INTRODUCTION
There are multiple reasons for an individual to be unvaccinated, including individual or parental choice, healthcare access, and contraindication to vaccination [Reference Brown1–Reference Pearce4]. However, being unvaccinated leaves an individual susceptible to a host of infections which can result in serious morbidity or mortality. The combined measles, mumps and rubella (MMR) vaccine has particularly high rates of rejection. Introduced in 1988, uptake of MMR vaccine is currently peaking at 92% in the UK [5], still below the required levels to confer herd protection.
In 2003, uptake rates were as low as 79%, partly in response to media publicity regarding MMR vaccine following a now discredited and subsequently retracted article in the Lancet in 1998 [Reference Wakefield6, Reference Friederichs, Cameron and Robertson7]. This study was widely criticized [Reference Chen and DeStefano8, Reference Nicoll, Elliman and Ross9] and the Medical Research Council reviewed all the evidence regarding MMR vaccine and its links to inflammatory bowel disease (IBD) in the same year, and concluded that there was no evidence to link MMR vaccine to IBD [Reference Bower10–Reference Fombonne12]. Furthermore, several studies [Reference Patja13–Reference Taylor17] demonstrated that MMR vaccine does not cause autism or IBD. Despite the wealth of literature regarding the safety of MMR vaccine, parental confidence, as observed in uptake rates, has been affected, although this has improved in recent years and continues to improve.
In order to understand the factors which may have influenced parents' or carers' decisions not to immunize their children with MMR vaccine, we undertook a descriptive qualitative study using a semi-structured questionnaire that was completed during one-to-one telephone interviews with parents of confirmed measles cases. The aim of the study was to identify factors that continue to affect MMR uptake rates, and consider key issues related to parents or carers of confirmed measles cases.
METHODS
Participants and setting
This study was conducted in Merseyside following a measles outbreak in the area [Reference Vivancos18]. Merseyside has a resident population of about 1·4 million, while first-dose MMR uptake is >92% and second-dose uptake is ~85%. This was the largest outbreak in the North West of England since the introduction of MMR vaccine in 1988, with previous outbreaks being sporadic. The outbreak began in January 2012 and was declared closed in September 2013. There were 647 laboratory-confirmed cases and 286 probable cases, and 43% of confirmed cases were children aged <5 years. Twenty-one percent of confirmed cases required hospitalization at time of notification. Cheshire & Merseyside Health Protection Unit case records were used to identify potential participants and access contact details. Inclusion criteria were: parents or carers of laboratory-confirmed measles cases; cases were aged between 13 months and 9 years (inclusive); cases were eligible for MMR vaccination; and cases had not received MMR vaccination prior to developing measles. This information was validated further during the interview with participants.
Questionnaire and analysis
A secure online questionnaire was developed in order to collect anonymized data. Attempts were made to contact participants a minimum of three times and a maximum of five times via telephone between 09:00 and 21:00 hours. If participants answered, they were then given information about the caller and reasons for the call using an agreed and standardized script. Verbal consent was obtained from participants and vaccination status was confirmed before progressing with the interview. If participants consented and confirmed that the child was unvaccinated, the interviewer progressed with the interview and completed the questionnaire. All four interviewers received briefing and training with regard to interview process and completion of questionnaires in order to limit interviewer bias.
Questions included covered: receipt of invitation letter; clarity of invitation letter; receipt of reminder letters; whether child has had other vaccinations; whether child has had MMR vaccination since recovery; reasons for not vaccinating with MMR; what would be useful in aiding vaccination; advice to other parents who had not consented to vaccination; and other general comments. Prompts were not given to participants in relation to comments to ensure that their own views were accurately recorded. Responses were analysed using thematic analysis, i.e. responses were analysed and grouped into themes relating to original reasons for not vaccinating.
Ethical standards
Ethical approval was not required as this study was undertaken as part of the Merseyside measles outbreak investigation. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
RESULTS
Response rate and characteristics of participants
A total of 227 laboratory-confirmed measles cases were identified as not vaccinated with MMR. Of these, 142 were eligible to be included in the study and contact details were available for 110 cases. Of the 110 cases identified, 30 cases could not be contacted. Of the remaining 80 cases, 23 were excluded as they had already been vaccinated prior to infection, four were too young to be eligible for MMR vaccination at time of infection, two responses were recorded incompletely and four had incorrect identification codes recorded. This left a final sample of 47 cases, 46 of which were from Merseyside and one from Cheshire. Ethnicity was poorly recorded, with 91% (43/47) failing to state their ethnic background. Only 13 cases provided maternal age at birth of child.
In relation to an offer of MMR vaccination, 81% of participants received a letter of invitation for vaccination, of which 67% felt it was clear and informative. The majority (85%) of the children were up to date with other vaccines. Nearly half (43%, 20/47) of those questioned had been given the MMR vaccine since recovery and a further six children were due to have the vaccine after the interview (Table 1).
Table 1. Responses to questions regarding vaccination of cases and their siblings, including the process

* Six children were due to have the vaccine.
What was the reason for not vaccinating your child with MMR?
Four general themes arose from the responses: concerns regarding vaccine safety, child illness at time of vaccination, healthcare factors, and other individual factors (Table 2). Twenty-eight responses mentioned safety concerns, the most common reason provided, and of these 23 specifically referred to autism. These responses were mainly just discussing general links to autism; however, eight responses specifically mentioned the role of the media or the Wakefield study [6], while three responses discussed personal experience of autism with friends or family. Four responses discussed concerns about vaccination side-effects or reactions not specified to autism, while one respondent discussed concerns about a mental health risk.
Table 2. Themes discussed in response to why child did not receive the MMR vaccine
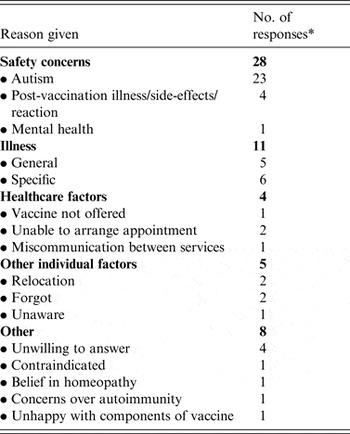
* Response count above 47 as some responses discussed multiple themes.
Child illness was the next major factor which influenced the decision of 11 participants. Of these, six provided a firm diagnosis of an illness at the time of vaccination, with the remaining five providing non-specific illness as a reason for not vaccinating. Specific diagnoses provided included recurrent croup, ear infection, glandular fever, chest infection and ‘strep throat’. Four responses discussed healthcare factors, including two who were unable to arrange an appointment for vaccination, one who claimed the vaccine was not offered and one who explained a situation of miscommunication between the local hospital and the General Practitioner (GP). Five response indicated individual factors as the reason for not vaccinating, including forgetting (2), moving house (2) and being unaware of the MMR vaccine on the immunization schedule (1).
Other non-specific reasons included belief in alternative methods such as homeopathy (1), concerns regarding autoimmunity (1), contraindication (1) and concerns over vaccine components (1). Four respondents were unwilling to elaborate on reasons for not vaccinating.
What things would you have found useful to persuade you to vaccinate your child?
When asked ‘What things would you have found useful to persuade you to vaccinate your child?’ the participants were offered four set responses and ‘other’. Twenty-five of 47 agreed ‘more information or advice’ would improve services, 30 agreed with ‘discussion with a health professional’, 16 agreed with ‘a wider choice of clinics and venues’ and 15 agreed with ‘earlier or later opening times’. Other responses varied and include the following comments:
-
• More should be done to make it clearer how serious measles is (3).
-
• Accessibility to clinics should be easier (1).
-
• Single vaccines should be available on the NHS (1).
-
• More information on the benefits of the MMR vaccine (1).
-
• More information on the invalidity of the Wakefield study (1).
-
• Take services into the community for those who do not go to their GP (1).
Do you have any advice that you would give now to parents who have not vaccinated their child?
There were 28 responses to this optional question; 22 answered they would recommend vaccination, one was unsure and one would still not recommend MMR vaccination. Other responses included advice to discuss concerns with a health professional, advice to recognize the seriousness of measles and advice to make the services work for individual needs.
Other general comments
This was an open question for participants to provide additional information if they wished to do so. Only three participants responded. One respondent was unhappy with the standard of care provided in the local hospital, another felt that health professionals were narrow minded when explaining MMR vaccine and the final respondent commented that parents ‘shouldn't be pressured to have vaccinations’.
DISCUSSION
The main findings in this study support the hypothesis that publicity around the discredited MMR paper remains a major issue influencing parental decision regarding the MMR vaccine. Despite strong evidence and clear information which fully discredited the link to autism, this remains a concern for parents and carers. The high frequency of response to improving services by making more information available and wanting a discussion with a health professional also supports this. Furthermore, two participants had requested for single vaccines to be available through the NHS, indicating the impact of the negative publicity regarding MMR vaccination on parental confidence in the vaccine. The results suggest that other safety concerns are not widely held, with only single responses for mental health risks, post-immunization illness, side-effects and autoimmunity. A large number of respondents indicated that cases were up to date with other childhood vaccines, suggesting the concerns focus solely on the MMR vaccine for many parents and carers. Vaccine safety concerns have previously been demonstrated to have an important influence on parental decision regarding vaccination [Reference Alfredsson19, Reference Bardenheier20], while specific concerns regarding links with autism, immune overload and higher safety of single vaccines have been documented [Reference Casiday21, Reference Gellatly, McVittie and Tiliopoulos22].
Although a lack of awareness with regard to the dangers of measles was only stated by one participant as a direct factor in deciding not to take up MMR vaccination, participants were keen to recommend that the dangers of measles should be publicized, and the change in opinion regarding the seriousness of measles following the experience of caring for a child with measles indicate that lack of awareness on the dangers or severity of measles is a significant issue. This is a common thread in vaccination literature, with a low perception of disease severity and risk of contracting the disease associated with lower vaccine uptake [Reference Brown1, Reference Cassell23, Reference Mills24]. The change seen in vaccination intentions after the outbreak suggests that experience of measles directly influences vaccination beliefs. Studies assessing views on outbreak prevention found conflicting evidence regarding vaccine decliners reconsidering their decision due to an outbreak [Reference Brown1]; however, research has shown an increase in MMR vaccine uptake during a measles outbreak [Reference Le25].
These findings suggest that safety concerns remain a key area in the decision-making process which is prohibitive to vaccine uptake. Considering the change in beliefs caused by experiences, increasing awareness of measles and its dangers could be beneficial in improving uptake, with media campaigns being potentially useful. Furthermore, the prominence of the historical MMR autism link in decision making would suggest that catch-up campaigns, new methods to disseminate information and opportunistic approaches during outbreaks could be useful [Reference Le25–Reference Nyhan27]. Previous evidence supports the use of parental meetings to improve the vaccination process [Reference Jackson28], with GPs and health visitors viewed as trusted sources of information [Reference McMurray29]. The use of personally tailored vaccine invitation letters which are more informative may also be of benefit. However, it is important to recognize that parents who currently reject the MMR vaccine seem to express more complex beliefs which may require novel approaches [Reference Brown30].
Around a third of all participants felt that longer opening hours and a variety of venues would improve services, suggesting access is a concern for parents and carers. However, it is noteworthy that only 9% of participants highlighted access as a reason for not vaccinating, suggesting that the perception parents have with regard to accessing services does not match with their previous experiences. This could potentially be explained as access issues have been shown to be more prevalent in incomplete vaccination rather than unvaccinated individuals, and the sample does not include incompletely vaccinated children [Reference Samad31]. It is important to recognize that access is an issue which can be directly influenced through policy, and given the economic and health benefits of increased vaccination uptake, it is a clear area of concern. Previous evidence shows that general practice factors have a significant impact on vaccination uptake; practices which had a clear immunization strategy and used a national call/recall system performed significantly better [Reference Lamden and Gemmell2].
Almost a quarter of participants stated illness as the reason preventing their children receiving MMR vaccine. Half of these participants responded that the child was unwell for vaccination without a specific diagnosis, which suggests that a clinician or immunizer did not have the opportunity to see the child when they were due for MMR vaccination. This is important as it indicates that parents were making the decision whether or not the child should receive the MMR vaccine and not the healthcare professional. Thus, a number of potentially eligible children may have been denied the MMR vaccine unnecessarily. This is a possible indication of belief that children should not be vaccinated when unwell with even a minor illness [Reference Mills24]. Effective dissemination of information regarding contraindications and reasons to postpone vaccination could resolve this concern.
The sample size achieved is relatively high for a study of this nature, while the setting allows for a unique perspective. To perform the research during and after a large measles outbreak has allowed for a direct investigation of the impact of experience of measles on opinion of vaccination. However, a number of limitations are present. The short and direct nature of the questionnaire allowed for a high number of participants, but did not allow detailed analysis of the reasons provided, or follow-up questions. This would have been particularly valuable in distinguishing causes when illness was provided as a reason for not vaccinating. Additionally, further questions regarding change in views and the impact of direct experience would have been useful. This study was conducted with parents and carers of children who had recently had measles, therefore there is a potential for overstatement bias, as respondents could feel that a somewhat acceptable reason should be provided for their decision not to vaccinate, while the retrospective nature introduces the risk of recall bias.
CONCLUSIONS
The publicity surrounding the discredited MMR paper suggesting a link between MMR vaccine and autism continues to be a major issue influencing parental decision regarding the MMR vaccine. Information which highlights the safety of the MMR vaccine is readily available; however, this information remains elusive or unconvincing to some parents. The change in views regarding vaccination which occur due to direct experience of measles suggests that, although not a reason to refuse vaccination, highlighting the risks of measles would be an effective approach to improve MMR vaccine uptake. Finally, parents or carers of cases with measles infection perceive access to immunization services and the information that relates to MMR vaccination to be inadequate. This needs to be considered and reviewed regularly by service providers.
ACKNOWLEDGEMENTS
We thank Cheshire & Merseyside Health Protection Team staff for their support with conducting the project including maintaining up-to-date data of measles cases.
DECLARATION OF INTEREST
None.





