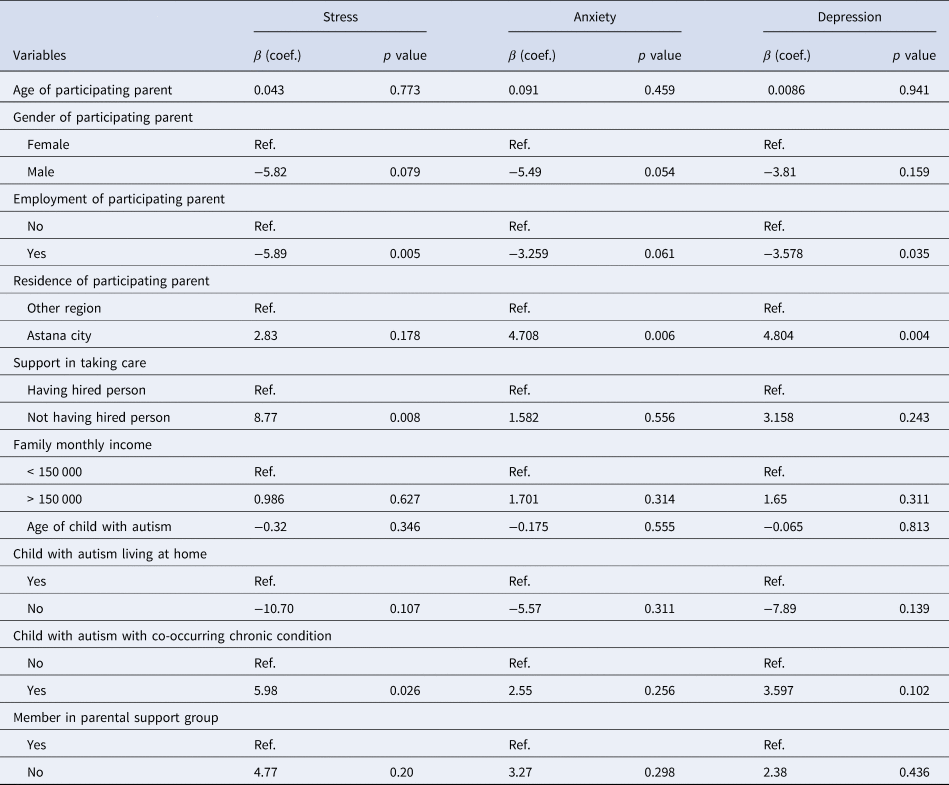
The results of the bivariate analysis using simple linear regression are presented in Table 3. Parents' age, gender, family income and membership in support groups were not associated with either of DASS's outcomes. Employed parents were less stressed and depressed than parents who were unemployed. Parents from Astana city were more anxious and depressed in comparison with their counterparts from other regions. Also, respondents who had not hired a person to assist in caring for their ASD child were found to be more stressed than those who had hired someone (all p values < 0.05). Among children with autism, having co-occurring conditions was associated with a higher level of parental stress.
Table 3. Psychological distress among parents in relation to parental and child's characteristics utilizing bivariate simple linear regression analysis
Parents with children receiving ABA therapy were reported to be more likely to have mood disorders than those who did not receive ABA therapy (Table 4).
Table 4. Parental psychological distress by treatment and behavioral interventions utilizing bivariate simple linear regression analysis
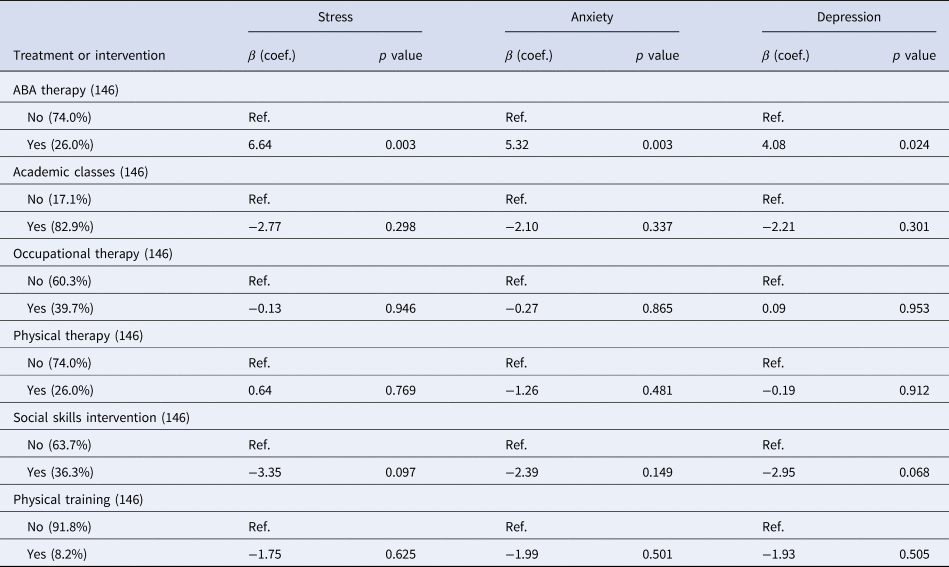
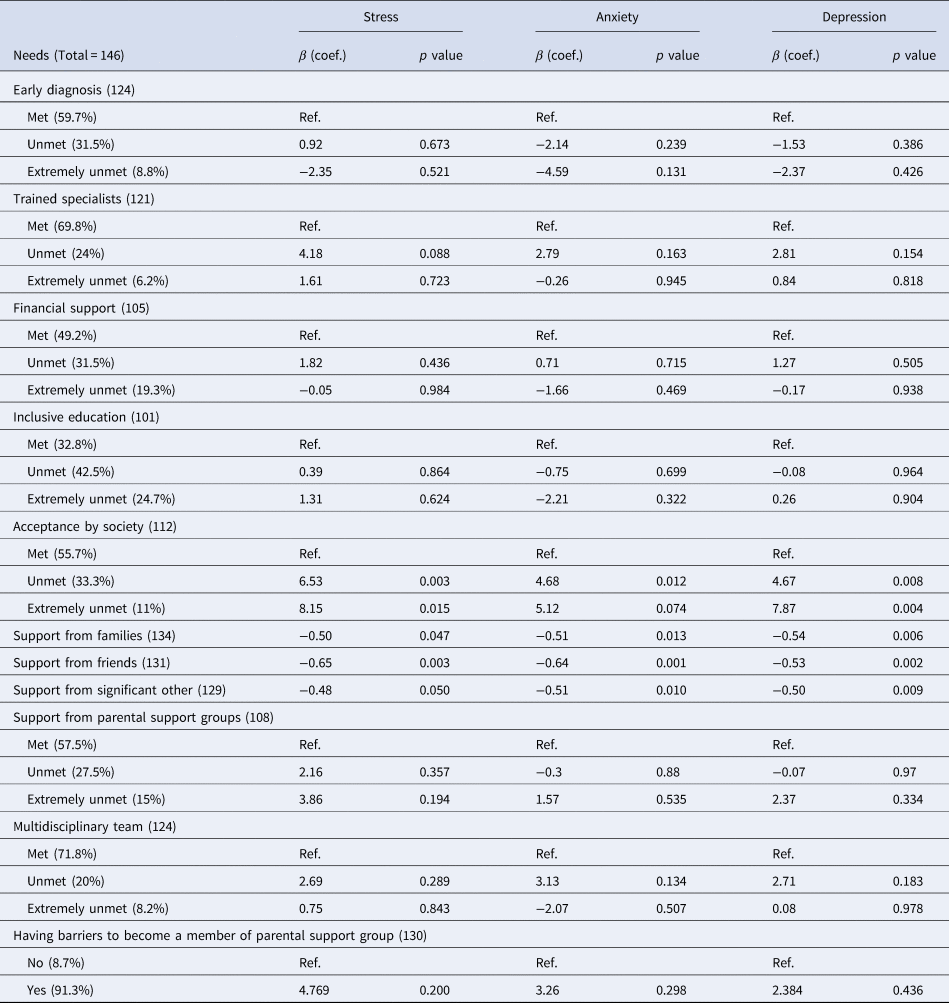
Table 5 shows that those respondents who perceived that acceptance by society was unmet-or-extremely-unmet were more depressed, anxious, and stressed than parents who reported that acceptance by society was satisfactory. The more support parents reported receiving from their family, friends, and significant others, the lower the levels of depression, anxiety, and stress they experienced.
Table 5. Parental psychological distress by perceived fulfillment of needs utilizing bivariate simple linear regression analysis
Multivariate linear regression analysis
For each of the DASS's outcomes (depression, anxiety and stress), a separate linear regression model was generated. Three variables, employment of participating parent, support of friends, acceptance by society, were statistically significantly associated with at least one outcome variable (Table 6).
Table 6. Factors associated with parental psychological distress utilizing multivariate linear regression analysis
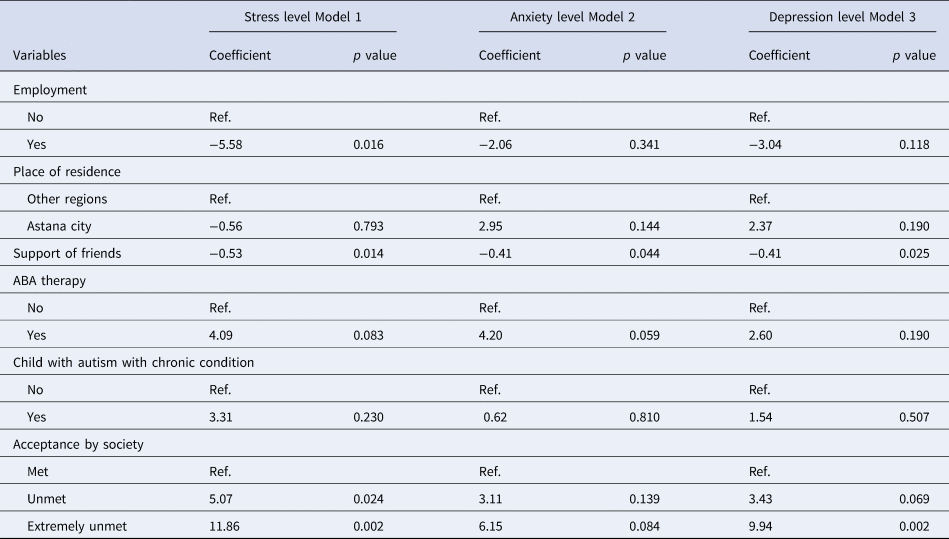
The strongest association with stress was observed for perceived level of acceptance by society; parents reporting level of acceptance by society as an extremely-unmet need were more stressed than those reporting this need as adequately met (mean difference 11.86, p value 0.002). Similarly, there was also a strong association for extremely-unmet need of acceptance by society with depression (mean difference 9.94, p value 0.002). Also, employed parents had lower stress levels than unemployed respondents. A higher level of perceived friends' support was found to be associated with lower levels of stress, anxiety and depression (coefficients: −0.53 for stress, −0.41 for anxiety and depression with p-values 0.014, 0.044 and 0.025, respectively). Additional analysis in our study found that children who received ABA therapy were more likely to have chronic conditions; in the final multivariate analysis that including confounders parent's employment status and social support, ABA was no longer associated with parental stress and mood disorders.
Discussion
To our knowledge this cross-sectional survey, utilizing internationally validated scales, is the first study conducted in a post-Soviet Central Asian country to investigate a wide range of potential risk and protective factors associated with mental health problems in parents of children with autism. Our findings showed that symptoms of depression, anxiety and stress are common among parent caregivers of children with ASD. Perceived lack of social acceptance was the most significant factor contributing to psychological distress of parents, while friends' social support and employment status were found to be protective factors for parental mental health wellbeing in families caring for children with autism.
Clinically significant depressive symptoms were reported by 37.5% of caregivers of autistic children in our study, which was similar to other findings. A recent meta-analysis by Schnabel et al. (Reference Schnabel, Youssef, Hallford, Hartley, McGillivray, Stewart, Forbes and Austin2020) identified overall prevalence of depressive disorders of 31% among parents of children with ASD, though other individual studies have shown variability in these findings. These disparate findings may be due to differences in the scales utilized, what the scale was measuring, and/or real differences in the socio-cultural contexts of study populations. A large-scale study from the USA conducted by Cohrs and Leslie in Reference Cohrs and Leslie2017, utilizing medical health claims of more than 85000 families, found a much lower prevalence of depression of 12.5%, in contrast to the 37.5% in our study.
We found that parents with moderately-to-extremely severe levels of anxiety symptoms accounted for 47.8% of all respondents, and a total of 38.2% had symptoms of stress. While our findings are similar to the findings of the study from Oman by Al-Farsi et al. (Reference Al-Farsi, Al-Farsi, Al-Sharbati and Al-Adawi2016) for anxiety (45.9%), there is some difference from our study in their prevalence measure of stress symptoms, with 46%. The Davis and Carter study (Reference Davis and Carter2008) conducted in the US utilizing the Beck Anxiety Inventory found a prevalence of 12% among parents having anxiety symptoms, contrasting with our 47.8% using the DASS-21 instrument. The prevalence of anxiety in our study population is also higher than the 33% found in a meta-analysis consisting of papers with self-reported measures (Schnabel et al., Reference Schnabel, Youssef, Hallford, Hartley, McGillivray, Stewart, Forbes and Austin2020).
Employment status of participants in our sample, mostly comprised of mothers, was associated with reduced levels of stress, similar to findings of a study from Australia by Einam and Cuskelly (Reference Einam and Cuskelly2002), which showed that the number of hours of paid employment was inversely associated with reported psychological problems in mothers of young adults with multiple disabilities. Studies have found that maternal employment positively impacts mood, feelings of accomplishment, and a positive sense of identity (McCabe, Reference McCabe2010). Our findings provide further evidence that mothers' employment may be protective for mothers of children with developmental disabilities by increasing their social network, as suggested by previous findings (Einam and Cuskelly, Reference Einam and Cuskelly2002).
Our findings showed that parents of children with autism and other impairments who were participating in ABA therapy were no longer at increased risks for stress and mood disorders after controlling for the effects of parent's employment status and level of perceived social support from friends and society; these factors confounding the risks. Our findings were consistent with those of the study by Hastings and Johnson (Reference Hastings and Johnson2001), which found that parents involved in intensive home-based behavioral intervention for their young child with autism reported no difference in stress levels from that of other parents of children with autism. Only a few studies have considered the impact of ABA intensity on parents. Contrary to our findings, previous studies by Schwichtenberg and Poehlmann (Reference Schwichtenberg and Poehlmann2007) and Eikeseth et al. (Reference Eikeseth, Klintwall, Hayward and Gale2015) showed that mothers of children participating in ABA intervention reported elevated depressive symptoms, and those mothers who were more involved in their child's ABA program reported more personal strain. The intense requisites that ABA programs place on children and families were hypothesized to explain these findings. Further research is needed to address these inconsistencies.
A substantial number of previous studies showed protective effects of informal social support for parents' mental well-being in families of children with disabilities (Weiss, Reference Weiss2002; Zaidman-Zait et al., Reference Zaidman-Zait, Mirenda, Duku, Vaillancourt, Smith, Szatmari, Bryson, Fombonne, Volden, Waddell, Zwaigenbaum, Georgiades, Bennett, Elsabaggh and Thompson2017; Picardi et al., Reference Picardi, Gigantesco, Tarolla, Stoppioni, Cerbo, Cremonte, Alessandri, Lega and Nardocci2018). Our findings additionally showed that among different types of informal support, friends' support was more effective in helping parents of autistic children cope with stress and psychological disorders, similar to findings of previous studies (Ekas et al., Reference Ekas, Lickenbrock and Whitman2010; Drogomyretska et al., Reference Drogomyretska, Fox and Colbert2020). Informal social network applications, mostly WhatsApp, were reported as the main source of social, informational and emotional support for parents of children with ASD in Kazakhstan in a previous study by An et al. (Reference An, Chan and Kaukenova2018). There is a strong sense of camaraderie and solidarity among these parents, and many of them have become close friends. The strong stress-buffering effect of friends' social support for parents of children with ASD found in our study might be channeled in part through these parental informal social networks.
Study findings showed that parents who reported social acceptance as unmet-or-extremely-unmet needs had significantly higher levels of stress, anxiety, and depression symptoms, as compared to those who reported social acceptance as adequately met. Our findings are consistent with those of a systematic review by Papadopoulos et al. (Reference Papadopoulos, Lodder, Constantinou and Randhawa2019), which found that autism-related stigma, including public stigma and internalized stigma, negatively impact informal caregivers' mental health, including depression, anxiety, and psychological distress. Findings of previous studies suggest that the adverse impact of autism stigma upon caregiver mental health generally declines over time because parents form new trusted friends who accept their child's disability (Gray, Reference Gray2002; Divan et al., Reference Divan, Vajaratkar, Desai, Strik-Lievers and Patel2012; Papadopoulos et al., Reference Papadopoulos, Lodder, Constantinou and Randhawa2019). Positive meaning of caregiving, self-esteem, social support and caregiver burden acted as a buffer against the negative influence of stigma on caregiver well-being (Werner and Shulman, Reference Werner and Shulman2013). Families with children with ASD in Kazakhstan reported experiences of social rejection and stigma linked to autism in their community, in the mainstream health care, and in the educational systems (An et al., Reference An, Chan and Kaukenova2018). Interventions are needed to increase parental social support networks that can buffer the adverse impacts of stigma on caregivers' mental health. Awareness-raising activities that target the general public and parents themselves are vital to combating stigma and improving psychological wellbeing of parents and the entire family of children with ASD.
Strengths and limitations
The major strength of this study is that it examined a wide range of risk and protective factors associated with stress, anxiety, and depressive symptoms in parents of children with ASD in the context of a region of the world with limited research in this field. Several limitations should be considered when reviewing this study. Firstly, we utilized a cross-sectional study design which prevents us from drawing inferences about causality. Secondly, choosing a self-reported research instrument may be somewhat less valid that a clinical diagnosis. However, the internationally-validated widely-used standardized DASS that we utilized has been validated using clinical diagnosis as the gold standard and provides a comprehensive overview of the psychological burden among caregivers of children with ASD, including an assessment of severity of symptoms. Third, we did not control for the effect of severity of the autistic child's symptoms; however, in previous studies, indicators of parental cognition and social support were found to be more important predictors of parental mental health than child-centric variables (Falk et al., Reference Falk, Norris and Quinn2014). Fourth, a relatively small sample size could decrease the power of the study to reveal significant differences between groups. Finally, since the majority of participants were from urban areas, the generalizability of findings to a rural population is limited.
We recommend further studies to characterizing the psychological burden of parents by gender to inform the planning of more effective targeted interventions for improving the mental health of parents caring for autistic children. A longitudinal study design would help in understanding how the associations of social support acceptance with parental mental health changes over time, and whether social support provides short-term and/or long-term benefits. In addition, there is a sparsity of studies on the associations of rural v. urban residence and other culture-specific factors with autism stigma and the mental health of caregivers. We just conducted our study prior to the COVID-19 pandemic. Follow-up studies are recommended to examine how social isolation and further lack of services due to the pandemic has impacted the already distressed families caring for children with ASD. This may provide compelling evidence for planning future interventions aimed to improve the mental wellbeing and health outcomes of these families.
Conclusion
This study highlights the concern that caregivers of children with autism predominantly from urban households are observed to be more vulnerable to stress, anxiety, and depression symptoms. Given the evidence that parental stress has an impact on the effectiveness of interventions for children with autism, a more holistic parent-centric approach is needed, which includes further psychological support for parents to reach favorable outcomes for interventions providing parenting-skills training. Significant findings in terms of risk factors associated with parental mood disorders, such as the lack of social acceptance and stigmatization highlighted the vital importance of awareness raising activities in the context of post-Soviet countries with emerging and fragmentary care provisions for children with ASD and their families. Increased attention needs to be given to the employment opportunities of parents of children with ASD and development of social support networks that can play a protective role for caregivers' mental health and well-being of the entire family.
Acknowledgements
The authors would like to acknowledge the Nazarbayev University School of Medicine for the administrative support in implementing this project. We are grateful to Mrs. Saltanat Esmagambetova, Chair of Public Union ‘ORDA’ for Parents of Children with Autism, for her great support with data collection and interpretation of study findings. We would like also to thank all study participants, mothers and fathers of children with autistic spectrum disorders, who made this project possible.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.









