1.1 Historical Background of Health Education
The first reforms in health education occurred in response to the publication of the Flexner Report in 1910, more than a hundred years ago [Reference Flexner1]. The reforms, sparked by the discovery of the germ theory in Europe and other scientific advances, led to the integration of early developments in medical science into the academic education of physicians. Ten years ago, the Lancet published a report, “Health Professionals for a New Century: Transforming Education to Strengthen Health Systems in an Interdependent World,” based on the findings of a global independent commission to address the inequities in health, despite enormous scientific advances in medicine [Reference Frenk, Chen and Bhutta2]. In this report, twenty professional and academic leaders representing the perspective of diverse countries defined an educational strategy for medicine, nursing and public health. Its intention was to consider the relationship between health systems and education and recommend strategies to produce a workforce that addresses the health needs of a particular country.
According to the report, the initial reforms following the Flexner Report led to a radical transformation of medical education based on scientific evidence. This shift to a scientific foundation into the education of health professionals made such enormous differences as doubling the life span during the twentieth century [Reference Frenk, Chen and Bhutta2]. The authors of the Lancet report summarized three levels of learning: informative learning of skills acquisition, formative learning of values and professionalism and transformative learning to prepare for leadership (Figure 1.1). Transformative learning is considered the highest level, which, following the acquisition of skills to establish expertise and acquiring values and professionalism, develops leadership attributes to “produce enlightened change agents.”
The Fellowship in Family Planning’s educational vision and implementation are aligned with all three objectives: it defines and imparts clinical skills, fosters ethics and professionalism and, finally, produces leaders who change medical education, service delivery and health policy. (See Chapters 3 and 7.)
1.2 Health Systems: Preparing the Workforce
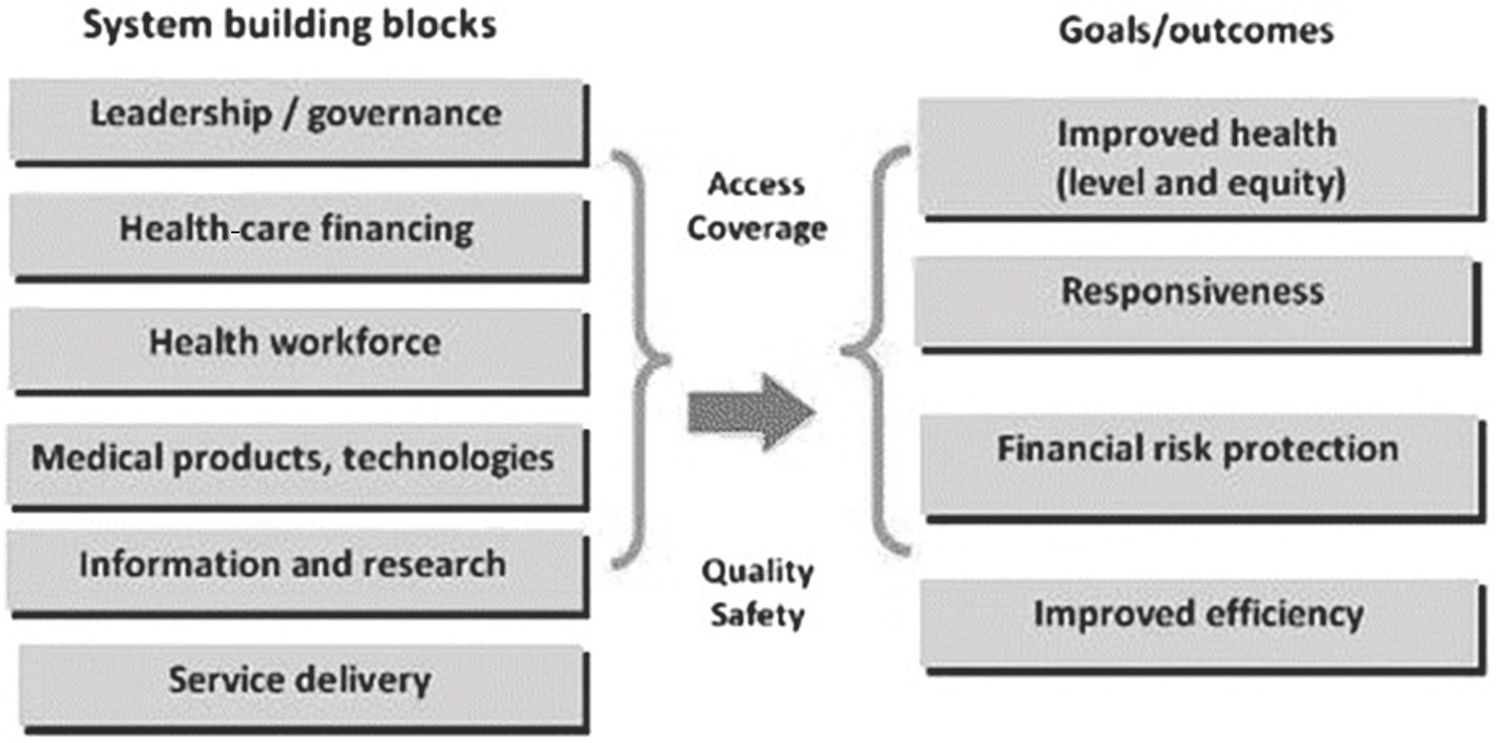
According to the World Health Organization (WHO), health systems have six components: leadership and governance, health information systems, health financing, human resources, essential medicines and technologies and delivery of health services (Figure 1.2).
The education of professionals is affected by and in turn impacts all components of the health system. Most important, health services and their delivery directly depend on the education of professionals to create the needed workforce. Professionals, in turn, because of the time-consuming and financial investment in their training, bear special responsibilities to become competent beyond the basic technical skills to be effective in teamwork, critical analyses, coping with uncertainty, conducting themselves ethically and becoming leaders in effective health systems [Reference Frenk, Chen and Bhutta2, p1951]. It is the professional who is capable of focusing on innovations for learning and institutional change.
Professional education in turn depends on a number of factors:
1. Who has the authority to create mandates?
2. How transparent is the system?
3. What are the roles of governments, professional organizations and other bodies in ensuring the education of the workforce?
4. How accountable is the process?
5. What function does accreditation play?
1.2.1 Educating a New Workforce in Family Planning through Integration into the Educational Systems
When a formerly illegal medical intervention becomes legal, there is an immediate need to prepare a new workforce. The 100 professors who published their statement in anticipation of the legalization of abortion attempted to describe the anticipated service delivery in hospital wards that formerly treated women suffering from medical complications from illegally induced abortion [4]. They did not address specifically the demands and challenges of integrating this new aspect of women’s health into education and training of obstetrician-gynecologists (ob-gyns). Likely they assumed that by providing the services, the residents would be trained as they are trained in all other clinical interactions and procedures taking place in the teaching hospital.
While some hospitals did initiate abortion services, most ceded to the newly created outpatient clinics, creating a serious gap in educating physicians needed to build a solid family planning workforce of physicians, nurses and other health-care workers. (See Chapter 3.)
Systems integration of family planning into medical education requires many changes, including institutional attitudes and practice. A number of important questions need to be asked:
1. What institutions are responsible for medical education?
For example, in the USA, there are 1,100 teaching hospitals. They might be academic, private, public and/or religiously affiliated institutions. There are 120 such hospitals directly affiliated with a medical school, and these are typically tertiary care hospitals, which take care of patients with complex medical problems and engage in research.
2. Who pays for the training of the workforce?
The primary financial source of resident education in the USA is the federal government, through Medicaid and Medicare funds allocated to teaching hospitals in a complex arrangement [5]. Additional training funds come from the state governments for state-affiliated, sometimes also private teaching hospitals, and public or private insurance payments for clinical services. Faculty are typically paid through clinical revenues, research grants and contracts. They may be paid a small proportion of their salaries by the medical school itself depending on their clinical, research and administrative responsibilities.
1.2.2 The US Systems Responsible for Post-Graduate Medical Education
Instead of a ministry or other governmental body, US physicians have created their own transparent systems of evaluation through professional medical organizations that set educational post-graduate standards and systems of enforcing them, both for the individual residents and fellows as well as the training sites.
1.2.2.1 The American Board of Medical Specialties (ABMS)
The American Board of Medical Specialties (ABMS) was formed in 1933 to create national standards for the education and practice of specialist practitioners [6]. In the past, the process of certification relied on occasional continuing medical educational courses and periodic assessment. It has evolved into a continuous cycle of assessment, learning and evaluation. It now places greater emphases on professionalism, patient safety and performance improvement.
In this system,
physicians become active participants in the evaluation of their own practices. They can see how their practice compares to those of their peers, how it differs from published best practices, and how their own practice evolves over time, progressing toward the ideal practice.
ABMS is responsible for approving medical specialties and subspecialties and certifying its members through member boards. Twenty-four specialties are currently represented on the ABMS board. The American Board of Obstetrics and Gynecology (ABOG) serves on the board on behalf of obstetrics and gynecology (obgyn). Obgyn subspecialties were created in the early 1970s in response to a “biological revolution in the reproductive sciences” to address, for example, the rapidly growing scientific understanding of hormonal action, conduct further research into maternal and fetal health and translate these findings into clinical practice and innovations Reference Ryan[7]. More specific, in-depth study beyond generalist training was necessary to pursue research and expand scientific knowledge [Reference Creinin and Darney8,Reference Goldberg, Greenberg and Darney9].
1.2.2.2 American Board of Obstetrics and Gynecology (ABOG)
ABOG was one of the founding members of ABMS, the third board of medical specialties in 1930 following the College of Surgeons and the American Board of Ophthalmology, which established the first system of certification.
ABOG is a not-for-profit professional medical organization representing the ob-gyn specialist areas and subspecialist divisions of reproductive endocrinology and infertility, maternal and fetal medicine, gynecologic oncology and female pelvic medicine and reproductive surgery. Its mission is “to define standards, certify obstetricians and gynecologists, and facilitate continuous learning to advance knowledge, practice, and professionalism in women’s health” [10].
ABOG, as ABMS’s specialty board, is responsible for the certification of ob-gyns and, until recently, the certification of ob-gyn subspecialties. The board creates and administers both oral and written exams that ob-gyn residents are eligible to take after four years of training. The board’s examinations are based on a rigorous system of case lists and subject-specific questions indicating clinical experience, competence and knowledge of the current evidence of practice and its underlying scientific principles. (See Chapter 19.) After passing the exams, a graduated resident becomes certified to practice in the field. Board certification confers “Diplomate” status that has to be reviewed periodically. Although ABOG certification is voluntary, it is required to practice in hospitals and other institutions as well as for membership as a fellow in ACOG.
Certification is also required for hospitals’ credentialing systems. To practice in a hospital, the physician must undergo a process of credentialing, which may, for example, include specific operations. The performance of a later second-trimester abortion, for example, may require the licensed physician to be proctored and credentialed before given permission to practice.
ABOG also administers written and oral exams in the four ABMS-approved subspecialties that now include family planning as the Fellowship in Complex Family Planning. Once a practice area achieves recognition as a subspecialty, ABOG selects representatives from the subspecialty community to inform the design of questions for the written and oral exams in a transparent, complex sequence of reviews of the depth and breadth of practice and roles of the subspecialist. In addition, ABOG creates a new division and appoints the members of the division based on the recommendation of, in the case of Complex Family Planning, ACOG, the Society of Family Planning and the National Office of the Fellowship. Each division is headed by a division chair who represents the division on the ABOG board.
1.2.2.3 Accreditation Council for Graduate Medical Education (ACGME)
The Accreditation Council for Graduate Medical Education (ACGME) is a nonprofit professional organization that was established in 1981, preceded by the Liaison Committee for Graduate Medical Education formed in 1972. ACGME is the accreditation organization that sets and maintains the educational standards of graduate medical education programs to ensure they meet the institutional and program requirements for which they prepare their graduates [11].
It currently oversees the post-graduate education and training (residents and fellows) in 830 teaching hospitals for all US medical doctors and doctors of osteopathy. As of 2020, it accredits 180 specialties and subspecialties through its current 28 Residency Review Committees (RRCs). Its mission is “to improve the quality of health care by ensuring and continually improving the quality of graduate medical education for residents by establishing graduate medical education standards, assessing training programs continually through a process of accreditation, and promoting high-quality educational programs for trainees” [11].
“We accomplish our Mission guided by our commitment to the Public Trust and the ACGME values of:
Honesty and Integrity
Excellence and Innovation
Accountability and Transparency
Fairness and Equity
Stewardship and Service
Engagement of Stakeholders
Leadership and Collaboration” [11]
Site visits are conducted at the time of the initial accreditation request, two years after initial accreditation, and later if the yearly Accreditation Data System information prompts concern or needs follow-up. They involve a complex process of gathering information from the residency program director, department chairperson, faculty members, current residents as well as chairpersons of other clinical departments or hospital administrators involved in residency training.
Programs can be put on probation at the discretion of the Review Committee.
All sponsoring institutions and programs undergo a full accreditation site visit every 10 years. This is preceded by a comprehensive self-study process that includes a description of how the sponsoring institution or program creates an effective learning and working environment leading to the desired educational outcomes. For the self-study, programs are also asked to review their aims and conduct an analysis of strengths and areas for improvement and to formulate and document plans for improvement.
Practice and training standards are periodically revised.
It was the ACGME that issued the first US abortion training mandate in 1995.
1.2.2.4 The Residency Review Committee (RRC)
The RRC represents each specialty (currently twenty-eight) under the ACGME and is responsible for defining and enforcing training standards for residents and subspecialists. Members of the RRC are nominated by the American Medical Association’s Council on Medical Education; the specialty board that certifies physicians within the specialty (ABOG); and by the professional college or another professional organization or society associated with the specialty [12].
Committee members are expected to be actively involved in graduate medical education; experienced in administration and/or teaching in the specialty, that is, as a Residency Program Director; be familiar with the accreditation process; and be part of an institution or program in good standing with the ACGME. The committee’s chair is elected by the committee membership.
The purpose of the RRC is to assess whether an institution or program is in substantial compliance with the institutional requirements and to confer an accreditation or recognition status. Programs with serious shortcomings and deficiencies will receive citations, which may lead to a shorter ACGME accreditation period or probationary status. For example, if residents do not perform a minimum number of a particular surgery, the department may receive a citation. Several citations and overall quality concerns can lead to probationary status. Departments have received citations for lack of abortion training.
Training expectations for subspecialty fellows in Family Planning and their sponsoring sites are defined and published in the Guide to Learning and the General Requirements [13,14]. While these guidelines were produced by the Fellowship’s National Office and Fellowship in Family Planning (FFP) directors previously during a period of twenty years of programmatic growth, ACGME will define new learning objectives with the recognition of subspecialty status.
1.2.3 The Teaching Hospital Prepares the Workforce
As the Lancet Commission report states:
Recognition the teaching hospital is a critical component of the Health Care System as it delivers services and trains the future health care worker.
We see educational institutions as crucial to transform health systems. … Through their educational function, they produce professionals who can implement change in the organisations in which they work.
Successful institutional changes in service delivery and training depend on a comprehensive understanding of the components of the system: the agencies that deliver care, those that finance it and the regulatory bodies that ensure that both workforce and care adhere to agreed-upon standards.
The health-care workforce educated in the teaching hospital includes physicians, nurses and other health-care providers. The physician workforce depends on the teaching hospital for core training of students, residents and fellows. Each teaching hospital, whether private or public, associated with a medical school or religiously affiliated, community-based or part of a hospital chain, is a component of the health system. While revenue streams may vary, patient care and overall training objectives are similar. Operating rooms, outpatient clinics, emergency departments, labor and delivery wards, pharmacy and specialty departments all make up the hospital system, each with its own particular service-delivery structures and culture and driven by the economics that determine its survival.
Recognition of family planning as an essential aspect of women’s health sets the stage for integrating family planning into the curriculum and services with expert faculty who provide care, teach, mentor, do research and are capable of leadership.
Integration requires familiarity with what roles the specialist will play within the system, interaction with other departments and their leadership and gaining their support.
1.2.3.1 Changing Hospital Services to Ensure Family Planning Training
Most FFP graduates join teaching hospitals as junior faculty members. To be an effective participant in a teaching hospital, particularly when attempting to change systems and services, requires understanding the domains of authority and the complex interactions among a multitude of stakeholders and decision makers: deans; hospital and nursing administrators; labor and delivery and outpatient clinic nurses; operating room (OR) staff, including anesthesiologists, nurses and technicians; leaders in central supply to ensure appropriate equipment, particularly for the OR; and directors of the emergency department (ED) as well as pharmacy. Every hospital unit and staff may be directly or indirectly part of abortion or contraceptive services. Establishing collaborations with pharmacy, for example, is necessary to ensure stocks of contraceptives and distribution of mifepristone.
Teamwork with departments and hospital units is essential to forge successful collaborations for the integration of family planning services. The authors of the Lancet Report observed that “Professionals are falling short on appropriate competencies for effective teamwork, and they are not exercising effective leadership to transform health systems” [Reference Frenk, Chen and Bhutta2, p1926].
The priorities of each hospital player must be taken into consideration when introducing new technologies and services.
The head of the obgyn department plays a significant role in facilitating institutional support. While some may be focused primarily on department finances, others may stress their departments’ educational mission. Family planning requires the introduction of new approaches and interventions in many points of service and departments and collaboration with various teams in order to gain the endorsement of the leadership. Nursing and anesthesia play a particularly decisive role in supporting and participating in abortion. Workshops and in-service trainings, specifically in the context of abortion, can be essential to gain support and cooperation. (See Chapters 10 and 17.)
In addition to understanding and connecting with the operational side of the hospital, knowledge of its overall philosophy of patient care and the economics of practice will inform any attempts for change. It is also helpful to become familiar with the diverse roles and degree of influence of each stakeholder. When the hospital is part of a medical school, private or public, the educational and political roles of deans and heads of the school are informed, at least in part, by their relationship with hospital administration and governing bodies such as boards of regents.
Each teaching hospital has an office of Graduate Medical Education (GME) responsible for training residents and fellows, including allocating their funding. The GME leadership is responsible for upholding and facilitating the educational expectations as defined by the professional educational organizations, which in the USA are the ACGME and the RRC.
What are the demographics and payer mix of the hospital’s patient population? What roles do patient numbers, access to care and patient satisfaction play in the hospital’s priorities? What connections exist with the community outside of the hospital, the other health service providers and practitioners, such as abortion clinics? What is the history of any collaborations and their effectiveness? (See Chapter 12.) What are the institution’s sources of pride and prestige? How much weight is given to its reputation as a teaching institution versus its technical innovation and research? How much are research grants valued? How much effort is focused on fundraising from private donors, adapting new technologies and media visibility?
A last question that can have an enormous impact on the institution and its leadership is whether it is a public or private institution. In either case, how and by whom is the relationship with the legislators carried out? To what degree are the deans and department chairs involved? Does the family planning expert provide evidence of patient care and satisfaction, the impact of family planning on the student and resident curriculum, the health impact of contraception and abortion care, particularly on vulnerable and medically complex patients? What role, if any, do training mandates, the education mission and workforce considerations play when legislators and government threaten interference? A family planning workforce prepared to engage in effective advocacy can play a pivotal educational role in contending with institutional and political interference and controversy.
And finally, what are the policies that directly affect patient care and training in family planning? What are hospital policies regarding pregnancy termination, postpartum contraceptive practices and sterilization? Even in states that have liberal laws regarding abortion care, hospital policies may be restrictive Reference Zeldovich, Rocca, Langton, Landy, Ly and Freedman[15].
Gaining an understanding of the numerous aspects of institutional functions, interrelationships and cultures takes time, but gaining familiarity with the hospital system and becoming an engaged member will increase the likelihood of making effective and lasting changes to institutionalize family planning training.
The family planning faculty will also benefit from connecting and becoming visible in the larger institutional context:
1. presenting the evidence
2. making personal connections
3. using patient stories as an advocacy tool
4. serving on committees and in roles in the department, school, hospital or institution, even if they don’t seem immediately related to family planning
With the institutionalization of services and training, the teaching hospital plays a major role in access to care:
1. as a referral site for other departments and specialists
2. in collaborations with community partners
3. in research
4. by educating future practitioners and change agents
When expert contraception and abortion services are in place, patients who are treated for other diseases can benefit from evaluation for their contraceptive needs and options for pregnancy termination. Professional collaboration among specialists within the hospital allows for optimal patient care.
1.2.4 Partnerships with the Private Sector to Enhance Training
While significant changes in the teaching hospital can be achieved, the number of abortions may be insufficient to train residents and fellows to achieve the expected clinical competence, particularly in hospitals with severe restrictions on abortion services. Under these circumstances, the teaching hospital seeks partnerships with the private sector freestanding clinics that provide the bulk of abortion care. Again, successful training outcomes depend on understanding patient care philosophy and economic demands of the clinics. Financial viability is of primary concern in most. Training may be perceived as interfering with efficient patient care, and special arrangements are made to provide incentives, either by having the academic physician mentor teach the residents while working in the clinic, offering needed equipment, or with an agreement to treat complex patients and complications. (See Chapter 17.)
1.3 The Global Realm
Unlike the US model, the education of health professionals in mid- and low-income countries is often under the purview of ministries of health or education, determining the parameters of health-care services and education of their medical workforce. Here, WHO or nongovernmental organizations (NGOs) may inform the country standards of care and their enforcement mechanisms. Colonial history is likely to impact the models for training and service, for example, in the countries formerly under British colonial rule in which the UK training model is used. Considerations for access and country health priorities, as well as the burden of disease such as maternal mortality, often determine the focus for family planning. (See Chapter 2.) Quality of care or training the future workforce may be of lesser concern.
When abortion laws are changed, again, access remains the primary, often only, concern. As the Lancet Commission states, external donors and NGOs are brought in for specific training initiatives, whereas the education of professionals is overlooked. (See Chapters 29 and 32.) As a consequence, integration of services and didactics into graduate, resident education is often missing, as are considerations of long-term workforce needs and policy leadership.
1.3.1 Impediments to Creating an Effective Workforce
The latest edition of the WHO’s “Technical and Policy Guidance for Health Systems” on safe abortion (2012) reflects its priorities of workforce capacity and training midlevel practitioners [16]. The preceding guidance (2003), “Putting Services in Place,” stress the need for standards including provider skills [17]. “Training programmes, both pre and in-service, should be based on a competency approach … to allow the health practitioner to demonstrate clinical competence” [17, p70].
The health system’s responsibility is to ensure supervision and clinical competence. No consideration is given to the role that physicians and medical education must play, as described by the Lancet Commission, beyond skills acquisition to develop professionalism and ethical practice, and educate physicians for change agent leadership in research and policy making. Instead, WHO states in its Guidance that as for Certification and Licensing of Health Professionals and Facilities, “its sole purpose should be to ensure that providers meet essential criteria for the safe provision of abortion care, as with other medical procedures” [17, p73].
Typically, the ministry of health or education prescribes learning outcomes and may engage NGO partners for implementation and/or evaluation. Eventually, however, institutionalization is essential to ensure a vibrant in-country workforce that leads and moves the field ahead: creating a system that develops experts to create educational standards, encourage research and advocate for an evidence-based health policy.
A major impediment to systems integration can be the stigmatization of abortion. (See Chapter 24.) It can discourage personal engagement and leadership and may prevent institutional implementation of the law after its passage.
Effective institutionalization of family planning training may also be hindered by the traditional staffing and setting of the family planning clinic in the teaching hospital. (See Chapter 29.) For example, the location of the clinics, far from other parts of the hospital where surgeries take place and residents work, may connote low status and service priority for the trainees. In addition, a high-volume, understaffed service may leave little room for the introduction of new technical advances or a focus on quality of care and patient interactions.
Academic teaching hospitals in any country can play an essential role in transforming the health system. By institutionalizing training of a physician and nursing workforce, they can document the impact and shortcomings of new services on patient care and the parameters and approaches to educating its future medical workforce, that is, residents, students and nurses. (See Chapters 20, 23 and 16.) Findings can then be used to change practices in the organization and hospitals in which they work. By virtue of the professionalism these leaders demonstrate, they will engender trust and confidence in their institutions: “This trust is earned through a special blend of technical competence and service orientation, steered by ethical commitment and social accountability, … [and] forms the essence of professional work” [Reference Frenk, Chen and Bhutta2, p1925].
1.3.2 Institutionalizing a Global Physician Community
Our vision is global rather than parochial, multiprofessional and not confined to one group, committed to building sound evidence, encompassing of both individual and population-based approaches, and focused on instructional and institutional innovations. Our goal is to encourage all health professionals, irrespective of nationality and specialty, to share a common global vision for the future. In this vision, all health professionals in all countries are educated to mobilise knowledge, and to engage in critical reasoning and ethical conduct, so that they are competent to participate in patient-centred and population-centred health systems as members of locally responsive and globally connected teams. The ultimate purpose is to assure universal coverage of high-quality comprehensive services that are essential to advancing opportunity for health equity within and between countries. The aspiration of good health commonly shared, we believe, resonates with young professionals who seek value and meaning in their work.
1.3.2.1 The Fellowship in Family Planning’s Global Vision
Terminal Objective:
The Fellow must have knowledge of the public health, legal, and service delivery aspects of family planning, abortion, and reproductive health in less developed nations.
Enabling Objectives:
A. Fellows should complete a three- to eight-week placement in a less developed country during their two-year fellowship.
B. Fellows must have knowledge of the effects of limited resources on family planning in the country of their placement.
C. Fellows must have knowledge of the public health, legal, and service delivery aspects of family planning care in the country of their placement. [16]
From start of the Fellowship in Family Planning in 1991, its vision reflected a global perspective that foresaw many opportunities for exchange of educational and clinical perspectives, institutional implementation and research in contraception and abortion. The vision stemmed from the founder of the FFP, Dr. Philip Darney, who participated in global exchanges with governmental agencies, the Agency for International Development (AID), the Centers for Disease Control and Prevention (CDC) and NGOs. These experiences demonstrated the lasting, mutually inspiring effects that strengthened health-care delivery, leadership, advocacy and research. His global vision was institutionalized through the FFP global health rotations and the Fellowship’s close collaborations with WHO.
Many of the fellows over the years pursued these opportunities to build community and experience the interdependence of individuals and institutions in bringing about system changes in family planning. Exchanges relied on already established contacts by Fellowship directors whose work connected them globally, or institutional connections already in place between academic institutions, departments and individual physicians. Visibility through presentations and posters by the national director and a growing number of Fellowship graduates, some of whom presented their research at international professional meetings, such as the International Federation of Gynecology and Obstetrics (FIGO) and the International Conference on Family Planning (ICFP), led to new interests for collaboration [Reference Landy18].
1.3.2.2 Impact on the Fellows
While not all fellows are inclined toward a global perspective or establishing formal connections, the experience is enriching for both fellow and host. Differing cultural perspectives on education, health-care systems, educational approaches and service delivery bring new insights about access to care, patient interactions and physician championship. Witnessing the consequences of unsafe abortions, overcrowded family planning clinics, the social injustice inflicted on women, and lack of professional, governmental or social support serves as a stark reminder and motivator to protect reproductive health and access at home. In addition, professional connections lead to further exchanges and research collaborations post-fellowship, which enhance local infrastructure and capacity. At their best, these exchanges help everyone to feel affirmed and empowered, recognizing the many similarities and opportunities to strengthen each other in the global quest for reproductive health and justice.
Fellows established global connections in Nepal where they helped institutionalize abortion and contraception training; in Vietnam, where they published a side-by-side English and Vietnamese contraceptive guide for medical students, Managing Contraception; and other projects in Malawi, Haiti, Thailand, Zimbabwe, Rwanda, Kenya, Uganda, India and many other countries around the world Reference Zieman, Hatcher, Allen, Lathrop and Haddad[19]. Some of the initial contacts were maintained by extended in-country stays at partner institutions to pursue research with local academic physicians, for example, or consulting visits over years with NGOs and continuing relationships through subsequent fellows.
1.3.2.3 Institutional Impact
The impact of these placements and exchanges encompass many areas: introducing new technologies and procedures offered to patients; addressing specific aspects of service delivery, educational principles and approaches, such as the evaluations of students, residents and faculty; and the principles of professionalism and mentorship.
1.3.2.4 Research: Mulago Hospital, Makarere University, Uganda and the University of California, San Francisco
The research projects of several fellows at the Mulago Hospital in Uganda, the national teaching and referral hospital in Kampala with 30,000 deliveries per year, led to a formal collaboration between the obgyn departments of the University of California, San Francisco (UCSF) and the Mulago Hospital at Makerere University. Goals included expanding research activities that support evidence-based practice of abortion and contraception care in Uganda and strengthening capacity to conduct independent research in family planning. Previous fellows’ research studies helped set in place the research infrastructure to conduct a larger randomized trial on the effect of immediate versus delayed initiation of postpartum contraceptive implants. Each study involved residents, fellows and junior and senior faculty at both institutions, enhancing training in research skills at many levels.
As a result, one Ugandan faculty member completed his PhD in reproductive science and developed an independent research program with a specific focus on postpartum contraception and contraception for women at risk for HIV and living with HIV. A Medical Students for Choice chapter at Makerere University will be supported with mentorship and teaching by the US partners who are now faculty and direct family planning fellowships at US teaching hospitals. The chair of the Mulago hospital is pursuing further clinical training, particularly in dilation and evacuation (D&E), and the Ministry of Health in Uganda lent its support for the research proposals and the results of the studies informed policy change at the national level. The collaboration led to publications in major peer-reviewed journals [Reference Morse, Rowen, Steinauer, Byamugisha and Kakaire20,Reference Lester, Kakaire and Byamugisha21,Reference Kakaire, Byamugisha, Tumwesigye and Gemzell-Danielsson22,Reference Averbach, Kakaire, McDiehl, Dehlendorf, Lester and Steinauer23,Reference Averbach, Kakaire and Kayiga24].
1.3.2.5 Research: Malawi College of Medicine and the University of North Carolina
Another example of systems building is that of the collaboration between the University of North Carolina’s (UNC) Division of Global Women’s Health, the Malawi government and the Malawi College of Medicine. A graduated fellow and faculty member at UNC worked for five years in Lilongwe, Malawi, with UNC Project—Malawi to help build up obgyn clinical and research infrastructure. There, she worked with both governmental and nongovernmental organizations to advance women’s health research and clinical capacity through teaching, mentoring and serving on various Malawi Ministry of Health (MoH) committees. For example, she served on the National Family Planning Sub-Committee, Safe Motherhood Sub-Committee, Population and Development Technical Working Group, and Cervical Cancer Control and Prevention Program Task Force, partnering with the MoH to implement postpartum intrauterine device (IUD) insertion throughout the country and advising the MoH on its National Cervical Cancer Control Strategy 2016–2020 Reference Lester, Kakaire and Byamugisha[21].
In addition to her contributions to Malawi family planning policy, in her role as an Honorary Senior Lecturer at the Malawi College of Medicine, she was a founding member of the country’s first obgyn Residency Program in 2013, establishing the country’s first annual obgyn Scientific Meeting, developing the country’s first obgyn protocols and guidelines handbook, and leading the residency’s first weekly journal clubs and didactic sessions. The residency has now graduated twelve residents, with another thirteen currently in training, which will quadruple the number of Malawian ob-gyns practicing in-country within a decade. She also helped to build clinical capacity by teaching the residents and other learners while working at Lilongwe’s two biggest public hospitals and by organizing trainings for hundreds of providers in family planning, long-acting reversible contraception (LARC) insertion, postpartum IUD insertion, cervical cancer screening and emergency obstetrics and neonatal care (EmONC) [Reference Lemani, Tang and Kopp25,Reference Lemani, Kamtuwanje and Phiri26,Reference Tang, Kaliti and Bengtson27]. Four family planning fellows completed their international fellowship rotations with her in Malawi, helping to lead the postpartum IUD trainings and implementation and publishing related research [Reference Krashin, Lemani and Nkambule28,Reference Krashin, Haddad and Tweya29]. Finally, she has mentored fourteen Malawians in research to date, including Malawian ob-gyns, residents, medical officers, nurses and social scientists, most of whom have already either published or submitted first-author manuscripts [Reference Chinula, Nelson and Wiener30,Reference Chinula, Hicks and Chiudzu31,Reference Gausi, Chagomerana and Tang32,Reference Mbichila, Chagomerana and Tang33,Reference Bula, Kopp, Maman, Chinula, Tsidya and Tang34,Reference Mwafulirwa, O’Shea and Hamela35].
1.3.2.6 Education: Guyana, Kenya and Ethiopia
Guyana: Over a period of seven years, ten fellows spent their global health rotations in Georgetown at the Georgetown Public Hospital Corporation, the teaching hospital of the University of Guyana. For some, these were training and consultation visits based on partnerships between their own academic institution and Guyana, or through an NGO. Their focus was on abortion training, leading the country’s annual safe abortion workshops, including Train the Trainers workshops. The trainees were residents and nurses, physicians from other regional hospitals to encourage decentralization and widen access to safe abortion services throughout the country, who received training and proctoring, leading to certification by the Guyana Ministry of Health in manual vacuum aspiration (MVA) and D&E. Another accomplishment was the initiation of post-placental IUD insertions. Their teaching efforts led to the tripling of physicians who incorporated abortion into their practice.
Kenya and Ethiopia – recent examples of infrastructure building
Kenya: A recently graduated family planning fellow, now on the faculty at Indiana University’s School of Medicine, leads an academic global health collaboration between Indiana University and Moi Teaching and Referral Hospital in Eldoret, western Kenya. Her focus is expanding access to family planning, especially among women with HIV and other chronic medical conditions. As a visiting faculty member in the Department of Reproductive Health, she teaches residents and medical students about family planning and conducts research and care projects expanding the roles of community health workers to improve linkages to reproductive health care, integrating family planning services within the hospital and outpatient chronic disease clinics, and improving reproductive health counseling for women with HIV and other chronic diseases. [Reference Bernard, Pekny and Omukagah36,Reference Patel, Jakait and Thomas37,Reference Bernard, Jakait and Fadel38]
Ethiopia: A partnership was created by the Ethiopian Society of Obstetricians and Gynecologists, ACOG, the Ethiopian Federal Ministry of Health and the Center for International Reproductive Health Training (CIRHT), which is committed to improving maternal health to help build infrastructure through medical education and preparedness by transforming equity and quality of care. Specific projects included standardization of residency training and assessment of outcomes, as residency programs recently increased from three to ten, leadership development, research infrastructure and creating a code of medical ethics, among others.
Expanding on these systems and educational infrastructure building efforts, a new Ethiopian Fellowship in Family Planning was started by CIRHT in 2017 to produce competent clinicians, trainers, researchers, advocates and leaders in family planning. (See Chapter 29.) A Fellowship graduate and director of the Fellowship Program at the University of Washington joined the faculty at the St. Paul’s Hospital Millennium Medical College (SPHMMC) during a one-year sabbatical as director of this first Family Planning Fellowship in Ethiopia, building on the educational infrastructure of Ethiopian colleagues and other Fellowship graduates to strengthen capacity. The Fellowship will soon have its first three graduates, who will be able to manage the administration and training requirements of the SPHMMC fellowship and continue to train other ob-gyns in Ethiopia in contraception and abortion. In partnership with the Ethiopian and US family planning specialists, she is developing a curriculum for continued training, along with necessary exams to evaluate skills and knowledge Reference Negussie, Bekele and Curran[39].
1.4 Institutional Mandates and Prescriptions for Medical Practice after Legalizing Abortion
As countries consider legalization of abortion, the medical profession plays a pivotal role. Their support is necessary for two reasons: to emphasize the health consequences of unsafe abortion and the positive impact on patient care of safe abortion, and to ensure commitment to create the necessary systems educating the next generations of practitioners. (See Chapter 4.) Tensions over the role of conscientious objection often arise, especially in countries where religion plays an important role Reference Truong and Wood[40]. Should physicians, particularly gynecologists, be expected to do abortions? Feminist groups are united in their recommendation that they should, whereas physician organizations insist on physician autonomy to opt out or object.
Several factors likely affect these attitudes. While stigma surrounding illegal abortion and religion, especially in countries that are predominantly Catholic, lead to reluctance to do them once legal, many physicians lack the necessary skills and clinical competence. In addition, the stigma of illegality combined with the perception that abortion is a low level of medical practice lacking the prestige of other aspects of obgyn care likely discourage physicians to seek training. Even if physicians have been instrumental advocates for legalization (Uruguay), they do not support the demand that every physician must do abortions Reference Stifani, Couto and Lopez[41].
The focus and often controversy whether current practitioners intend to do abortions distracts from the most consequential consideration, the long view: the need for institutionalizing and mainstreaming abortion and family planning practice by setting mandates and expectations for training the future generations of practitioners. Training requirements can be institutionalized through academic medical centers, although current practice cannot, although Uruguay and Nepal are examples of institutionalizing services and training of current practitioners. (See Chapters 31 and 27.)
Establishing training mandates, implementing education and ensuring a future workforce will make legalization meaningful and sustainable. The clinical skills, acquired sense of professionalism and the understanding of the social and emotional aspects of abortion will be valuable when they decide to incorporate abortion in their future practice, without forcing them to make such a commitment. (See Chapter 23.)
“Those who conscientiously serve women seeking abortion often face stigma and discrimination from their colleagues, exacerbating other obstacles that complicate their work. Health care providers at the convening underscored the importance of comprehensive training and support for those who work in abortion care ” Reference Truong and Wood[40].
Another advantage to institutionalizing education and training is their effects over time on attitudes and practice. (See Chapters 7 and 23.) While in the USA the ob-gyn physician leadership endorsed legalization and anticipated its ability to fulfill the demand for safe abortion once legalized, stigmatization continued, and the initial enthusiasm and structured training declined until the passage of a professional mandate and the launch of national training initiatives. (See Chapter 3.) These initiatives, the US Ryan Residency Training Program and the Fellowship in Family Planning, ensure implementation of the law and long-term patient access by teaching the necessary technical skills, fostering research and inspiring new champions who continue to transform the cultures in their institutions and beyond. (See Chapter 7.)
1.5 Medication Abortion and Institutionalization of Abortion
When legalization is under consideration, access to medication abortion outside of the legal system may hinder institutional and professional support. Misoprostol availability can lead to misleading conclusions that (1) abortions are accessible to women if they want them, without the need to legalize, and (2) the skills necessary to administer medication abortion are simple and do not require the care of a clinician. While both may be correct on the surface, they fail to acknowledge that institutionalization of physician training creates the in-country workforce necessary to serve as trainers, set standards of care, conduct research, act as change agents and inform policy makers who will promote the practice of safe legal abortion as an integral part of women’s health. In turn, stigma will decline as a result of integrated training of health-care providers.
1.6 Conclusion
Medical education is an essential part of a country’s health-care system. It may be governed by the county’s ministries or by professional organizations. Its effectiveness depends on governmental and societal support and acknowledgment of its impacts on health. The Lancet Commission’s report on “Health Professionals for a New Century” scrutinized the impact of medical education on health systems and proposed a new philosophy and vision. Family planning, contraception and abortion offer a concrete example of the role of medical education in transforming health Reference Frenk, Chen and Bhutta[2]. The Lancet Commission’s report creates a guide to understanding the systems of health care and the role of medical education in creating a competent workforce empowered to lead and be responsive to the health-care needs of its community.
A systems approach to institutionalize training in abortion and contraception depends on a number of factors, all equally important for success:
1. understanding the ownership, affiliations and structures of the health-care system
2. knowing which institutional bodies define medical education standards and are responsible for their enforcement
3. setting a professional training mandate for abortion and contraception
4. understanding the systems in which training takes place
5. preparing the workforce to become
a. expert service providers who abide by their professional and ethical responsibilities
b. researchers and evaluators of services
c. leaders, advocates and change agents
i. for service and policy within teaching hospitals,
ii. the systems in which they work,
iii. their professional associations and
iv. their communities and society at large
6. creating a system to ensure a community of support
Educational initiatives like the Fellowship in Family Planning and the Ryan Residency Training Program are systems-changing programs. By educating the obgyn workforce, these programs ensure access to care and the availability of services, set standards of professionalism, foster research and promote systemic institutional change within teaching hospitals and professional organizations. They work to set and enforce standards and ultimately change the professional culture.