Preventing youth suicide is an urgent public health need. Suicide is the second cause of death for young people aged 15–24, and reports of suicidal thoughts and behaviors (STBs) have risen in the past 10 years (Curtin & Heron, Reference Curtin and Heron2019; Kann et al., Reference Kann, McManus, Harris, Shanklin, Flint, Queen, Lowry, Chyen, Whittle, Thornton, Lim, Bradford, Yamakawa, Leon, Brener and Ethier2018). Data from both self-reported and clinical assessments suggest that maltreated youth are more likely to consider and attempt suicide (Angelakis et al., Reference Angelakis, Austin and Gooding2020; Norman et al., Reference Norman, Byambaa, De, Butchart, Scott and Vos2012). A recent meta-analysis showed young people who experienced any type of child abuse or neglect were 2.91 times more likely to attempt suicide and 2.36 times more likely to have suicidal ideation compared to their non-maltreated counterparts, respectively (Angelakis et al., Reference Angelakis, Austin and Gooding2020). The prevalence of child maltreatment in the United States is substantial, making its impact on youth suicide alarming. There were over 3.4 million children involved in a child maltreatment investigation in the United States in 2019 (U.S. Department of Health & Human Services, Administration for Children and Families, Administration on Children, Youth and Families, 2021). Further, estimates show 37.4% of US youth are involved in a child maltreatment investigation by the time they reach age 18 (Kim et al., Reference Kim, Wildeman, Jonson-Reid and Drake2017). Globally, the World Health Organization (2020) estimates approximately one billion children aged 2–17 experience violence such as child maltreatment each year. Thus, suicide prevention for maltreated youth globally is an urgent public health problem.
A large body of research exists on the associations between child maltreatment and suicide risk (for a review, see Miller et al., Reference Miller, Esposito-Smythers, Weismoore and Renshaw2013), but scientists have yet to consolidate this body of knowledge into a conceptual model to guide research and prevention in this area. In the present paper, we argue that suicide prevention for maltreated youth will benefit from integrating theories of suicide with developmental perspectives, which give attention to age-specific mechanisms and antecedents of STBs in this vulnerable youth population. While current theoretical models of suicide (e.g., the interpersonal theory of suicide) specify the causal mechanisms that underlie STBs among adult samples, they have largely not integrated developmental perspectives on youth suicide.
A developmental lens is essential for understanding the etiology between child maltreatment and STBs during adolescence, specifically. Adolescence is a developmental period wherein young people undergo multiple changes at the biological, psychological, and interpersonal levels (e.g., puberty, the development of romantic relationships, and transitioning to spending more time with peers than family members). There is evidence that adolescence is a sensitive period in development with heightened brain plasticity (Fuhrmann et al., Reference Fuhrmann, Knoll and Blakemore2015). This makes adolescence both a time of vulnerability and opportunity. While adolescents are often at risk for the onset of mental health disorders (Kessler et al., Reference Kessler, Berglund, Demler, Jin, Merikangas and Walters2005), heightened plasticity during this time confers a “window of opportunity” for preventive programs that build upon youth strengths to prevent suicide (Wyman, Reference Wyman2014).
Overall, a developmental model of the link between child maltreatment and youth suicide will contribute to this research area by offering (a) hypothesized mechanisms underlying the link between child maltreatment and youth suicide; (b) hypothesized risk and protective factors for youth STBs; and (c) implications for preventative efforts. Specifying the role of child maltreatment in the developmental processes leading to youth STBs, as opposed to the role of other childhood adversities (e.g., poverty, parental incarceration, divorce), is an important endeavor due to the unique nature of child maltreatment as a toxic interpersonal stressor and the salience of interpersonal stressors in the etiology of STBs (Van Orden et al., Reference Van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner2010). Children exposed to maltreatment not only experience extreme and often chronic stress, but often do so at the hands of their primary or secondary attachment figures. Ultimately, an integrative developmental conceptual model of the link between child maltreatment and youth suicide will inform targeted prevention efforts to reduce the rates of STBs among youth with child maltreatment experiences.
Consequently, in this paper we will outline the current knowledge on child maltreatment and youth suicide and review the theoretical frameworks that guide our conceptual model, which are primarily the developmental psychopathology perspective and ideation-to-action theories of suicide. Next, based on the literature and our existing theoretical frameworks, we will propose a developmentally informed conceptual model for the association between child maltreatment and suicide risk. The purpose of this conceptual model is to propose developmental pathways from child maltreatment to youth suicide that are based on the existing literature and relevant theoretical models (McGregor, Reference McGregor2018). Note that we do not intend for this model to be exhaustive nor to present a formal causal theory, but instead to offer insight and future directions for research in this specific area. Last, we will discuss implications of this model for advancing efficacious suicide prevention efforts, with a focus on upstream prevention.
Youth suicidal thoughts and behaviors: definitions and overview
We define STBs as including cognitions or actions (non-fatal or fatal) that involve intent to die. Specifically, suicidal ideation is defined as “thinking about, considering, or planning for suicide” (Crosby et al., Reference Crosby, Ortega and Melanson2011, p. 21), suicide attempts are defined as “a non-fatal self-directed potentially injurious behavior with any intent to die as a result of the behavior” (Crosby et al., Reference Crosby, Ortega and Melanson2011, p. 21), and suicide as “death caused by self-directed injurious behavior with any intent to die as a result of the behavior” (Crosby et al., Reference Crosby, Ortega and Melanson2011, p. 21). Although suicidal ideation, attempts, and suicide are correlated, they differ significantly in etiology and prevalence, and therefore should be investigated separately. Suicidal ideation increases the likelihood of a suicide attempt, but most individuals who think about suicide do not ultimately attempt or die by suicide (Klonsky et al., Reference Klonsky, May and Saffer2016). For instance, an estimated 12.0 million adults in the United States exhibited suicidal ideation and 1.4 million attempted suicide in the year 2019 (U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, 2020). Thus, informed by recommendations in the suicide literature, we will be referring to suicidal thoughts and suicidal behaviors as separate but related phenomena.
Child maltreatment and suicide risk
Current state of the literature
Direct associations
There is consensus in the literature that child maltreatment experiences heighten the risk for future STBs (for a review, see Miller et al., Reference Miller, Esposito-Smythers, Weismoore and Renshaw2013). Investigators have found significant associations between childhood maltreatment and adolescent suicidal ideation (Fergusson et al., Reference Fergusson, Woodward and Horwood2000) and attempts (Fergusson et al., Reference Fergusson, Woodward and Horwood2000; Rhodes et al., Reference Rhodes, Boyle, Bethell, Wekerle, Goodman, Tonmyr, Leslie, Lam and Manion2012) using both cross-sectional (Hoertel et al., Reference Hoertel, Franco, Wall, Oquendo, Wang, Limosin and Blanco2015) and prospective designs (Fergusson et al., Reference Fergusson, Woodward and Horwood2000). These results extend to studies with young adults (Dunn et al., Reference Dunn, McLaughlin, Slopen, Rosand and Smoller2013; Johnson et al., Reference Johnson, Cohen, Gould, Kasen, Brown and Brook2002; Puzia et al., Reference Puzia, Kraines, Liu and Kleiman2014) and adult samples (Dube et al., Reference Dube, Anda, Felitti, Chapman, Williamson and Giles2001). In a nationally representative sample of maltreated youth, researchers found that 23% of adolescents reported suicidal ideation (Coohey et al., Reference Coohey, Dirks-Bihun, Renner and Baller2014). Additionally, a study using a population-based Canadian sample found adolescents permanently removed from their homes due to maltreatment were five times more likely to present to the emergency department for STBs, compared to non-maltreated youth (Rhodes et al., Reference Rhodes, Boyle, Bethell, Wekerle, Goodman, Tonmyr, Leslie, Lam and Manion2012).
Mediators
Although the association between child maltreatment and youth STBs is well established, there is less research and subsequently less consensus on the mechanisms of this association. In other words, although we know that child maltreatment confers risk for STBs during adolescence and young adulthood, we have much to learn regarding the developmental processes that underlie this association. Thus, to inform our proposed conceptual model, we conducted a literature review on the mechanisms between child maltreatment and youth STBs (see Table 1 for a summary). This review highlights that the processes in the association between child maltreatment and youth suicide are multi-level in nature, spanning from interpersonal factors (e.g., mother-daughter relationship problems; Handley, Adams, et al., Reference Handley, Adams, Manly, Cicchetti and Toth2019) to psychological factors such as internalizing symptomology (Kwok & Gu, Reference Kwok and Gu2019; Paul & Ortin, Reference Paul and Ortin2019). In Table 1, we categorized the literature by type of mediator (i.e., biological, psychological, or interpersonal) and type of outcome (i.e., suicidal ideation, suicidal behavior, or a combination). It is clear from our findings that there are notable gaps in the literature. Most studies have focused on individual-level psychopathology or symptomology as mediators. Additionally, most studies use suicidal ideation as a primary outcome, and thus there is a need for more research on mediators linking child maltreatment to suicidal behavior. Additionally, there is a lack of research on biological mechanisms in the association between child maltreatment and youth suicide (as an exception, see Russell et al., Reference Russell, Heron, Gunnell, Ford, Hemani, Joinson, Moran, Relton, Suderman and Mars2019).
Table 1. Identified mediators in the association between child maltreatment and adolescent and young adult STBs

Note. Emotional abuse includes verbal abuse. Neglect includes physical and emotional neglect. Studies using ACE measures (broadly defined) not included in table.
*Studies using longitudinal or prospective designs.
a Finding was significant for boys only.
b Finding was significant for girls only.
Moderators
Similar to the literature on mediators of child maltreatment and youth suicide, moderators (e.g., risk or protective factorsFootnote 1 ) in the association between maltreatment and youth STBs range from biological to contextual factors (see Table 2). For example, individual traits such as empathy, problem-solving, and emotional competence have all been found to be protective factors in the association between child maltreatment and youth suicidal ideation in US-based and international samples (Esposito & Clum, Reference Esposito and Clum2002; Kwok et al., Reference Kwok, Yeung, Low, Lo and Tam2015; Low et al., Reference Low, Kwok, Tam, Yeung and Lo2017), while substance use problems were found to amplify this association (Miller & Esposito-Smythers, Reference Miller and Esposito-Smythers2013). At the interpersonal level, there is evidence for protective factors including social support (Esposito & Clum, Reference Esposito and Clum2002; Logan-Greene et al., Reference Logan-Greene, Tennyson, Nurius and Borja2017), school belonging (Zhang et al., Reference Zhang, Liu and Long2020), and participation in youth activities (Cero & Sifers, Reference Cero and Sifers2013). Researchers also note evidence for biological modifying factors, such as the oxytocin genotype (CD38), in the association between child maltreatment and youth STBs (Handley, Warmingham, et al., Reference Handley, Warmingham, Rogosch and Cicchetti2019). However, more research is needed to identify and replicate protective and moderating risk factors that modify the association between child maltreatment and youth STBs. Additionally, there are very few studies investigating protective factors between child maltreatment and suicidal behavior specifically.
Table 2. Identified moderators in the association between child maltreatment and adolescent and young adult STBs

Note. Emotional abuse includes verbal abuse. Neglect includes physical and emotional neglect. Studies using ACE measures (broadly defined) not included in table.
*Studies using longitudinal or prospective designs.
a This result was found among adolescents in Kenya but not in the other countries investigated (Haiti, Tanzania).
b Outcome measure was suicidal behavior, consisting of actual, attempted, and ambiguous suicide attempts and visits to the emergency room for severe suicidal ideation.
c Outcome measure was a composite of suicidal behavior, consisting of behavioral preparation for suicide attempts, efforts to avoid communication about suicide ideation, and lethality of attempt.
d The association between child maltreatment and suicide attempts was significant for females but not for males.
The literature suggests the link between child maltreatment and STBs have different etiological mechanisms for boys and girls (e.g., moderation by gender). For example, Ammerman et al. (Reference Ammerman, Serang, Jacobucci, Burke, Alloy and McCloskey2018) observed a significant association between child maltreatment and suicide attempts for girls but not boys. Similarly, Cromer et al. (Reference Cromer, Villodas and Chou2019) found that depressive symptoms mediated the association between cumulative child maltreatment exposure and suicidal ideation among girls only. Last, Barbot et al. (Reference Barbot, Eff, Weiss and McCarthy2020) found that psychosis mediated the association between emotional abuse and suicide attempts for girls only, while mood disorder symptoms mediated this association for boys only.
Current theoretical models of suicide
Research on child maltreatment and youth STBs must be guided by relevant theories in the field of suicidology. Our conceptual model of child maltreatment and youth STBs is specifically guided by the interpersonal theory of suicide (Van Orden et al., Reference Van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner2010), due to the salience of interpersonal stressors for maltreated youth, as well as other ideation-to-action frameworks of suicide (Klonsky & May, Reference Klonsky and May2015). The interpersonal theory of suicide proposes that individuals develop a desire for suicide through two interpersonal processes, thwarted belongingness (i.e., social isolation or lack of social connectedness) and perceived burdensomeness (i.e., the belief that one is a burden to close others, which includes aspects of self-hatred and the belief that one’s life is a liability; Van Orden et al., Reference Van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner2010). Further, an acquired capability for suicide (i.e., learned fearlessness of death and tolerance for pain) is required for suicidal behaviors and suicide to occur. Other ideation-to-action frameworks of suicide similarly propose that the pathways leading to risk for suicidal ideation differ from those leading to suicidal behavior and suicide. For example, according to the three-step theory of suicide, psychological pain and hopelessness are critical explanatory factors for the development of suicidal ideation, while the progression from suicidal ideation to suicidal behavior is explained by one’s capacity to inflict self-injury (Klonsky & May, Reference Klonsky and May2015). We draw from these current theories of suicide in our conceptual model by differentiating the processes leading to suicidal ideation and suicidal behaviors.
In the field of suicidology, the preponderance of theoretical models are based on adult samples and lack a developmental perspective specific to youth suicide risk. Current theories in suicidology such as the ones above suggest the same set of risk and protective factors for suicide for all individuals despite their age and/or developmental stage. Some mechanisms towards suicide (e.g., depression) indeed are most likely the same for all individuals across development. However, other mechanisms and risk and protective factors are likely more salient for adolescents and young adults due to normative developmental changes and the stage-salient developmental tasks during this period. For instance, adolescent risk factors such as a lack of future orientation (i.e., having low or no expectations or goals for one’s future; Oshri, Duprey, et al., Reference Oshri, Duprey, Kogan, Carlson and Liu2018) and bullying may not be as relevant for older individuals. Adolescents are also particularly sensitive to acute stress due to normative developmental changes in biological stress response systems, and “failure” of these stress response systems have been proposed as a key risk factor for adolescent suicide (Miller & Prinstein, Reference Miller and Prinstein2019). These risk factors may be particularly salient for maltreated youth, and may moderate (i.e., exacerbate) the association between maltreatment and youth STBs. Additionally, theories in suicidology tend to be broad and do not specify the hypothesized developmental chain stemming from a triggering event, such as child maltreatment, towards youth STBs.
A developmentally informed model of child maltreatment and youth suicide will contribute to the literature by considering the unique aspects of the developmental period across multiple levels of analysis with the aim of identifying salient risk and protective factors and mechanisms. This will inform research in several ways, including but not limited to measurement (e.g., using appropriate measures for the specific developmental stage being tested), conceptualization (e.g., how concepts are operationalized and tested for adolescents compared to older adults), and study design (e.g., sampling and recruitment). Further, a developmentally informed model of suicide will contribute to applied research by providing developmentally appropriate mechanisms to target in interventions (e.g., targeting attachment processes for children or peer skills among high school students), and by emphasizing that mechanistic targets will be different and must be tuned to participants’ developmental stage. Importantly, the model we present in this paper focuses on child maltreatment as a specific precursor to suicide risk. Thus, our model is specific to maltreated youth and is intended to inform suicide prevention approaches among youth exposed to child abuse and neglect.
A developmental perspective on youth STBs
We utilize a developmental psychopathology perspective to understand and integrate the disparate literature on mechanisms and moderators in the link between child maltreatment and youth STBs, and to inform our conceptual model of the pathways from child maltreatment to youth STBs. Developmental psychopathology is an overarching framework for studying typical and atypical behavior (Cicchetti, Reference Cicchetti1984). Several core principles of this framework shape our proposed conceptual model, including the principles of equifinality and multifinality. According to the concept of equifinality, the same outcome can be reached through multiple different developmental pathways (Cicchetti & Rogosch, Reference Cicchetti and Rogosch2002). For example, two adolescents who each exhibit suicidal ideation may have reached that outcome through various developmental risk processes: one may have experienced extreme early childhood neglect, resulting in an insecure attachment relationship that cascaded into mistrust of others, social isolation, and depression; the other may have experienced physical abuse that resulted in externalizing behaviors and impulsivity. These illustrative developmental pathways, although different, each may predict the emergence of STBs during adolescence. Alternatively, according to the concept of multifinality, the same or a similar set of risk factors may result in different processes and outcomes (Cicchetti & Rogosch, Reference Cicchetti and Rogosch2002). For example, two children who were sexually abused may show distinct outcomes by exhibiting either psychopathology or resilience in adolescence. Different risk factors (e.g., disordered neighborhoods, peer victimization) and protective factors (e.g., peer social support, emotion regulation) contribute to the process of multifinality by modifying (i.e., moderating) the outcomes stemming from child maltreatment, including the developmental processes that are implicated in the pathway from child maltreatment towards youth STBs. Additionally, risk and protective factors at different levels of the youths’ ecology may interact with one another to produce cascading transactional effects that lead to diverse outcomes.
The developmental systems perspective, which has over time been integrated into the developmental psychopathology approach, informs the concepts of multifinality and equifinality (Lerner & Castellino, Reference Lerner and Castellino2002). According to this perspective, developmental processes emerge from integrating multiple systems, both internal and external to the individual (Lerner & Castellino, Reference Lerner and Castellino2002). Here, systems are defined as “…a complex of interacting components together with the relationships among them that permit the identification of a boundary-maintaining entity or process” (Laszlo & Krippner, Reference Laszlo, Krippner and Jordan1998, p. 47). A growing child, in this perspective, is thought of as a developmental system that consists of the elements or subsystems within it (e.g., biological systems) that change over time due to the interactions among internal subsystems and with other outside systems (e.g., the family system). In our conceptual model, we draw from the transactional model of the developmental systems perspective, which posits that human development is the product of interdependent and bidirectional influences between the person and their environment (Sameroff, Reference Sameroff2009). Transactions can also occur between different subsystems within the individual. For example, the development and functioning of the stress response system and the immune system may both influence one another bidirectionally over time (Oshri, Duprey, Liu & Ehrlich, Reference Oshri, Duprey, Liu and Ehrlich2020; Sameroff, Reference Sameroff2009).
The proposed theoretical model was also informed by the organizational theory of development, a core tenet of the developmental psychopathology approach. According to the organizational theory, children must successfully master stage-salient developmental tasks, such as attaining secure attachment with a primary caregiver or gaining a positive self-concept and sense of mastery in early childhood (Cicchetti & Banny, Reference Cicchetti, Banny, Lewis and Rudolph2014). At each stage of development, the attainment of new developmental tasks requires reorganizing multiple systems within the individual (e.g., physiological, cognitive, and socioemotional). Successful reorganization is necessary to master subsequent tasks in the same developmental domain. Harsh, chaotic, or impoverished rearing environments can lead to failure in mastering critical developmental tasks (Cicchetti & Banny, Reference Cicchetti, Banny, Lewis and Rudolph2014). Accordingly, children who experience child maltreatment are at risk for STBs due in part to disruption in the attainment of stage-salient tasks.
The aforementioned tenets of the developmental psychopathology and developmental systems frameworks have been integrated into several existing models of youth STBs, including models on the development of borderline personality disorder and self-injurious behaviors (Crowell et al., Reference Crowell, Beauchaine, Lenzenweger, Beauchaine and Hinshaw2008; Derbridge & Beauchaine, Reference Derbridge, Beauchaine, Lewis and Rudolph2014), the developmental-transactional model of youth suicidal behavior (Bridge et al., Reference Bridge, Goldstein and Brent2006), and the recent theory of adolescent suicide as a failure of physiological stress response systems (Miller & Prinstein, Reference Miller and Prinstein2019). Our model adds to this knowledge base by considering the developmental processes involved in the emergence of youth STBs specifically for maltreated youth. Additionally, our conceptual model integrates the developmental psychopathology and developmental systems frameworks with modern theories of suicide, including the interpersonal theory of suicide and other ideation-to-action frameworks of suicide, as detailed prior (Klonsky & May, Reference Klonsky and May2015; Van Orden et al., Reference Van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner2010).
A conceptual model of child maltreatment and youth suicide risk
Based on the literature reviewed above, the developmental psychopathology framework, and ideation-to-action theories in suicidology, we propose a developmental model of the progression from child maltreatment to adolescent STBs (see Figure 1). There are three overarching propositions to this model. First, we suggest three primary, dynamic mechanisms at different levels of analysis (i.e., biological, psychological, and interpersonal) that link child maltreatment to the emergence of STBs in adolescence. These mechanisms are not separate processes, but instead interact with and influence one another over time. Together, in line with the three-step theory of suicide, these biological, psychological, and interpersonal processes may culminate in extreme psychological pain that can prompt youth to desire ending their lives (Klonsky & May, Reference Klonsky and May2015).
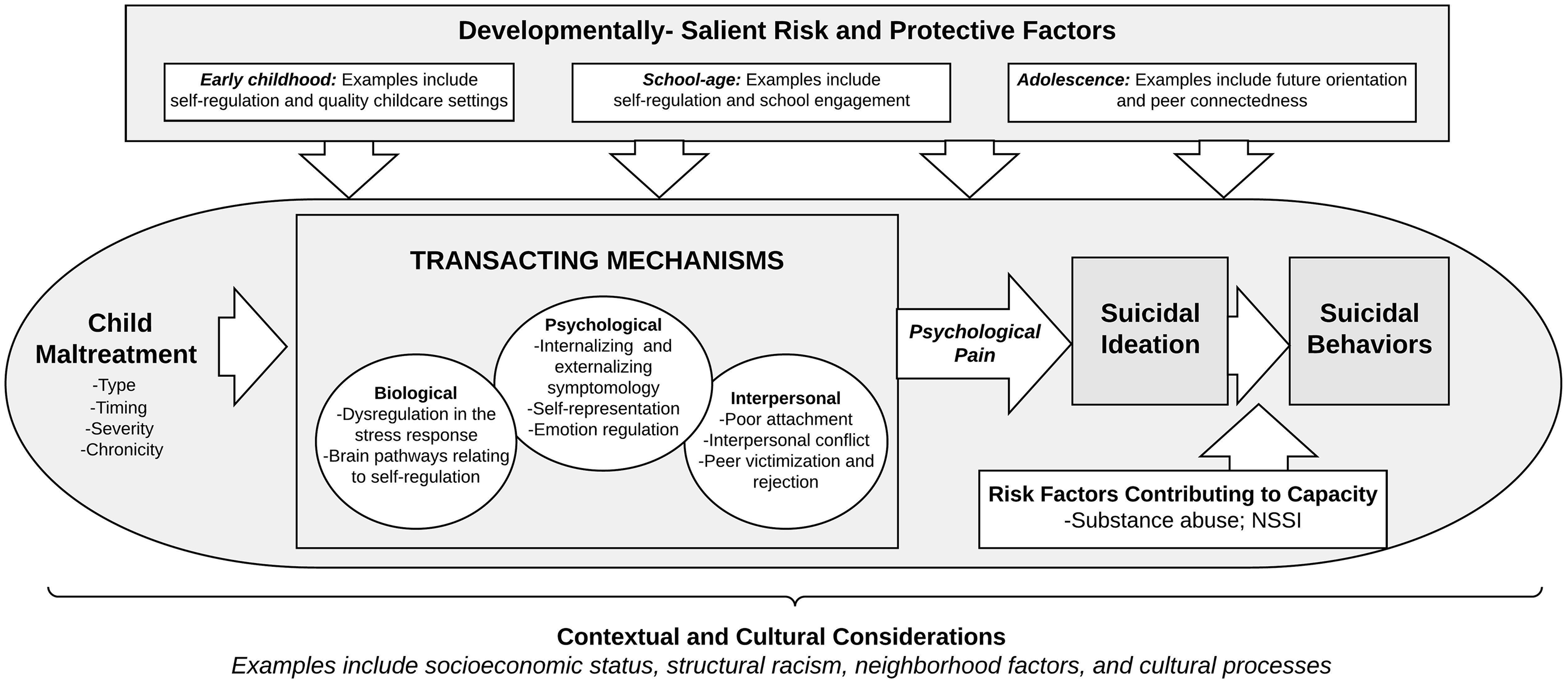
Figure 1. Developmental conceptual model of child maltreatment and youth suicidal thoughts and behaviors.
Second, we propose developmentally salient risk factors for adolescent STBs, such as pubertal development, stressful life events, and peer problems, and protective factors such as school belonging and future orientation. Last, in line with ideation-to-action frameworks of suicide, we propose that for youth with maltreatment experiences, the progression from suicidal ideation to suicidal behaviors is exacerbated by individual vulnerabilities that may increase youths’ propensity for participating in suicidal behaviors. Such vulnerabilities include consequences of child maltreatment, such as dysregulation of the physiological stress response, substance use behaviors, and non-suicidal self-injury (NSSI). External factors associated with child maltreatment, such as recent stressful life events, may also exacerbate the pathway from suicidal ideation to suicidal behaviors. This third aspect of our model, which explains the transition from suicidal ideation to behaviors, differentiates our model from other etiological theories for related psychopathology outcomes.
Together, our model proposes a set of risk factors and a set of hypothesized relations between these risk factors. Consistent with the concept of multifinality, many of our proposed risk factors (e.g., child maltreatment exposure, interpersonal risk factors, and psychopathology) are general-risk factors that are associated not only with STBs but other adverse outcomes such as substance use disorders or NSSI. However, several aspects of our model are specific to STBs. For instance, psychological pain (i.e., psychache or mental pain) is a suicide-specific risk factor that we propose results from several multi-level transacting developmental mechanisms. A recent systematic review revealed that mental pain is a predictor of suicide risk both within clinical samples of adolescents and adults and within non-clinical samples (Verrocchio et al., Reference Verrocchio, Carrozzino, Marchetti, Andreasson, Fulcheri and Bech2016). Additionally, we propose several suicide-specific risk factors that are involved in the progression from suicidal ideation to suicide attempts. Thus, the following model of child maltreatment and youth STBs is specific to the goal of understanding the development of youth STBs, and can be used to guide suicide-specific prevention interventions.
Considering the dimensionality of child maltreatment
Our model considers the complex and multidimensional nature of child maltreatment experiences and how this influences developmental trajectories towards suicide risk. Child maltreatment can be measured along several dimensions including type, severity, developmental timing (i.e., the age or developmental stage at which maltreatment occurs), relationship with the perpetrator (i.e., familial versus non-familial), and chronicity (i.e., whether maltreatment occurs once or is a recurring event throughout childhood; English et al., Reference English, Upadhyaya, Litrownik, Marshall, Runyan, Graham and Dubowitz2005; Manly et al., Reference Manly, Kim, Rogosch and Cicchetti2001). Accounting for the dimensionality of child maltreatment is important not only for ecologically valid measurement, but also per the developmental psychopathology theoretical framework. Different dimensions of child maltreatment represent distinct experiences children may have in their rearing environment. Consequently, the complexity in child maltreatment experiences contributes to the multifinality in youth developmental outcomes. This complexity is particularly important to consider in our model of child maltreatment and youth STBs, as different dimensions of child maltreatment experiences can differentially impact the developmental mechanisms that are most salient in the pathway to youth STBs. Additionally, the dimensionality of child maltreatment has implications for the way maltreatment is operationalized and modeled. For instance, within samples of maltreated youth, dimensions of maltreatment such as severity or perpetrator type may moderate the association between maltreatment exposure and youth STBs.
Developmental timing and chronicity of maltreatment are critical to consider in the context of youth STBs. According to the organizational theory of development, maltreatment will impact the stage-salient developmental tasks that correspond to the developmental stage of the child when maltreatment occurs. Consequently, which developmental tasks are disrupted will impact children’s and adolescents’ developmental trajectories and the possible emergence of psychopathology. For instance, maltreatment during infancy may reasonably disrupt the attainment of a secure attachment relationship with a primary caregiver (Stronach et al., Reference Stronach, Toth, Rogosch, Oshri, Manly and Cicchetti2011). In contrast, maltreatment that occurs during adolescence may disrupt salient milestones such as identity development. Likewise, maltreatment is often chronic throughout childhood and adolescence (Warmingham et al., Reference Warmingham, Handley, Rogosch, Manly and Cicchetti2019), and this chronicity can influence the developmental pathways to youth suicidal thoughts and behaviors. Chronic childhood maltreatment that occurs in several developmental stages may upend the attainment of multiple stage-salient developmental tasks, compounding the risk for subsequent psychopathology outcomes, including STBs. Several studies have indeed investigated maltreatment timing and chronicity in relation to subsequent suicidal thoughts and behaviors during adolescence. In the National Longitudinal Study of Adolescent Health, adolescents who were first exposed to physical abuse in preschool (i.e., ages 3–5) or in adolescence (i.e., ages 11–17), and adolescents who were first exposed to sexual abuse in preschool, had a heightened risk for suicidal ideation (Dunn et al., Reference Dunn, McLaughlin, Slopen, Rosand and Smoller2013). Further, emerging adults who first experienced maltreatment during infancy were more likely to exhibit suicidal ideation compared to those who first experienced maltreatment in later childhood (Handley, Warmingham, et al., Reference Handley, Warmingham, Rogosch and Cicchetti2019).
The developmental timing and chronicity of child maltreatment are also pertinent to the onset and timing of youth STBs. In a cross-national study, a history of childhood physical or sexual abuse increased the odds of a suicide attempt in childhood (i.e., ages 4–12) by 6–10-fold, respectively (Bruffaerts et al., Reference Bruffaerts, Demyttenaere, Borges, Haro, Chiu, Hwang, Karam, Kessler, Sampson, Alonso, Andrade, Angermeyer, Benjet, Bromet, de Girolamo, de Graaf, Florescu, Gureje, Horiguchi and Nock2010). The same study showed that childhood abuse had a smaller but still significant impact on the onset of suicidal behavior in young adulthood and adulthood (OR range: 2.5–3.1). However, child maltreatment was assessed retrospectively, and thus it is unclear whether timing of childhood sexual and physical abuse played a role in the onset and timing of suicidal behavior. Theoretically, the timing of child maltreatment may be related to both the onset of youth STBs and the mechanisms relevant to this onset. Childhood maltreatment that is chronic throughout both childhood and adolescence may reasonably be related to an earlier onset of STBs that occurs concurrently with the abuse. However, more research is needed to assess how timing and chronicity of child maltreatment is related with timing (e.g., onset and persistence) of youth STBs.
Different subtypes of maltreatment may also impact unique developmental processes that serve as mechanisms linking maltreatment to subsequent STBs. There is indeed evidence for the impact of maltreatment type on eventual STB outcomes. For example, a recent meta-analysis showed differential associations between child maltreatment type and risk for suicidal behavior among young people. Findings showed that sexual abuse contributed to a 3.41-fold increase in odds of suicidal behavior, while physical neglect contributed to a 1.79-fold increase in odds of suicidal behavior (Angelakis et al., Reference Angelakis, Austin and Gooding2020). Relatedly, recent perspectives on childhood adversity posit that threat (e.g., physical abuse) and deprivation (e.g., neglect) are unique aspects of adversity with specific mechanisms towards adverse outcomes (McLaughlin & Sheridan, Reference McLaughlin and Sheridan2016). For instance, disruptions to emotional processing are hypothesized to be a primary mechanism linking experiences of threat to adverse psychopathology outcomes (McLaughlin & Sheridan, Reference McLaughlin and Sheridan2016). Further research is needed that incorporates dimensional models of childhood maltreatment with respect to the development of STBs.
Recent studies have also demonstrated the complexity in child maltreatment experiences, and the common co-occurrence of types, by using person-centered approaches. For example, among a sample of child protective services (CPS) involved children, latent classes of child maltreatment experiences (e.g., type, chronicity) predicted different child functioning outcomes. The majority of children in this study were characterized as having chronic and multi-subtype maltreatment, and subsequently had the highest risk for emotional and behavioral problems (Warmingham et al., Reference Warmingham, Handley, Rogosch, Manly and Cicchetti2019). Future research is needed to uncover how the complexity in child maltreatment experiences relates to risk for youth STBs, and to better understand the developmental pathways in these associations.
Biological, psychological, and interpersonal mediating processes
Following a developmental psychopathology approach, our model of youth STBs proposes three critical developmental processes at three levels of analysis (biological, psychological, and interpersonal). These processes include physiological dysregulation, disruptions in emotion regulation, and risky interpersonal and family processes (see Figure 1). Importantly, informed by the developmental systems perspective, these three mediating processes are not discrete, but instead transact with one another over time to influence the emergence of STBs. For example, physiological dysregulation can underlie or exacerbate psychopathology while also contributing to stressful family contexts. There is also evidence that youth psychopathology and family stress transact with and exacerbate one another (Chan et al., Reference Chan, Doan and Tompson2014). A child’s disruptive or internalizing behavior can cause conflict within the family system, which may prolong or exacerbate the internalizing or externalizing behaviors of the child. Together, these risky processes may result in the psychological pain that theoretically precedes suicidal behavior (Klonsky & May, Reference Klonsky and May2015). Below, we outline the specific developmental mechanisms we propose in the pathway from child maltreatment experiences to youth STBs.
Biological processes
Experiences of early life stress, including childhood maltreatment, are known to negatively impact the development of various bio-regulatory systems within the individual (Lovallo, Reference Lovallo2013; Obradović, Reference Obradović2012; Wismer Fries et al., Reference Wismer Fries, Shirtcliff and Pollak2008). Thus, at the biological level, we propose that child maltreatment impacts neurobiological and physiological systems of self-regulation, which in turn can transact with other proposed mechanisms (e.g., internalizing psychopathology and interpersonal problems), leading to the psychological pain that is the theoretical root cause for STBs (Klonsky & May, Reference Klonsky and May2015). Specifically, we propose that child maltreatment impacts risk for youth STBs via (a) dysregulation of psychophysiological stress response systems, and relatedly, (b) neurobiological mechanisms associated with self-regulation.
Stress response systems
There is a consensus through psychophysiological, genetic, and neuropsychological (e.g., functional magnetic resonance imaging (fMRI)) studies that childhood adversity such as child maltreatment can impact multiple biological systems involved in the stress response. This includes the two primary stress response systems, the autonomic nervous system and the hypothalamic-pituitary-adrenal (HPA) axis (Gunnar & Quevedo, Reference Gunnar and Quevedo2007). The autonomic system consists of the sympathetic nervous system, which responds to external demands with immediate fight or flight reactions, and the parasympathetic nervous system, which works to regulate the individual and maintain homeostasis (Gunnar & Quevedo, Reference Gunnar and Quevedo2007). The autonomic nervous system transacts with the HPA axis, which mediates the individual response to stressors by facilitating the secretion and action of glucocorticoids (i.e., cortisol) throughout the body (Tarullo & Gunnar, Reference Tarullo and Gunnar2006). Glucocorticoids have a variety of actions in the body, including suppressing the immune and inflammatory response (Irwin & Cole, Reference Irwin and Cole2011), regulating energy via glucose metabolism, and inhibiting the short-term fight or flight response (Gunnar & Quevedo, Reference Gunnar and Quevedo2007).
According to the adaptive calibration model, an evolutionary-developmental theory, early life experiences shape the development of stress response systems (del Giudice et al., Reference del Giudice, Ellis and Shirtcliff2011). Specifically, inputs from the physical environment modify physiological systems, including the autonomic nervous system and HPA axis, to facilitate adaptation to the current environment (Frankenhuis et al., Reference Frankenhuis, Young and Ellis2020). For example, it is possible that young children exposed to physical abuse will become hyper-responsive to stress to facilitate their survival in this type of threatening environment. However, adaptive strategies that include hyper- or hypo-stress-responsiveness can lead to maladaptation later in life when the individual is no longer in the threatening or adverse environment.
There is a robust research literature linking early life stress, and specifically child maltreatment, to physiological dysregulation in stress response systems (Obradović, Reference Obradović2012). For example, several research groups have investigated the impact of early life stress by utilizing samples of chronically deprived children from orphanages in Romania (Gunnar et al., Reference Gunnar, Morison, Chisholm and Schuder2001; Humphreys et al., Reference Humphreys, Guyon-Harris, Tibu, Wade, Nelson, Fox and Zeanah2020). Children who spent most of their childhood in these institutions were found to have heightened salivary cortisol levels (a marker of dysregulated HPA axis function), as compared to children who were not raised in institutions and children who were adopted early in life (Gunnar et al., Reference Gunnar, Morison, Chisholm and Schuder2001). In US-based samples, experiences of childhood maltreatment have also been found to impact diurnal patterns of cortisol (Bernard et al., Reference Bernard, Butzin-Dozier, Rittenhouse and Dozier2010), as well as cortisol reactivity (Harkness et al., Reference Harkness, Stewart and Wynne-Edwards2011), although this literature is mixed. There is also literature documenting the associations between child maltreatment and activity in the autonomic nervous system (Huffman et al., Reference Huffman, Oshri and Caughy2020). For example, adolescents who reported experiences of childhood maltreatment were more likely to have a heightened sympathetic nervous system response to a common psychosocial stress task, as compared to non-maltreated adolescents (McLaughlin et al., Reference McLaughlin, Sheridan, Alves and Mendes2014). Early life adversities such as child maltreatment confer risk for methylation and other epigenetic changes in genes relating to HPA function (Cicchetti et al., Reference Cicchetti, Hetzel, Rogosch, Handley and Toth2016), suggesting that epigenetic modifications in genes relating to the stress response may serve as an underlying mechanism between child maltreatment and suicide. However, most epigenetic studies have used clinical adult samples, and thus additional research is needed on how child maltreatment influences youth STBs via epigenetic mechanisms, and how this relates to stress response reactivity.
Dysregulation in physiological stress response systems may serve as a critical and developmentally salient risk factor for suicide among adolescents (Miller & Prinstein, Reference Miller and Prinstein2019). Moreover, an abnormal response to stress in the HPA axis has been posited as a risk factor for suicidal behavior in part due to associated behaviors such as impaired decision making and aggression (Steinberg & Mann, Reference Steinberg and Mann2020). There is some empirical evidence to support these suggestions. For example, heightened reactivity in the HPA axis in response to a laboratory-administered psychosocial stress task was related to suicidal ideation three months later in a sample of adolescent girls at risk for suicidal behaviors (Giletta et al., Reference Giletta, Calhoun, Hastings, Rudolph, Nock and Prinstein2015). Alterations in the autonomic nervous system have also been observed in relation to STBs. Women with a history of suicide attempts had lower basal high-frequency heart rate variability, a measure of parasympathetic nervous system capacity, as compared to women without a history of suicide attempt (Wilson et al., Reference Wilson, Chesin, Fertuck, Keilp, Brodsky, Mann, Ceren, Benjamin-phillips and Stanley2016). This finding indicates that a lesser capacity of the parasympathetic nervous system, or a dampened ability to regulate oneself, may be linked with suicide-related behaviors.
It is important to note that early life stress such as child maltreatment can produce both dampened responsiveness (hypo-responsivity; Liu et al., Reference Liu, Cui, Duprey, Kogan and Oshri2020; Lovallo, Reference Lovallo2013) as well as heightened responsiveness (hyper-responsivity; e.g., Harkness et al., Reference Harkness, Stewart and Wynne-Edwards2011) in stress response systems. It is possible that the type and timing of stressor experienced, genetic and temperamental differences, and the developmental stage of the child impacts whether youth exhibit hypo- or hyper-reactivity to stress (Bosch et al., Reference Bosch, Riese, Reijneveld, Bakker, Verhulst, Ormel and Oldehinkel2012; Cicchetti et al., Reference Cicchetti, Rogosch, Gunnar and Toth2010; Obradović, Reference Obradović2012). Indeed, the stress response system exhibits marked plasticity and adapts dynamically to changing environmental circumstances such as stressful rearing contexts. For example, there is some evidence that the stress response system is initially hyper-active after a child experiences toxic stressors such as child maltreatment, and then eventually becomes suppressed due to habituation of the stress response (Trickett et al., Reference Trickett, Noll, Susman, Shenk and Putnam2010). Additionally, some research suggests that child psychopathology might moderate the association between child maltreatment and cortisol regulation (Cicchetti et al., Reference Cicchetti, Rogosch, Gunnar and Toth2010). However, more research is needed to investigate the complex relationships between early life stress experiences and dysregulation of physiological stress response systems. Thus, our proposed model suggests that dysregulation in stress response systems, including both dampened and heightened responsiveness, can serve as a mechanism between child maltreatment and youth STBs.
Neurobiological pathways relating to self-regulation
We also propose that neurobiological changes to brain pathways relating to self-regulation may underlie the association between child maltreatment experiences and youth STBs. Although we discuss these mechanisms here separately, these neurobiological mechanisms are related to the aforementioned psychophysiological stress response mechanisms. Below we discuss several findings relevant to a neurobiological pathway related to self-regulation; however, an exhaustive review of the brain mechanisms related to child maltreatment and youth suicide are outside the scope of the present article.
Experiences of early life stress, including child maltreatment, may impede normative and healthy brain development (Berens et al., Reference Berens, Jensen and Nelson2017; Twardosz & Lutzker, Reference Twardosz and Lutzker2010). The developing brain shows marked plasticity throughout childhood and adolescence, and consequently, traumatic environmental experiences such as maltreatment can influence both the structure and function of certain brain areas and networks (Twardosz & Lutzker, Reference Twardosz and Lutzker2010). Child maltreatment is known to impact brain areas that are implicated in heightened emotional reactivity and increased salience of threatening stimuli, both of which are common for individuals exposed to childhood trauma, and which have been suggested as behavioral mechanisms linking child maltreatment to future psychopathology (McLaughlin & Lambert, Reference McLaughlin and Lambert2017). Indeed, structural and functional differences have been found among maltreated children and adults in areas relating to emotion processing and emotion regulation (e.g., limbic and frontal brain regions; Hallowell et al., Reference Hallowell, Oshri, Liebel, Liu, Duda, Clark and Sweet2019; Oshri et al., Reference Oshri, Gray, Owens, Liu, Duprey, Sweet and MacKillop2019). For example, children and adults who have prior experiences of child maltreatment are more likely to exhibit increased activation in the amygdala in response to an fMRI task with emotional stimuli (Hein & Monk, Reference Hein and Monk2017; Tottenham et al., Reference Tottenham, Hare, Millner, Gilhooly, Zevin and Casey2011). Functional changes in relevant frontal cortex areas may also underlie emotion regulation difficulties among maltreated children and adolescents (McLaughlin et al., Reference McLaughlin, Peverill, Gold, Alves and Sheridan2015; Pechtel & Pizzagalli, Reference Pechtel and Pizzagalli2011).
Neurobiological deficits in emotion regulation and reactivity have also been implicated in suicidal ideation and behaviors (Li et al., Reference Li, Chen, Gong and Jia2020; Pan et al., Reference Pan, Hassel, Segreti, Nau, Brent and Phillips2013). For instance, a meta-analysis comparing findings from task-based fMRI studies found that adult patients with major depressive disorder and history of a suicide attempt, compared to major depressive disorder patients without a history of attempt, showed functional changes in brain areas relevant to emotion regulation and processing, including the insula and fusiform gyrus (Li et al., Reference Li, Chen, Gong and Jia2020). In another study, adolescents with a history of suicide attempts evinced significantly different activation patterns of several brain areas in response to an emotion-processing paradigm, in comparison to a group of adolescents with depression but no history of suicide attempts and to a healthy control group (Pan et al., Reference Pan, Hassel, Segreti, Nau, Brent and Phillips2013). Specifically, adolescent suicide attempters presented a heightened response to angry faces in sensory cortical areas and areas associated with attention processing. Thus, although no studies to our knowledge have used formal mediation analysis to examine brain pathways as mechanisms between child maltreatment and youth STBs, it is evident that neurobiological pathways implicated in emotion regulation can influence the risk for STBs among youth with exposure to child maltreatment. Specifically, these neurobiological findings may reflect an individuals’ inability to adaptively cope with stressful or emotional experiences, which in turn can lead to excessive or prolonged negative mood states (i.e., psychological pain) and subsequent suicidal ideation (Van Heeringen & Mann, Reference Van Heeringen and Mann2014).
Psychological processes
The second proposed mechanism linking early life stress with adolescent suicide-related behaviors is through psychological processes, including emotion regulation, self-representation, and internalizing and externalizing symptomology. In accordance with the organizational perspective on development, a key tenet of the developmental psychopathology perspective, adverse rearing environments can disrupt stage-salient tasks relating to children’s socioemotional development, such as self-concept development and emotion regulation (Cicchetti & Banny, Reference Cicchetti, Banny, Lewis and Rudolph2014). For example, opinions and actions of caregivers toward the child contribute to the child’s own perceived worth (Harter, Reference Harter and Cicchetti2016). Consequently, a child in an insecure or abusive rearing environment may grow to make negative attributions about oneself which are associated with concurrent or subsequent internalizing symptoms such as anxiety and depression (Harter, Reference Harter and Cicchetti2016). Further, child maltreatment can disrupt the attainment of self-regulation abilities, including emotion regulation and self-system processes, cascading into externalizing behaviors such as disruptiveness and impulsiveness (Kim & Cicchetti, Reference Kim and Cicchetti2009). These disruptions in stage-salient developmental tasks prompted by maltreatment can subsequently lead to increased risk for STBs during adolescence and emerging adulthood.
Emotion regulation
Children and adolescents who have been exposed to child maltreatment are more likely than non-abused peers to have problems with emotion regulation, including having less access to emotion regulation strategies and greater emotion reactivity (Kim-Spoon et al., Reference Kim-Spoon, Cicchetti and Rogosch2013). For instance, children aged 6–12 who were exposed to child maltreatment, measured prospectively, were more likely to exhibit emotion regulation problems such as low emotional awareness and inappropriate emotional displays (Kim & Cicchetti, Reference Kim and Cicchetti2009). In a recent meta-analysis, child maltreatment was significantly associated with emotion dysregulation (Lavi et al., Reference Lavi, Katz, Ozer and Gross2019). The biological underpinnings of emotion regulation, including the neurological processes involved in emotion processing and the physiological processes relating to the acute stress response, have also been associated with child maltreatment (Koss & Gunnar, Reference Koss and Gunnar2018; Twardosz & Lutzker, Reference Twardosz and Lutzker2010).
Adolescents and young adults who have problems regulating and coping with difficult emotions may think about suicide and act upon self-injurious thoughts to escape from their psychological pain. Indeed, in a sample of adolescent inpatients, youth who had impulse control difficulties and who lacked sufficient access to emotion regulation strategies were more likely to have past-year suicidal ideation, even when controlling for mood, anxiety, and behavioral disorders (Hatkevich et al., Reference Hatkevich, Penner and Sharp2019). In another study using a sample of high school students in rural, low-income communities, teens who reported having limited access to emotion regulation strategies were more likely to also report a suicide attempt (Pisani et al., Reference Pisani, Wyman, Petrova, Schmeelk-Cone, Goldston, Xia and Gould2013). Relatedly, a recent cross-sectional study found evidence for emotion dysregulation as a mediator between child maltreatment and adolescent self-harm (Peh et al., Reference Peh, Shahwan, Fauziana, Mahesh, Sambasivam, Zhang, Ong, Chong and Subramaniam2017). Thus, sufficient evidence exists to encourage further investigations of emotion regulation (including emotion regulation strategies and emotion reactivity) as a mediator between child maltreatment and youth STBs.
Self-representation
The availability of sensitive and stable caregivers is crucial to the normative development of self-representation throughout childhood (Harter, Reference Harter, Damon and Lerner2006). Theoretically, having a secure attachment relationship gives children a solid foundation for healthy development, including the development of a positive self-concept. Experiences of abuse may trigger youth to incorporate negative feedback from caregivers (e.g., connotations of being “bad”) into their own self-concept. Studies show that youth who have been abused or neglected by their caregivers have lower self-esteem compared to their non-maltreated peers (Kim & Cicchetti, Reference Kim and Cicchetti2006; Shen, Reference Shen2009). In a story-telling task, the narratives of maltreated preschoolers were more likely to contain negative self-representations compared to the narratives of their non-maltreated counterparts (Toth et al., Reference Toth, Cicchetti, MacFie, Maughan and Vanmeenen2000).
Several studies provide support for the role of self-representation in the developmental pathway from child maltreatment to youth STBs. In a sample of adolescents living in rural China, those who had experienced neglect and emotional abuse were more likely to report suicidal ideation, and this was mediated by a lack of self-compassion (Zhang et al., Reference Zhang, Liu and Long2020). There is also evidence for the role of self-representation, including self-esteem and self-criticism, in the association between child maltreatment and suicidal behaviors (Cero & Sifers, Reference Cero and Sifers2013; Falgares et al., Reference Falgares, Marchetti, Manna, Musso, Oasi, Kopala-Sibley, de Santis and Verrocchio2018). For instance, in a sample of undergraduate students in Italy, self-criticism partially mediated the association between retrospectively reported experiences of child maltreatment and an index measuring the propensity for suicide (Falgares et al., Reference Falgares, Marchetti, Manna, Musso, Oasi, Kopala-Sibley, de Santis and Verrocchio2018). It is possible that these self-processes are underlying behavioral symptomology, including internalizing and externalizing symptoms, in the psychological developmental pathways from child maltreatment to youth STBs.
Internalizing and externalizing psychopathology
There is much empirical research that has linked child maltreatment with mental illness and symptoms of psychopathology during adolescence. Abuse or neglect during childhood predicts heightened internalizing symptoms in longitudinal studies (Bolger & Patterson, Reference Bolger and Patterson2001; Duprey et al., Reference Duprey, Oshri and Caughy2017; Lewis et al., Reference Lewis, Kotch, Wiley, Litrownik, English, Thompson, Zolotor, Block and Dubowitz2011). For example, findings from the longitudinal Isle of Wight study indicated that youth who were maltreated were 15.5 times more likely to experience minor depression and 8.11 times more likely to experience an anxiety disorder, compared to non-abused youth (Collishaw et al., Reference Collishaw, Pickles, Messer, Rutter, Shearer and Maughan2007). Internalizing symptomology, in turn, is a strong predictor of suicide-related behaviors during adolescence and emerging adulthood (Bridge et al., Reference Bridge, Goldstein and Brent2006).
It is also likely that, for some youth, externalizing psychopathology (e.g., disruptiveness and impulsivity) plays a role in the connection between child maltreatment and youth STBs. Child maltreatment is a robust predictor of externalizing disorders throughout childhood, adolescence, and young adulthood (Oshri et al., Reference Oshri, Rogosch, Burnette and Cicchetti2011; Thompson et al., Reference Thompson, English and White2016). In turn, recent studies have shown that externalizing disorders are a direct risk factor for suicide-related behaviors. For example, in a clinical sample of psychiatrically hospitalized adolescents, 67.9% of those who had attempted suicide multiple times were diagnosed with an externalizing disorder (e.g., disruptive behavior disorders, substance use disorders; D’Eramo et al., Reference D’Eramo, Prinstein, Freeman, Grapentine and Spirito2004). In fact, scholars have recently posited that impulsivity may serve as a primary mechanism linking childhood maltreatment with suicide (Braquehais et al., Reference Braquehais, Oquendo, Baca-García and Sher2010).
Most investigations on mechanisms between child maltreatment and youth STBs have focused on individual symptomology, including internalizing and externalizing-related symptoms. Not surprisingly, internalizing problems (including depression and depressive symptoms) were found as a mediator between child maltreatment and suicidal ideation in numerous studies (Cromer et al., Reference Cromer, Villodas and Chou2019; Handley, Adams, et al., Reference Handley, Adams, Manly, Cicchetti and Toth2019; Sekowski et al., Reference Sekowski, Gambin, Cudo, Wozniak-Prus, Penner, Fonagy and Sharp2020; Wan & Leung, Reference Wan and Leung2010). There is also evidence for other related mediators, including psychache (i.e., psychological pain; Li et al., Reference Li, You, Ren, Zhou, Sun, Liu and Leung2019), negative emotionality (Cho & Glassner, Reference Cho and Glassner2020), and recent psychological distress (Thompson et al., Reference Thompson, Proctor, English, Dubowitz, Narasimhan and Everson2012). Similar mediating mechanisms have been found in the association between child maltreatment and suicide attempts. For instance, depressed mood was found as a mediator between both sexual abuse and family conflict and adolescent suicide attempts (Sigfusdottir et al., Reference Sigfusdottir, Asgeirsdottir, Gudjonsson and Sigurdsson2013). There are considerably fewer studies investigating externalizing behaviors in the pathway from child maltreatment to youth STBs, but some evidence exists. For instance, externalizing problems mediated the association between childhood physical abuse and youth suicidal ideation in a large sample of Chinese high school students (Wan & Leung, Reference Wan and Leung2010).
Taken together, there is strong evidence that various forms and symptoms of psychopathology play a role in the developmental pathway between child maltreatment and adolescent STBs. It is possible that more generalized forms of psychopathology, as opposed to specific diagnoses, are mechanisms in this link. Recent models suggest that a higher-order, p factor, of general psychopathology underlies traditional psychiatric diagnoses such as in the DSM and includes diagnoses on both the internalizing and externalizing spectrum (Caspi et al., Reference Caspi, Houts, Belsky, Goldman-Mellor, Harrington, Israel, Meier, Ramrakha, Shalev, Poulton and Moffitt2014). This model on the structure of psychopathology can also explain the high rates of comorbidity that exist between internalizing and externalizing disorders (Caspi et al., Reference Caspi, Houts, Belsky, Goldman-Mellor, Harrington, Israel, Meier, Ramrakha, Shalev, Poulton and Moffitt2014). To our knowledge, just one study has specifically investigated comorbidity between externalizing and internalizing symptomology as a mechanism between childhood maltreatment and adolescent STBs (Duprey et al., Reference Duprey, Oshri and Liu2019b). Theoretically, the combination of internally focused symptoms like depression and anxiety with externally focused symptoms like substance use, impulsivity, and deviance might exacerbate vulnerability for risk behaviors such as suicidal thoughts and behaviors during adolescence. Thus, given the high rates of comorbidity between symptoms and disorders on the internalizing and externalizing psychopathology spectrums, and newer models on the structure of psychopathology, future research should investigate psychopathology comorbidity as a mediator in the link between child maltreatment and youth STBs.
Interpersonal and family processes
The third broad transactional mechanism that we propose is risky family and interpersonal processes (Repetti et al., Reference Repetti, Taylor and Seeman2002), and more specifically, attachment processes, family conflict, and peer problems. As with other aspects of our model, these proposed mechanisms are informed by prior literature and developmental psychopathology theory. Additionally, the interpersonal theory of suicide (Van Orden et al., Reference Van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner2010) guides the proposed interpersonal mechanisms linking child maltreatment to youth STBs. The interpersonal theory of suicide posits that interpersonal risk factors (particularly, thwarted belongingness and perceived burdensomeness) lead to the emergence of STBs (Van Orden et al., Reference Van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner2010). Thwarted belongingness and perceived burdensomeness may result from youth’s interpersonal interactions with their families and peers. In the family context, youth who grow up in abusive households may develop feelings of both thwarted belongingness and perceived burdensomeness due to a lack of connectedness to their family unit, and/or a self-hatred that might stem from emotional abuse or other forms of maltreatment. Indeed, experiences of childhood emotional abuse predicted both thwarted belongingness and perceive burdensomeness (Smith et al., Reference Smith, Monteith, Rozek and Meuret2018), and perceived burdensomeness was found to mediate the association between childhood experiences of emotional abuse and young adult suicidal ideation (Puzia et al., Reference Puzia, Kraines, Liu and Kleiman2014).
Attachment
In accordance with a developmental psychopathology framework, children who are maltreated may develop insecure attachment relationships with their caregivers (Stronach et al., Reference Stronach, Toth, Rogosch, Oshri, Manly and Cicchetti2011), and these poor attachment relationships can cascade into future adverse outcomes, including psychopathology (Hankin, Reference Hankin2005). As noted prior, theories of attachment and developmental psychopathology suggest that a secure attachment relationship with one’s caregiver is a foundation on which subsequent healthy development can build upon (Sroufe et al., Reference Sroufe, Carlson, Levy and Egeland1999). Insecure attachment may initiate a cascade of developmental maladaptation, and together these early experiences and developmental perturbations may probabilistically result in future psychopathology including suicide risk. Accordingly, attachment processes are deeply interconnected with the other developmental mechanisms named in our model such as emotion regulation, self-representation, and behavioral problems. For instance, a maltreated child with an insecure attachment relationship with their caregiver may develop negative self-representations and poor self-esteem, which paired with a consistent negative home environment, can trigger depressive symptomology and suicide risk during adolescence.
Family conflict
Youth who lack secure attachment to a primary caregiver may also later develop relationships with that caregiver characterized by conflict and insecurity (Aikins et al., Reference Aikins, Howes and Hamilton2009). Family conflict is a major source of stress and psychological pain for adolescents and may precede suicidal thoughts and behaviors (Pelkonen et al., Reference Pelkonen, Karlsson and Marttunen2011). Thus, we propose that conflict with family members is a key mechanism linking child maltreatment to future STBs. Theoretically, conflict with family members can predispose youth to feeling burdensome and lacking belonging to a central family unit, and this burdensomeness and thwarted belonging may cause STBs to emerge. Indeed, there is empirical support for the role of family conflict as a mediator between child maltreatment and youth suicidal ideation. Within a sample of depressed low-socioeconomic status adolescent girls, Handley, Adams, et al. (Reference Handley, Adams, Manly, Cicchetti and Toth2019) tested three competing mediators (i.e., mother-adolescent conflict, mother-adolescent relationship quality, and depressive symptoms) and found evidence for mother-daughter relationship quality and depressive symptoms as mediators in the association between child maltreatment and suicidal ideation. Similarly, poor family relationships (operationalized as lower levels of cohesion and expressiveness, and higher levels of conflict) mediated the association between physical abuse and suicidal ideation in a large sample of Chinese high school students (Wan & Leung, Reference Wan and Leung2010).
Peer problems
Child maltreatment experiences increase the risk for bullying victimization and peer rejection in childhood and adolescence (Hong et al., Reference Hong, Espelage, Grogan-Kaylor and Allen-Meares2012). Similar to family conflict, youth who experience peer victimization or rejection may lack feelings of belonging, which can predispose them to engage in suicidal thinking. Indeed, there is a large body of evidence showing that adolescents who are bullied by their peers (in person or via cyberbullying) are more likely to engage in suicidal thinking and suicide attempts (Hinduja & Patchin, Reference Hinduja and Patchin2010). A recent meta-analysis found that bullying victimization and perpetration were both significantly associated with a greater odds of suicidal ideation and behaviors, with odds ratios ranging from 2.12 to 4.02 (Holt et al., Reference Holt, Vivolo-Kantor, Polanin, Holland, DeGue, Matjasko, Wolfe and Reid2015). Certain groups of youth, particularly those who identify as lesbian, gay, bisexual, transgender, and questioning (LGBTQ), are subject to increased levels of bullying and discrimination from peers that can put them at an increased risk of suicide (Ybarra et al., Reference Ybarra, Mitchell, Kosciw and Korchmaros2015).
Taken together, there is convincing theoretical and empirical support that interpersonal processes play a unique role in the developmental pathway from child maltreatment experiences to the emergence of STBs in adolescence and young adulthood. However, more research is needed to replicate prior findings and investigate specific interpersonal processes in the pathway from child maltreatment to youth STBs. For example, disruption in attachment processes is a candidate mechanism that is associated with child maltreatment and poor mental health outcomes (Hankin, Reference Hankin2005; Stronach et al., Reference Stronach, Toth, Rogosch, Oshri, Manly and Cicchetti2011), but has not been investigated specifically in relation to youth STBs. Additionally, most studies investigating interpersonal processes in the association between child maltreatment and youth STBs examined suicidal ideation as an outcome variable. It will be important for future research to examine the role of interpersonal processes, both within and outside of the family, as precursors to youth suicidal behaviors and suicide.
Developmentally salient risk and protective factors
In our model, we specify the role of developmentally salient risk and protective factors that can buffer youth from the harm posed by exposure to child maltreatment. According to the developmental psychopathology approach and the concept of multifinality, the emergence of youth STBs is one of many possible outcomes stemming from exposure to child maltreatment. Importantly, many youth who experience child maltreatment along with its various adverse outcomes (e.g., internalizing psychopathology or family-child conflict) do not end up exhibiting suicidal thoughts and behaviors in adolescence nor later in life. Protective factors are moderators that can buffer, or lessen, the impact of child maltreatment exposure on the likelihood of developing suicidal thinking or behaviors (Rutter, Reference Rutter1985), while moderating risk factors can exacerbate the impact of child maltreatment on youth STBs.
In line with a developmental perspective on youth STBs, it is important to consider that both protective and risk (i.e., exacerbating) factors can affect suicidal ideation and behaviors differently depending on the time in a child’s development. In Figure 1, we give examples of empirically supported risk and protective factors for maltreated children and adolescents at different stages of development (i.e., early childhood, school age, and adolescence). For example, school belonging and participation in youth activities were found to be protective in the association between physical abuse and suicidal ideation and attempts among adolescents (Cero & Sifers, Reference Cero and Sifers2013; Zhang et al., Reference Zhang, Liu and Long2020). These protective factors are salient to the developmental stage of adolescence, which is characterized by rapid social development and the growing importance of peer groups.
Our conceptual model also posits that there are developmentally salient moderating risk factors that can exacerbate the pathway from child maltreatment to youth STBs. Adolescence marks an extended transition between childhood and young adulthood, and includes biological shifts such as puberty, as well as personality and social shifts including identity development and the increased salience of peers. During this time, certain developmental transitions and risk factors (both direct and moderating) may exacerbate the pathway towards suicidal ideation, and between suicidal ideation and suicidal behaviors. Therefore, in this model, the transactions between vulnerability factors that may have been continuous throughout childhood (i.e., physiological dysregulation, psychopathology, and interpersonal problems), coupled with the challenges of adolescence, can result in the emergence of STBs. For example, stressful life events exacerbated the association between child maltreatment and suicidal ideation in a sample of adolescent girls (Duprey et al., Reference Duprey, Handley, Manly, Cicchetti and Toth2021). Other possible developmentally salient risk factors to consider by future research include, but are not limited to, pubertal development, risky sexual behaviors, and peer victimization.
Progression from suicidal ideation to suicidal behaviors
Our conceptual model is informed by ideation to action theories of suicide, such as the interpersonal theory of suicide (Van Orden et al., Reference Van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner2010) and the three-step theory (Klonsky & May, Reference Klonsky and May2015), which posit that different risk factors and processes characterize the development of suicidal thoughts versus those that characterize the progression from suicidal thoughts towards suicidal behaviors. We integrate these theories of suicidology (which are based on adult models) with a developmental psychopathology lens to apply them to the emergence of STBs in adolescence and emerging adulthood. According to these frameworks, the progression from suicidal ideation to suicide behaviors (i.e., attempts) is driven by capability (defined as an individual’s capacity to engage in self-harming behaviors). For most people, including those who may have suicidal ideation, there is a biologically and evolutionary-driven fear of engaging in suicidal behaviors. However, for some individuals with increased capability, this fear is reduced, and they are subsequently more likely to engage in suicidal behaviors. Consequently, our model suggests that there are capability-building risk factors that contribute to the progression from suicidal ideation towards suicidal behaviors, which stem from experiences of child maltreatment.
In the interpersonal theory of suicide, capability includes two components, both of which are not innate but acquired or learned throughout the lifetime: reduced fear of death, and an increase in pain tolerance (Van Orden et al., Reference Van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner2010). In contrast, the three-step theory posits that capability can also be trait-like, or dispositional, in addition to acquired. This theory also considers the role of practical sources of capability, such as access to lethal means (Klonsky & May, Reference Klonsky and May2015). In our model of child maltreatment and youth STBs, we focus specifically on the role of acquired capability. The developmental consequences of child maltreatment are multifaceted, and include several outcomes related to an increased capability for suicide. These outcomes include but are not limited to dysregulated responses to stress, substance use behaviors, and engagement in NSSI. Below, we detail how these three specific risk factors might contribute to the ideation-to-action pathway. Note that these risk factors might work by exacerbating the association between suicidal ideation and behaviors (i.e., acting as a statistical moderator), or by contributing directly to the likelihood of suicidal behaviors (i.e., having a direct statistical association with suicide attempts).
As detailed above, child maltreatment and other adverse, chronic stressful experiences in childhood can predict future dysregulation in physiological stress response systems (Gunnar et al., Reference Gunnar, Morison, Chisholm and Schuder2001; Lovallo, Reference Lovallo2013). Specifically, a blunted physiological response to acute stressors is characteristic for youth and adults who have undergone traumatic childhood experiences like child maltreatment (Lovallo, Reference Lovallo2013). There is some empirical evidence for the role of blunted stress reactivity in the capacity for suicidal and self-harming behaviors. For example, a recent study with adolescent girls found that psychosocial stressors predicted suicidal ideation, while the combination of psychosocial stressors with blunted HPA function predicted suicidal behaviors (Eisenlohr-Moul et al., Reference Eisenlohr-Moul, Miller, Giletta, Hastings, Rudolph, Nock and Prinstein2018). Additionally, in the same study, adolescents with a history of suicidal behavior had a significantly more blunted cortisol response to a psychosocial stressor compared to those with only suicidal ideation and to controls with no lifetime suicidal ideation or behaviors. A separate study also found that adolescent girls with a history of self-harm had a blunted HPA reaction to a laboratory social stress task compared to girls with no history of self-harm (Plener et al., Reference Plener, Zohsel, Hohm, Buchmann, Banaschewski, Zimmermann and Laucht2017).
Similarly, youth who suffer from child abuse and neglect are more likely to engage in substance use behaviors, including alcohol, marijuana, and other drug use (Cicchetti & Handley, Reference Cicchetti and Handley2019). Substance use is a major proximal risk factor for engagement in suicidal behaviors among youth (Esposito-Smythers & Spirito, Reference Esposito-Smythers and Spirito2004). For instance, in a case-control study, substance use disorders were significant risk factors for adolescent suicide attempts (Kelly et al., Reference Kelly, Cornelius and Lynch2002). Substance use was also associated with suicide attempts, after controlling for sociodemographic factors and psychiatric disorders including suicidal ideation, in a cross-sectional study using a community sample of adolescents (Wu et al., Reference Wu, Hoven, Liu, Cohen, Fuller and Shaffer2004). Additionally, a recent study found that cannabis and other illicit drug use predicted the transition from suicidal ideation to attempts in a high-risk sample of adolescents (Mars et al., Reference Mars, Heron, Klonsky, Moran, O’Connor, Tilling, Wilkinson and Gunnell2019).
The frequency and severity of substance use behaviors increase dramatically during adolescence and emerging adulthood, and risky substance use is even more common for youth with histories of child maltreatment (Cicchetti & Handley, Reference Cicchetti and Handley2019). While under the influence of substances that cause disinhibition, such as alcohol or opiates, youth have reduced impulse control and may also have reduced fear of risk behaviors and self-injury (Dawes et al., Reference Dawes, Mathias, Richard, Hill-Kapturczak and Dougherty2008). Indeed, in a community sample of adolescents, alcohol abuse and dependence, drug use, and cigarette use were all significant predictors for suicide attempts even after controlling for depressive symptoms and suicidal ideation (Wu et al., Reference Wu, Hoven, Liu, Cohen, Fuller and Shaffer2004). Thus, we recommend that future research investigate alcohol and drug use as predictors of suicidal behaviors in samples of youth with histories of maltreatment.
A third possible capacity-enhancing factor stemming from experiences of child maltreatment is NSSI. A recent meta-analysis showed that child maltreatment significantly predicted engagement in NSSI, with an average effect size of OR = 3.42 (Liu et al., Reference Liu, Scopelliti, Pittman and Zamora2018). Through the process of habituation (Van Orden et al., Reference Van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner2010), youth who frequently engage in NSSI may have an increased tolerance for pain, thus enhancing their capacity for engaging in suicidal behavior. Indeed, evidence shows that a lifetime history of NSSI predicts future suicide attempts in adolescent clinical (Horwitz et al., Reference Horwitz, Czyz and King2015) and non-clinical samples (Scott et al., Reference Scott, Pilkonis, Hipwell, Keenan and Stepp2015). It is also possible that engagement in NSSI reduces youths’ fear of death, thereby increasing the risk for suicidal behaviors. Several researchers have tested this hypothesis, with mixed findings that both support (George et al., Reference George, Page, Hooke and Stritzke2016) and refute (Harris & Ribeiro, Reference Harris and Ribeiro2021) the role of reduced fear of death in the association between NSSI and suicidal behaviors. Further research is needed that explores the role of NSSI in perpetuating suicidal behavior, specifically in samples of maltreated youth.
Contextual and cultural considerations
One of the hallmarks of the developmental psychopathology framework is the incorporation of multiple levels of analysis, ranging from biological influences outwards towards macro-system and cultural influences. Accordingly, our model considers the role of youths’ context, and particularly the role of the institutions and cultures in which they belong, in the etiological processes linking child maltreatment and STBs. Child maltreatment and suicide are both phenomena that are heavily influenced by the institutions and contextual systems that individuals are a part of. It is particularly important to account for the inequities perpetuated by these institutions and systems when investigating associations between child maltreatment and youth suicide. Racism, poverty, and other sources of disparities must be considered as part of our model of child maltreatment and youth STBs. Below, we outline several ways that culture and context play a role in our proposed conceptual model.
First, context plays a role in the prevalence and reporting of child maltreatment. Environmental characteristics such as family poverty and neighborhood disadvantage can be considered enduring vulnerability factors that contribute to the etiology of child maltreatment (Cicchetti & Toth, Reference Cicchetti and Toth2016). Importantly, Black families in the United States are disproportionally reported to CPS, and Black children are disproportionally more likely to be removed from their homes as a result of CPS investigations (Palusci & Botash, Reference Palusci and Botash2021). More than half (53.0%) of Black children in the United States are involved in a child welfare investigation by the time they reach age 18, which is substantially higher than the prevalence of child welfare involvement in the general population of US youth (37.4%; Kim et al., Reference Kim, Wildeman, Jonson-Reid and Drake2017). Experts have often attributed disparities in CPS reporting to increased surveillance in neighborhoods with large percentages of racial-ethnic minority families, and racial bias in the reporting and investigation of child maltreatment (Palusci & Botash, Reference Palusci and Botash2021). Beyond the effects of child maltreatment, involvement with the child welfare system, including separation from caregivers, can lead to disruptions in stage-salient tasks and cascading mental health problems including suicidality.
Contextual factors relevant to the etiology of child maltreatment, such as poverty and parental psychopathology, are also implicated in the developmental mechanisms we hypothesize in the pathway between child maltreatment and youth STBs. For instance, although family poverty may increase the likelihood of child maltreatment, it is also associated with developmental mechanisms in our model such as problems with self-regulation (Cicchetti & Toth, Reference Cicchetti and Toth2016; Palacios-Barrios & Hanson, Reference Palacios-Barrios and Hanson2019). It is also particularly important to consider the role of racism in the mechanistic pathways from child maltreatment towards youth suicidal ideation and behaviors. Racism is an acute and chronic stressor that can the health and development of children and adolescents (Trent et al., Reference Trent, Dooley, Dougé, Trent, Cavanaugh, Lacroix, Fanburg, Rahmandar, Hornberger, Schneider, Yen, Chilton, Green, Dilley, Gutierrez, Duffee, Keane, Krugman, McKelvey and Wallace2019). Racism can impact children directly through the effects of interpersonal racism including bias and discrimination, and indirectly through the effects of structural racism. Structural and historical racism permeates the culture of the United States, impacting children of color in a multitude of ways including by diminishing families’ economic opportunities, interfering with the ability to secure safe and stable housing, and sustaining educational disparities (Trent et al., Reference Trent, Dooley, Dougé, Trent, Cavanaugh, Lacroix, Fanburg, Rahmandar, Hornberger, Schneider, Yen, Chilton, Green, Dilley, Gutierrez, Duffee, Keane, Krugman, McKelvey and Wallace2019).
The aforementioned contextual factors must also be considered when studying the acute (i.e., immediate) direct and exacerbating risk factors for suicide. According to the Cultural Model of Suicide (Chu et al., Reference Chu, Goldblum, Floyd and Bongar2010), culture-specific risk factors for suicide may be related to cultural norms (e.g., acceptability of self-harm in some communities) and culture-specific stressors (e.g., discrimination and acculturation stress). Relatedly, some scholars assert that youth suicide should be framed as a sociopolitical issue, and that power and oppression play an integral role in rates of youth suicide in the United States (White & Kral, Reference White and Kral2014). For instance, negative attitudes towards the LGBTQ community and the heteronormative sociopolitical context in the United States can lead to emotional distress, bullying, and other immediate risk factors for suicide among LGBTQ youth (Aranmolate et al., Reference Aranmolate, Bogan, Hoard and Mawson2017). Furthermore, there are racial disparities in recent suicide trends among youth in the United States. Specifically, rates of suicide among Black children and adolescents are increasing, and among all children, young Black boys are the demographic group most likely to die by suicide (Bridge et al., Reference Bridge, Asti, Horowitz, Greenhouse, Fontanella, Sheftall, Kelleher and Campo2015; Emergency Taskforce on Black Youth Suicide and Mental Health, 2019; Shain, Reference Shain2019). There are also disparities in rates of STBs by geography, with rural youth more likely to die by suicide (Fontanella et al., Reference Fontanella, Hiance-Steelesmith, Phillips, Bridge, Lester, Sweeney and Campo2015). Youth who live in rural or otherwise under-resourced communities that lack access to healthcare, or who do not have access to behavioral healthcare due to their socioeconomic status, may be particularly at risk (Campo, Reference Campo2009; Graves et al., Reference Graves, Abshire, Mackelprang, Amiri and Beck2020).
Culture not only plays a role in the risk factors for youth STBs, but also when considering protective factors that can prevent suicide and promote positive mental health outcomes. Parallel to the culture-specific risk factors listed prior, culture-specific protective factors may also be related to cultural norms, such as the unacceptability of suicide. For instance, religiosity (e.g., belonging to a church community and attending religious events) is a protective factor that reduces the risk for suicidal thoughts and behaviors among Black teens (Fitzpatrick et al., Reference Fitzpatrick, Piko and Miller2008). Another relevant culture-specific protective factor for teens is familism, a cultural value for many Latino individuals and communities which places value on interconnectedness and commitment to one’s family. Research shows that Latina teens with higher levels of familism were less likely to attempt suicide compared to teens who reported lower levels of familism (Peña et al., Reference Peña, Kuhlberg, Zayas, Baumann, Gulbas, Hausmann-Stabile and Nolle2011). Thus, future research on the developmental processes leading to STBs among youth exposed to child maltreatment should consider both contextual and culture-specific risk and protective factors.
Discussion
In sum, we propose that child maltreatment may lead to suicidal thoughts in adolescence via several mechanisms at the biological, psychological, and interpersonal levels. It is not the individual action of a single mechanism, but the transactional and joint nature of these mechanisms that can cause the psychological pain necessary for a youth to think about ending their own life. Furthermore, experiences of child maltreatment may increase the risk for several capacity-building factors (e.g., substance abuse) that can further propel the adolescent or young adult to move from thinking about suicide towards engaging in suicidal behavior. Notably, there are different risk and protective factors at every stage of development that can either exacerbate this developmental pathway and further propel the youth towards STBs, or buffer this pathway and reduce the probability of STBs.
Implications for suicide prevention: future directions for research
Our proposed model of child maltreatment and youth STBs has implications for future research in basic and applied areas. It is apparent from our review that there are several major gaps in the literature on mechanisms and moderators between childhood maltreatment and youth STBs that should be considered for future research. First, most studies looking at mechanisms and moderators in the association between child maltreatment and youth STBs have examined psychological mediators, such as depressive symptoms, self-esteem, and psychache. Very few studies have investigated biological mechanisms or moderators, despite empirical and theoretical evidence that supports these investigations (Cicchetti et al., Reference Cicchetti, Rogosch, Gunnar and Toth2010; Miller & Prinstein, Reference Miller and Prinstein2019). There is also a lack of research examining contextual processes (e.g., involvement with child welfare services and neighborhood factors) in the association between child maltreatment and youth STBs. Additionally, few studies have investigated concurrent or interacting multi-level mechanisms (i.e., interpersonal, psychological, and biological) in the link between child maltreatment and youth suicide (notable exceptions include Ammerman et al., Reference Ammerman, Serang, Jacobucci, Burke, Alloy and McCloskey2018; Salzinger et al., Reference Salzinger, Rosario, Feldman and Ng-Mak2007; Wan & Leung, Reference Wan and Leung2010). Alternatively, in line with a developmental psychopathology approach and our proposed conceptual model, we posit that there are multi-level transactional factors that mediate the link between child maltreatment and youth suicide. Thus, based on gaps in prior literature and our proposed conceptual model, future research should examine mediators of child maltreatment and youth STBs at multiple levels of analysis, and should consider how these mechanisms interact or transact with one another over time.
There is also a dearth of literature investigating mediators and moderators of child maltreatment and suicidal behaviors (specifically, suicide attempts). The majority of articles that we reviewed used suicidal ideation as an outcome instead of suicide attempts or suicide. Our model suggests that the mechanisms, risk factors (both direct and moderating), and protective factors in the developmental pathway to suicidal ideation are different from those in the pathway from ideation to suicidal behaviors. It will be important for future research to differentiate these outcomes, and to specifically investigate predictors and risk factors for suicidal behaviors in high-risk samples. We proposed three possible capacity-building factors that may play a role in the pathway from suicidal ideation towards suicidal behavior among maltreated youth: (1) stress response reactivity, (2) substance use behaviors, and (3) NSSI. These and other possible factors need to be further examined both in clinical and non-clinical samples of youth.
We also found that many studies have used cross-sectional data to investigate the link between child abuse and neglect and STBs among adolescents and emerging adults (see Table 1). Large prospective studies are needed to test the hypothesized mechanisms and risk and protective factors suggested by the present conceptual model. Thus, future research should strive to use prospective data to investigate mechanisms and moderators of the link between child maltreatment and youth suicide at multiple levels of analysis, while also considering developmentally salient risk and protective factors. Our model of child maltreatment and youth STBs provides a conceptual framework that researchers can use to inform studies in this area.
Additionally, child maltreatment is a complex and multidimensional construct. More work is needed to specifically assess the role of maltreatment type, timing, severity, and chronicity in the etiology of adolescent and young adult suicidal thoughts and behaviors. Person-centered approaches to modeling child maltreatment, such as latent class analysis, may help to better understand the complexity of child maltreatment in relation to subsequent suicide risk (e.g., Warmingham et al., Reference Warmingham, Handley, Rogosch, Manly and Cicchetti2019). Additionally, dimensional approaches to studying childhood adversity and maltreatment (McLaughlin & Sheridan, Reference McLaughlin and Sheridan2016) should be extended to investigations of youth STBs.
It will also be important for future research to address the role of culture (e.g., race, ethnicity, immigrant status, and nationality), discrimination, and systemic disparities in the development of STBs for youth with histories of child maltreatment. Thus far, there is a lack of research that has examined child maltreatment and youth suicide using underrepresented samples of youth, including Black youth and LGBTQ youth. These two subpopulations are critical: rates of suicide among Black youth, particularly males, are rising rapidly compared to rates in other demographic groups (Emergency Taskforce on Black Youth Suicide and Mental Health, 2019). Relatedly, youth who identify as LGBTQ are at an increased risk for experiencing suicidal ideation and partaking in suicidal behaviors (Ivey-Stephenson et al., Reference Ivey-Stephenson, Demissie, Crosby, Stone, Gaylor, Wilkins, Lowry and Brown2020). Relatedly, and in line with our prior recommendation of investigating contextual processes in the pathway from child maltreatment to youth STBs, social determinants of health are imperative to consider when studying youth suicide. This is particularly important given the increasing rates of STBs among youth in the last decade (Ivey-Stephenson et al., Reference Ivey-Stephenson, Demissie, Crosby, Stone, Gaylor, Wilkins, Lowry and Brown2020). It is possible that child maltreatment and other social determinants of health are related to these epidemiological shifts in rates of youth STBs. The suicide prevention community, including researchers, clinicians, and survivors, will need to focus critically on social determinants of health to understand and prevent suicide among youth with maltreatment histories.
Importantly, to advance the science on child maltreatment and youth STBs, a cohesive conceptual model is necessary. The proposed developmental model of child maltreatment and youth STBs provides a basis for asking questions and forming hypotheses about the developmental processes involved in the pathway between child abuse and neglect and youths’ suicidal ideation and attempts. Our conceptual model involves various transactions at multiple ecological levels and, due to this complexity, it likely is not possible to test all components of our model at once.
We propose several proximal next steps to test and refine our model. First, research with longitudinal designs and statistical models (e.g., cross-lagged models; latent growth models) can be used to test the role of multiple mediators at the different levels we propose in our model (biological, psychological, and interpersonal) in the pathway between childhood maltreatment and youth STBs. With sufficient power, designs such as moderated mediation will also help elucidate relations between different mechanisms and risk and protective factors in our model. Second, we propose that an important next step for refining our model is to test the role of moderating risk factors that contribute to capacity for suicide (e.g., NSSI, substance abuse) among youth exposed to child maltreatment. This research can inform interventions that respond to acute suicide risk in populations of maltreated adolescents and young adults. Third, applied research that tests suicide prevention and intervention programs can inform the mechanisms proposed in our model. Relatedly, experimental therapeutics is a research approach originally used in medicine that has recently been applied to behavioral interventions, including suicide prevention, to elucidate theoretical mechanisms of action (Insel & Gogtay, Reference Insel and Gogtay2014). Research using the experimental therapeutics approach not only can help develop and refine suicide prevention interventions for maltreated youth, but can also iteratively inform and refine the present developmental model of child maltreatment and youth STBs.
Implications for suicide prevention
Our model focuses on the short and long-term developmental antecedents of youth suicidal ideation and behavior. As such, the implications of our model for suicide prevention center around upstream prevention. Upstream prevention programs seek to modify salient risk and protective factors and mechanisms for suicide (e.g., those established by the present model such as child maltreatment, internalizing and externalizing psychopathology, emotion regulation, and interpersonal processes) before the emergence of suicidal thoughts and behaviors (Caine et al., Reference Caine, Reed, Hindman and Quinlan2018). Accordingly, these interventions have the potential to make population-level impacts on reducing youth suicidal thoughts and behaviors. Our recommendations for suicide prevention are also grounded in the Institute of Medicine continuum of care model (Gordon, Reference Gordon1987), which differentiates three types of prevention: universal (i.e., programs that target the general population), selective (i.e., programs that target a subpopulation who have a specific vulnerability factor for an eventual adverse outcome, such as youth with maltreatment histories) and indicated (i.e., programs that target a subpopulation who have elevated vulnerability and are showing some signs or symptoms, such as maltreated youth with elevated depressive symptoms).
The model presented in this paper has implications for the mechanistic targets of suicide prevention and intervention programs for youth with maltreatment histories. For instance, we consider the etiology of adolescent suicide-related behavior to consist of transactions between multiple levels of influence (i.e., physiological, behavioral, and contextual). Accordingly, efforts to intervene and interrupt processes leading to adolescent STBs may be most effective through modifications in the relations, or transactions, between multiple levels, as opposed to altering a single level of analysis (Lerner & Castellino, Reference Lerner and Castellino2002). For example, the Good Behavior Game (GBG) intervention focuses on improving young children’s behavioral self-regulation in the classroom and aims to alter the social environment to promote social integration (Kellam et al., Reference Kellam, Brown, Poduska, Ialongo, Wang, Toyinbo, Petras, Ford, Windham and Wilcox2008). An intervention that only targeted self-regulation skills or school social environment may not have had as efficient an impact in reducing risk for suicidal behaviors. In such interventions, mechanisms and outcomes of investigation should be considered at multiple levels of analysis. As an example, Cicchetti and colleagues found that an interpersonal intervention for maltreated youth and families was related to a biological outcome. Specifically, this intervention produced changes in infants’ HPA functioning (Cicchetti et al., Reference Cicchetti, Rogosch, Toth and Sturge-Apple2011). Last, it should be noted that various mechanisms presented in our model (e.g., emotion regulation) are also relevant etiological pathways for other disorders, including depression and substance use disorders. Thus, suicide prevention approaches that are implied from our model may also serve to prevent other adverse outcomes.
Interventionists and researchers must always consider developmental timing and the developmental salience of risk and protective factors when selecting intervention targets for youth. For example, while interpersonal processes are hypothesized in our model as a primary mechanism linking child maltreatment to youth STBs, and consequently would be an appropriate target for suicide prevention interventions, it is important to specify which interpersonal processes are being targeted and if these are appropriate for participants’ developmental stage. For young children who have been exposed to child abuse and neglect, attachment processes are an appropriate intervention target to prevent downstream suicide risk, and several intervention approaches (e.g., parent-child psychotherapy) have been shown to effectively improve attachment security (Toth et al., Reference Toth, Rogosch, Manly and Cicchetti2006). Below, we give specific recommendations for suicide prevention along with examples across different developmental stages of participants, settings, and target mechanisms.
Prevention of child maltreatment
First, the model presented in this paper focuses on the detrimental impact of child maltreatment on future suicidal behavior. This highlights the importance of universal prevention of childhood maltreatment. Child maltreatment places an extreme burden on children, families, communities, and our society – including an economic burden estimated to range from $428 billion to $2 trillion per year in the United States (Peterson et al., Reference Peterson, Florence and Klevens2018). Globally, violence against children has been estimated to cost up to $7 trillion (Pereznieto et al., Reference Pereznieto, Montes, Routier and Langston2014). The primary prevention of child maltreatment must be a public health priority both in the United States and globally, given these programs’ potential for numerous downstream effects, including the prevention of psychopathology and suicidal behaviors during adolescence. Several programs have shown promise for the primary prevention of maltreatment in the United States, including the Nurse-Family Partnership (Olds, Reference Olds2008) and the Building Healthy Children program (Demeusy et al., Reference Demeusy, Handley, Manly, Sturm and Toth2021). The prevention of child maltreatment can, and should be, considered a form of universal suicide prevention.
Prevention in normative social settings
Our conceptual model of child maltreatment and youth suicide also has several implications for developmentally focused upstream suicide prevention interventions for children and adolescents with histories of maltreatment. In Wyman’s developmental model of upstream suicide prevention for adolescents (2014), the author proposes that upstream prevention can have the most impact when implemented via normative and reparative social systems throughout childhood and adolescence. Normative social systems are those that reach the broadest youth populations, such as schools and families and, with increasing age, more complex and influential peer networks. Reparative social systems are settings or systems designed for youth with particular vulnerabilities, such as juvenile justice or foster care systems (Wyman, Reference Wyman2014). Strengthening the natural social systems that youth are a part of can have positive cascading effects on reducing psychopathology and promoting positive youth outcomes.
In normative social systems, there is evidence for the effectiveness of suicide prevention programs that reduce children’s and adolescent’s risk for STBs by modifying selective risk and protective factors, and the transaction among those factors. For example, the early grade school-based GBG, a classroom-based universal program that aims to reduce externalizing (i.e., aggressive and disruptive) behaviors in childhood (Kellam et al., Reference Kellam, Brown, Poduska, Ialongo, Wang, Toyinbo, Petras, Ford, Windham and Wilcox2008), has shown promise in long-term follow-up of participants. Emerging adults who had participated in the GBG intervention as children were significantly less likely to report prior suicidal ideation or behaviors, as compared to emerging adults who had been in a non-GBG comparison condition (Wilcox et al., Reference Wilcox, Kellam, Brown, Poduska, Ialongo, Wang and Anthony2008). Increased peer group social integration in later grade school partially mediated the effect of the GBG program on reduced STBs (Newcomer et al., Reference Newcomer, Roth, Kellam, Wang, Ialongo, Hart, Wagner and Wilcox2016).
School-based universal prevention programs may also have potential in reducing suicide risk by modifying interpersonal risk processes that are implicated in our model of child maltreatment and youth STBs. Peer-based interventions may be particularly salient for adolescents with maltreatment experiences, due to the increased likelihood of involvement in peer victimization and lack of peer support (Hong et al., Reference Hong, Espelage, Grogan-Kaylor and Allen-Meares2012; Pepin & Banyard, Reference Pepin and Banyard2006). For example, the school-based Sources of Strength program prepares diverse adolescent opinion leaders to disseminate healthy coping norms and practices through their natural social networks and fosters youth connections to supportive and trustworthy adults (Wyman et al., Reference Wyman, Brown, LoMurray, Schmeelk-Cone, Petrova, Yu, Walsh, Tu and Wang2010). Results from a group-randomized control trial showed that Sources of Strength increased school-wide positive norms relating to suicide, including the acceptability of seeking help from trusted adults, and trained peer leaders were four times more likely to refer suicidal peers to adults for support (Wyman et al., Reference Wyman, Brown, LoMurray, Schmeelk-Cone, Petrova, Yu, Walsh, Tu and Wang2010).
There is also evidence for various school-based indicated suicide prevention programs, which have been shown to be effective for youth with risk factors for suicide. For example, the C-CARE (Counselors CARE) and CAST (Coping and Support Training) programs are school-based interventions that have been tested and found to be efficacious with high school youth who are at an indicated risk due to their academic problems and presence of suicidal ideation (Thompson et al., Reference Thompson, Eggert, Randell and Pike2001). Findings from an efficacy study showed that youth in either the C-CARE or CAST programs exhibited reductions in suicidal ideation, hopelessness, and depression, while youth in the CAST program (an intervention supplemented with small-group skill training) also showed improvements in protective factors such as coping (Thompson et al., Reference Thompson, Eggert, Randell and Pike2001). Additional work is needed, however, to determine whether and/or how programs such as CAST, CARE, and Sources of Strength are effective in reducing STBs in populations of youth with histories of child maltreatment. Other peer-based programs, including those that incorporate peer mentoring or youth advocacy, might be impactful for improving mental health outcomes and reducing suicide risk factors (e.g., substance use) among maltreated adolescents, but this has not yet been tested.
Upstream suicide prevention programs that occur in the family context are also important for this population. We recommend family-based suicide prevention programs that target interpersonal skills and processes that have been posited as mechanisms in our conceptual model. Many of the existing family-based suicide prevention interventions are indicated programs, and consequently have primarily been developed and implemented with youth who are showing proximal signs of suicide risk such as suicidal ideation and/or deliberate self-harm. For instance, Parents CARE (P-CARE) is an adaptation of the CARE suicide prevention program that incorporates parent training in socioemotional skills (e.g., conflict reduction, supportive listening) and psychoeducation (e.g., learning suicide warning signs; Hooven et al., Reference Hooven, Walsh, Pike and Herting2012). An efficacy study found that P-CARE reduced direct risk factors for suicide, such as suicidal ideation and hopelessness, compared to an active control group (Hooven et al., Reference Hooven, Walsh, Pike and Herting2012). Another prevention program that could have potential among maltreated youth is the Resourceful Adolescent Parent Program (RAP-P), which was developed for use with youth after they present to the emergency department for suicidal behavior (Pineda & Dadds, Reference Pineda and Dadds2013). Like P-CARE, RAP-P provides psychosocial skills and psychoeducation to parents to enhance family-based protective factors and reduce family risk factors for suicidal youth. In an randomized controlled trial, youth whose families enrolled in RAP-P reported less suicide risk at follow-up compared to youth in a treatment-as-usual condition, and this was fully mediated by the effects of RAP-P on parent-reported family functioning (Pineda & Dadds, Reference Pineda and Dadds2013). Thus, there is evidence of efficacy for family-based indicated suicide prevention programs for youth. However, due to their special family context and circumstances (e.g., placement in foster care; history of abuse in the family context), we recommend that these interventions be tested and adapted specifically for youth with maltreatment histories.
Prevention in reparative social settings
There is potential for suicide prevention strategies for maltreated youth to be implemented in reparative systems, including foster care and juvenile justice settings. Among teenage girls in the juvenile justice system, Multidimensional Treatment Foster Care (a family-based preventative intervention for youth in the foster care system) reduced trajectories of depression symptoms and suicidal ideation at the two-year follow-up (Kerr et al., Reference Kerr, DeGarmo, Leve and Chamberlain2014). Thus, reparative social systems may be an ideal setting for selective suicide prevention interventions that target all youth in that setting, many with maltreatment histories.
More work is needed to integrate universal suicide prevention programs into reparative social systems that are relevant to maltreated youth. Specific future directions in this area include: (a) examining exposure to childhood maltreatment as a moderator of treatment effect in existing upstream prevention interventions; (b) collecting qualitative data on the acceptability and feasibility of existing upstream prevention interventions among children and adolescents with involvement in child welfare services; (c) calibrating new or existing prevention interventions to align with the specific suicide risk factors for maltreated youth, which may be different from risk factors in the general population of adolescents; and (d) developing and/or adapting suicide prevention programs to be implemented in reparative social system settings such as foster care and juvenile justice settings.
Screening
Finally, screening is an essential part of suicide prevention. We have several recommendations for suicide risk screening based on our model. First, given their overall increased risk of suicide, we recommend that child welfare-involved youth be screened regularly for suicide risk factors. Youth who are exposed to child maltreatment are often involved in multiple systems (e.g., healthcare, behavioral health, and child welfare; Cerulli et al., Reference Cerulli, Cicchetti, Handley, Manly, Rogosch and Toth2021). Accordingly, we recommend a multi-pronged approach to suicide risk screening that involves multiple systems including but not limited to healthcare (e.g., screening at pediatrics well-child visits), child welfare services (e.g., screening by case workers), and court-based settings where many of these children find themselves for issues related to family disruption, custody, visitation and child welfare adjudications. Second, practitioners should screen for suicide risk factors (such as substance use and/or NSSI) among child maltreatment-exposed youth who are already having suicidal thoughts. Identifying such proximal risk factors that predict the transition from suicidal ideation to attempts in samples of child maltreatment-exposed youth will be necessary to inform future screening approaches. Screening tools that may show utility in at-risk populations of youth include the widely used Ask Suicide-Screening Questions (Horowitz et al., Reference Horowitz, Bridge, Teach, Ballard, Klima, Rosenstein, Wharff, Ginnis, Cannon, Joshi and Pao2012), which has been validated for use in multiple clinical settings including hospitals and primary care offices (Aguinaldo et al., Reference Aguinaldo, Sullivant, Lanzillo, Ross, He, Bradley-Ewing, Bridge, Horowitz and Wharff2021; DeVylder et al., Reference DeVylder, Ryan, Cwik, Jay, Wilson, Goldstein and Wilcox2020), and the newly developed Computerized Adaptive Screen for Suicidal Youth (King et al., Reference King, Brent, Grupp-Phelan, Casper, Dean, Chernick, Fein, Mahabee-Gittens, Patel and Mistry2021).
Implications for clinical interventions
Our conceptual model and current findings on child maltreatment and youth suicide also have implications for clinical practice. We briefly review these implications here, although a full discussion of these implications are beyond the scope of the present paper. First, our model has implications for treatment interventions that aim to prevent suicide among those with indicated risk factors (e.g., current suicidal ideation or a recent suicide attempt). The development, testing, and implementation of indicated suicide prevention interventions is sorely needed. A recent meta-analysis showed that, among all studies in the past 50 years that tested clinical interventions to reduce self-injurious thoughts and behaviors, cumulative effect sizes were small and did not show improvement over time (Fox et al., Reference Fox, Huang, Guzmán, Funsch, Cha, Ribeiro and Franklin2020). Notably, these effect sizes were smallest in studies testing interventions with children and adolescents. This underscores the need for more efficacious interventions to reduce suicidal thoughts and behaviors among young people. However, as noted by Kleiman and colleagues in their recent editorial (Reference Kleiman, Bentley, Glenn, Liu and Rizvi2021), these meta-analytic findings do not necessarily indicate the need for novel interventions but instead indicate the need to further refine and improve the efficacy of existing interventions.
Interventions that are individualized for specific subpopulations and risk factors (e.g., youth with maltreatment experiences) may be more effective in reducing suicide risk. Consequently, current interventions to reduce STBs should be modified to treat adolescents and emerging adults with maltreatment exposure. Clinical interventions that focus on the role of family support and repairing familial relationships may be particularly effective for use with adolescents who have experienced maltreatment. Indeed, family-based interventions and interventions that target other sources of social support are effective in reducing adolescent STBs (Brent et al., Reference Brent, McMakin, Kennard, Goldstein, Mayes and Douaihy2013). Studies that extend these family-based interventions to youth who have histories of maltreatment may be particularly beneficial. For instance, attachment-based family therapy has been shown to be efficacious in reducing suicidal ideation and depressive symptoms among adolescents (Diamond et al., Reference Diamond, Wintersteen, Brown, Diamond, Gallop, Shelef and Levy2010), but to our knowledge has not been tested among youth with maltreatment histories.
Additionally, multiple studies have provided evidence for Dialectical Behavior Therapy for Adolescents as an effective tool for mitigating risk for suicide and self-harm among high-risk youth. For instance, in two randomized trials by McCauley et al. (Reference McCauley, Berk, Asarnow, Adrian, Cohen, Korslund, Avina, Hughes, Harned and Gallop2018) and Mehlum et al. (Reference Mehlum, Tørmoen, Ramberg, Haga, Diep, Laberg, Larsson, Stanley, Miller and Sund2014), results supported Dialectical Behavior Therapy as an efficacious intervention to reduce self-harm, suicidal ideation, and depression among adolescents with repetitive self-harming behavior. Results indicated that improvements in emotion regulation mediated the association between Dialectical Behavior Therapy for Adolescents and reductions in harm behaviors (Asarnow et al., Reference Asarnow, Berk, Bedics, Adrian, Gallop, Cohen, Korslund, Hughes, Avina, Linehan and McCauley2021). Additionally, work by Berk et al. (Reference Berk, Shelby, Avina, Tangeman, Timmer and Urquiza2014) supports the Dialectical Behavior Therapy approach in targeting suicidal and self-harm behaviors and posttraumatic stress disorder symptoms among adolescents exposed to early trauma. Thus, Dialectical Behavior Therapy for Adolescents is a treatment modality with potential to reduce STBs specifically among youth with exposure to child maltreatment, and is consistent with the mechanisms we propose in our conceptual model.
Another possible direction for future research is to modify current interventions that are effective in reducing symptomatology among maltreated youth, into adapted interventions that specifically target the reduction of STBs in this population. Interpersonal Therapy for Depressed Adolescents and Dialectical Behavior Therapy for Adolescents are two modalities of note that target mechanisms included in our model (respectively, interpersonal processes and emotion regulation; Berk et al., Reference Berk, Shelby, Avina, Tangeman, Timmer and Urquiza2014; Lipsitz & Markowitz, Reference Lipsitz and Markowitz2013; Toth et al., Reference Toth, Handley, Manly, Sturm, Adams, Demeusy and Cicchetti2020). These treatment modalities may have potential application to the treatment of STBs among youth exposed to maltreatment. For example, Interpersonal Therapy for Depressed Adolescents was found to be efficacious in treating depressive symptoms among adolescent girls with a history of maltreatment (Toth et al., Reference Toth, Handley, Manly, Sturm, Adams, Demeusy and Cicchetti2020). It is possible that an enhanced version of Interpersonal Therapy for Depressed Adolescents of could also effectively treat and reduce suicidal ideation in this population, but this remains to be tested.
Implications for policy
Our model likewise has relevance for suicide prevention policy. First and foremost, upstream suicide prevention involves reducing risk factors that contribute to STBs, including exposure to child maltreatment. Thus, policies to prevent child maltreatment are an important step to reducing suicide among young people. Funding is needed for research on evidence-based or informed child maltreatment prevention services to reduce child maltreatment risk (e.g., Nurse-Family Partnership and other home visiting programs; Olds, Reference Olds2008). Additionally, policies are needed to support accessible and affordable mental health care, including suicide prevention services, for underserved populations (including families and youth with involvement with CPS). Youth who are in transition from foster care are an especially vulnerable population (Kaspar, Reference Kaspar2014) and policies are needed to fund and support services for these youth. Enhancing community-based and culturally informed services are important, as well as including laws that support parity for behavioral healthcare. Schools play an important role in suicide prevention, and resources should be provided to implement suicide prevention strategies in school settings, including trauma-informed training. However, youth impacted by abuse and neglect are at higher risk for dropping out of school, and thus support is also needed for community-based interventions. Ultimately, cross-sector collaborations are needed to support and integrate preventative mental health services for youth with maltreatment histories, including youth involved with CPS and the foster care system. Both public and private sector organizations can play a role in strengthening the services and resources available to youth and families with maltreatment histories to prevent STBs.
Conclusion
To better understand the processes connecting child maltreatment and adolescent suicide, there is a need for a developmentally informed theoretical model that explains and offers hypotheses regarding the risk for suicide in adolescence associated with adverse rearing contexts. In this paper, we reviewed and provided a brief synopsis of the relevant literature on mechanisms and moderators of the link between child maltreatment and youth suicide. Based on this review, the developmental psychopathology framework, and current theories in suicidology, we presented a conceptual model on child maltreatment and the development of suicide risk during adolescence and emerging adulthood.
We acknowledge that there are several limitations of our model, including the potential absence of other variables of interest (e.g., family history of suicidality) that are pertinent to the study of child maltreatment and youth STBs. Additionally, although we propose an integrative conceptual model for youth STBs, several components of our model (e.g., biological and interpersonal mechanisms) overlap with other etiological models of psychopathology. This is understandable given the multifinality of outcomes stemming from child maltreatment and related developmental sequelae, and the recent understanding that there are shared transdiagnostic mechanisms towards multiple forms of psychopathology. Despite these limitations, it is our hope that this conceptual model will provide a starting point for theoretically grounded and developmentally driven research on child maltreatment and youth suicide, and that this future research will iteratively inform modifications to our model’s precepts.
Importantly, given that an estimated 3.5 million youth in the United States are involved in a child maltreatment investigation each year, suicide prevention for youth who suffer these adverse childhood experiences should be an utmost priority in the field (U.S. Department of Health & Human Services, Administration for Children and Families, Administration on Children, Youth and Families, & Children’s Bureau, 2020). Primary prevention of child maltreatment and upstream prevention programs that focus on mending consequences of child maltreatment are necessary to prevent STBs and suicide in this at-risk youth population.
Funding statement
We are grateful to the National Institute of Child Health and Human Development (P50-HD096698 to Sheree L. Toth and Dante Cicchetti) for their support of this work. Training support was provided to the lead author via the National Institute of Mental Health (T32 MH20061).
Conflicts of interest
None.






