The published experience of health care providers involved in disasters over the past decade has repeatedly emphasized the importance of planning, preparation, and evacuation procedures in these situations. Critically ill patients are especially vulnerable during disasters, because they are both medically fragile and their care and evacuation require special equipment and expertise. Insufficient coordination of resources and patient monitoring during movement of critically ill patients are often cited as reasons for clinical deterioration during transport.Reference Orlando, Bernard and Mathews 1 – Reference Tanaka, Iwai and Oda 5 Simulation of patient preparation and transport using actual transport equipment increases the likelihood of successful individual evacuation performance as well as system-wide cooperation.Reference Gildea and Etengoff 6 , Reference Cybulski 7
Little is known about provider preparedness or the performance of effective and safe evacuation of critically ill patients during disasters. Intensive care unit (ICU) providers rarely consider the challenges of moving a critically ill patient within or outside of the hospital in the event that their ICU is rendered incapable of supporting appropriate ongoing care. Although ICU providers are familiar with horizontal transport (moving ICU patients laterally on the same floor), they are less familiar with vertical transport (moving patients either up or down floors), especially in disaster situations that require transport up or down stairs. Although many patients have common critical care requirements (such as mechanical ventilation or vasopressor infusion) that would be routine for most receiving hospitals, some patients require specialized care that may exceed the capability of transport teams and receiving locations (eg, extracorporeal life support [ECLS], intracranial pressure management, and micro-prematurity neonatal care). Deliberate planning is the only way to appropriately address the complex challenges that ICU providers may face in a disaster.
Hurricane Sandy was the deadliest storm outside of the southern United States since 1972,Reference Blake, Kimberlain and Berg 8 claiming more than 250 lives. Although the extent of its devastation could not have been fully predicted, the New York City area hospitals most affected received ample warning through news media of the cyclone’s impending landfall on November 5, 2012. Hurricane Sandy therefore provides a unique opportunity to evaluate critical care provider preparedness and experience with this single major evacuation event from multiple hospital perspectives and to inform future critical care disaster evacuation planning. The objectives of this report were to describe (1) ICU provider preparedness efforts in New York City prior to ICU evacuation, (2) provider roles and activities during ICU evacuation following Hurricane Sandy, and (3) ICU provider perspectives on their evacuation preparedness, tools, and systems.
Methods
Following study approval by the Seattle Children’s Hospital Institutional Review Board, phone or e-mail contact was attempted with all medical ICU directors from identified New York City area hospitals affected by Hurricane Sandy. Respondents were asked to voluntarily participate in a research survey. Directors who consented were asked to distribute an anonymous electronic survey tool to their ICU nursing, respiratory therapy, and physician staff that they knew to be involved in the Hurricane Sandy ICU evacuation.
Study Tool
An electronic cross-sectional survey addressing ICU evacuation preparations and practices was developed by the study principal investigator. Content validity was ensured by focusing questions on issues raised in previous articles describing ICU evacuation.Reference Gildea and Etengoff 6 , Reference Sternberg, Lee and Huard 9 – Reference Manion and Golden 15 Consensual validity was achieved through the review of 7 internal medicine, critical care, and disaster response experts and serial adaptation of the questionnaire on the basis of their suggestions. The final structured questionnaire contained 23 items and included both open and closed questions (see Appendix 1 in the online data supplement).
Respondents were asked to provide demographic information including their job title or leadership position and their role during the hurricane. They next answered a series of questions using a 5-point anchored Likert scale on pre-event ICU planning and preparation, evacuation coordination and leadership, ICU evacuation processes, and major performance stressors. Vertical evacuation was a particular area of focus because of the prominent experience and challenge with critically ill patients in this area in other published disaster experiences.Reference Taylor 4 , Reference Sternberg, Lee and Huard 9 , Reference Schultz, Koenig and Lewis 11 , Reference Murphy and Foot 12 Finally, the respondents were asked to describe the key highlights of their disaster response experience in a series of open-ended questions including the following: (1) major successes, barriers, and problems that they encountered; (2) specific tools, supplies, and equipment that were helpful or missing; and (3) any ethical concerns that they encountered.
Study Population
Via a literature search of the press and through consultation with ICU physicians and private industry, we identified 7 New York area hospitals that had been forced to evacuate ICU patients as a result of infrastructural damage during Hurricane Sandy. In alphabetical order, those hospitals were (1) Bellevue Hospital, (2) Coney Island Hospital, (3) Good Samaritan Hospital, (4) Manhattan VA Medical Center, (5) New York Downtown Hospital, (6) NYU Langone Medical Center, and (7) Staten Island Hospital. The American College of Chest Physicians provided the research team with the contact details for the medical ICU directors of these institutions (telephone numbers and e-mails). All ICU directors were initially approached by e-mail, and 2 attempts to contact each were made by e-mail and phone. ICU directors who agreed to participate were asked to complete a questionnaire and to electronically distribute a similar survey to the nurses, respiratory therapists, and physicians who had played direct roles in the evacuation. The final sample size of the group was based on the principle of theoretical saturation in qualitative research.Reference Glaser and Strauss 16
Survey Method
A uniquely identified electronic version of the survey (SurveyMonkey, Palo Alto, CA) was e-mailed to each responding ICU director, who in turn distributed the survey to the relevant staff within the institution. The survey opened December 3, 2012, and closed March 28, 2013. All surveys were completed electronically and anonymously.
Data Collection and Statistical Analysis
Questionnaire responses were collected and analyzed by using Microsoft Office EXCEL 2007 (Microsoft Corp, Redmond, WA) and STATA 10.1 (STATA Corp, College Station, TX). Open-ended responses were coded for thematic penetrance by 2 independent reviewers. The number of interviewees repeating each comment was documented. Because there are common themes on evacuation between adult medical, pediatric, and neonatal ICUs, we decided to include all responses in our analysis. Descriptive statistics included counts and proportions. Percentages were calculated from the total number of respondents. Responses are presented primarily by aggregate totals to observe entire cohort trends and by individual hospital for ICU evacuation and leadership.
Results
Four medical ICU directors from 4 different hospitals that had evacuated their ICUs because of Hurricane Sandy agreed to participate in the study. Given the extenuating circumstances during December 2012 for many of these hospitals when this survey was distributed, the ICU directors were not asked to provide the number of staff members who received the questionnaire; hence, the survey denominator is unknown. Seventy-five medical professionals who had participated in the Hurricane Sandy ICU evacuation initially responded and 68 (91%) completed the questionnaire (hospital A=7, hospital B=11, hospital C=24, hospital D=26).
The demographics of the respondents are provided in Table 1. Most respondents (n=56, or 63%) worked in medical or mixed ICUs. Although we had targeted adult ICUs, 3% of the respondents stated that they were working primarily in neonatal or pediatric ICUs (n=2). More than one-third of the respondents were physicians (n=9 [13%] attending physicians and n=17 [25%] physicians-in-training). Almost half of the respondents were ICU nurses (n=24, or 35%) and respiratory therapists (n=14, or 21%). A third of the respondents (n=23, or 34%) held leadership roles during the ICU evacuation defined as (1) Incident Command leadership role, (2) ICU nursing manager (RN), or (3) ICU medical director (MD). The 23 respondents with leadership roles included 9 ICU nurses, 3 respiratory therapists, 7 ICU physicians, 1 chief resident, 2 ICU residents, and 1 chief medical officer.
Table 1 Provider Demographics by Provider Type, Unit Type, and Leadership Role During Hurricane Sandy ICU Evacuation, Both by Hospital and for Total RespondentsFootnote a

a Abbreviations: CMO, chief medical officer; ED, emergency department; ICU, intensive care unit; RT, respiratory therapist. The total number of respondents was 68.
ICU Evacuation Planning and Preparation
Responses on this topic are summarized in Table 2. Most respondents (n=41, or 61%) stated that their ICU had been at least “somewhat” involved in regional evacuation planning prior to Hurricane Sandy, and 51% of the respondents felt that they were at least “somewhat” adequately trained to evacuate ICU patients. In contrast, less than one-fourth of the respondents reported participating in an ICU evacuation drill in the past 2 years (n=11 [22%]; Figure 1), and among these, only 5 reported prior hands-on evacuation experience using actual equipment and simulated patients.

Figure 1 Responses to a Survey by Health Care Professionals Who Played Direct Roles in Hurricane Sandy ICU Evacuations. N=68 respondents. ICU, intensive care unit.
Table 2 Provider Responses to ICU Evacuation Planning and Preparation Questions, Both by Hospital and for Total RespondentsFootnote a

a Abbreviation: ICU, intensive care unit. The survey included questions on regional planning participation, ICU evacuation drills and prior experience, and evacuation training. The total number of respondents was 68.
Although all 4 hospitals housed their ICU patients above ground level, very few (n=19, or 28%) had any vertical evacuation training or prior experience. A total of 72% of respondents (n=48) reported that they had never participated in any type of vertical evacuation training or experience. As presented in Figure 2, despite the admitted lack of practical training or prior experience, only 23% of respondents (n=15) felt that they had been inadequately trained to perform a vertical ICU evacuation.

Figure 2 Responses to a Survey by Health Care Professionals Who Played Direct Roles in Hurricane Sandy ICU Evacuations. N=68 respondents. ICU, intensive care unit.
Almost two-thirds of the respondents (n=43, or 64%) were directly involved in patient preparation or actual patient transfer following Hurricane Sandy. Providers with more direct involvement in patient transfer during Hurricane Sandy were more likely to report that they felt adequately trained to perform these roles. Only 1 of the 16 respondents who prepared patients for transfer and 3 of the 17 responders who performed actual patient transfer felt inadequately trained. These individuals also felt better trained for vertical evacuation compared with respondents who were not directly involved in these activities. The 8 responders who provided direct vertical evacuation leadership, however, were more ambiguous regarding their preparation: 3 felt adequately trained, 3 felt inadequately trained, and 2 were neutral.
ICU Evacuation Coordination and Leadership
Most respondents (n=57, or 83%) felt that they had good situational awareness during the event (Supplemental Table 1 in the online data supplement). More than half (57%) mentioned teamwork as one of their primary successes, although the response varied among hospitals (A: 71%, B: 27%, C: 50%, D: 73%). By contrast, less than one-third of the respondents (29%) mentioned leadership as a primary success (A: 14%, B: 0%, C: 38%, D: 38%). Communication was identified as a major barrier to success by almost half (43%) of respondents (A: 43%, B: 27%, C: 54%, D: 38%), and 7% mentioned the lack of communication tools (ie, walkie-talkies/phones) as an additional barrier. Two-thirds of these ICU respondents (n=42, or 65%) felt that the ICU director should be the ICU evacuation leader rather than the chief medical officer, the Incident Commander, emergency medical services, federal authorities, or another source.
ICU Evacuation Processes
Details of survey responses are summarized in Table 3. Almost half of the respondents reported that patient triage and prioritization methods were primarily determined during rather than prior to the disaster (n=32, or 47%). A quarter reported that patient triage and prioritization was performed by using predetermined ICU criteria (n=16, or 24%), whereas the rest responded that triage was performed by using “other” criteria (n=8, or 12%) or random selection (n=2, or 3%). Some respondents (n=10, or 15%) were not privy to the triage process. Although the survey did not provide direct insight into the effectiveness of these triage practices, none of the respondents identified the patient distribution process as a primary success, and 6 of the respondents (5 from a single hospital) commented that they had to deal with ethical issues during patient distribution. One best practice identified through ICU director comments was the manual documentation of ICU resource requirements for each patient on a ruled pad of paper during evacuation. This documentation tool was considered essential by the respondents at that institution and was used iteratively during evacuation to provide real-time situational awareness of both patient numbers and resource requirements to inform distribution and transport decisions.
Table 3 Provider Responses to ICU Evacuation Process Questions, Both by Hospital and for Total RespondentsFootnote a
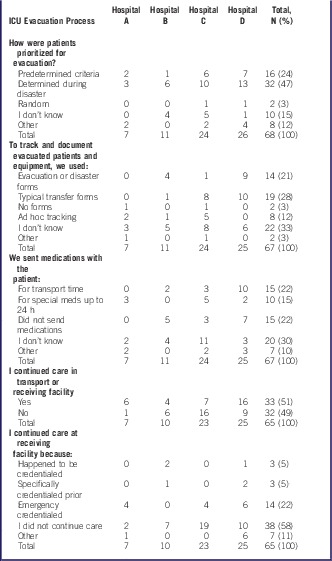
a Abbreviation: ICU, intensive care unit. The survey included questions on patient prioritization, patient tracking, medications, and delivering ongoing patient care in transport or at receiving facility. The total number of respondents was 68.
During transfer, providers more frequently used transfer forms (n=19, or 28%) common to their daily practice to track patients instead of special evacuation or disaster forms (n=14, or 21%). Some respondents reported “I don’t know” (n=22, or 33%) or no forms/ad hoc/other (n=12, or 18%) to this question, but interestingly, only 5% of respondents mentioned transfer records as a major barrier to successful patient transfer.
More than one-third of the respondents (n=25, or 37%) reported that they sent medications with patients for the immediate 24 hours after transfer. Over half of the respondents (n=33, or 51%) continued to provide patient care within their skill set either during transport or at the receiving facility, despite the fact that very few were credentialed (n=3, or 5%) or specifically pre-credentialed (n=3, or 5%) to perform these duties. Two thirds of the respondents who performed inter-facility patient transfer required emergency credentialing at the receiving facility (n=14, or 22%). Only 15% of respondents across all hospitals mentioned patient safety during the transfer process as a primary success.
Evacuation Tools
Respondents were asked to list which tools were most helpful during the evacuation process and which were most sorely missed. The responses to these questions are presented in Table 4. The most helpful ICU-specific equipment was transport sleds (21%) and oxygen tanks or respiratory therapy supplies (19%), and the most helpful general evacuation tools were flashlights (24%). The ICU-specific wish list most commonly included portable ventilators and suction (16%), whereas the general evacuation wish list included a greater variety of tools, eg, walkie-talkies/phones (26%), lighting/electricity (18%), and flashlights (10%).
Table 4 Main Evacuation Successes and Barriers and Tools, Equipment, and Systems Either Helpful or Needed as Identified by Respondents in Free Text and CategorizedFootnote a
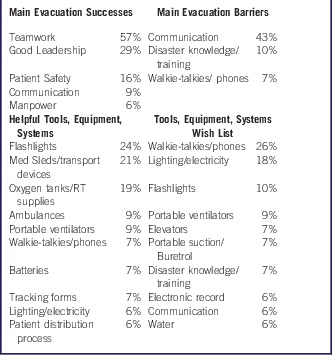
a Abbreviation: RT, respiratory therapy. Data are presented as the mean percentage of respondents mentioning each category and weighted by hospital.
Provider Performance Stressors
Respondents listed lack of water, food, and toilets; personal issues (eg, concern regarding family members); and limited appropriate means to dispose of the dead as major stressors affecting their performance during the ICU evacuation process.
Key Thematic Issues
Respondents identified a long list of key considerations in the survey comment section. These are presented in Supplemental Table 2 in the online data supplement.
Discussion
To our knowledge, this is the first study to systematically gather survey data from an interdisciplinary group of ICU providers from multiple institutions to analyze a regional evacuation response to a major disaster event. Our study had several strengths, including diligent pursuit of surveys within 4 months of the event, input from ICU providers from diverse disciplines who were directly involved in the ICU evacuation process, and the elaboration of themes concordant with reports on similar events. These facts allowed us to analyze our survey with some confidence to identify important associations and lessons that may help to inform future ICU evacuation practices. Although it has been suggested that practical equipment is integral to evacuation successes, ours is also the first study to highlight that flashlights, water, walkie-talkies, and other specific “wish list” items may be just as important as (if not more so) complicated ICU-specific equipment (such as transport ventilators).Reference Aghababian, Lewis and Gans 17 These small, simple tools may play a more significant role in successful ICU evacuations than previously appreciated and ICUs should be included in basic disaster tool planning.
Despite a number of natural disasters in recent years and an increasing emphasis on disaster preparedness by regulatory agencies like the Joint Commission, 18 our survey responses reflect common areas for improvement that have been raised by reports following similar events. Although most institutions surveyed had participated in regional evacuation planning and had significant advance warning of Hurricane Sandy’s landfall, leadership coordination and communication remained significant problems. Triage and prioritization decisions for ICU patient evacuation were generally still determined locally, and most providers performing these activities were not designated leaders and had little or no practical training. It is significant to note that institutional evacuation planning may not always involve the ICU director, because disaster preparedness efforts are often focused on the emergency department. This may create a management challenge for critically ill patients, who are generally the most vulnerable during an evacuation and frequently require specific subject matter expertise to effectively deliver their complex care. The insufficient and slow dissemination of critical information may contribute to continued challenges in creating efficient, streamlined disaster evacuations.
Given multiple reports of lack of regional coordination of hospital resources during disaster-induced hospital evacuationsReference Iwashyna, Christie and Moody 19 – Reference Kanter 24 as well as the numerous responses in this survey about the lack of patient distribution coordination, we recommend that disaster planning agreements include pre-event local mapping of regional critical care capacity, specialty resources, and ground and air transport with critical care capabilities. For large or late evacuations like Hurricane Sandy, these resources should be reported by each hospital within the region to a centralized Incident Command System or regional evacuation command center.Reference Burkle, Hsu and Loehr 25 The Incident Command System can determine how to best utilize the existing resources and will be responsible for coordination using stereotyped evacuation patterns based on volume, severity, and special needs of critically ill patients.Reference Fuzak, Elkon and Hampers 22 , Reference Born, Briggs and Ciraulo 26 Our survey results also suggest that continuity of provider care throughout the patient transfer process contributed to the overall perception of safer care. A priori regional credentialing of appropriate ICU staff as part of the overall disaster plan could avoid the challenges of emergency credentialing that the Hurricane Sandy ICU providers and hospitals faced.
System-wide cooperation should be encouraged and practiced, especially in health care systems that do not use a standardized coordinating system as part of their daily routine. Drills should include ICU providers in order to test command and communication systems and should include preparation and transport of simulated patients using actual transport equipment.Reference Gildea and Etengoff 6 , Reference Cybulski 7 , Reference Yurt, Lazar and Leahy 27 In our survey, the reported lack of concern with such technically challenging practices as vertical evacuation underlines the importance of systematic training, for which detailed recommendations and core competencies have already been published. 28 , 29 These drills would not only increase provider preparedness but also help to identify important tools that were missing in the Hurricane Sandy experience, such as flashlights, transport sleds, walkie-talkies or phones, portable ventilators, and suction.
The benefits of a systematic approach to patient prioritization and resource requirements demonstrated by the practical experience of one of the participating hospitals underlines the benefits of a evacuation preparation checklist and tracking system, which are readily available.Reference Hoskins, Graham and Robinson 30 – Reference Maltz, Ng and Li 35 Providers who are stressed will typically revert to familiar daily routines and processes. The fact that respondents more frequently reported the use of routine transfer forms over disaster forms represents either suboptimal preparation, with the potential for process improvement, or poor correlation between the content and structure of the forms and real-time documentation requirements. The use of disaster forms should be either reconsidered or studied more critically in simulated and real-time events. Lessons from Haiti and Toronto suggest that electronic tracking may be more effective than paper formsReference Callaway, Peabody and Hoffman 36 , Reference MacDonald, Farr and Neill 37 ; however, disaster conditions (such as those that existed in Hurricane Sandy) may necessitate a manual or paper version. If a decision is made to continue working with disaster forms, the staff should undergo appropriate training and routinely practice the use of these forms. Detailed planning and realistic drills using likely disaster scenarios increase successful individual performance.Reference Hoskins, Graham and Robinson 30 , Reference Verni 38 Communication and leadership are frequently cited challenges to effective ICU management and evacuation following a disaster. The experience from survey respondents following Hurricane Sandy highlights the importance of a critical care team or unit leader, who can maintain real-time situational awareness of the quantity, severity, resource requirements, special equipment, and transport needs of multiple critically ill patients and communicate this information effectively to the Incident Command System. The critical care unit leader role in the Hospital Emergency Incident Command System was eliminated under the new Hospital Incident Command System, and revision 28 , 29 , Reference Verni 38 of this change according to the Hurricane Sandy experience warrants serious consideration. Additionally, integration into the framework as defined by the Institute of Medicine’s Crisis Standards of Care may be beneficial for alignment with other regional hospitals and planning bodies.Reference Burkle, Hsu and Loehr 25 , Reference Powell, Hanfling and Gostin 39 , 40
Our survey did not delve into specific assessment of post-traumatic stress or dysfunction. We highlighted some of the ethical obstacles identified by providers, but did not address their functional status or stress symptoms at the time of the survey, which would have been a ripe opportunity to assess long-term effects of such evacuations. We also did not allow providers to self-rate their performance in terms of patient care, although responses in support of excellent patient safety outcomes indirectly addressed this. A complete description and analysis of the complex events and ICU evacuation responses following Hurricane Sandy is clearly not possible by using a simple survey tool. Owing to financial limitations and sheer geographic distance, we were forced to conduct our study remotely. A major limitation to our study was the participation of only 4 of 7 area hospitals affected by this storm, and the associated risk of selection and response biases. Although we attempted to highlight a variety of subspecialty ICU types, we primarily captured responses from medical ICUs as a result of the sampling methods. Future studies could aim to provide more responses from neonatal, pediatric, medical, cardiac, and other ICUs.
Responses by certain specialty providers, such as respiratory therapists, may have biased the prioritization of some of the tools on the wish lists, for example. Even among the hospitals that agreed to participate, we encountered significant limits to available data due to respondent concern regarding the appropriate use of this information. Outside providers, such as emergency medical services or purely administrative staff, were not queried but might provide a different perspective on the events. By definition, data collected in a disaster situation are frequently limited and nonuniform, raising concerns regarding the public relations and medical-legal ramifications of submitting this information to public scrutiny. Developing clear guidelines for minimum elements of data collection to consider in these situations and an anonymous reporting system at the national or international level may help to facilitate more comprehensive study and understanding of best practices for ICU evacuation that may aid providers and improve patient outcomes in future disaster events.
Conclusions
The experiences shared by ICU providers involved in the response to Hurricane Sandy identified themes common with other published literature in this area. Disaster planning and preparation at the ICU level continues to represent an area for improvement, especially in the area of vertical evacuation. Early initiation of patient evacuation efforts led to greater communication and coordination both within and between hospitals, but still left room for improvement in the areas of communication and leadership, especially in the area of patient distribution. Triage, prioritization, and documentation processes were highly variable, and emergency credentialing was frequently necessary to provide patients with the care that they needed during and after transport to new facilities. Phones, flashlights, and portable ventilators are important, high-yield resources that could be targeted for preparation in the event of future ICU evacuations. Many other areas for improvement above could be addressed by better efforts to incorporate ICU providers into hospital evacuation planning and training efforts. A possible solution to improve the ICU processes observed in this event includes the creation of standardized evacuation communication processes and documentation tools, managed by a critical care unit leader who coordinates care and plays a defined and integrated role in the Incident Command System. The development of a standard, uniform database utilized by all evacuating hospitals during a disaster could also better inform patient and system outcomes to further advance critical care evacuation practices in the future.
Acknowledgments
We would like to especially acknowledge the willingness and effort of the ICU medical directors who helped facilitate the participation of their ICU staff as well as the ICU providers themselves who were willing to share their experiences with the medical community. We also thank Dr Asha Devereaux, Dr Jeffrey Dichter, and Dr Jeffrey Upperman for their guidance and expertise in generation of the survey questions.
Supplementary Material
To view supplementary material for this article, please visit http://dx.doi.org/10.1017/dmp.2015.94








