Introduction
Self-harm is associated with a greater risk of premature death, especially by suicide (Bergen et al., Reference Bergen, Hawton, Waters, Ness, Cooper, Steeg and Kapur2012b). Previous research has shown that certain methods of self-injury are associated with an elevated risk of subsequent death by suicide when compared to self-harm by poisoning (Bergen et al., Reference Bergen, Hawton, Waters, Ness, Cooper, Steeg and Kapur2012a; Geulayov et al., Reference Geulayov, Casey, Bale, Brand, Clements, Farooq and Hawton2019; Runeson, Haglund, Lichtenstein, & Tidemalm, Reference Runeson, Haglund, Lichtenstein and Tidemalm2016; Runeson, Tidemalm, Dahlin, Lichtenstein, & Långström, Reference Runeson, Tidemalm, Dahlin, Lichtenstein and Långström2010). However, findings in relation to self-cutting and risk of subsequent suicide have been mixed (Bergen et al., Reference Bergen, Hawton, Waters, Ness, Cooper, Steeg and Kapur2012a; Olfson et al., Reference Olfson, Wall, Wang, Crystal, Gerhard and Blanco2017; Runeson et al., Reference Runeson, Tidemalm, Dahlin, Lichtenstein and Långström2010, Reference Runeson, Haglund, Lichtenstein and Tidemalm2016) although in all of these studies the risk of suicide in patients who presented to hospitals for self-cutting or stabbing was comparable to the risk of suicide following self-harm by poisoning. Recent studies suggest that individuals who cut themselves are a heterogeneous group who vary by the method of laceration (e.g. site of cut and severity of self-cut injury), the involvement of other methods of self-harm, their psychopathology as well as gender and age and thus their outcomes may vary.
Self-cutting often involves the wrist and arm, but cuts to other parts of the body are also common. Laukkanen, Rissanen, Tolmunen, Kylma, and Hintikka (Reference Laukkanen, Rissanen, Tolmunen, Kylma and Hintikka2013) found that self-cutting on parts of the body other than the arm was associated with female gender, more severe psychiatric symptoms and suicidal ideation relative to self-cutting on the arm. A study on adolescents (Gardner et al., Reference Gardner, Bickley, Turnbull, Kapur, Taylor and Clements2020) has shown that concealed self-cutting was associated with previous self-harm, current psychiatric treatment and greater risk of self-harm repetition. A single-site study (Carroll et al., Reference Carroll, Thomas, Bramley, Williams, Griffin, Potokar and Gunnell2016) found that suicide risk was 4.5 times greater after cutting to areas other than the wrist/arm relative to self-poisoning. No suicides by individuals who presented to hospital after self-cutting the wrist or arm were observed so it is not clear how the site of laceration compares in terms of suicide risk. However, this study was relatively small, involving a short follow-up (mean of 2 years), during which 27 deaths by suicide were identified. In another study, investigators showed a comparable risk of death by either suicide or a cause other than suicide in patients who presented to hospitals for self-cutting to the wrist or arm alone, those who self-cut elsewhere than wrist or arm, and in patients who had self-poisoned. However, this study was also relatively small, including 69 suicides in total (Birtwistle, Kelley, House, & Owens, Reference Birtwistle, Kelley, House and Owens2017).
Using data from the Multicentre Study of Self-harm in England, we aimed to (a) describe the characteristics of patients who had presented to general hospitals following self-cut or stab according to site of laceration, and (b) investigate the relative risk of death by suicide in relation to site of self-cut or stab. We distinguished between those who cut their wrist or arm v. another site. This division was consistent with previously published research (Carroll et al., Reference Carroll, Thomas, Bramley, Williams, Griffin, Potokar and Gunnell2016; Morey, Mellon, Dailami, Verne, & Tapp, Reference Morey, Mellon, Dailami, Verne and Tapp2017). We further examined patients' characteristics and outcomes according to specific site of self-cut or stab (e.g. neck and leg).
Method
This observational cohort study is based on data from the Multicentre Study of Self-harm in England. It includes follow-up for mortality through record linkage to the national mortality register. Information on site of self-cut or stab was available for presentations occurring between 2004 and 2014; followed-up for mortality until 31.12.2019.
Study setting and participants
The Multicentre Study is an ongoing study which involves five general hospitals from three cities in England: Oxford (one hospital), Manchester (three hospitals) and Derby (two hospitals until 2009, subsequently merged into one hospital). All presentations to the emergency departments following an episode of non-fatal self-harm between 1 January 2004 and 31 December 2014 were included. We included individuals aged 10 years or older at their first recorded hospital attendance.
Information on demographic and clinical characteristics of patients was collected through either (a) psychosocial assessments (of the patient's mental state, risks and needs) by specialist psychiatric clinicians in the general hospital, or (b) for patients who had not received a psychosocial assessment, through data extracted from emergency department electronic databases by trained staff. The latter yields less complete information.
We used an episode-based approach, a method which we used previously (Geulayov et al., Reference Geulayov, Casey, Bale, Brand, Clements, Farooq and Hawton2019). Patients who self-cut tend to repeat self-harm more often than patients using other methods (Larkin, Di Blasi, & Arensman, Reference Larkin, Di Blasi and Arensman2014; Lilley et al., Reference Lilley, Owens, Horrocks, House, Noble, Bergen and Kapur2008). Therefore, including all episodes in the analysis rather than selecting a single (index) episode is imperative.
Measures
Non-fatal self-harm
Refers to any act of intentional self-poisoning or self-injury, irrespective of the nature of the motivation including degree of suicidal intent (Hawton et al., Reference Hawton, Hall, Simkin, Bale, Bond, Codd and Stewart2003). Self-poisoning includes the intentional ingestion of any drug in an amount that is more than that prescribed or recommended, the ingestion of non-ingestible substances, or overdoses of ‘recreational drugs’ and severe alcohol intoxication where clinical staff consider this to be an act of intentional self-harm. Self-injury is defined as any injury that has been intentionally self-inflicted.
Self-harm episodes are identified through (a) completion of monitoring forms on all self-harm patients assessed by the general hospital psychiatric service and (b) scrutiny of emergency department electronic databases by research clerks using a detailed protocol in order to identify all other patients presenting to the hospital following self-harm who have not been assessed.
Site of laceration
We grouped episodes as follows (groups are mutually exclusive): (1) self-cut or stab to wrist or arm alone (which could include either or both sites within this category); (2) self-cutting or stabbing to other (than wrist or arm) bodily part/s involved (may also include laceration to wrist or arm in addition to other sites); (3) self-cut or stab to unknown site; (4) other method of self-injury and (5) self-poisoning alone.
In a subsequent analysis we also grouped episodes according to the specific site of laceration: (1) head; (2) neck; (3) torso; (4) wrist or arm; (5) leg; (6) groin; (7) other (e.g. genitals) and (8) unknown site. Each group may include episodes in which the person lacerated only the specific site of interest or the site of interest in combination with an additional site (i.e. not mutually exclusive groups; although they were mutually exclusive in relation to the reference group of patients who present to the hospital after self-poisoning alone).
Information on the specific site of self-cut was collected in Oxford during 2004–2014, in Manchester in 2005–2011 and in Derby in 2004–2013.
History of self-harm
Patients were assigned a positive status if they had a previous recorded presentation to the hospital in the study database, reported previous self-harm during their psychosocial assessment or were identified with a prior self-harm episode through the hospital electronic records.
Psychiatric care
Patients who were identified as having previously received or currently receiving psychiatric treatment in a specific episode through either their psychosocial assessment or the hospital electronic records were assigned a positive status in this and for all subsequent episodes. A negative status was assigned to patients who had no record of psychiatric treatment through any of these sources. Otherwise, this item was considered as not known.
Linkage to mortality register
Information on mortality was obtained through record linkage with data from NHS Digital. Follow-up for mortality was until 31.12.2019. Individuals were followed up for a minimum of 5 years and a maximum of 15 years. Cause of deaths was based on the International Statistical Classification of Diseases and Related Health Problems version 10 (ICD-10). ICD-10 codes of intentional self-harm (codes X60–X84) or death due to undetermined intent (codes Y10–Y34) were defined as suicide deaths, as currently practiced in the UK (Gunnell et al., Reference Gunnell, Bennewith, Simkin, Cooper, Klineberg, Rodway and Kapur2013; Linsley, Schapira, & Kelly, Reference Linsley, Schapira and Kelly2001; Office for National Statistics, 2015).
Ethical approval
The monitoring systems in all three research sites have approval to collect data on self-harm for local and multicentre projects. The monitoring systems in Oxford and Derby have approval from local National Health Service (NHS) Research Ethics Committees. Self-harm monitoring in Manchester is part of a clinical audit system, and has been ratified by the local Research Ethics Committee. All three monitoring systems are fully compliant with the Data Protection Act 1998. All centres have approval under Section 251 of the NHS Act 2006 to collect patient identifiable information without patient consent. Each of the three centres holds a data-sharing agreement with NHS Digital to conduct mortality linkage with respect to their cohort.
Statistical analyses
Observations were excluded if patients had missing information on gender, age or mortality (lost to follow-up) or if their cause of death was unknown (Fig. 1).
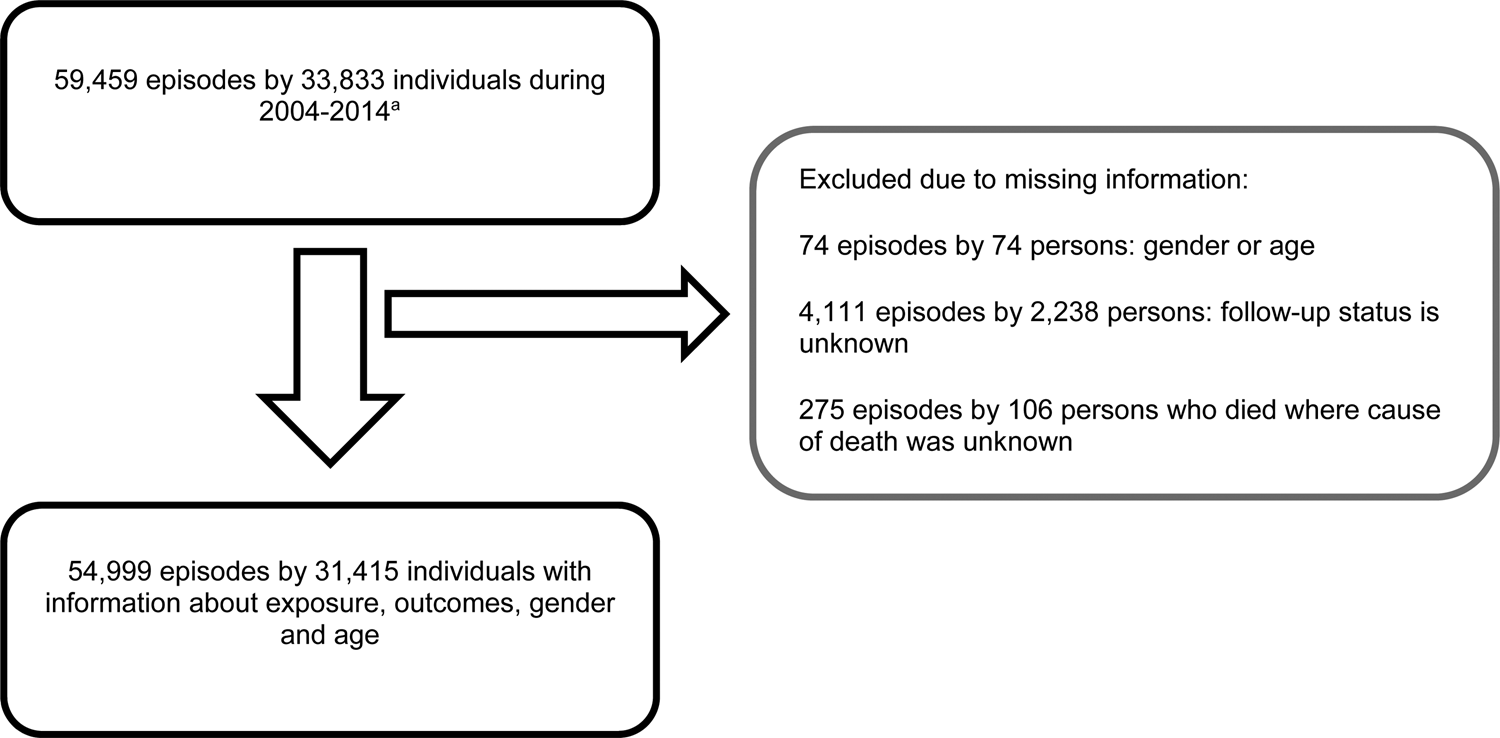
Fig. 1. Sample selection process. aOxford includes data on presentations to hospital which occurred during 2004–2014, Manchester 2005–2011, Derby 2004–2013.
The characteristics of patients who were included and excluded from the analysis were compared using analysis for categorical and continuous variables as appropriate (online Supplementary Table S1).
We used mixed-effect logit regression models to examine the associations between site of self-cut at hospital presentation and subsequent suicide. All episodes of self-harm were used in these regression analyses with suicide as the dependent variable and random intercepts at the patient level to account for clustering of episodes in patients.
Two sets of models were run: (1) comparing the likelihood of suicide after hospital presentation for self-harm in patients who self-cut/stab to wrist/arm, self-cut/stab elsewhere on the body (regardless of whether or not self-cut/stab to wrist/arm was also involved), other self-injury or self-poisoning alone; and (2) comparing the likelihood of suicide in patients who self-cut or stab by specific site of self-cut or stab (wrist/arm, neck, torso; see list above) relative to self-harm by poisoning.
Unstructured covariance of multiple episodes per patient was specified. Post-estimation intraclass correlation coefficients (ICCs) were used to estimate the amount of variation accounted for by the latent variable (patient). Likelihood ratio tests indicated that clustering of patients in hospitals was not required. Gender, age (in years), previous self-harm, psychiatric treatment and hospital were included as covariates unless otherwise specified. These covariates were selected a priori as they have been shown to influence suicide risk and were associated with the exposure variables of interest (Rudd et al., Reference Rudd, Berman, Joiner, Nock, Silverman, Mandrusiak and Witte2006).
We further examined suicide risk by time of follow-up including first year and 4-year suicide risks after hospital attendance for self-harm.
Sensitivity analyses
(1) We re-ran the models using data from 2005 to 2011 only because data in one centre were available for this period only, allowing for an equal follow-up period for patients in the three centres.
(2) We excluded patients if their history of self-harm was unknown. This variable was missing for ~20% of self-harm episodes.
(3) We further examined the impact of excluding episodes where psychiatric treatment was unknown, also missing for ~20% of self-harm episodes.
(4) Episodes which also involved self-poisoning (4.7% of episodes) were excluded in order to examine how site of self-cutting/stabbing alone relates to suicide.
(5) We re-ran the analysis using penalised maximum likelihood regression to explore a possible sparse data bias.
Analyses were carried out using Stata 14.2.
Results
During the study (2004–2014), there were 59 459 presentations to the study hospitals by 33 831 patients. Patients who were missing information on age or gender (74 episodes by 74 patients), follow-up for mortality (4111 episodes by 2236 patients) and cause of death (275 episodes by 106 persons) were excluded resulting in 31 415 patients involved in 54 999 presentations to the study hospitals (93% of the intended sample, see Fig. 1).
A comparison between included and excluded individuals is shown in the Appendix (online Supplementary Table S1).
Sample characteristics
Over two-thirds (69%) of presentations to the hospital in 10–24-year-olds were by females, decreasing to a little over 50% in older patients (Table 1).
Table 1. Characteristics of patients who presented to hospitals for self-harm between 2004 and 2014a
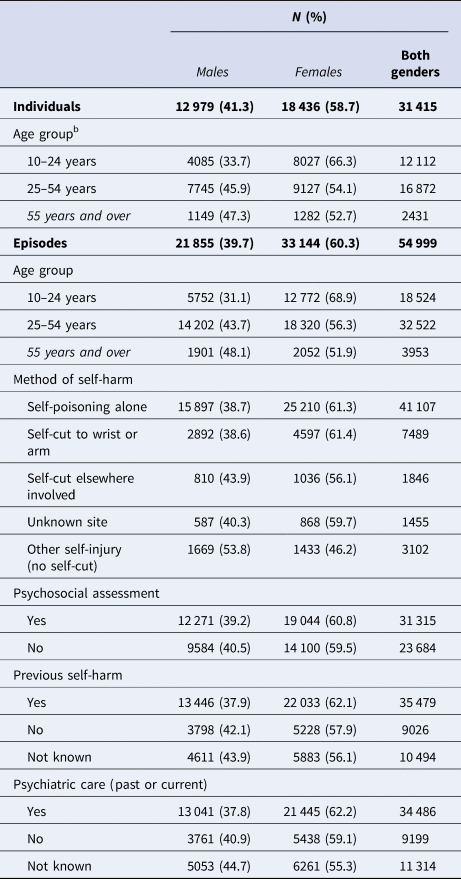
The majority of episodes involved self-poisoning alone (41 107/54 999, 74.7%), 61.4% by females. A further 7489 episodes (13.6%) were due to laceration to the arm or wrist (61.4% by females), whereas 1846 episodes (3.4%) involved cutting or stabbing elsewhere on the body (56.1% by females). In 1455 episodes (2.7%) the site of cut or stab was unknown (59.7% by females). The remaining episodes (3102, 50.6%) were due to self-injury other than cutting or stabbing (46.2% by females).
Characteristics of patients who self-cut/stab
In total, 61% of patients who self-cut or stab their wrist or arm alone were females (the same proportion as for self-poisoning). Females represented 56% of patients whose cut or stab involve other bodily sites (Table 1).
Although based on small numbers, of note is the greater involvement of males than females in intentional cut or stab to their neck (4.8% v. 2.4%), head (3.2% v. 1.5%) and torso (6.2% v. 4.1%) (all p < 0.0001). The involvement of leg in cutting was more common in females (8.6%) than in males (6.2%) (p < 0.0001). The proportion of patients who presented after a cut or a stab to more than one part of the body was similar in the two genders (Table 2).
Table 2. Characteristics of patients who presented to hospitals for self-cut/staba
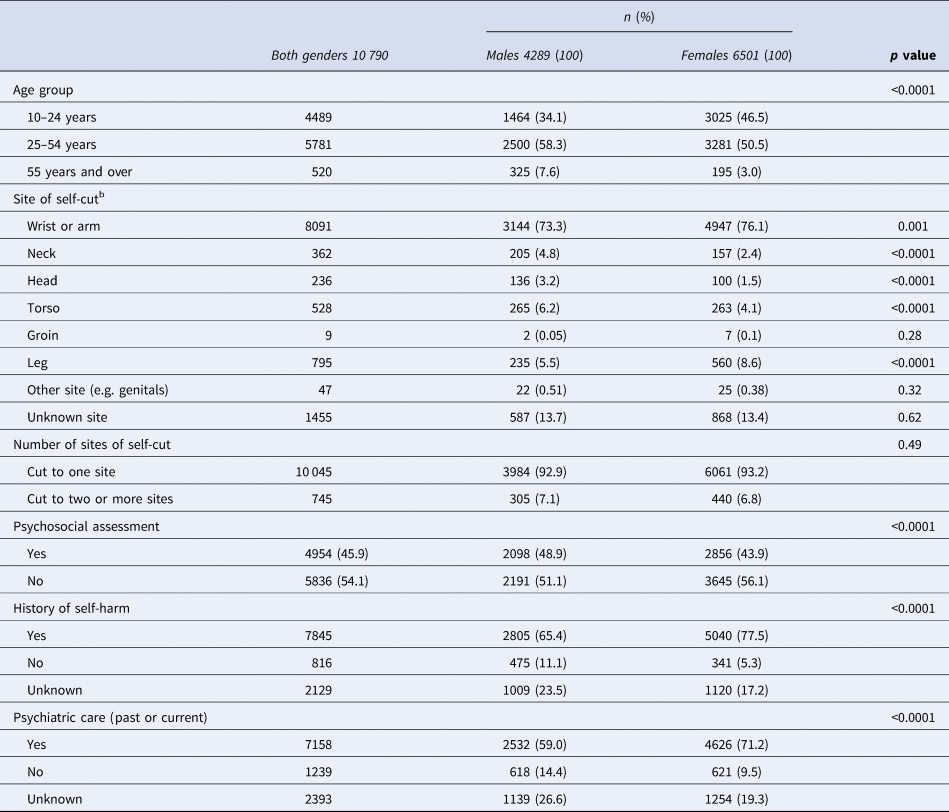
Numbers and percentages are displayed by episodes.
a Includes only patients who self-cut.
b Episodes may involve more than one site.
The involvement of sites other than wrist/arm was more common in patients of 55 years and older (120/520 episodes, 23.1%) than in 15–24-year-olds (705/4489 episodes, 15.7%) (results not shown).
The proportion of patients who were currently receiving psychiatric treatment and/or had done so in the past was 70% among those whose cut or stab involved another bodily site (other than wrist or arm) relative to 65% in those cutting their wrist or arm. The age distribution and history of previous self-harm were similar in these two groups (online Supplementary Table S2).
Site of cut or stab and subsequent suicide
Site of cut/stab was associated with a likelihood of subsequent suicide (Table 3). Presenting to the hospital with self-cut or stab to bodily parts other than wrist or arm was associated with 1.8-fold greater chance of subsequent suicide relative to presenting to the hospital after self-poisoning alone [odds ratio (OR) 1.83, 95% confidence interval (CI) 1.10–3.03, p = 0.02]. This was also the case after adjusting for gender, age, previous self-harm, psychiatric care and hospital [adjusted OR (aOR) 1.75, 95% CI 1.03–2.96, p = 0.038]. The likelihood of death by suicide after presentations to the hospital for cut or stab to the wrist or arm alone (not involving other sites of self-cut or stab) was comparable to that observed after self-poisoning alone.
Table 3. Likelihood of suicide following presentation to hospital for self-harm by site of self-cut, mixed effect logistic regression, N = 54 999 episodes
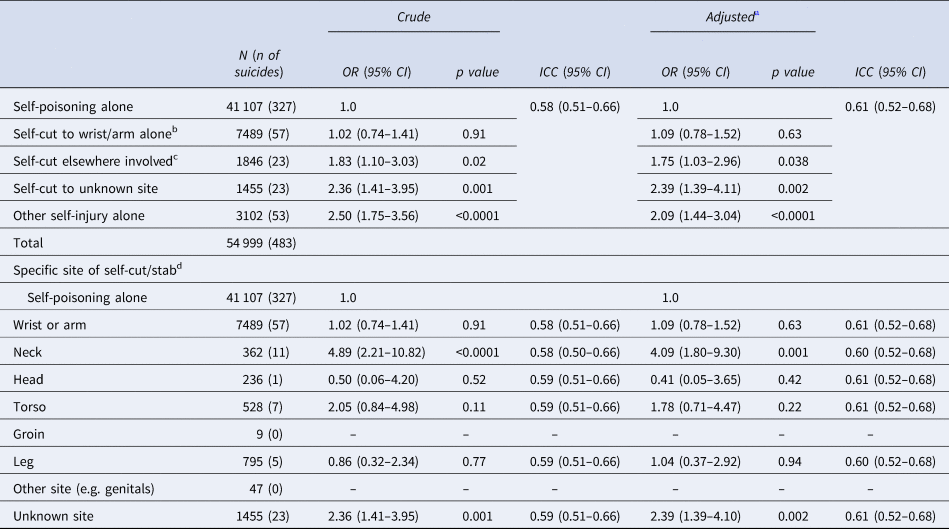
ICC, interclass correlation coefficient.
a Adjusted for age (in years), gender, previous self-harm, psychiatric treatment and hospital.
b Self-cut or stab involved only arm and/or wrist but no other bodily parts.
c Presentations involving cutting or stabbing elsewhere on the body (than wrist or arm). Could also be in combination with wrist or arm in the same episode.
d Relative to presentations to hospital after self-poisoning alone.
Controlling for confounders, the likelihood of death by suicide following cut or stab to an unknown bodily site was higher relative to that of patients who had attended hospital for self-poisoning alone (aOR 2.39, 95% CI 1.39–4.11, p = 0.002).
Specific site and subsequent suicide
Compared to hospital attendances after self-poisoning alone, presentation after laceration involving the neck was associated with a four-fold greater chance of subsequent suicide after adjusting for covariates as above (aOR 4.09, 95% CI 1.80–9.30, p = 0.001) (Table 3). Hospital attendance after cut or stab to all other specific sites showed that the likelihood of suicide in relation to these sites of self-cut or stab was comparable to that observed for after self-poisoning alone.
There was no evidence for gender differences in risk of suicide according to site of self-cut or stab although the gender specific models were based on small groups.
The ICCs ranged between 0.58 and 0.61 (Table 3), indicating a moderate correlations between episodes within the patient cluster variable (i.e. episodes of the same person resemble each other).
Suicide following self-harm by time of follow-up
One-year risk of suicide
In total, 201 suicides occurred within the first year after hospital attendance. Relative to presentation to hospital after self-poisoning alone, the likelihood of suicide was higher in relation to presentations which involved intentional cutting or stabbing to bodily parts other than wrist or arm alone (aOR 2.28, 95% CI 1.05–4.92, p = 0.037). Presentations to the hospital after lacerations to wrist or arm were associated with a comparable suicide risk to that of patients who self-poisoned (aOR 1.04, 95% CI 0.60–1.80, p = 0.88) (online Supplementary Table S3).
Four-year risk of suicide
In total, 333 suicides were recorded within the first 4 years of hospital attendance. The likelihood of suicide was higher after presentations to the hospital which involved self-cutting or stabbing elsewhere than wrist or arm alone (aOR 1.82, 95% CI 0.98–3.38, p = 0.058). Presentations after lacerations to wrist or arm had a comparable suicide risk to presentations after self-poisoning alone (aOR 1.23, 95% CI 0.83–1.82, p = 0.31).
The heightened suicide risk after hospital attendance for self-cut or stab to the neck was evident 1-year after the episode (aOR 3.49, 95% CI 0.93–13.14, p = 0.07) and after 4 years (aOR 3.48, 95% CI 1.29–9.37, p = 0.014), adjusting for covariates as above although at 1-year the p value exceeded the conventional significance level. However, the effect estimates were almost identical at the two follow-up time points (online Supplementary Table S3).
Sensitivity analyses
Online Supplementary Table S4 shows the findings from the sensitivity analyses (see online Supplementary material).
Using the data of patients who had presented during 2005 and 2011 (25 790 patients involved in 43 286 presentations to the hospital for self-harm) was in keeping with the findings from the main analysis.
Excluding episodes where information on previous self-harm or psychiatric care was missing resulted in attenuated effect estimates of some but not all models. For example, after excluding the data of patients whose previous self-harm status was unknown, the involvement of cut or stab to bodily parts other than the wrist or arm was associated with a higher likelihood of subsequent death by suicide but after adjustment for confounders the association was not statistically significant at the conventional significance level (aOR 1.65, 95% CI 0.89–3.04, p = 0.11). Nevertheless, the increase in the risk of subsequent suicide in patients who presented to the hospital for intentional cut or stab to their neck was not attenuated after excluding patients with missing information on previous self-harm or psychiatric care (e.g. adjusted model excluding episodes where previous self-harm was not known: aOR 4.92, 95% CI 2.03–2.89, p < 0.0001).
Excluding episodes which also involved self-poisoning (4.7% of episodes) showed that the risk of suicide was greater in relation to episodes involving self-cutting or stabbing elsewhere than wrist or arm but the association was not statistically significant after adjustment for confounders (aOR 1.65, 95% CI 0.92–2.94, p = 0.09). Nevertheless, the risk of subsequent suicide in patients who presented to the hospital for intentional cut or stab to their neck was in keeping with the findings from the main analysis (aOR 4.60, 95% CI 1.92–11.03, p = 0.001).
Furthermore, the results from models in which we included only presentations which occurred in 2005–2011 (overlapping period in all three centres) were consistent with findings from the main analyses also after excluding the above sub-groups. For example, the involvement of a cut or stab to sites other than wrist or arm was associated with a heightened suicide risk after self-harm after excluding patients whose episode of self-cut or stab also involved self-poisoning (aOR 2.08, 95% CI 1.11–3.88, p = 0.021) (online Supplementary Table S4).
Discussion
We estimated the likelihood of subsequent death by suicide in patients attending hospitals for self-harm according to the bodily site of self-cut or stab relative to patients who self-poisoned. Self-cutting varied considerably from cuts or stab to one's wrist or arm to laceration to the neck, head or torso. Self-cutting or stabbing to neck, head and torso were more common among males compared to females while cutting or stabbing wrist or arm and leg were slightly more common among females. The likelihood of subsequent death by suicide in patients who present to the hospital after self-cutting or stabbing to their wrist or arm was comparable to that of patients who had presented to the hospital after self-poisoning. The likelihood of subsequent death by suicide in patients whose cutting or stabbing involved other bodily parts was almost twice that of patients who had attended hospitals after self-poisoning.
Similarly, findings froman earlier relatively small study (Carroll et al., Reference Carroll, Thomas, Bramley, Williams, Griffin, Potokar and Gunnell2016) showed that lacerations to bodily parts other than wrist or arm were associated with an increased risk of suicide relative to self-poisoning, although the investigators did not compare the risk of death by suicide in relation to lacerations to the wrist or arm since no suicides were observed in this group at the time follow-up ended. In the current study, however, we were also able to compare laceration to wrist/arm with self-harm by poisoning (a comparison which, to the best of our knowledge, has not been reported before). Our long follow-up and the large sample enabled us to also observe suicide in patients who lacerated their wrist or arm (as well as other specific sites of cutting). The estimated increase in the risk of suicide in individuals whose laceration involved other parts of the body (than the wrist or arm) in our study was considerably smaller than that reported by Carroll et al. (Reference Carroll, Thomas, Bramley, Williams, Griffin, Potokar and Gunnell2016). This could be attributed to several methodological differences. We used all hospital presentations and accounted for multiple episodes by some individuals statistically while other studies have tended to base their estimates of suicide risk on person's first recorded presentation to the hospital. Differences in the duration of follow-up may have also accounted for the above; it has been shown that the risk of suicide varies by time since hospital attendance, with suicide risk being particularly high nearer the time of hospital attendance for self-harm (Cooper et al., Reference Cooper, Kapur, Webb, Lawlor, Guthrie, Mackway-Jones and Appleby2005; Geulayov et al., Reference Geulayov, Casey, Bale, Brand, Clements, Farooq and Hawton2019; Hawton et al., Reference Hawton, Bergen, Cooper, Turnbull, Waters, Ness and Kapur2015; Kuo, Gunnell, Chen, Yip, & Chen, Reference Kuo, Gunnell, Chen, Yip and Chen2012). In a further analysis, we estimated the 1-year and the 4-year risks of suicide after hospital attendance. The estimates from these analyses were consistent with those of the main analysis.
Previous studies have shown that patients who cut elsewhere than wrist/arm show more severe psychopathology (Gardner et al., Reference Gardner, Bickley, Turnbull, Kapur, Taylor and Clements2020; Laukkanen et al., Reference Laukkanen, Rissanen, Tolmunen, Kylma and Hintikka2013; Morey et al., Reference Morey, Mellon, Dailami, Verne and Tapp2017). More severe psychopathology may have contributed to the higher risk of suicide in patients whose laceration involved bodily parts other than their wrist or arm. In our study, we found that 70% of patients whose laceration involved another bodily part have been in contact with psychiatric care relative to 65% of patients who cut their wrist or arm with no involvement of other sites. However, our analysis has shown that cutting or stabbing to other bodily parts was associated with a greater risk of suicide after accounting for psychiatric care although the finding that information on psychiatric care was missing for 20% of patients and that this was higher among the non-assessed and hence more so among patients who self-cut (whose assessment rate is lower than that for patients presenting after other methods of self-harm) suggest that our findings need to be interpreted with caution.
It may be that suicidal intent varies by the site of self-cut. Suicide intent may explain some of the variation in characteristics and adverse outcomes and may be an important subject of future research. However, it should be highlighted that individuals who self-harm without, or with low suicidal intent, may also die by suicide and that these patients are also at risk of other adverse outcomes relative to the general population (Carroll et al., Reference Carroll, Thomas, Bramley, Williams, Griffin, Potokar and Gunnell2016; Mars et al., Reference Mars, Heron, Crane, Hawton, Lewis, Macleod and Gunnell2014).
It is commonly assumed that individuals who self-cut are less likely than other patients who self-harm to die by suicide. Self-cutting is often referred to as non-suicidal self-injury (Taylor et al., Reference Taylor, Jomar, Dhingra, Forrester, Shahmalak and Dickson2018). However, studies from various countries show that the risk of suicide in patients who self-cut or stab is comparable (Olfson et al., Reference Olfson, Wall, Wang, Crystal, Gerhard and Blanco2017; Runeson et al., Reference Runeson, Tidemalm, Dahlin, Lichtenstein and Långström2010) or even higher (Bergen et al., Reference Bergen, Hawton, Waters, Ness, Cooper, Steeg and Kapur2012a; Runeson et al., Reference Runeson, Haglund, Lichtenstein and Tidemalm2016) than that of many other patients who self-harm using other methods. Evidence from previous studies has shown that many patients who attend hospitals following self-harm are discharged without appropriate evaluation or a care plan. Of particular concern is the finding that individuals who self-cut are less likely than patients using other methods of self-harm to receive psychosocial assessment when presenting to the hospital (Bennewith, Peters, Hawton, House, & Gunnell, Reference Bennewith, Peters, Hawton, House and Gunnell2005; Geulayov et al., Reference Geulayov, Kapur, Turnbull, Clements, Waters, Ness and Hawton2016; Kapur et al., Reference Kapur, Murphy, Cooper, Bergen, Hawton, Simkin and Owens2008).
It is important to recognise that all patients who self-harm carry a significant risk of subsequent suicide. Using data from the Multicentre Study of Self-harm, we have shown that patients who present to hospitals for self-harm are 50 times more likely to die by suicide relative to the general population, and that this risk was as high as 175 times greater during the first month after hospital attendance (Geulayov et al., Reference Geulayov, Casey, Bale, Brand, Clements, Farooq and Hawton2019). Thus, clinicians who encounter patients who self-harm need to provide a comprehensive psychosocial assessment and jointly plan follow-up care which is tailored to patient's needs. This includes all patients who cut themselves. Of note is the particularly high suicide risk in patients who present to the hospital following cut or stab to their neck. It is worth highlighting that self-harm which occurs in the community and which may or may not result in presentation to hospitals or other healthcare facilities often involves self-cutting. Little is known about the risk of death by suicide of this group of individuals and how it compares with other methods of self-harm and with that of patients who self-cut and whose self-harm result in hospital attendance. Furthermore, their care needs are also poorly understood.
Strengths and limitations
This is a large multicentre study which spans over 15 years. This allowed us to accrue a sizable group of patients who had presented to hospitals after self-cutting or stabbing bodily sites which are less commonly observed. This study also includes a socioeconomically diverse population (Geulayov et al., Reference Geulayov, Casey, Bale, Brand, Clements, Farooq and Hawton2019). Furthermore, data on mortality were obtained through a national register which means that we were less likely to have missed information about suicides which may have occurred outside the catchment areas involved in this study. However, it is limited in several ways.
For 13.5% of episodes where self-cutting or stabbing was recorded as the method of self-harm, there was no further information about the site of cut or stab. Those patients were more likely than patients who had presented to hospitals after self-poisoning alone to die by suicide by the end of follow-up. In this group, the proportion of patients who had received a psychosocial assessment following their presentation to hospitals was 39% relative to 47% of patients who presented after cutting or stabbing to arm or wrist and 49% whose presentation involved a site other than wrist or arm (online Supplementary Table S2).
For about 20% of presentations information on previous self-harm and psychiatric care was missing. Further examination of our data has shown that the proportion of assessed episodes and hence the proportion of missing information on these two variables was disproportionately higher for patients who had self-cut. This is because, as noted above, this method of self-harm is least likely to result in an assessment during hospital attendance.
Our analysis of the association between specific sites of cut or stab and suicide relies on some small groups so the possibility of sparse data bias should be acknowledged. However, we assessed the possible sparse data bias using penalised maximum likelihood regression models and the estimates from these were consistent with those of the main analysis.
Furthermore, for each centre information was available for a different period of time. This is because the centres collected this additional information as part of their core variables during different periods. As we mentioned above, we addressed this by excluding the data for non-overlapping periods, the results of which led to the same conclusion.
Finally, we did not have very detailed information about the nature of the self-cut act. Thus, we could not distinguish between self-cutting and self-stabbing as these were recorded as a single group. Furthermore, we did not have information about the depths and severity of the lacerations or the number of cuts because this information was not recorded in the raw data. Risk of suicide may vary between these different methods.
Conclusions
Patients who cut or stab themselves and attend the hospital are a heterogeneous group. Although some present to hospitals after relatively superficial lacerations others may attend due to lacerations which could be more severe and potentially life threatening. The bodily parts involved in the act of self-cut or stab also vary from lacerations to the arm or wrist to those involving the head, neck and abdomen. Patients' characteristics as well as their risk of subsequent death by suicide may also vary considerably. This heterogeneity in profile and risk suggest that practitioners who encounter them in medical settings need to address their individual risk and needs. Appropriate psychosocial assessment and follow-up care should be offered to all patients, as specified in clinical guidelines (National Institute for Health and Care Excellence, 2004; National Institute for Health and Clinical Excellence, 2011). In considering risk and needs of those who self-cut, there should be special caution in addressing the needs of those who cut parts of the body other than the wrist or arm, especially when self-cut or stab involves the neck.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291721002956
Acknowledgements
The study was funded by the Department of Health and Social Care. KH is supported by Oxford Health NHS Foundation Trust. We thank Dr Apostolos Tsiachristas (University of Oxford) for providing statistical advice. We also thank the clinicians and the research staff in all research centres for their support with the data collection.
Author contributions
KH and GG were responsible for study conception and design, and interpretation of the results. GG was responsible for data analysis. DC, LB, FB, NK, CC, BF, JN, AP and KW acquired the data. GG drafted the report, which all authors critically revised for intellectual content. All authors approved the final report and are accountable for all aspects of this work.
Financial support
The Multicentre Study of Self-harm in England is funded by the UK Department of Health and Social Care. Role of the funding source: The Department of Health and Social care had no role in study design, data collection, analysis and interpretation of data, or in the writing of the report, and in the decision to submit the paper for publication.
Conflict of interest
KH declare grants from the National Institute for Health Research and the Department of Health and Social Care. He is a member of the National Suicide Prevention Strategy for England Advisory Group. KH is a National Institute for Health Research (NIHR) Senior Investigator (Emeritus). NK is a member of the Department of Health's National Suicide Prevention Advisory Group. NK chaired the NICE guideline development group for the longer-term management of self-harm and is currently Topic Advisor for the new NICE self-harm guideline. He also chairs the NICE guideline committee for depression in adults. All other authors declare no competing interests. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care.







