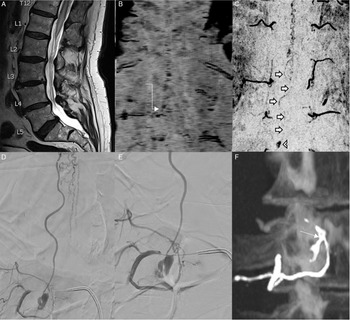
An 80-year-old male presented with a 3-month history of progressive right leg weakness and bilateral lower limb paresthesias. Examination at presentation showed right leg weakness (3/5 hip flexors, 4/5 knee extension, 4/5 foot dorsiflexion, and 4/5 foot plantar flexion), no bowel, or bladder dysfunction. An MRI of the spine demonstrated spinal cord edema extending from the mid-thoracic region to the conus, with serpiginous flow voids surrounding the lower cord and conus suggestive of a spinal dural arteriovenous fistula (SDAVF; Figure 1A). Time-resolved MRA was initially performed which suggested a SDAVF at the right L2 level (Figure 1B). At angiography, this level could not be catheterized due to focal aortic ectasia, and the SDAVF could not be identified. He underwent attempted surgical disconnection based on the MRI findings. Subsequent high-resolution MRA of the spine demonstrated a small venous pouch in the anterolateral epidural space at the right L3 level with persistent shunting to enlarged peri-medullary veins (Figure 1C). Diagnostic spinal angiogram was performed which demonstrated a spinal epidural arteriovenous fistula (SEAVF) with arterial supply from the right L2 and L3 segmental arteries, a large anterior epidural venous pouch and shunting to the perimedullary veins via a prominent radicular vein (Figure 1D/E) . Decision was made for endovascular embolization given the difficulties encountered with finding such fistulae on open surgical approach. Embolization was performed from the right L3 segmental level with Squid 12 EVOH copolymer liquid embolic (Balt Extrusion, Montmorency, France). Penetration of the fistula network including the epidural pouch was achieved, as well as the distal aspect of the L2 segmental artery via reflux. Subsequent angiographic runs demonstrated no persistent fistula. Follow-up unenhanced CT demonstrates the liquid embolic cast highlighting the SEAVF anatomy (Figure 1F) . The patient was discharged without complication.
SEAVF is a rare spinal shunt which often presents with perimedullary venous drainage. These lesions are often misdiagnosed, as highlighted by this case, as spinal SDAVF. Reference Kiyosue, Matsumaru and Niimi1,Reference Nasr, Brinjikji, Clarke and Lanzino2 One study found the rate of misdiagnosis for this entity as high as 70.8 % of cases. Reference Nasr, Brinjikji, Clarke and Lanzino2 Imaging criteria have been proposed to differentiate the two shunt types. Reference Kiyosue, Matsumaru and Niimi1,Reference Brinjikji, Yin, Nasr and Lanzino3 SEAVF are typically seen in older males in the thoracic/lumbar region with shunting seen to an epidural venous pouch within the ventral epidural space and subsequent drainage into perimedullary veins, paravertebral veins, or both. Reference Kiyosue, Matsumaru and Niimi1 Although previously thought to demonstrated lower incidence of spinal venous reflux, more recent work suggests that spinal venous drainage is common resulting a presentation with myelopathy. Reference Kiyosue, Matsumaru and Niimi1,Reference Geibprasert, Pereira and Krings4 Endovascular treatment has been the mainstay for these lesions due to the difficulties encountered with microsurgical approach. Reference Nasr, Brinjikji, Clarke and Lanzino2 However, a recent multicentre study from Japan demonstrated superiority of microsurgical management with lower risk of treatment failure. Reference Takai, Endo and Yasuhara5 As management of these uncommon lesions evolve, it is imperative that the characteristic features of SEAVF are recognized and the correct diagnosis is made. The present case exquisitely highlights the characteristic anatomy of SEAVF with a prominent ventral epidural venous pouch and perimedullary venous shunting. In addition, the results of the endovascular treatment are shown with a liquid embolic cast of the fistula that is beautifully seen on subsequent CT.

Figure. 1. Sagittal T2 images (A) of the lumbar spine demonstrates lower cord and conus edema. Time resolved MRA (B) suggests a possible spinal dural arteriovenous fistula at the right L2 level (white elbow arrow). Post-surgery high resolution MRA (C) demonstrates a persistent fistula, and a small ventral venous pouch is seen at the right L3 level (white arrow head) with a vein coursing towards to conus (white short arrows), suggesting the presence of a spinal epidural arteriovenous fistula (SEAVF). Repeat angiography (D,E) demonstrates a SEAVF with a ventral venous pouch at the right L3 level with arterial supply from the right segmental L3 (and L2) segmental arteries, and shunting to peri-medullary veins. Post-embolization CT (F), shows the cast of the liquid embolic highlighting the disconnected fistula(white arrow) with the epidural venous pouch.
Acknowledgements
None.
Disclosures
The authors do not have any conflicts related to this manuscript.
Statement of Authorship
Clinical management: AK, FP, PM, LD
Manuscript preparation: AK
Manuscript review, revisions and approval: AK, FP, PM, LD