Introduction
Detailed knowledge of facial nerve anatomy, topography and morphometry is a prerequisite for performing facial interventions, especially parotid gland surgery.Reference Al-Qahtani, AlQahtani, Baqays and Islam1,Reference Kochhar, Larian and Azizzadeh2 Preservation of facial nerve integrity is essential as any injury of the facial nerve may lead to either temporary or permanent palsy. Facial nerve sacrifice is only indicated in cases of malignant infiltration.Reference Cracchiolo and Shaha3 Landmarks such as tragal pointer, angle of the mandible and tip of the mastoid process have been employed to help surgeons identify the facial nerve.Reference Ji, Donoff, Peacock and Carlson4 Precise knowledge of anatomy requires time, training and experience.
The branching pattern of the extratemporal portion of facial nerve can be determined only after careful dissection of cadaveric or surgical specimens.Reference Davis, Anson, Budinger and Kurth5–Reference Tsai and Hsu7 A thorough and complete dissection of the facial nerve is a tricky and time-consuming task because of the small calibre of the nerve and high anatomical variability in its course. Anatomical textbooks and current surgical literature lack extensive information about the branching patterns of the facial nerve.Reference Bendella, Spacca, Rink, Stoffels, Nakamura and Scaal8
In fact, branching patterns of the facial nerve vary among studies, and more than one classification has been proposed since 1945.Reference Davis, Anson, Budinger and Kurth5–Reference Tsai and Hsu7 Davis et al. presented a thorough classification in 1956.Reference Davis, Anson, Budinger and Kurth5 The Davis landmark study included 350 carefully dissected cadaveric specimens. This classification has been adopted by the vast majority of anatomists and surgeons, although there are still rare cases that cannot be classified based on these patterns.Reference Salame, Ouaknine, Arensburg and Rochkind9 The Davis classification includes six different patterns (I–VI), based on the presence of anastomoses among the terminal branches, with its simplest pattern being type I.Reference Davis, Anson, Budinger and Kurth5
A systematic review of all existing evidence regarding facial nerve course could raise awareness about its high anatomical variability, thus potentially improving surgical planning and reducing iatrogenic facial nerve injury. The aim of this paper was to synthesise data concerning the frequency of different branching patterns of the extratemporal portion of the facial nerve based on Davis classification. In addition, information about the topography and surgical or anatomical landmarks will be presented.
Materials and methods
We performed this systematic review in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (‘PRISMA’) statement and as recommended by the Cochrane Collaboration. Original studies assessing facial nerve extratemporal branching pattern on surgical or cadaveric specimens according to the Davis classification were identified. No restrictions concerning article language were placed.
A comprehensive electronic search of Medline, ScienceDirect and the Cochrane Library electronic databases was conducted on 1 April 2021 to source studies pertaining to the research question. No restrictions concerning year of publication were imposed. In order to maximise sensitivity, the references section of every relevant review article and all full-text articles identified for inclusion were also carefully hand-searched and assessed for relevance. Archives of major recent ENT conferences were also searched with the aim of identifying grey literature. Taking into account that this study was a systematic review of published articles, neither informed consent nor ethics approval was needed.
The comprehensive literature search was independently performed by two authors (AP and NT). The following free-text terms were used for the Medline, ScienceDirect and Cochrane Library database search: (‘facial nerve’) AND (anatomy OR course) AND (patterns OR variations). The two reviewers worked independently on the selection of included articles, and any arising disagreements were resolved through consensus. Both inclusion and exclusion criteria were determined before commencement of the literature search.
Only studies complying with the following criteria were considered for inclusion: (1) cadaveric or surgical dissection studies; (2) the study population comprised specimens of all ages coming from all races or ethnicities; (3) studies presented facial nerve branching patterns according to the Davis classification; and (4) studies with other classifications were included only if their results could be translated into the Davis classification.
Exclusion criteria were as follows: (1) branching-pattern classification irrelevant to Davis classification; (2) animal studies; and (3) case reports.
All identified studies were screened separately in terms of their eligibility by two authors (AP and NT), according to the predetermined criteria, and if found eligible, were subjected to data extraction. Any arising discrepancies were discussed by the two authors until an agreement was reached. A preformulated extraction sheet was employed by both reviewers. The following data were retrieved from each one of the eligible studies: study characteristics (first author, year of publication, study design, population of study, race or ethnicity, inclusion criteria, exclusion criteria, primary endpoint, secondary endpoints) and outcome data.
Facial nerve branching pattern, as described by Davis in 1956, was the primary outcome. Secondary endpoints were main trunk furcation variations (bifurcation or trifurcation or other) as well as topography of anatomical landmarks (tragal pointer, angle of mandible, tip of the mastoid process) and total length of extratemporal portion of the main trunk (from stylomastoid foramen to bifurcation point).
The Quality Appraisal for Cadaveric Studies scale, a highly reliable tool for evaluating the methodological quality of observational dissection studies, was used to critically appraise all included studies. Each 1 of its 13 items was scored independently by the two reviewers (AP and NT) with either 0 points (no or not stated) or 1 point (yes or present) (total score: 13).Reference Wilke, Krause, Niederer, Engeroff, Nurnberger and Vogt10
Results
The literature search resulted in a total of 2818 records (Figure 1). Additionally, seven records were identified through other sources (reference lists). After removing duplicates, 2443 records were eligible for title and abstract screening. After thorough screening, 2397 studies were excluded because they did not meet our predetermined criteria. The full text of 46 articles was assessed for eligibility and, ultimately, 21 articles that could provide data able to answer the research question were selected for inclusion in this systematic review.
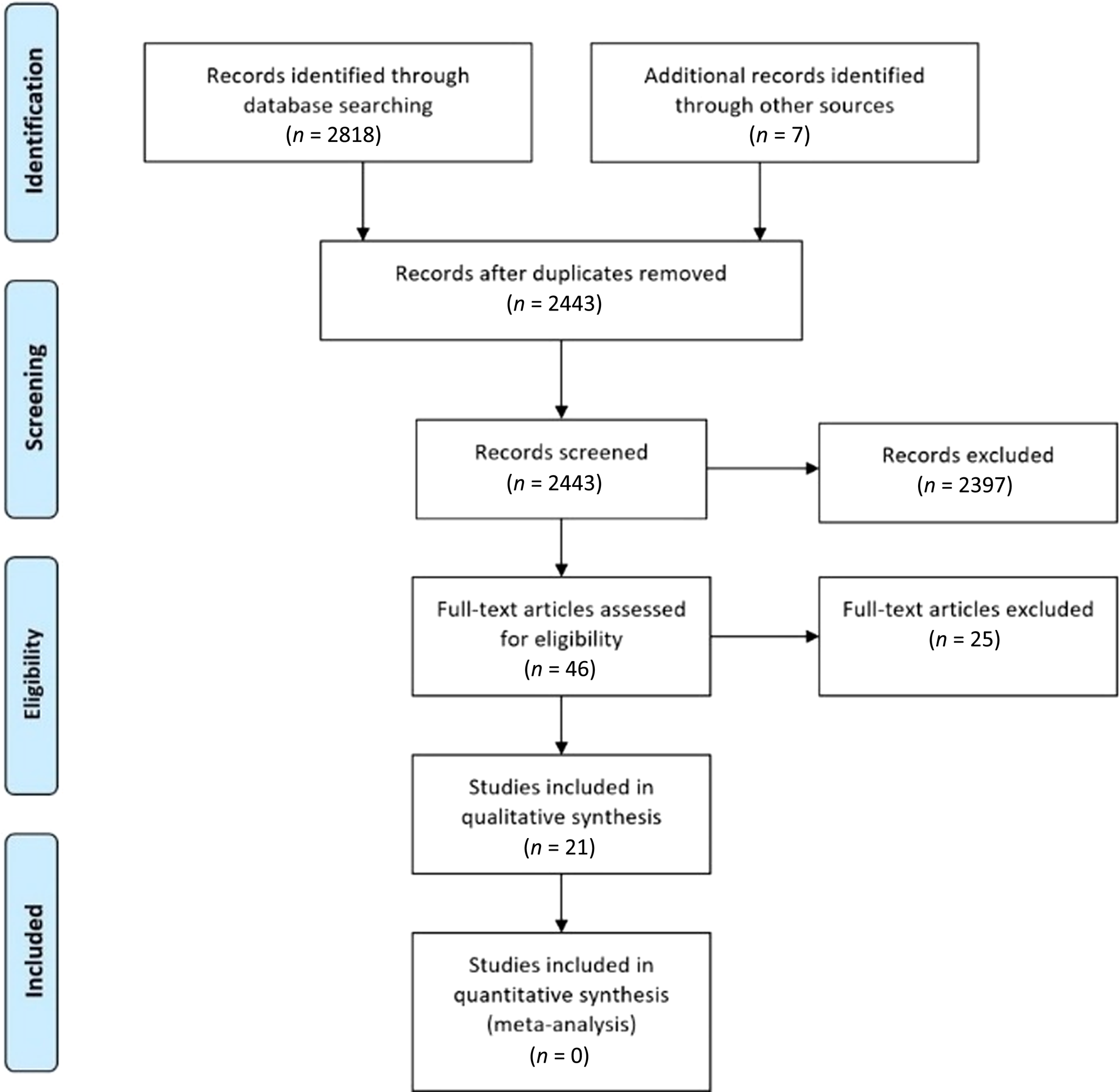
Fig. 1. Literature search strategy using Preferred Reporting Items for Systematic Reviews and Meta-Analysis (‘PRISMA’) flowchart detailing literature search and review.
Fourteen studies were conducted in Asia,Reference Ahmed, Ahmad, Kaukab, Haque and Ahmed11–Reference Weerapant, Bunaprasert, Chokrungvaranont and Chentanez24 three in the USA,Reference Davis, Anson, Budinger and Kurth5,Reference Bernstein and Nelson25,Reference Katz and Catalano26 three in Europe,Reference Bendella, Spacca, Rink, Stoffels, Nakamura and Scaal8,Reference Martínez Pascual, Maranillo, Vázquez, Simon de Blas, Lasso and Sañudo27,Reference Stankevicius and Suchomlinov28 and one in Africa.Reference Thuku, Butt, Guthua and Chindia29 All studies were published between 1956 and 2019. The number of specimens in each study ranged from 20 to 350. Overall, a total of 1497 specimens were examined. The largest study was conducted by Davis et al. and involved 350 cadavers.Reference Davis, Anson, Budinger and Kurth5 Table 1 presents the baseline demographic characteristics of selected studies.
Table 1. Demographic characteristics of included studies
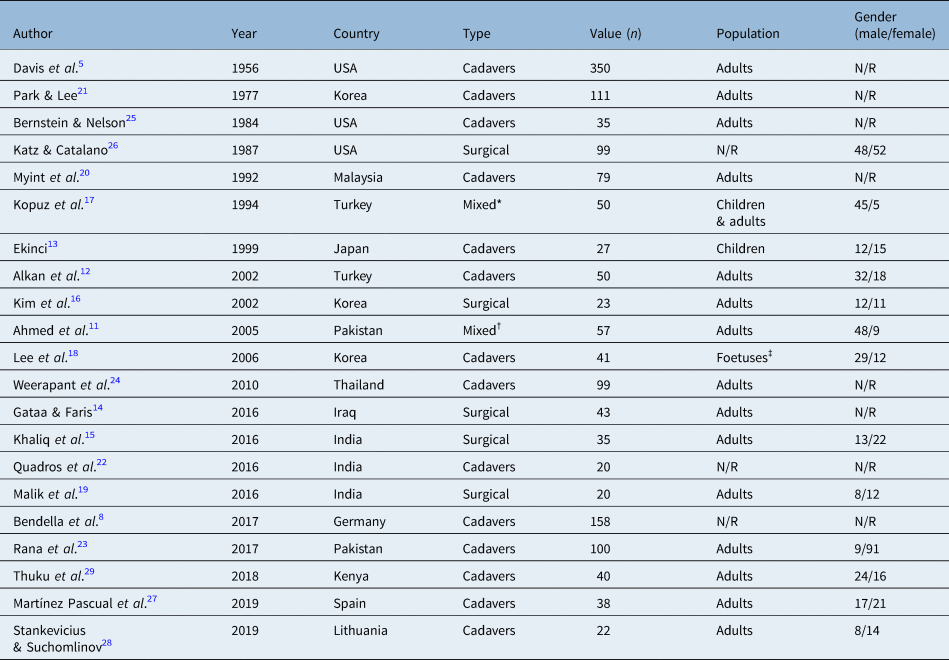
*48 cadavers and 2 patients; †42 cadavers and 15 patients; ‡38 foetuses and 3 stillborn infants. Ν/R = not reported
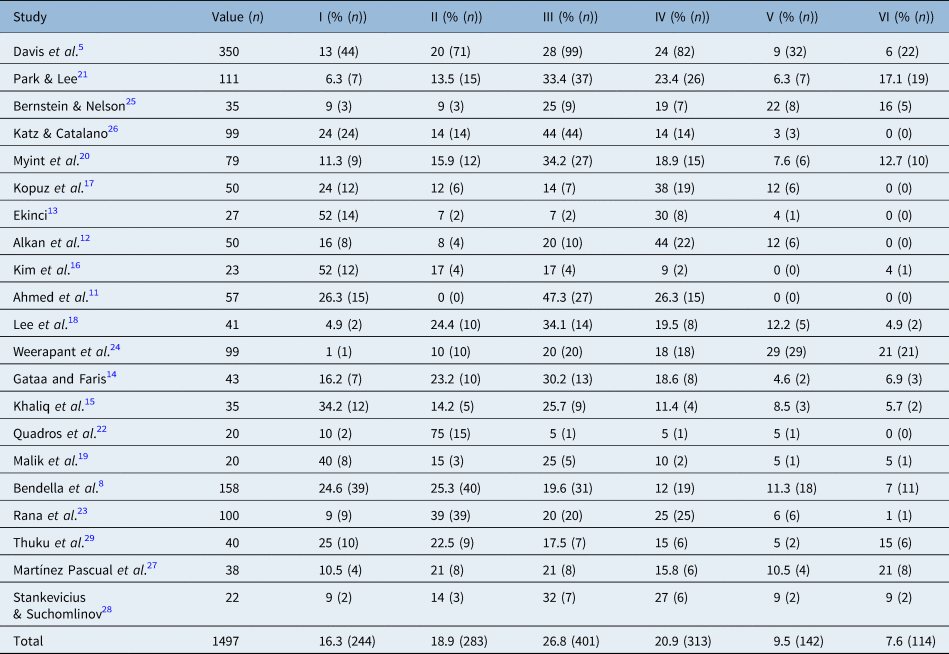
The facial nerve branching pattern was recorded in a total of 1497 cadavers or patients. The most common facial nerve branching pattern was type III (26.8 per cent), followed by type IV (20.9 per cent) and type II (18.9 per cent). The least common pattern was type VI (7.6 per cent; Table 2 and Figure 2).
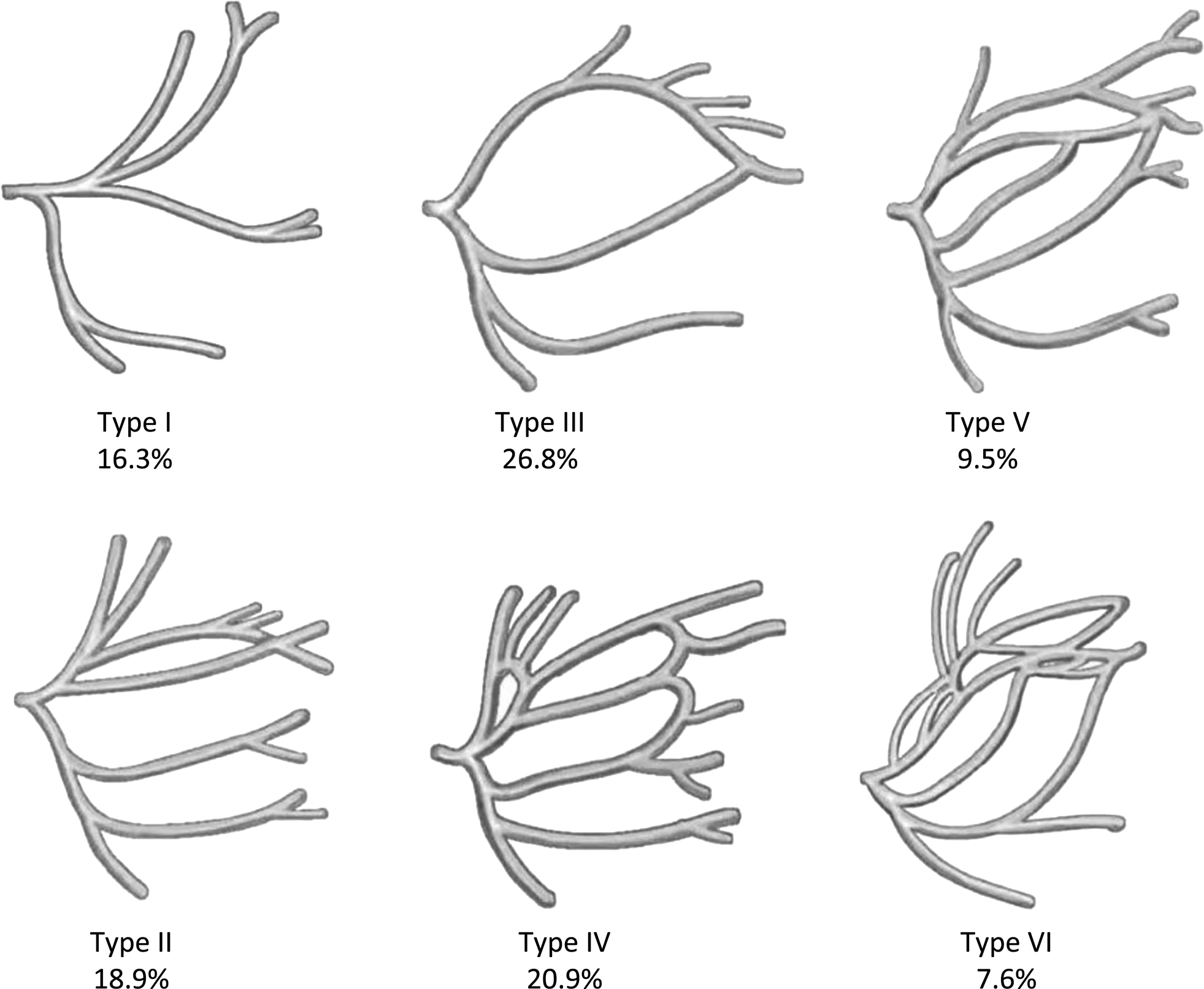
Fig. 2. Branching patterns of the facial nerve classified according to the method introduced by Davis with percentages. Type I: absence of an anastomosis between the temporofacial division and cervicofacial division; type II: anastomosis among the branches of the temporofacial division only; type III: single anastomosis among the branches of the temporofacial division and cervicofacial division; type IV: combination of type II and III; type V: double anastomosis between the temporofacial division and cervicofacial division; type VI: complex multiple anastomoses between the two divisions, where many anastomotic fibres from the cervicofacial division and the mandibular branch join the buccal branch.
Table 2. Facial nerve branching pattern according to the Davis classification
Facial nerve furcation type was recorded in 17 of the included studies. The majority of specimens (96.4 per cent) had a bifurcated main trunk of the facial nerve, and only 3.2 per cent had a trifurcation. Some studies presented specimens with no clear furcation of the main trunk. No case of quadfurcation of the main trunk was described in included studies. Table 3 shows the anatomical variations of the furcation of the facial nerve main trunk.
Table 3. Facial nerve furcation type
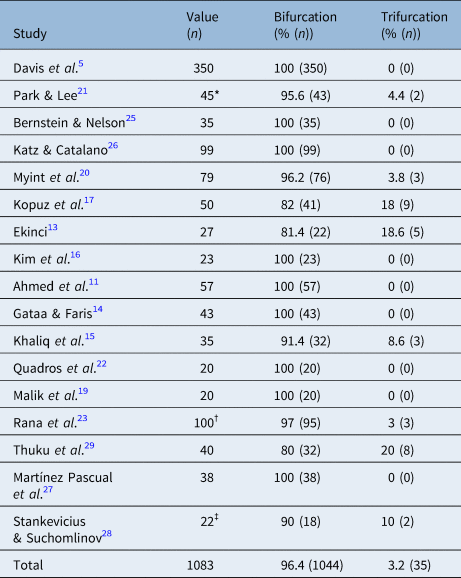
*45 out of 111 specimens studied for the furcation type; †2 of the specified had a single trunk and could not be classified; ‡2 out of 22 specimens had double trunk and could not be classified in this table
Six studies recorded the length of the facial nerve trunk (distance from stylomastoid foramen to furcation point). Four studies recorded the distance between the angle of the mandible and furcation point. Both facial nerve trunk length and its distance from angle of the mandible are presented in Table 4.
Table 4. Morphometric characteristics of the facial nerve in relation to landmarks
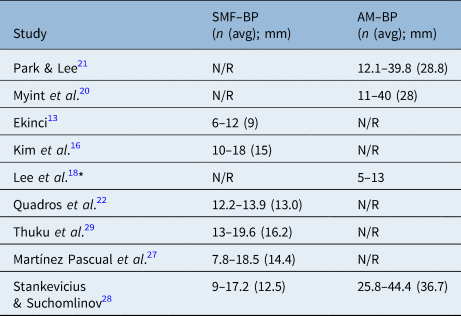
*Foetuses. SMF = stylomastoid process; BP = bifurcation point; AM = angle of the mandible; avg = average; N/R = not reported
Based on the Quality Appraisal for Cadaveric Studies scale, the study with the highest reliability was that of Thuku et al., scoring 13 of 13 points,Reference Thuku, Butt, Guthua and Chindia29 followed by the study by Stankevicius and Suchomlinov with 12 of 13 points.Reference Stankevicius and Suchomlinov28 The study with the lowest methodological quality was that by Quadros et al. with 5 of 13 points.Reference Quadros, hat, Jaison and D'Souza22 Overall, studies had an average score of eight points. Scores of individual studies are reported in Table 5.
Table 5. Score assessing the degree of realism based on Quality Appraisal for Cadaveric Studies scale (only cadaveric studies)
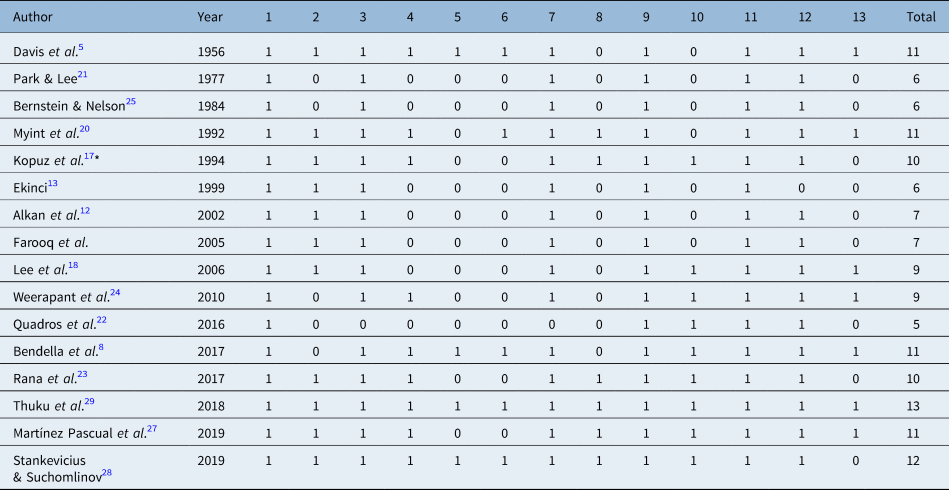
*Study was assessed as cadaveric because most specimens were cadavers. 1 = objective stated; 2 = basic information about sample; 3 = applied methods are described comprehensibly; 4 = study reports condition of the examined specimens; 5 = education of dissecting researchers is stated; 6 = findings are observed by more than one researcher; 7 = results presented thoroughly and precisely; 8 = statistical methods appropriate; 9 = details about consistency of findings are given; 10 = photographs of the observations are included; 11 = study is discussed within the context of the current evidence; 12 = clinical implications of results are discussed; 13 = limitations of the study are addressed
Discussion
Τo the best of our knowledge, this is the first systematic review to collect all existing evidence regarding facial nerve branching patterns, based on the classification proposed by Davis et al. in 1956. We found that the most common facial nerve branching pattern was type III. A bifurcated main trunk was the case for the vast majority of examined specimens. Included studies scored at least fair on the risk of bias assessment scale used, which means that the results of this systematic review can be considered reliable.
Multiple attempts have been made to classify the branching patterns of the facial nerve since the middle of the 20th century. In 1945, McCormack et al. proposed a classification with 8 different types of ramification in 100 cadaveric dissections.Reference McCormack, Cauldwell and Anson6 This pioneer study was the first to establish a classification system with statistical results. In 1956, Davis et al. dissected 350 cadavers, and they proposed a new classification system, simplifying McCormack's classification.Reference Davis, Anson, Budinger and Kurth5 This new classification included six main patterns of facial nerve ramification and is based on the anastomoses among the five main branches. Type I is the simplest (no anastomoses), and type VI is the most complex with multiple anastomoses among the main branches, except for the cervical division. The most complex patterns are related to lower risk of post-operative complications because anastomoses between nerve divisions can prevent facial palsy. The establishment of this classification determined the majority of subsequent studies of facial nerve anatomy because most of them used this classification to describe their results.
In 1987, Katz and Catalano proposed a new classification with five facial nerve branching patterns.Reference Katz and Catalano26 Types I–IV are almost identical to those described by Davis, whereas type V is characterised by two main trunks. These trunks (one major and one minor) could be considered as an early bifurcation of the nerve in the mastoid segment of the temporal bone or an anatomic anomaly because of its low frequency. It should be stated that this unusual pattern was not found by Davis et al. in a much larger sample. In 1992, Kopuz et al. proposed a classification with five main branching patterns.Reference Kopuz, Turgut, Yavuz and Ilgi17 They subcategorised the main types of ramification of the facial nerve by highlighting some topographic variations in the rise of small branches. This classification was similar to that proposed by Katz and Catalano. In 2019, Martínez Pascual et al. combined the classifications of Davis et al., Katz and Catalano and Kopuz et al. and proposed a 12-type branching pattern classification including every possible pattern.Reference Martínez Pascual, Maranillo, Vázquez, Simon de Blas, Lasso and Sañudo27 In 2021, Alomar presented a study of 460 patients and suggested a totally different classification system based on surgical landmarks that help surgeons identify the main trunk of the facial nerve.Reference Alomar30
We found that the type I facial nerve branching pattern, which is characterised by no anastomoses between the main ramifications, accounts for only 16.3 per cent of specimens. The vast majority of anatomical books present this branching pattern as the normal anatomy of the facial nerve course. However, it seems that this simple ramification pattern constitutes the fourth most frequent anatomic variation. In 1999, Ekinci presented a study of 27 child cadavers. In this study, facial nerve branching pattern type I was the most common (52 per cent). These results led the author to make the hypothesis that anastomoses among branches may occur later in adult life.Reference Ekinci13 However, this attractive hypothesis was not supported by later studies. Interestingly, in 2006, Lee et al. presented a study of 41 foetuses and newborn cadavers in which the type I branching pattern was found only in 4.9 per cent of the specimens and was classified as the most infrequent among all types.Reference Lee, Young and Kim18
We also showed that the type III branching pattern of the facial nerve is the most common, with a frequency of 26.8 per cent. It is characterised by a single anastomosis between the temporofacial and cervicofacial divisions. Type IV is the second most common pattern (20.9 per cent). This pattern is more complex, with two anastomotic loops between the temporofacial and cervicofacial divisions. Type II (18.9 per cent), type V (9.5 per cent) and type VI (7.6 per cent) constitute the remaining branching patterns of facial nerve. Overall, our results agree with those reported by Davis et al. Racial differences seem to exist, but there is no conclusive evidence to support them. Thuku et al., in a study of a black African population showed that type I and type II are the most dominant. However, a sample of 40 specimens does not suffice to extract safe conclusions.Reference Thuku, Butt, Guthua and Chindia29
Bifurcation of the main trunk seems to be the dominant furcation type, while trifurcation has only been the case in 3.2 per cent of the specimens. Quadrification of the main trunk is also possible,Reference Baker and Conley31 while cases with a single trunk have also been documented in the literature.Reference Rana, Akhtar, Atif and Javaid23 Stankevicius and Suchomlinov reported that two (9 per cent) out of 22 studied specimens had two separate main trunks emerging from the skull base.Reference Stankevicius and Suchomlinov28 This anatomical feature of a ‘double-trunk’ facial nerve is rather rare and has only been reported a few times. Specifically, Katz and Catalano reported that the incidence of this variation was 3 per cent,Reference Katz and Catalano26 and Kopuz et al. reported only 1 case (2 per cent).Reference Kopuz, Turgut, Yavuz and Ilgi17 These anatomical variations should always be kept in mind, especially when performing parotid surgery, in order to avoid accidental injury of the nerve.
The importance of the extratemporal facial nerve main trunk length, as measured from the point of its exit from the stylomastoid foramen to its bifurcation, has been previously highlighted by many studies. The facial nerve must be long enough to allow an anastomosis with neither tension nor looseness.Reference Salame, Ouaknine, Arensburg and Rochkind9 Facial nerve trunk length does not seem to be fixed and ranged from 12.5 mm to 16.2 mm among included studies. Salame et al. measured facial nerve length in 46 specimens and reported a value of 16.44 ± 3.20 mm.Reference Salame, Ouaknine, Arensburg and Rochkind9 Nishanthi et al. (2006) presented an even longer value (18.51 ± 3.80 mm).Reference Nishanthi, Hewapathirana and Nanayakkara32 Τhe only study that presented morphometric data in children was that of Ekinci. The average length in children's facial nerve main trunk was 4 mm shorter than that of adults.Reference Ekinci13 This finding comes as no surprise because the total length of the nerve depends on the height of the specimen.
The results of our systematic review are liable to certain limitations. To begin with, for the sake of greater power, we included both cadaveric and surgical studies. The vast majority of surgical patients were dissected during parotidectomy, and one should keep in mind that parotid gland tumours tend to exert pressure on the facial nerve and change its anatomic relations. On the other hand, cadaveric specimens almost always have no parotid gland pathology, and dissection is meticulous without risk of iatrogenic injury. Furthermore, we decided to include only studies examining facial nerve branching patterns based on the Davis classification. Therefore, the risk of excluding high quality studies or studies with a large sample size because they used a different classification is not to be underestimated. Additionally, studies were deemed eligible for inclusion if they presented their results using a classification similar to that of Davis. Finally, as most of the studies did not present the number of variants by gender, age or ethnicity, we were not able to perform subgroup analyses.
Conclusion
Accurate knowledge of facial nerve anatomy, topography and morphometry is a prerequisite for performing facial interventions and especially parotid gland surgery. Many studies have examined the branching pattern of the facial nerve, presenting considerably different results and proposing different classifications. It seems that the Davis classification remains the most practical because it focuses on the main anatomical variations, with no complex details that could potentially confuse the surgeon.
Competing interests
None declared









