1. Introduction
In the United States, attention-deficit/hyperactivity disorder (ADHD) is the most prevalent neurobehavioral disorder, affecting 5%–10% of children (American Psychiatric Association, 2013; Child and Adolescent Health Measurement Initiative, 2016; Thomas et al., Reference Thomas, Sanders, Doust, Beller and Glasziou2015). Available clinical practice guidelines state that impairment must be demonstrated in two or more settings (typically, home and school) to diagnose ADHD, and that patient response to treatment should be longitudinally assessed in these settings (American Academy of Pediatrics, 2000; Perrin et al., Reference Perrin, Stein, Amler, Blondis, Feldman, Meyer, Shaywitz and Wolraich2001). Treatment options include behavioral interventions, pharmacotherapy, or their combination (Austerman, Reference Austerman2015), but nearly half of ADHD patients fail to adhere to treatment guidelines (Ferrin & Taylor, Reference Ferrin and Taylor2011). The most common reasons for treatment discontinuation are adverse effects, suboptimal response, and poor adherence (Gajria et al., Reference Gajria, Lu, Sikirica, Greven, Zhong, Qin and Xie2014). Critically, families of children with ADHD may fail to follow up with physicians after initiating treatment, precluding assessment of children’s response to therapy (Epstein et al., Reference Epstein, Langberg, Lichtenstein, Mainwaring, Luzader and Stark2008).
The National Institute for Children’s Health Quality Vanderbilt Assessment Scales provide a validated tool for clinicians to evaluate the current degree of ADHD symptom control to guide treatment plans. At our outpatient pediatric clinic, we identified concern about return rates of Vanderbilt assessments, limiting adequate monitoring of symptoms. In response, we implemented the Parent and Teacher Vanderbilt Agreement, which required parents to bring completed Vanderbilt rating scales to every appointment. We retrospectively investigated adherence to this policy, measured by return rates of Parent and Teacher Vanderbilt ADHD Assessments at clinic visits. Our secondary aims were to analyze the impact of the Parent and Teacher Vanderbilt Agreement policy on appointment rescheduling and ADHD symptom control.
2. Methods
The study was approved by the local Institutional Review with a waiver of consent, and was conducted in compliance with the Helsinki Declaration of 1975, as revised in 2008. The pediatric outpatient clinic at our center is part of an academic health system serving a rural region in the Southeastern United States. We retrospectively reviewed records of patients 5–18 years old who had an ADHD visit at the pediatric outpatient clinic in 2017 and 2018 and had a diagnosis of ADHD (International Classification of Diseases, 10th revision code F90). The intervention consisted of a written agreement between the ADHD Nurse Specialist and the patient’s parents or guardians to return forms at scheduled visits.
Visits were scheduled monthly for a new diagnosis or medication dose change and otherwise every 3 months. Paper copies of assessment forms were provided to caregivers at clinic visits. The agreement was introduced by the nurse when patients were first seen for ADHD or returned for follow-up visits. The agreement stated that medication would only be provided with return of Vanderbilt forms, and was initially implemented in August 2017. When parents did not return forms in violation of the agreement, enforcement was at the discretion of the physician. Typically, physicians prescribed medication for 1–2 weeks with the expectation of the patient returning forms at a scheduled follow-up. We included patients whose caregivers signed the Parent and Teacher Vanderbilt Agreement before February 1, 2018.
Outcomes were assessed 1 year before the agreement was signed, and 1 year after the agreement date. The primary outcome was return of Vanderbilt ADHD Diagnostic Parent and Teacher Rating Scale Assessment (any forms returned before and after policy implementation, and the number of forms returned in each period). The secondary outcomes were Vanderbilt ADHD Diagnostic Parent and Teacher Rating Scale Assessment scores and appointment adherence (canceled appointments, no-show appointments, and appointments where the patient left without being seen). Additional patient characteristics (gender, age, and type of medical insurance) were assessed at the earliest clinic visit during the review period.
Data were summarized using counts with percentages for categorical variables, and medians with interquartile ranges (IQRs) for continuous variables. Vanderbilt form return for each patient was dichotomized as none versus any forms returned before and after the agreement was signed, and compared using McNemar tests of paired proportions. Additional analyses compared the number of forms returned in each period using nonparametric signed-rank tests, and compared the proportion of patients with any missed appointments in each period using a McNemar test. Vanderbilt assessment scores for each domain (inattention, hyperactivity, and performance) were analyzed using fixed-effects linear regression, which controlled for all time-invariant patient characteristics, and accounted for the potential that each patient contributed multiple observations before and after policy implementation. Data analysis was performed in Stata/IC 15.1 (StataCorp, LP, College Station, TX), and p < .05 was considered statistically significant.
3. Results
The analysis included 145 boys and 47 girls; the median age was 10 years (IQR: 8, 12), and the majority of the sample (70%) were non-Hispanic Black, compared to 20% non-Hispanic White and 10% other race/ethnicity. Ninety-three percent of patients had Medicaid insurance. For included patients, we identified 552 visits in the pre-intervention period (of which 36% had returned parent assessment forms and 78% had returned teacher assessment forms), and 689 visits in the post-intervention period (of which 40% had returned parent assessment forms and 83% had returned teacher assessment forms). At the patient level, the number of Vanderbilt assessment forms returned before and after the policy was implemented is summarized in Table 1. After policy implementation, approximately two-third of families returned any parent assessment forms, and approximately three-quarters returned any teacher assessment forms. However, on McNemar tests of paired proportions, we found no statistically significant increase in the likelihood of returning either parent or teacher assessments (p = .185 and p = .225, respectively).
Table 1. Number of returned Vanderbilt assessment forms (N = 195 patients)
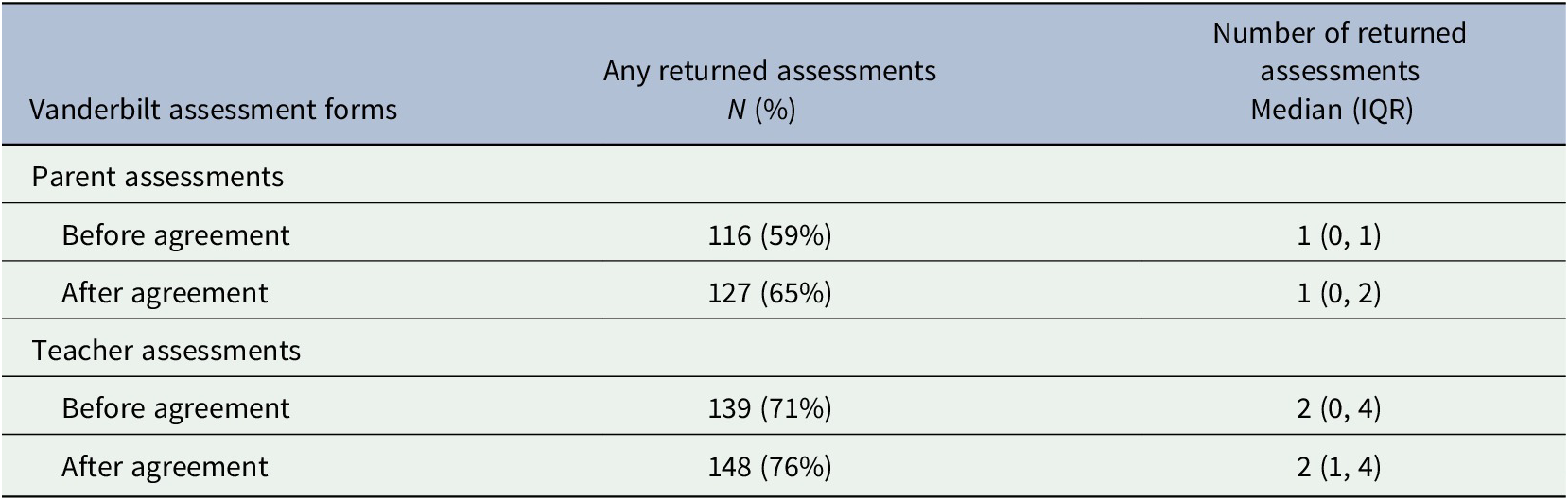
Abbreviation: IQR, interquartile range.
When comparing the total number of forms returned for each patient, families tended to return more forms of each type after policy implementation (parent assessments, p = .002; and teacher assessments, p = .004 on signed-rank test). For example, the proportion of families returning at least five teacher assessment forms increased from 11% (n = 22) to 23% (n = 45) after policy implementation (McNemar p < .001). Vanderbilt assessment scores before and after policy implementation are summarized in Table 2, with the statistical significance of the policy effect evaluated using fixed-effects linear regression. The policy did not appear to cause a significant change from baseline assessment scores. Missed appointments were rare both before and after policy implementation (3% and 4%, respectively), and the increase in the proportion of patients with a missed appointment did not reach statistical significance (McNemar p = .549).
Table 2. Vanderbilt assessment scores before and after policy implementation
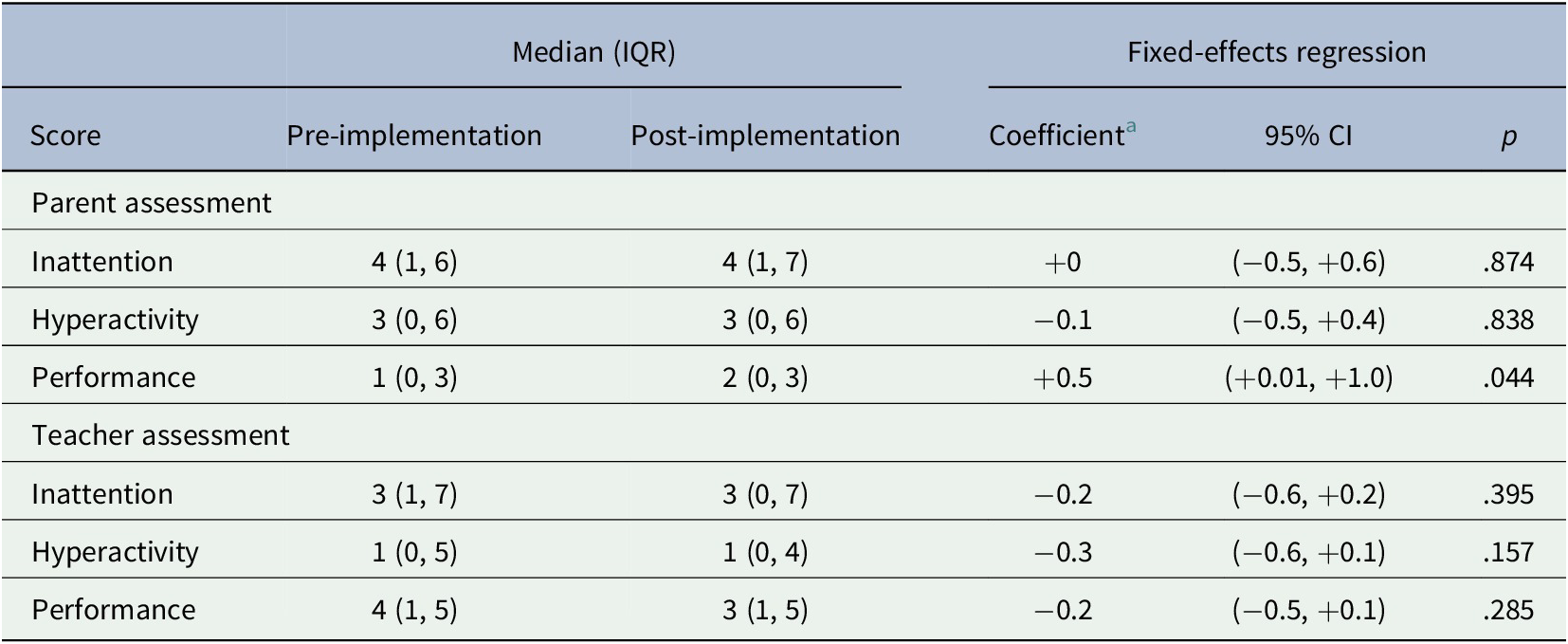
Abbreviations: CI, confidence interval; IQR, interquartile range.
a Difference in score attributable to policy implementation, controlling for all time-invariant patient characteristics.
4. Discussion
Vanderbilt forms have been found to accurately diagnose ADHD using a parent’s assessment of their child’s behavior, yet both parent and teacher forms are needed to optimize symptom management (Lavigne et al., Reference Lavigne, Dulcan, LeBailly and Binns2012; Silverstein et al., Reference Silverstein, Hironaka, Feinberg, Sandler, Pellicer, Chen and Cabral2016). Teacher forms are particularly important for capturing the impact of ADHD on children’s academic outcomes, but are infrequently used in pediatric clinics (Barbaresi et al., Reference Barbaresi, Katusic, Colligan, Weaver and Jacobsen2007; Epstein et al., Reference Epstein, Kelleher, Baum, Brinkman, Peugh, Gardner, Lichtenstein and Langberg2014; Reference Epstein, Kelleher, Baum, Brinkman, Peugh, Gardner, Lichtenstein and Langberg2017; Shapiro et al., Reference Shapiro, Wolz and Munro2018). One study of 128 pediatric offices found that 1 year after ADHD diagnosis, <11% of parent forms and <8% of teacher forms had been returned (Epstein et al., Reference Epstein, Langberg, Lichtenstein, Mainwaring, Luzader and Stark2008). Our policy intervention primarily increased the number of teacher forms returned, which may have signaled increased frequency of assessment and improved quality of care.
Despite increasing the number of forms returned, our intervention did not increase the proportion of families that returned any teacher forms. In comparison with prior studies, our baseline return rate was significantly higher (71% vs. 9%; Epstein et al., Reference Epstein, Langberg, Lichtenstein, Mainwaring, Luzader and Stark2008), and a similar policy may have been more effective in a clinic with a lower baseline return rate. Providing families and teachers with more options for completing assessment forms (e.g., via a secure online portal) may have helped more families assure ongoing monitoring of their child’s symptoms. In contrast to studies that suggested that use of teacher forms is correlated with a decrease in symptom scores, we found no significant changes in symptoms reported by teachers, despite an increased number of Vanderbilt assessments returned after agreement signature. Parent assessment performance scores exhibited a marginal change after the agreements were implemented, but differences between parent and teacher assessments may have led to discrepant scores between the forms.
Current guidelines for children with ADHD state the standard of treatment as medication, cognitive behavioral therapy, or a combination of both (Subcommittee on ADHD; Steering Committee on Quality Improvement and Management, 2011). Psychostimulant medication (e.g., methylphenidate and dextroamphetamine) is the predominant intervention for children with ADHD (Danielson et al., Reference Danielson, Bitsko, Ghandour, Holbrook, Kogan and Blumberg2018; Felt et al., Reference Felt, Biermann, Christner, Kochhar and Harrison2014). Although there is evidence that treatment can improve patient outcomes, ADHD requires additional familial responsibilities including scheduling multiple follow-up appointments and collecting regular assessments from teachers. This is a large burden for many families, and many patients are unable to follow recommendations for appointment scheduling or returning questionnaires (Dreyer et al., Reference Dreyer, O’Laughlin, Moore and Milam2010; Gardner et al., Reference Gardner, Kelleher, Pajer and Campo2004). Despite the importance of symptom questionnaires for tracking the response to treatment, many providers continue to refill medications and adjust treatments without receiving these measures in follow-up. As such, interventions to assure comprehensive and continuous monitoring of ADHD symptoms are needed to provide clinicians with data needed to guide patient treatment.
There are several limitations for this study that must be considered. We implemented a single intervention at one point in time, and did not compare the effectiveness of multiple interventions in improving Vanderbilt assessment return. Considering the rural location of our clinic, appointment nonadherence may have been related to barriers such as cost, transportation, employment, and family support. Another limitation was that patients may have left the clinic after the agreement was signed, but before they were due to return the next Vanderbilt assessment. Furthermore, although a majority of children with ADHD are diagnosed and treated by primary care pediatricians, some pediatricians may feel that they are not properly trained to manage mental health conditions. This may lead to ineffective treatment modifications in response to Vanderbilt assessments and may blunt the impact of increased assessment form return on symptom scores.
Future clinic interventions to increase return rates should consider targeted incentives or interventions to encourage families currently not returning any teacher forms to do so. Clinics implementing the Vanderbilt assessment forms to guide ADHD treatment should prioritize proper training for using the form, provide standard templates for documenting assessment scores and changes over time, and encourage form completion. Future research may consider evaluating Vanderbilt assessment return rate compliance and the effect on treating ADHD symptoms given the lack of association found in our study.
Abbreviations
- ADHD
attention-deficit/hyperactivity disorder
- IQR
interquartile range
Funding statement
The authors have no funding to disclose.
Conflict of interest
The authors have no conflicts of interest to disclose.
Data Availability Statement
Full data cannot be released to protect patient confidentiality. Deidentified data and statistical software code will be provided by authors for replication purposes upon request.




Comments
Comments to the Author: This is a well-written paper on an important practical topic. A few suggestions and questions to consider:
-Please clarify the denominator in the Methods and Table 1. I believe it is a percent of patients with a returned assessment, but it could also be the number of appointments with a returned assessment.
-If possible, it would be interesting to report the percentage of appointments when assessments were returned. The increase in the proportion of families completing multiple forms suggests a possible effect at the appointment level. That is, the intervention may have led to more frequent/ongoing assessment, which is also important to the quality of care and typically receives less attention than initial assessment.
-Consider adding a brief description of how forms were typically collected (e.g., paper copies provided by provider or front desk, links to online forms, paper forms mailed before appts) for more context.
-It would be interesting to read more about why a parent agreement was chosen as the intervention to improve return rates and how this type of intervention might change providers’ behavior. What other interventions are worth considering given that this was less effective than expected?