Introduction
Coronavirus disease 2019 (COVID-19) is a major challenge to African health systems due to the scarcity of healthcare workers, lack of intensive and high care facilities, few public health specialists as well as weak primary health care (PHC) systems. The pandemic has not been as severe as feared in terms of mortality and hospital admissions, although confirmed cases may be low due to a lack of testing capacity, disguising the true extent of the pandemic (Bamgboye et al., Reference Bamgboye, Omiye, Afolaranmi, Davids, Tannor, Wadee, Niang, Were and Naicker2020). A household survey of six districts in Zambia showed a 100-fold higher level of COVID-19 infections than cases reported through the official national statistics, indicating a high level of hidden infections (Mulenga et al., Reference Mulenga, Hines, Fwoloshi, Chirwa, Siwingwa, Yingst, Wolkon, Barradas, Favaloro, Zulu and Banda2021). Some countries, such as South Africa, have reported rates on par with Europe and the USA. African populations may have fewer of the risk groups seen in high-income countries, such as the elderly and those with non-communicable diseases, but have other potential risk factors, such as HIV and TB (Dyer, Reference Dyer2020). In addition, widespread poverty and overcrowding in informal settlements and urban slums make isolation, quarantine and lockdown very difficult (Corburn et al., Reference Corburn, Vlahov, Mberu, Riley, Caiaffa, Rashid, Ko, Patel, Jukur, Martínez-Herrera and Jayasinghe2020). Many African countries were used to responding to epidemics, such as Ebola, and may have been more experienced in handling outbreaks of infectious diseases than other countries (Bamgboye et al., Reference Bamgboye, Omiye, Afolaranmi, Davids, Tannor, Wadee, Niang, Were and Naicker2020).
The Astana Declaration, with its goal of universal health coverage (UHC), endorses a vision of sustainable PHC embedded in strong health systems, with three components. These are first, primary care and public health functions as the core of integrated health services, including health promotion, surveillance, preparedness and response for health emergencies and outbreaks; second, empowered people and communities, for whom health literacy and active participation in decisions about their health are facilitated; and third, multisectoral policy and coordinated action across sectors to achieve health goals and reduce health threats (Rasanathan & Evans, Reference Rasanathan and Evans2020).
For COVID-19 responses to be aligned with the Astana Declaration, interdisciplinary collaboration between primary care, public health, community-based structures, emergency medicine and referral mechanisms is essential. Effective emergency preparedness requires urgent and responsive communication and coordination between centralised planners, policymakers and managers, with their implementation partners at primary care levels (Garg et al., Reference Garg, Basu, Rustagi and Borle2020). A review of guidelines during January to April 2020 from 14 countries identified public health guidance on outbreak control measures, use of telehealth and telephone triage to ensure continued delivery of essential primary care services and integrated planning for training, capacity building and data sharing with partners from various sectors (Haldane et al., Reference Haldane, Zhang, Abbas, Dodd, Lau, Kidd, Rouleau, Zou, Chao, Upshur and Walley2020). Guidance from some countries recommended involvement of community networks and organisations, especially for high-risk groups, including use of community health workers (CHWs) to create supportive local environments and facilitate contact tracing and case finding. Community structures were also identified as resources for delivering food, medication and other goods, especially for home-bound patients and their families. Gaps in guidance included mechanisms for ensuring adequate provision of personal protective equipment (PPE), testing kits and supply chain management. The authors suggest that strong partnerships between primary care and public health are essential for effective testing, contact tracing and support services. Communication and coordination between primary and secondary care services also need strengthening (Haldane et al., Reference Haldane, Zhang, Abbas, Dodd, Lau, Kidd, Rouleau, Zou, Chao, Upshur and Walley2020).
Other authors commented that many countries were unprepared at the onset of the COVID-19 pandemic in service reorganisation, COVID-19 screening and testing, and ensuring other essential services continued. Community cadres were bypassed in surveillance and health promotion activities which were often instituted centrally, and restrictions limiting travel and access to primary care facilities undermined the role of primary care as the first line in healthcare for communities (Rasanathan & Evans, Reference Rasanathan and Evans2020). Reviews of how primary care systems coped at the onset of the COVID-19 pandemic revealed not only critical weaknesses in health systems and intersectoral responses but also rapid adaptations in response to new challenges (Allen & Dambha-Miller, Reference Allen and Dambha-Miller2020). In well-resourced countries with already functioning UHC, the initial assessment and triage of people suspected of having COVID-19 was carried out by primary care teams, sometimes in assessment centres or remotely by telephone, email and videoconferencing (Huston et al., Reference Huston, Campbell, Russell, Goodyear-Smith, Phillips, van Weel and Hogg2020). In many countries, primary care facilities were reorganised to prioritise COVID-19 patients and to reduce risk of transmission, especially to vulnerable people (Chang & Chiu, Reference Chang and Chiu2020; Garg et al., Reference Garg, Basu, Rustagi and Borle2020; Huston et al., Reference Huston, Campbell, Russell, Goodyear-Smith, Phillips, van Weel and Hogg2020; Lim & Wong, Reference Lim and Wong2020; Sarti et al., Reference Sarti, Lazarini, Fontenelle and Almeida2020).
Information dissemination through daily press briefings, civic education and clear guidelines boosted confidence in government agencies. Such actions were proactively implemented at early stages of the pandemic by Taiwan and Singapore, who built on lessons learnt from the 2003 SARS (severe acute respiratory syndrome) and 2009 Influenza H1N1 epidemics (Chang & Chiu, Reference Chang and Chiu2020; Lim & Wong, Reference Lim and Wong2020). In countries like Brazil and India, these adaptations were sometimes limited by inflexible infrastructure and poor coordination (Garg et al., Reference Garg, Basu, Rustagi and Borle2020; Sarti et al., Reference Sarti, Lazarini, Fontenelle and Almeida2020). Brazil, albeit with an extensive primary care network and established UHC, struggled with difficulties in funding, personnel, supply and service restructuring (Sarti et al., Reference Sarti, Lazarini, Fontenelle and Almeida2020).
Telemedicine, video and zoom consultations rapidly expanded and became more accessible to the public (Huston et al., Reference Huston, Campbell, Russell, Goodyear-Smith, Phillips, van Weel and Hogg2020; Sarti et al., Reference Sarti, Lazarini, Fontenelle and Almeida2020). Reviews stressed the importance of already-established public health surveillance systems to ensure real-time data were collected to monitor emerging symptoms, complications, access to services, testing results and actions (Huston et al., Reference Huston, Campbell, Russell, Goodyear-Smith, Phillips, van Weel and Hogg2020). External and internal travel restrictions, border controls, as well as testing and home isolation or quarantine arrangements, required prior pandemic planning and legislative frameworks for rapid implementation.
Public understanding of the urgent need for restrictive public health measures such as physical distancing, mask-wearing, travel restrictions, hand hygiene and homeworking was essential. Provision of PPE and testing/contact-tracing services were slow to be established and suffered from competition in global markets for supplies (Garg et al., Reference Garg, Basu, Rustagi and Borle2020). Decreased use of primary care services for non-communicable diseases (NCDs), disruptions of other essential primary care services such as maternal and child care (MCH), HIV and tuberculosis services, with reduced referral for investigations and specialist assessments, led to fears of increased morbidity and mortality from non-COVID-19 illnesses (Garg et al., Reference Garg, Basu, Rustagi and Borle2020).
As the pandemic gained traction in Africa during May 2020, the African Journal of Primary Health Care and Family Medicine (PHCFM)Footnote 1 called for primary care providers and family physicians from countries in Africa to submit short reports on how they were responding and what they were learning about COVID-19. We wanted to look for opportunities to prepare for the pandemic and to make the most of the period between the early cases and widespread community transmission, for training health staff, reorganising health facilities, exploring strategic approaches that describe clear roles, tasks and communications, and to develop ways of communities supporting each other (Ray, Reference Ray2020). We asked for descriptions of innovations and good practices in PHC and family medicine (FM), including the contributions of family physicians, the management of COVID-19 in district health services and responses of communities to the outbreak.
These short reports were descriptive and do not present empirical data. They did not report on research or provide definitive evidence of effectiveness of the ideas presented. They did not attempt to be representative of the total experience of COVID-19 services in Africa and were limited to authors who chose to respond to the journal’s call for short reports. Each short report was peer-reviewed by one or two reviewers. The aim of this paper is to synthesise the lessons described in these short reports and to guide readers to ideas and resources available in addressing the challenges raised by the COVID-19 pandemic.
Methods
This was a qualitative descriptive study of short reports published in PHCFM with a thematic analysis. All short reports accepted for publication in a special collection on COVID-19 were included in the qualitative analysis. The analysis was conducted by the two authors, SR and RM. SR is an assistant editor of PHCFM and oversaw the special edition; RM is the Editor-in-Chief of PHCFM and also an author on some of the short reports. The reports were initially divided between the two authors, who independently analysed their allocated documents. RM used Atlas-ti software, while SR carried out the analysis manually. Each conducted the analysis using the following steps: reading the reports to familiarise with the contents, coding all the documents inductively, creating coding groups and charts based on these groups that brought all the same coded data together and finally interpreting the data in the charts. The two researchers then discussed their analyses and came to a consensus on the code groups and themes they had derived. They reread all twenty-seven papers and integrated their analyses into one set of themes and analysis which are presented here.
Ethics approval and participant consent were not required since all the papers reviewed were published in the journal and in the public domain.
Findings
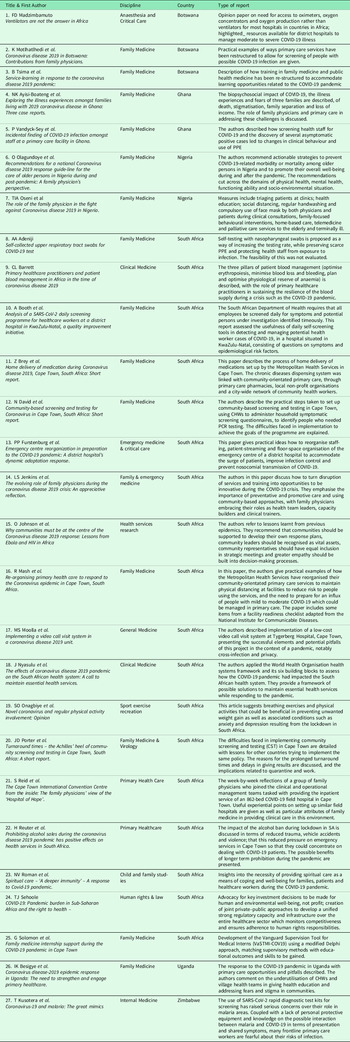
Twenty-seven short reports were accepted for publication in the PHCFM and were submitted from six countries: Botswana, Ghana, Nigeria, South Africa, Uganda and Zimbabwe (see Table 1). The majority of short reports published were from South Africa, reflecting the proportion of submissions to the journal in general. South Africa is a leading country in terms of academic outputs and family medicine in the region. There were eight main themes derived from the data: community-based activities; screening and testing; reorganisation of health services; provision of emergency care for COVID-19; maintenance of essential non-COVID-19 health services; caring for the vulnerable; use of information technology and reframing training opportunities.
Table 1. Summary of submissions published in special issue of Primary Health Care and Family Medicine on COVID-19 May–August 2020

Community-based activities
The Metro Health Services (MHS) in Cape Town, as part of the Government of the Western Cape, embraced the concept of Community Orientated Primary Care (COPC) since 2017 in policy and reorganised PHC accordingly (David & Mash, Reference David and Mash2020; Mash, Goliath & Perez, Reference Mash, Goliath and Perez2020). The principles of COPC involve delineation of geographic areas, alignment of these areas with primary care facilities and networks of CHW teams. There were approximately 2500 CHWs employed by multiple non-profit organisations. The MHS had a number of adaptive community-based responses to the COVID-19 outbreak, which were described in several articles by different authors (Brey et al., Reference Brey, Mash, Goliath and Roman2020; David & Mash, Reference David and Mash2020; Mash, Goliath & Perez, Reference Mash, Goliath and Perez2020; Porter, Mash & Preiser, Reference Porter, Mash and Preiser2020). CHWs provided domiciliary visits for follow-up of patients with HIV, TB, mental disorders, postnatal care and palliative care needs. They also home-delivered medications, non-pharmaceutical equipment and supplies to people with chronic conditions (184 000 parcels delivered in first month), thus protecting them from potential exposure at primary care facilities and in public transport (Brey et al., Reference Brey, Mash, Goliath and Roman2020; Mash, Goliath & Perez, Reference Mash, Goliath and Perez2020).
Beyond these examples from Cape Town, there was little evidence of community-orientated responses, engagement or local priority setting in the other short reports. Some described public health education campaigns that were carried out through community organisations and social media (Motlhatlhedi et al., Reference Motlhatlhedi, Maotwe, Bogatsu and Tsima2020; Oseni et al., Reference Oseni, Agbede, Fatusin and Odewale2020). National level health education and mass sensitisation of the population was carried out in Uganda at all levels, while district and community leaders in Uganda were responsible for enforcing bans on gatherings and funerals and ensuring that soap and water were available in public places (Besigye, Mulowooza & Namatovu, Reference Besigye, Mulowooza and Namatovu2020). Community support was provided as donations by local non-government organisations (NGOs), religious groups and businesses in Uganda (Besigye, Mulowooza & Namatovu, Reference Besigye, Mulowooza and Namatovu2020). In South Africa, provision of food parcels or vouchers for food and help with transport and communications was reported (Brey et al., Reference Brey, Mash, Goliath and Roman2020).
The COVID-19 response focused mainly on central hospitals and critical care provision, with prevention measures in Uganda enforced by security and military personnel, which may have deterred real community engagement. The authors felt that PHC-led activities could have utilised village health teams and CHWs more, as well as private health providers, to educate the public, address stigma and fear of infection (Besigye, Mulowooza & Namatovu, Reference Besigye, Mulowooza and Namatovu2020). Using the World Health Organization’s (WHO) Health Systems Framework, authors suggested ways in which providing services closer to communities could reduce the impact of the pandemic. These included integrating health education campaigns with other primary care messages and delegation of health promotion on primary care to lower level health workers (Nyasulu & Pandya, Reference Nyasulu and Pandya2020).
Social mobilisation brings together societal and individual influences to raise awareness of and demand for healthcare and to effect social change (WHO, no date). Authors wrote from experiences of Ebola in West Africa and of people living with HIV in Zimbabwe that social mobilisation in such epidemics needed to be at the top of the agenda, rather than the bottom, and that trust and confidence have to be built with communities to secure their cooperation (Johnson & Goronga, Reference Johnson and Goronga2020). Public health strategies need to take account of the social, religious, cultural and political dynamics that influence the uptake of health interventions, instead of imposing interventions on communities. More investment in community partnerships should lead to better outcomes. Stigma and fear of infection within communities or resistance to unfeasible interventions may otherwise paralyse action against the virus (Besigye, Mulowooza & Namatovu, Reference Besigye, Mulowooza and Namatovu2020; Johnson & Goronga, Reference Johnson and Goronga2020).
Punitive quarantine measures may result in people avoiding diagnosis and hiding from health services, especially when their livelihoods and their ability to pay rent and feed their families are threatened. Community leaders and representatives of affected people should be recognised as the experts on their lived realities and included in discussions to provide health education (Johnson & Goronga, Reference Johnson and Goronga2020). One author stressed the need to ensure that human rights and the right to health were protected, especially for the most vulnerable and not left to the private health marketplace in African countries (Sehoole, Reference Sehoole2020). Nation states are legally bound to ensure that privatisation of services is not a threat in such a crisis, to the availability, accessibility and quality of health services. The author suggested that more equitable and essential services for COVID-19 could be provided through the creation of a wealth tax especially targeting those who were making profits from the crisis (Sehoole, Reference Sehoole2020). Other mechanisms were proposed for protecting families against catastrophic out-of-pocket health expenditure, such as through public–private regulation, national health insurance or incentives for private health insurers to absorb costs of more equitable healthcare distribution (Sehoole, Reference Sehoole2020).
An apparent benefit of the alcohol prohibition during the first level lockdown in South Africa was a reduction in trauma and emergency admissions not only due to assaults, road traffic accidents, and other injuries related to alcohol misuse but also due to fewer vehicles on the road (Barrett, Reference Barrett2020; Reuter et al., Reference Reuter, Jenkins, De Jong, Reid and Vonk2020). Concerns for the resilience of blood supplies due to less availability of donors, thereby jeopardising emergency obstetric and intensive care, led to proposals for patient blood management systems to ameliorate the impact of shortages of donor blood, including the role of primary care practitioners in sustaining blood supplies (Barrett, Reference Barrett2020). Data reported from South Africa showed reductions in contact crimes (murder, rape and assault) and in numbers of unnatural deaths (Reuter et al., Reference Reuter, Jenkins, De Jong, Reid and Vonk2020). There were also negative health consequences associated with lockdown. These included depression, anxiety and increases in domestic violence from being isolated with abusers, as well as social consequences of loss of income, food insecurity and unrest (Ayisi-Boateng et al., Reference Ayisi-Boateng, Egblewogbe, Owusu-Antwi, Essuman and Spangenberg2020; Onagbiye et al., Reference Onagbiye, Mchiza, Bassett, Travill and Eijnde2020; Oseni et al., Reference Oseni, Agbede, Fatusin and Odewale2020).
Screening and testing
In Cape Town, highly vulnerable communities were identified as those with low socio-economic status and overcrowding in informal settlements. These communities also had high proportions of people suffering from HIV, tuberculosis, hypertension, diabetes and chronic lung disease, which predisposed them to more severe COVID-19 illness. All households in those communities were screened using a symptom-based questionnaire. Targeted screening was used to focus on households around known cases in other vulnerable communities. CHWs assisted with screening of communities using a symptom-based questionnaire (David & Mash, Reference David and Mash2020; Porter, Mash & Preiser, Reference Porter, Mash and Preiser2020).
Testing for COVID-19 was a major problem for most African countries because of difficulties in procuring test kits and the turn-around times (TAT) at laboratories. In Uganda, testing was limited by the number of laboratories available and tests were initially only performed in one central laboratory, with no plans for community-based sample collection (Besigye, Mulowooza & Namatovu, Reference Besigye, Mulowooza and Namatovu2020). The global shortage of rapid test polymerisation chain reaction (RT-PCR) kits, intended for diagnosis of acute infections, meant that some low- to medium-income countries resorted to using cheaper antibody (RDT-AB) test kits for screening, followed by PCR if positive, despite the low sensitivity of antibody tests (Kusotera & Nhengu, Reference Kusotera and Nhengu2020). In Zimbabwe, in high malaria prevalence areas, patients with malaria (which presents with symptoms similar to COVID-19) were suspected of having COVID-19, leading to panic on the part of health staff and communities. This was made worse if they were tested using RDT-AB and had a false positive result, but with a negative confirmatory PCR test only returning from a central laboratory days later (Kusotera & Nhengu, Reference Kusotera and Nhengu2020).
The community screening and testing programme in Cape Town used mobile testing centres that collected specimens from household members who had screened positive for COVID-19 symptoms by CHWs (Porter, Mash & Preiser, Reference Porter, Mash and Preiser2020). This was a strategy intended to slow the spread of COVID-19 by targeting hotspots in vulnerable communities. It was however made obsolete by the increasing TAT (Mash, Goliath & Perez, Reference Mash, Goliath and Perez2020). In primary care facilities, the TAT could take up to 31 days and rendered efforts at community screening useless as cases and contacts could not be followed up in time.
CHWs were then asked to screen households in their area but only refer for testing symptomatic people aged over 55 years or with co-morbidities. While the National Health Laboratory Service in South Africa aimed at a TAT of 48 h, this was seldom achieved. District hospitals had a median TAT of 3 days, which was longer than the median length of stay, so hospitalised patients were treated as persons under investigation (PUI) without a definitive diagnosis. In this way, the approach moved from preventing local transmission to case finding in high risk people (Porter, Mash & Preiser, Reference Porter, Mash and Preiser2020). One author proposed the idea of self-testing with nasopharyngeal swabs as a way of increasing the testing rate, while preserving scarce PPE and protecting health staff from exposure to infection, though the feasibility of this was not evaluated (Adeniji, Reference Adeniji2020).
Reorganisation of health services
Infrastructure at primary care facilities and hospitals had to be rapidly reorganised. In primary care, this was done to decongest services, to reduce the risk of infection and free up capacity to respond to the expected surge of patients with respiratory problems (Furstenburg et al., Reference Furstenburg, Mukonkole, Kibamba, Kuiler, Ngemntu, Lahri, Van Hoving, Moodley and Erasmus2020; Mash, Goliath & Perez, Reference Mash, Goliath and Perez2020; Motlhatlhedi et al., Reference Motlhatlhedi, Maotwe, Bogatsu and Tsima2020; Vandyck-Sey et al., Reference Vandyck-Sey, Amoh, Essuman and Lawson2020). A PHC facility readiness checklist was adapted from the National Institute for Communicable Diseases and used in Cape Town to assess the readiness of the PHC system across key inputs and service delivery domains. The checklist of 43 items assessed facility management, screening and streaming of patient flows, use of infrastructure, supply chains, health intelligence and communication (Mash, Goliath & Perez, Reference Mash, Goliath and Perez2020). Health staff were relocated from other services to COVID-19 screening and treatment locations (Motlhatlhedi et al., Reference Motlhatlhedi, Maotwe, Bogatsu and Tsima2020).
Facilities attempted to comply with essential infection control methods: hand washing/sanitisation, physical distancing, use of face masks and other PPE as appropriate (Motlhatlhedi et al., Reference Motlhatlhedi, Maotwe, Bogatsu and Tsima2020; Oseni et al., Reference Oseni, Agbede, Fatusin and Odewale2020; Vandyck-Sey et al., Reference Vandyck-Sey, Amoh, Essuman and Lawson2020). Most facilities attempted to separate patients into PUI with respiratory symptoms in a ‘hot’ stream and those without any symptoms into a ‘cold’ stream. In Cape Town, patients with minor ailments were treated and discharged as soon as possible in both streams (Mash, Goliath & Perez, Reference Mash, Goliath and Perez2020). Several primary care facilities rapidly constructed COVID-19 testing and treatment centres from prefabricated structures, containers and tents outside the entrance. In southern Africa, the first wave of the pandemic peaked during the winter months, which meant that outside spaces could no longer be used due to rain and cold temperatures (Furstenburg et al., Reference Furstenburg, Mukonkole, Kibamba, Kuiler, Ngemntu, Lahri, Van Hoving, Moodley and Erasmus2020; Mash, Goliath & Perez, Reference Mash, Goliath and Perez2020).
Authors explored methods of protecting health workers who were at significant risk of contracting COVID-19, especially when PPE was in short supply globally (Mash, Goliath & Perez, Reference Mash, Goliath and Perez2020; Vandyck-Sey et al., Reference Vandyck-Sey, Amoh, Essuman and Lawson2020). In some settings, staff fears led to overuse of PPE, while in other settings PPE had to be re-used or innovated. Staff were reportedly more likely to be infected in non-clinical areas and in the ‘cold’ stream as they felt less at risk and relaxed their precautions. Older staff members and those with co-morbidities were shielded from working in high exposure areas (Mash, Goliath & Perez, Reference Mash, Goliath and Perez2020; Vandyck-Sey et al., Reference Vandyck-Sey, Amoh, Essuman and Lawson2020). In many situations, frontline health workers became burnt out and overwhelmed so more caring for carers was necessary.
The South African Department of Health required employees to be screened daily for COVID-19 before commencement of duty. Authors reported from a hospital in KwaZulu-Natal that a self-administered symptom-screening tool was ineffective because of poor completion as well as inadequate awareness and training (Booth, Omed & Naidoo, Reference Booth, Omed and Naidoo2020). Several staff had positive symptoms but did not document what action was taken as a result. The team advised that internal quality control, improved oversight by managers and addition of temperature checks could improve adherence. They recommended that local champions (advocates and influencers within health teams) and management needed to endorse, drive and monitor implementation of the screening process and that staff had to be motivated to change their practices. Training in the need for safety measures, physical distancing, avoiding unnecessary meetings or social gatherings during breaks, and providing transport for staff to reduce use of public transport, were other measures suggested by authors (Booth, Omed & Naidoo, Reference Booth, Omed and Naidoo2020).
Provision of emergency care for COVID-19
Hospital emergency centres had to constantly adapt to the needs and volume of patients, and in South Africa, field hospitals were established to cope with large numbers of patients. The Hospital of Hope was established within a matter of weeks as an intermediate care facility at the Cape Town International Convention Centre, with over 800 beds, all with piped oxygen (Reid, Ras & von Pressentin, Reference Reid, Ras and von Pressentin2020). The availability of oxygen was a key feature that enabled care to be more than just assisted isolation. The medical management and staff were drawn mostly from family physicians, whose values included upholding the humanity of their patients despite the mass processing of people, clear leadership and planning, close multidisciplinary teamwork, frequent communication (with team members, patients and their families), continuity of care, commitment, mutual trust and willingness to adapt and learn. The importance of family-centred, multidisciplinary and team-based approaches in responding to the challenges of COVID-19 care was echoed in Ghana especially in supporting families that have been separated from their loved ones and the mental health challenges arising from this (Ayisi-Boateng et al., Reference Ayisi-Boateng, Egblewogbe, Owusu-Antwi, Essuman and Spangenberg2020).
The challenges of managing patients with severe illness at district hospitals, because central hospitals were overwhelmed, were also explored (Madzimbamuto, Reference Madzimbamuto2020). Instead of being preoccupied with finding or manufacturing ventilators, district hospitals could plan to utilise accessible resources more equitably, for example by establishing early warning systems for hypoxia, acquiring oximeters, oxygen concentrators and training health staff in fundamentals of critical care. Sources were publicised of appropriate technology that were already available, such as support for securing oxygen supplies through Assist International, and the Lifebox Scheme for oximeters, were promoted through international partnerships such as the World Federation of Societies of Anaesthesiologists (Madzimbamuto, Reference Madzimbamuto2020). These resources would continue to be useful in supporting emergency care in district hospitals for emergency surgical, obstetric and neonatal care.
Maintenance of essential non-COVID-19 health services
Authors (Barrett, Reference Barrett2020; Nyasulu & Pandya, Reference Nyasulu and Pandya2020) reminded us of the WHO definition of resilience as the inbuilt capacity of the system to sustain provision of essential health and health-related services even when challenged by outbreaks, disasters or other shocks. Health systems did not demonstrate resilience in this context since there was significant disruption to essential services, especially for MCH, HIV, tuberculosis and non-communicable diseases (NCDs). Public health advice to stay at home, to avoid public facilities and transport may have led to decreased uptake of essential primary care services even when they were available (Mash, Goliath & Perez, Reference Mash, Goliath and Perez2020). In Zimbabwe, authors described how stigma and fear of infection associated with COVID-19 prevented access to testing and treatment for malaria (Kusotera & Nhengu, Reference Kusotera and Nhengu2020). The authors reminded us of the WHO warning that malaria deaths could double if the focus on COVID-19 disrupted interventions for malaria (World Health Organization, 2020). Health workers were diverted from their usual workplaces to work in isolation centres and for local task forces, causing a breakdown in routine services. In Botswana, MCH services were restricted to immunisations and nutrition care, with reduced antenatal care only for high-risk pregnancies (Motlhatlhedi et al., Reference Motlhatlhedi, Maotwe, Bogatsu and Tsima2020).
Authors described actions taken to maintain essential primary care services and to prevent excess mortality from neglect of other conditions especially NCDs (diabetes, hypertension), HIV, tuberculosis and malaria. Activities, for instance in Botswana, included extension of review periods for stable NCD patients and medication refills at pharmacies without prior doctors’ consultation (Motlhatlhedi et al., Reference Motlhatlhedi, Maotwe, Bogatsu and Tsima2020). The WHO Health Systems Framework was used in one study to assess critical markers of resilience of the health system, for example, the ability to offer basic health care to pregnant women, immunisation for children and treatment for people with HIV (Nyasulu & Pandya, Reference Nyasulu and Pandya2020). Their suggested solutions to maintaining services, despite deployment of health staff to COVID-19 areas, were to integrate services, to utilise medical, nursing and clinical associate students in non-COVID-19 essential services, convert part-time contracts to full time, bring back retired health staff into service, and to explore other task shifting measures, such as co-opting NGO partners and non-health staff from other government departments. They also recommended that ways of acknowledging and appreciating the health workforce be explored, to encourage cohesiveness in working together.
Caring for the vulnerable
The need for explicit strategies to identify disadvantage and inequalities, and guidelines on providing targeted services for vulnerable groups, was a priority for authors from Uganda, South Africa and Nigeria (Besigye, Mulowooza & Namatovu, Reference Besigye, Mulowooza and Namatovu2020; Nyasulu & Pandya, Reference Nyasulu and Pandya2020; Olagundoye, Enema & Adebowale, Reference Olagundoye, Enema and Adebowale2020). Arrangements were required for provision of food, medication refills for chronic conditions, psychological support and communication (Ayisi-Boateng et al., Reference Ayisi-Boateng, Egblewogbe, Owusu-Antwi, Essuman and Spangenberg2020; Motlhatlhedi et al., Reference Motlhatlhedi, Maotwe, Bogatsu and Tsima2020; Olagundoye, Enema & Adebowale, Reference Olagundoye, Enema and Adebowale2020). There was particular concern for the impact of social isolation due to physical distancing on older persons, those with mental health conditions and those on medication for HIV or other chronic illnesses (Olagundoye, Enema & Adebowale, Reference Olagundoye, Enema and Adebowale2020).
Reorganisation of services to reduce risk to vulnerable people included remote access through the use of telemedicine and toll-free phone lines, home delivery of medication, reduced waiting times and triage, prioritised testing, prioritisation of welfare packages and community-based interventions from civil society organisations (Ayisi-Boateng et al., Reference Ayisi-Boateng, Egblewogbe, Owusu-Antwi, Essuman and Spangenberg2020; Brey et al., Reference Brey, Mash, Goliath and Roman2020; Nyasulu & Pandya, Reference Nyasulu and Pandya2020; Olagundoye, Enema & Adebowale, Reference Olagundoye, Enema and Adebowale2020; Oseni et al., Reference Oseni, Agbede, Fatusin and Odewale2020). Shielding of elderly family members at home could be done through changes in sleeping arrangements, especially keeping school-going children separate (Johnson & Goronga, Reference Johnson and Goronga2020). Financial arrangements included identifying responsible adults to have power of attorney if family members were incapacitated in hospital. Health insurance packages needed amendment to include home-based or palliative care (Olagundoye, Enema & Adebowale, Reference Olagundoye, Enema and Adebowale2020).
Use of information technology and social media
Several authors mentioned that telephone consultations, telemedicine and web-based platforms were used to keep patients from attending health facilities. This was more feasible for private sector patients with more reliable internet and cell phone connectivity (Ayisi-Boateng et al., Reference Ayisi-Boateng, Egblewogbe, Owusu-Antwi, Essuman and Spangenberg2020; Motlhatlhedi et al., Reference Motlhatlhedi, Maotwe, Bogatsu and Tsima2020; Nyasulu & Pandya, Reference Nyasulu and Pandya2020; Oseni et al., Reference Oseni, Agbede, Fatusin and Odewale2020). Telephonic consultations were introduced in Nigeria as alternatives to face-to-face consultations and if a visit was essential, a telephonic appointment systems ensured patients did not crowd together at the same time (Oseni et al., Reference Oseni, Agbede, Fatusin and Odewale2020).
Spiritual care was often limited as chaplains and religious leaders were not allowed to enter facilities. In hospitals, visitors were prohibited and staff wore full PPE when administering to sick patients with COVID-19. Although health professionals supported the provision of spiritual care especially in end-of-life situations, they often felt ill-equipped to deliver it. Information and communications technology contributed significantly to making the response more humane at the same time as being more effective. Solutions proposed included use of social media and video links for virtual family visits though this required high-speed internet access (Reid, Ras & von Pressentin, Reference Reid, Ras and von Pressentin2020; Roman, Mthembu & Roman, Reference Roman, Mthembu and Roman2020). In one hospital in Cape Town, “video call champions” were appointed in each ward whose role included raising awareness of the video call system and taking primary responsibility for making calls. Family members could visit from home or at the hospital in a separate room via web-based video calls (Moolla et al., Reference Moolla, Broadhurst, Parker, Parker and Mowlana2020).
Solutions to managing lockdown were proposed and included web-based games and videos (for those who could afford internet), which assisted people to take physical exercise, prevent weight gain and maintain good psychological well-being (Onagbiye et al., Reference Onagbiye, Mchiza, Bassett, Travill and Eijnde2020). Such initiatives could also benefit people with NCDs such as diabetes, hypertension and respiratory conditions. A WhatsApp robot was used in Cape Town to allow people to request home delivery of medication and to verify their addresses (Brey et al., Reference Brey, Mash, Goliath and Roman2020). Information dissemination via social media and WhatsApp messaging was used for patient groups and practitioners in Botswana and was especially useful for communication to rural practitioners (Motlhatlhedi et al., Reference Motlhatlhedi, Maotwe, Bogatsu and Tsima2020). WhatsApp audio messaging was also suggested to provide information on self-care to people with NCDs.
Reframing training opportunities
The reorientation of health services caused disruption to the learning environments and clinical training of registrars in family medicine (Jenkins et al., Reference Jenkins, Von Pressentin, Naidoo and Schaefer2020; Tsima, Masupe & Setlhare, Reference Tsima, Masupe and Setlhare2020). Many services were de-escalated or stopped and registrars re-deployed to tackle the pandemic. This meant that many of their planned training activities could not go ahead. Related examinations and research activities were stopped or postponed. Learning opportunities were refocused on opportunities presented by the response to the pandemic, particularly as family physicians were at the forefront of reorganising primary care services. Examples given were of closer intersectoral working, better resource management and cooperation with the private sector, shifting towards more health promotive and preventive community-based approaches (Jenkins et al., Reference Jenkins, Von Pressentin, Naidoo and Schaefer2020). Adapting in response to a crisis was a key skill to be learnt, recognising that over-centralising control may lose the opportunity to build capacity at district levels and for active experiential learning (Jenkins et al., Reference Jenkins, Von Pressentin, Naidoo and Schaefer2020). At one health centre, a novel supervision tool was created to maximise the opportunities for learning (Solomon et al., Reference Solomon, Allie, Fakier, Tadmor, Ashtiker, Le Roux, Omar and Namane2020). Educational activities in Botswana and South Africa were adjusted to use more virtual learning platforms and to develop alternative learning outcomes. Learning outcomes related to epidemic preparedness, emergency planning, surveillance and infection control, development of patient management protocols, knowledge synthesis from emerging scientific literature or work for the Ministries of Health on strategy and policy development. Flexibility with timetables also allowed registrars to use elective and self-directed learning periods to catch up on care for other conditions, even using web-based platforms to do this (Jenkins et al., Reference Jenkins, Von Pressentin, Naidoo and Schaefer2020; Solomon et al., Reference Solomon, Allie, Fakier, Tadmor, Ashtiker, Le Roux, Omar and Namane2020; Tsima, Masupe & Setlhare, Reference Tsima, Masupe and Setlhare2020).
Discussion
The experiences, learning and recommendations shared in these papers from sub-Saharan Africa are not from original research and represent a diverse range of snapshots of different responses to the pandemic from different African countries. This synthesis can only reflect what authors chose to submit to us for publication and may not be representative of all activities undertaken. The paucity of community-based innovations does not mean none were undertaken in the region, but that they were not written about or submitted to PHCFM. Examples of community responses to COVID-19 have been published elsewhere (Loewenson et al., Reference Loewenson, Colvin, Szabzon, Das, Khanna, Coelho, Gansane, Yao, Asibu, Rome and Nolan2021) and include activities mentioned here: community support for symptom surveillance, mobilising for blood donations, uptake of testing and contact tracing, distribution of food and other materials, involvement of local leadership and use of social media and telemedicine to disseminate information. Definitive evidence-based recommendations based on these papers cannot be made, but a number of themes have emerged, with ideas and lessons for better emergency preparedness and collaborative working. The papers in this special collection form a resource for providers for ideas on how to adapt and improve PHC services even in a time of crisis.
Many of the short reports described interventions similar to those in the international literature, especially in use of information technology, partnership between formal health structures and community-based cadres, and the role of primary care facilities in reorganising services to cope with the immediate crisis and to protect vulnerable people. According to these short reports, many African countries did not have PHC at the forefront of their responses to COVID-19 but the strength of preceding PHC systems may have predicted the ability to adapt and respond appropriately. For example, in Cape Town, implementation of policy on reorganising PHC was only possible because of strong functional governance structures that extended to the facility level and home delivery of medication was only possible because CHW teams were previously established in all communities. Community and village health workers in many countries were underutilised as mediators with the public, a shortcoming recognised by many authors. The challenges of stigma and fear of infection repeatedly experienced in disease outbreaks need much greater understanding since these phenomena posed barriers to screening, testing and care for COVID-19. Family physicians emphasised the importance of adaptive management that did not overly centralise control and which built peoples’ capacity to innovate, improve the response to emergencies in an incremental way and learn actively from experience at the frontline. Such decentralised leadership, however, also relied on family physicians or other clinical leaders within the PHC teams in distributed health services.
The COVID-19 pandemic exposed the need for countries to focus on strengthening PHC for more effective responses. In line with the Astana Declaration (Rasanathan & Evans, Reference Rasanathan and Evans2020), the importance of the COPC approach, which deliberately integrates public health and primary care approaches as well as facility and community-based services, is emphasised as the foundation from which to adapt and respond to emerging crises. Integration of public health and primary care approaches, rapid implementation of emergency preparedness plans and use of population based health data were found to be more important than having strong primary care systems in tackling COVID-19, albeit at an early stage of the pandemic (Goodyear-Smith et al., Reference Goodyear-Smith, Kinder, Mannie, Strydom, Bazemore and Phillips2020). The commitment of this COPC approach to community and stakeholder engagement may also be key in developing appropriate interventions, messages and reducing fear and stigma. Leadership from family physicians and primary care practitioners in establishing rapid communications, coordination and delegation from centralised policymakers and managers appeared to facilitate more sustainable and equitable pandemic responses.
The COVID-19 pandemic also highlighted the catalytic effect of access to appropriate technology and equipment. Key examples include cell phone and internet-based communication, laboratory capacity and the need to focus on oxygen supply rather than ventilators at this level of care. Access to cell phone technology and the internet transformed the way that health services related to patients and organised themselves. Technology was used to communicate with, protect vulnerable people and provide health care as well as coordinate teams of health care workers. Information and research findings were interrogated and disseminated more rapidly than in the past through webinars, podcasts and social media. Services could also more easily source equipment, PPE and other supplies. The crisis provided opportunities for innovation, which could have value for longer term development of health service delivery (Brey et al. Reference Brey, Mash, Goliath and Roman2020; Besigye, Mulowooza, & Namatovu Reference Besigye, Mulowooza and Namatovu2020; Jenkins et al. Reference Jenkins, Von Pressentin, Naidoo and Schaefer2020; Madzimbamuto Reference Madzimbamuto2020; Oseni et al. Reference Oseni, Agbede, Fatusin and Odewale2020).
The contribution of PHC will also be essential in the medium to long term as vaccination programmes are set up and in following up people with so-called “long” COVID-19. PHC will have to be at the forefront of the recovery stage of this pandemic in re-establishing services that may have been neglected, especially for HIV, tuberculosis, MCH and NCDs. The long-term impact of COVID-19 will be seen through its effect on UHC. The control of other priority diseases will have deteriorated, and the economic effects of lockdown on the social foundation of society will also impact on health. The measurement of impact will need to extend beyond hospitalisations and deaths. As we start to turn the corner on controlling the COVID-19 pandemic, we will need to continue the fight for UHC and PHC.
Conclusion
Lessons learnt from African family medicine and PHC systems in responding to the COVID-19 pandemic can be summarised under eight major themes: community-based services, screening and testing, reorganisation of health services, provision of emergency care for COVID-19, maintenance of essential non-COVID-19 services, caring for the vulnerable, use of information technology and reframing training opportunities. The community-orientated primary care approach was emphasised as well as long-term benefits of technological innovations. The COVID-19 pandemic exposed the need to deliver on governmental commitments to strengthening PHC and UHC.
Acknowledgements
The authors would like to thank the authors whose short reports are included in this PHCFM collection and to the reviewers of the articles who gave constructive comments on how they could be improved.
Conflicts of interest
None known.
Funding
None required.