Previous papers from the World Health Organization's (WHO's) World Mental Health (WMH) Survey Initiative Reference Kessler, Haro, Heeringa, Pennell and Üstün1 have described the pattern of mental health service use, Reference Wang, Aguilar-Gaxiola, Alonso, Angermeyer, Borges and Bromet2 unmet need for treatment Reference Demyttenaere, Bruffaerts, Posada-Villa, Gasquet, Kovess and Lepine3 and delays in seeking help for mental health problems. Reference Wang, Angermeyer, Borges, Bruffaerts and Chiu4 The current paper focuses on drop out, defined here as stopping treatment for mental health problems before the treatment provider thought that treatment was complete. Drop out is known to be a common and important contributing factor to poor outcomes and results in inefficient use of limited resources. Reference Wang5,Reference Wang, Gilman, Guardino, Christiana, Morselli and Mickelson6 Although mental health treatment drop out is common, patterns and predictors of drop out are poorly understood and are based on a small number of studies from high-income countries (Canada and the USA) with comparatively well-resourced health and specialist mental health sectors. Reference Wang5,Reference Edlund, Wang, Berglund, Katz, Lin and Kessler7,Reference Olfson, Mojtabai, Sampson, Hwang, Druss and Wang8 This study explores patterns and predictors of mental health treatment drop out in 24 countries that carried out WMH surveys. These countries vary widely in economic status, health service structure and resourcing. The countries are stratified into high, upper-middle and low/lower-middle income groups based on criteria established by the World Bank (http://data.worldbank.org/about/country-classifications). As with earlier studies from national samples in Canada and the USA, a uniform definition of treatment drop out was applied to the representative samples of adults. Mental disorders and patterns of health service use across health sectors were ascertained with the Composite International Diagnostic Interview (CIDI). Reference Kessler and Üstün9 The behavioural model of access to care Reference Andersen10 used in previous studies of treatment drop out Reference Edlund, Wang, Berglund, Katz, Lin and Kessler7,Reference Olfson, Mojtabai, Sampson, Hwang, Druss and Wang8 provided the framework for considering the person-level predictors of drop out that included predisposing demographic (age, gender) and social factors (marital status, educational level), enabling factors (household income, health insurance, type and number of treatment providers) and indicators of need for treatment (type of mental disorder, number of mental disorders, past treatment of mental disorder).
Method
Samples
Data from 24 countries are included in this paper, 6 of them low/lower-middle, 6 upper-middle and 12 high-income countries (see online Table DS1 for WMH sample charateristics by World Bank income categories). Trained lay interviewers conducted all interviews face to face in multistage clustered area probability samples of household respondents. Part I of the interview was administered to everyone, whereas Part II, in most countries, was administered to only a subsample consisting of those who met criteria for any Part I disorder and a random subsample of other participants. Core disorders were in Part I. Health service use was in Part II of the interview in most countries. The current analyses are limited to Part II respondents (n = 63 678). The data have been weighted to adjust for the undersampling into Part II of Part I respondents without Part I disorders.
Details about the standardised survey methods (interviewer training procedures, WHO translation protocols for all study materials, quality control procedures for interviewers and data accuracy) employed in all WMH surveys are available elsewhere. Reference Kessler and Üstün11 Informed consent was obtained prior to the beginning of all interviews. Informed consent procedures and human subject safeguards were approved by the institutional review boards of the organisations coordinating the survey in each country.
Measures
Diagnostic assessments
The WHO's Composite International Diagnostic Interview (CIDI) Version 3.0 Reference Kessler and Üstün9,Reference Kessler and Üstün11 was used to assess mental disorders using DSM-IV criteria. 12 Disorders considered in this paper include only 12-month disorders: mood disorders (major depressive episode, dysthymia, bipolar I or II disorder, subthreshold bipolar disorder), anxiety disorders (panic disorder, specific phobia, social phobia, generalised anxiety disorder, agoraphobia, post-traumatic stress disorder, separation anxiety), impulse disorders (conduct disorder, intermittent explosive disorder, attention-deficit hyperactivity disorder, oppositional-defiant disorder) and substance use disorders (alcohol and drug misuse with and without dependence). Lifetime prevalence and age at onset were assessed separately for each disorder. Reference Kessler, Angermeyer, Anthony, de Graaf, Demyttenaere and Gasquet13 All diagnoses were considered with organic exclusions and without diagnostic hierarchy rules.
Mental health service sectors
Sources of care were classified into five sectors: psychiatrist; other mental health specialty (psychologist or other non-psychiatrist mental health professional in any setting or social worker/counsellor in a mental health specialty setting, or use of a mental health hotline); general medical services (primary care doctor, other general medical doctor, nurse, any other health professional not previously mentioned); human services (religious or spiritual advisor or social worker/counsellor in any setting other than a specialty mental health setting); and complementary and alternative medicine (CAM) (treatment from healers and self-help groups).
Treatment drop out
For each treatment provider, respondents were asked whether they received treatment in the past 12 months for ‘problems with your emotions, nerves, mental health or your use of alcohol or drugs?’ If so, they were asked whether treatment had stopped or was ongoing. Those who had stopped treatment with a provider were asked ‘Did you complete the full recommended course of treatment? Or did you stop before the [provider] wanted you to stop?’ Respondents who reported quitting were classified as having dropped out from a treatment sector if they had quit all providers they had seen in that sector. A separate variable denotes dropping out from all sectors. Because self-help groups have no providers, it was not possible to determine whether drop out occurred before the provider wanted.
Predictors of treatment drop out
Sociodemographic predictor variables. Sociodemographic predictors included age (18–34, 35–49, 50–64, 65+), gender, marital status (married/cohabitating, separated/widowed/divorced, never married), educational attainment (no education, some primary, primary finished, some secondary, secondary finished, some college, college finished or more) and household income. The per capita income of the respondent's household was divided by the median income of the country the respondent was from. Based on this ratio, household income was categorised as either low (0.5 or less), low-average (0.5+ to 1), high-average (1+ to 2) and high (2+).
Health service predictor variables. A history of mental healthcare utilisation prior to the past 12 months included in-patient care, out-patient counselling/psychotherapy or prescription of psychotropic medications. The number of different provider groups seen in the past 12 months for mental health treatment, treatment stage (the number of visits in that period) and health insurance for treatment of mental disorders were also included as predictors of drop out.
Diagnostic predictor variables. Four groups of mental disorders were used as predictors: mood, anxiety, substance use and impulse disorders. The number of mental disorders was used as an indicator of comorbidity. Severity was included in some additional analyses. Severity in the past 12 months was categorised as severe, moderate or mild, depending on the mental disorders experienced and the extent of disability reported. Reference Demyttenaere, Bruffaerts, Posada-Villa, Gasquet, Kovess and Lepine3
Analysis procedures
As noted above, Part-II data (n = 63 678) were weighted to adjust for the undersampling of respondents without Part I disorders and to make the Part II sample representative of the initial Part I sample. All analyses also used weights to adjust for differential sample selection probabilities and differential non-response and to post-stratify to population sociodemographic characteristics.
Twelve-month treatment episodes were aggregated into the five treatment sectors. Kaplan–Meier curves were used to examine drop out by number of visits. Predictors of drop out were examined with discrete-time survival analysis. Differences in predictors across sectors were examined with interaction terms between predictors and dummy variables for sector. Standard errors were estimated using the SUDAAN software system on Unix to adjust for stratification, clustering and weighting. Multivariable significance tests were conducted using Wald χ2 tests based on coefficient variance–covariance matrices adjusted for design effects using the Taylor series method. Statistical significance was evaluated using two-sided design-based tests (α = 0.05). Nonetheless, for the many additional comparisons made in the online tables, only those with P<0.01 are reported here.
Results
Over all the countries combined, the prevalence of any treatment in the past 12 months for ‘emotions, nerves, alcohol or drug problems’ was 9.0% (s.e. = 0.2). Treatment was more common in high-income (12.0%, s.e. = 0.2) than in higher-middle-income (8.7%, s.e. = 0.3) or in low/lower-middle-income (3.4%, s.e. = 0.2) countries. All further results are based on the 8482 participants who reported any mental health treatment in the 12 months prior to interview.
Table 1 indicates that the general medical sector was the sector in which treatment was most likely to occur (58.7%), but the median number of visits (1.6) was the lowest in this sector and the upper quartile of visits was particularly low. When countries were grouped by income level (online Table DS2), general medical services were the most common source of treatment in all groups: high income (61.2%), upper-middle income (56.8%) and low/lower-middle income (45.9%). Similarly, the median number of visits in this sector was low (high income, 1.5; middle income, 2.1; low income, 1.4).
Across all countries, about a fifth of patients (22.0%) saw a psychiatrist and this varied little by country income level (19.7 to 22.8%). In contrast, the percentage of patients seen by other mental health services rose from 13.7% in low/lower-middle-income countries to 29.1% in high-income countries. The number of visits was for the most part positively related to country income level in each of the sectors, apart from general medical services. Nonetheless, because general medical services were the most common source of treatment, the median number of visits across all sectors was similar in high- and upper-middle-income countries (2.4 and 2.5 respectively), although the upper quartile was higher in high-income countries (9.0 v. 5.3). Low/lower-middle-income countries had a lower median (1.6) and a lower upper quartile (3.1).
Treatment status at time of interview
At the time of interview, respondents who had been treated in the past 12 months were classified as having ended treatment prematurely, having completed treatment or still being in treatment (Table 2). Overall, 48.0% were still in treatment, 20.3% had completed treatment and 31.7% had dropped out. Drop out was least likely from psychiatrists (21.3%) and most likely from general medical services (40.5%). Online Tables DS3a–c present treatment status at time of interview for high-, upper-middle- and low/lower-middle-income countries. Drop out overall was higher in upper-middle- (45.1%) than in low/lower-middle- (37.6%) and high-income countries (26.3%). This pattern was also seen for human services and for CAM, but drop out from treatment by a psychiatrist was similar for all three country groups (20.3 to 23.8%). In contrast, drop out from general medical services was higher for the two lower-income groups (52.5% for both) than for the high-income group (33.4%). Completion of treatment was similar across the income groups (19.5 to 24.2%). The percentage of patients still in treatment was higher in high-income countries (53.7%) than in upper-middle-income countries (35.4%) or low/lower-middle-income countries (38.2%), largely reflecting the pattern seen for general medical services (44.1%, 27.2%, 24.9%).
Table 1 Number in treatment and number of visits, by service
| In treatment | Number of visits | ||||
|---|---|---|---|---|---|
| Service provider | n Footnote a | %Footnote b | s.e. | Median | IQR |
| Psychiatrist | 2014 | 22.0 | 0.6 | 2.8 | 1.1–7.9 |
| Other mental health | 2097 | 24.7 | 0.7 | 3.5 | 1.2–11.3 |
| General medical | 5147 | 58.7 | 0.7 | 1.6 | 1.0–2.8 |
| Human services | 1091 | 13.8 | 0.5 | 2.3 | 1.1–4.4 |
| Complementary and alternative medicine | 1126 | 14.0 | 0.5 | 2.4 | 1.2–10.2 |
| AnyFootnote c | 8482 | – | – | 2.3 | 1.2–6.8 |
a. Unweighted number of respondents who received treatment in the sector.
b. The percentages in treatment with each service provider sum to more than 100% because some patients saw multiple providers. Percentages are weighted to adjust for differences in selection probabilities, differential non-response, oversampling of Part II cases and residual differences on sociodemographic variables between the sample and the population.
c. The median number of visits for any sector represents the median across all sectors, not within any one sector, among patients treated in one or more sectors.
Table 2 Treatment status by sector among World Mental Health Survey respondents who had received mental health treatment in the past 12 months (all countries)
| Treatment status at the time of interviewFootnote a | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Premature termination | Completed treatment | Still in treatment | |||||||||||||
| n Footnote b | % | (s.e.) | χ2 | P | n Footnote c | % | (s.e.) | χ2 | P | n Footnote d | % | (s.e.) | χ2 | P | |
| I. Among service providers | |||||||||||||||
| Psychiatrist | 405 | 21.3 | (1.3) | 414 | 21.8 | (1.2) | 1195 | 56.9 | (1.4) | ||||||
| Other mental health | 488 | 24.1 | (1.2) | 522 | 27.4 | (1.3) | 1087 | 48.5 | (1.3) | ||||||
| General medical | 2115 | 40.5 | (0.9) | 979 | 20.6 | (0.8) | 2053 | 38.9 | (1.0) | ||||||
| Human services | 307 | 29.5 | (2.1) | 249 | 23.4 | (1.8) | 535 | 47.1 | (2.1) | ||||||
| Complementary and alternative medicine | 249 | 25.8 | (1.8) | 141 | 12.7 | (1.4) | 736 | 61.6 | (2.0) | ||||||
| Any | 2699 | 31.7 | (0.7) | 1541 | 20.3 | (0.6) | 4242 | 48.0 | (0.8) | ||||||
| II. Significance tests | |||||||||||||||
| Statistical test across providers, 4 degrees of freedom | 174.3 | <0.001 | 55.2 | <0.001 | 196.4 | <0.001 | |||||||||
a. The three proportions in each row sum to 100%. Percentages are weighted to adjust for differences in selection probabilities, differential non-response, oversampling of Part II cases and residual differences on sociodemographic variables between the sample and the population.
b. Unweighted number of respondents who dropped out of treatment in the sector.
c. Unweighted number of respondents who completed treatment in the sector.
d. Unweighted number of respondents who were still in treatment in the sector.
The cumulative probability of drop out by visit number
Drop out was most likely to occur after the second visit, with 21.6% dropping out after the second visit. Figure 1 shows the cumulative probability of treatment drop out by the number of visits within the past 12 months. Each curve rises steeply and then tends to flatten out.
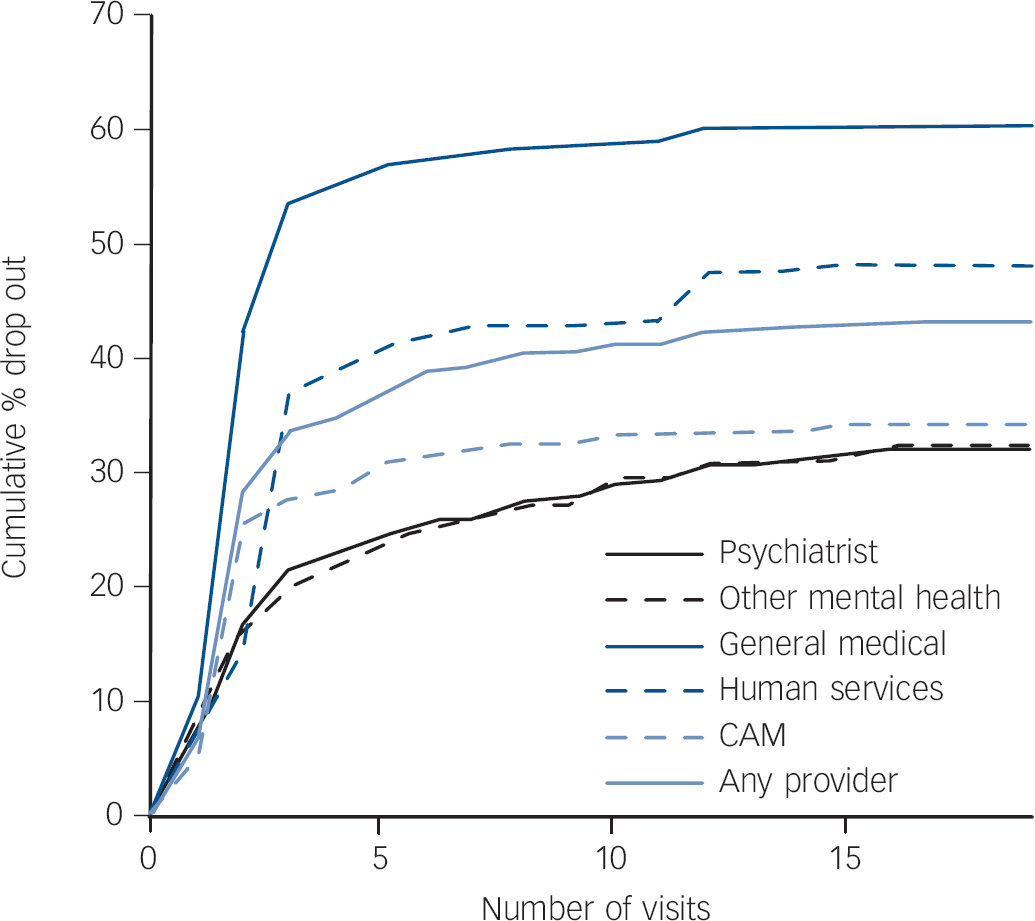
Fig. 1 Cumulative percentage that dropped out of treatment by visit, for each treatment provider sector.
CAM, complementary and alternative medicine.
The cumulative probability of drop out varied across the five sectors (P<0.0001). More than half (55.6%) of patients dropped out of general medical sector treatment by the fifth visit (online Table DS4). The next highest drop out by the fifth visit was from the human services sector (38.9%), followed by the CAM sector (28.6%), psychiatrists (23.0%) and other mental health providers (22.0%). Over all health sectors combined, approximately a third (34.8%) of patients dropped out of treatment by the fifth visit.
Table 3 Predictors of treatment drop out among World Mental Health Survey respondents who had received mental health treatment in the past 12 months, over all sectors (all countries)Footnote a

| Across all sectors (n = 8482) | ||||
|---|---|---|---|---|
| OR (95% CI) | χ2 | d.f. | P | |
| Number of visits in past 12 months | ||||
| 1–2 | 17.7 (15.0–20.9) | |||
| 3+ | 1.0 | 1177.4 | 1 | <0.0001 |
| Prior mental health treatment (ever) | ||||
| Yes | 0.7 (0.6–0.8) | 18.8 | 1 | <0.0001 |
| Number of providers | ||||
| 1 or 2 | 1.0 | 68.6 | 1 | <0.0001 |
| 3 or 4 | 0.2 (0.1–0.3) | |||
| Service provider | ||||
| Psychiatrist | 0.0 (0.0–0.1) | |||
| Other mental health profession | 0.2 (0.2–0.3) | |||
| General medical | 1.0 | 648.7 | 4 | <0.0001 |
| Human services | 0.7 (0.5–0.9) | |||
| Complementary and alternative medicine | 0.6 (0.4–0.8) | |||
| Insurance | ||||
| Yes | 1.1 (0.9–1.5) | 1.1 | 1 | 0.290 |
| Mental disorders | 7.4 | 4 | 0.120 | |
| Any mood | 1.1 (0.9–1.3) | |||
| Any anxiety | 1.1 (0.9–1.3) | |||
| Any substance use | 1.4 (1.1–1.9) | |||
| Any impulse | 1.1 (0.7–1.5) | |||
| Number of disorders | ||||
| Only 1 | 1.0 | 2.2 | 1 | 0.140 |
| 2 or more | 0.8 (0.6–1.1) | |||
a. The multivariable model was based on a discrete time survival framework with a person-visit file. Sociodemographic predictors – age group, gender, marital status, education and household income – were also included but were all non-significant with P≥0.40 (full model in online Table DS4).
Predictors of treatment drop out
Drop out across all sectors was investigated in a model that included sociodemographics (age group, gender, marital status, education and household income), clinical and treatment information as the predictors. Sociodemographic predictors were all non-significant (minimum P = 0.40, online Table DS5). Results for the other predictors are shown in Table 3.
Drop out was much more likely after only one or two rather than more visits (odds ratio (OR) = 17.7) and was less likely for those with prior mental health treatment (OR = 0.7) and for those seen by three or four v. only one or two types of providers (OR = 0.2). Drop out was highest among those seen in the general medical sector (OR = 1.0), lower among those seen in the human services (OR = 0.7) and CAM (OR = 0.6) sectors, and lowest among those seen by psychiatrists (OR = 0.0) and other mental health specialists (OR = 0.2). Neither health insurance for mental health treatment nor number of disorders was a significant predictor of treatment drop out, although patients with substance use disorders had elevated odds of drop out (OR = 1.4).
Predictors of drop out within sectors
To investigate the consistency of predictors of drop out within and across sectors, separate models were run to predict drop out within each sector and, in an overall model, interaction terms between predictor and sector were used to assess the heterogeneity of ORs across sectors (online Table DS6).
Drop out was more likely after the first or second than later visits within each sector (OR = 3.1 to 3.8), except for human services (sector heterogeneity P<0.0001). Prior treatment for mental disorders was consistently associated with lower drop out across sectors (OR = 0.6 to 0.8).
With three or more treatment providers, drop out was less likely from a psychiatrist (OR = 0.6) or from general medical services (OR = 0.4) but having multiple providers was unrelated to drop out from other sectors (sector heterogeneity P<0.0001). Insurance for mental health problems was unrelated to drop out within each sector.
Drop out within each sector was unrelated to the mental disorders experienced. Likewise the number of disorders was unrelated to drop out, except for human services for which those patients with two or more disorders were much less likely to drop out (OR = 0.3) (sector heterogeneity P = 0.003). As in the overall analysis, age group, gender, marital status and education were consistently unrelated to treatment drop out in the disaggregated analysis. Household income was related only to drop out from human services (OR = 1.8 to 1.9 for all groups relative to the high-income group (sector heterogeneity, P = 0.01)).
In summary, the predictors found to matter overall were mostly also found to predict within sectors, but there was some heterogeneity.
Predictors of drop out in high-, middle- and low-income countries
Table 4 shows the results for predictors of drop out within each country income group. Drop out was significantly more likely after the first two than later visits in all country groups but the extent differed, with ORs of 25.7 in high-income countries, 6.4 in upper-middle-income countries and 18.4 in low/lower-middle-income countries. There was also diversity across the country groups in the association of prior treatment with drop out: upper-middle-income countries (OR = 0.5), high-income countries (OR = 0.8), low/lower-middle-income countries (OR = 0.9). Three or more providers was associated with reduced drop out in high- and upper-middle-income countries (ORs of 0.1 and 0.3 respectively) but there were insufficient data to test for this in low/lower-middle-income countries.
Table 4 Predictors of treatment drop out among World Mental Health Survey respondents in high-, upper-middle-, low/lower-middle-income countries who had received mental health treatment in the past 12 months (over all sectors)Footnote a
| High-income countries | Upper-middle-income countries | Low/lower-middle-income countries | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | χ2 Footnote c | P | OR (95% CI) | χ2 Footnote c | P | OR (95% CI) | χ2 Footnote c | P | |
| Number of visits in past 12 months | 1069.8 | <0.0001 | 101.7 | <0.0001 | 125.1 | <0.0001 | |||
| 1–2 | 25.7 (21.2–31.3) | 6.4 (4.5–9.3) | 18.4 (11.0–30.6) | ||||||
| 3+ | 1.0 | 1.0 | 1.0 | ||||||
| Prior mental health treatment (ever) | 3.2 | 0.070 | 16.2 | <0.0001 | 0.1 | 0.770 | |||
| Yes | 0.8 (0.7–1.0) | 0.5 (0.4–0.7) | 0.9 (0.5–1.6) | ||||||
| Number of providers | 39.3 | <0.0001 | 31.3 | <0.0001 | |||||
| 1 or 2 | 1.0 | 1.0 | –Footnote b | ||||||
| 3 or 4 | 0.1 (0.1–0.2) | 0.3 (0.2–0.4) | –Footnote b | ||||||
| Type of provider | 525.4 | <0.0001 | 178.2 | <0.0001 | 63.2 | <0.0001 | |||
| Psychiatrist | 0.1 (0.0–0.1) | 0.0 (0.0–0.1) | 0.1 (0.0–0.1) | ||||||
| Other mental health profession | 0.2 (0.1–0.2) | 0.4 (0.3–0.7) | 0.7 (0.3–1.6) | ||||||
| General medical | 1.0 | 1.0 | 1.0 | ||||||
| Human services | 0.6 (0.4–0.9) | 1.0 (0.6–1.6) | 0.4 (0.2–0.7) | ||||||
| CAM | 0.2 (0.1–0.3) | 1.5 (0.9–2.2) | 1.1 (0.4–3.3) | ||||||
| Insurance | 1.5 | 0.230 | 3.7 | 0.053 | 0.0 | 0.950 | |||
| Yes | 0.8 (0.5–1.2) | 1.4 (1.0–1.9) | 1.0 (0.5–2.3) | ||||||
| Mental disorders | 9.9 | 0.040 | 16.8 | 0.002 | 6.0 | 0.200 | |||
| Any mood | 1.0 (0.8–1.3) | 1.5 (1.0–2.3) | 0.9 (0.4–1.9) | ||||||
| Any anxiety | 1.3 (1.1–1.6) | 0.8 (0.5–1.2) | 1.8 (0.9–3.5) | ||||||
| Any substance use | 1.1 (0.8–1.5) | 2.2 (1.4–3.6) | 1.4 (0.6–3.2) | ||||||
| Any impulse | 1.3 (0.8–2.1) | 0.8 (0.4–1.6) | 0.6 (0.3–1.4) | ||||||
| Number of disorders | 0.6 | 0.460 | 0.9 | 0.340 | 0.4 | 0.540 | |||
| Only 1 | 1.0 | 1.0 | 1.0 | ||||||
| 2 or more | 0.9 (0.6–1.2) | 0.7 (0.4–1.4) | 0.7 (0.2–2.3) | ||||||
CAM, complementary and alternative medicine.
a. Models are multivariable (all predictors in each column were entered at once) and based on a survival framework (with a person-visit file). Each column represents a separate multivariable model of drop out from care in a group of countries. Age group, gender, marital status, education and household income were included in each model but were all non-significant (minimum P = 0.14) except for an age effect in low-income countries (P = 0.04).
b. Results not shown because of small cell size. Small cell size determined by calculating the expected number of cases based on the percentage of people with the outcome and the total number of people with the condition. If the expected value was less than five, then the OR is dashed out.
c. Degrees of freedom (d.f.): number of categories minus one, except for mental disorders for which d.f. = 4 as the four groups of disorder were each entered as a binary variable.
Type of provider was significantly associated with drop out in each of the three country income groups but the pattern varied. The lowest drop-out rate was consistently for psychiatrists. High-income countries had a low drop out for other mental health services (OR = 0.2), as did upper-middle-income countries (OR = 0.4) but not low/lower-middle-income countries (OR = 0.7). The results for CAM were very different, with a low drop out relative to general medical services in high-income countries (OR = 0.2) but not in upper-middle-income countries (OR = 1.5) and low/lower-middle-income countries (OR = 1.1).
Drop out showed some minor relationship to which particular mental disorders were experienced in high-income countries (P = 0.04), a clearer relationship in upper-middle-income countries (OR of 1.5 for mood disorders and 2.2 for substance use disorders, P = 0.002 across all four disorder groups), and no relationship in low/lower-middle-income countries (P = 0.20). The number of disorders was not related to drop out in any of the income groups. Insurance was marginally associated with higher drop out in upper-middle-income countries (OR = 1.4, P = 0.053) and not associated elsewhere.
In all three country income groups sociodemographic predictors were non-significant except for a marginally significant non-ordinal association of age with drop out in low/lower-middle-income countries (P = 0.04) (results for the full model are available on request from the authors).
Severity was added as a predictor of drop out in some analyses (detailed results are available on request from the authors). For all countries combined there were no main effects for severity (moderate OR = 1.1 (95% CI 0.8–1.3) and severe OR = 1.1 (95% CI 0.9–1.4) compared with mild; χ2 = 0.4, d.f. = 2, P = 0.81) but a significant interaction effect whereby those with moderate or severe disorder(s) and three or more visits were less likely to drop out than expected from the main effects (moderate severity 3+ visits OR = 0.7 (95% CI 0.5–1.0); severe 3+ visits OR = 0.7 (95% CI 0.5–0.9); overall interaction χ2 = 8.8, d.f. = 2, P = 0.01). Results were similar within each income group.
Further analyses investigated predictors of drop out within sectors separately for country income groups (detailed results are available on request from the authors). Some sociodemographic predictors reached significance for some income groups for some sectors (possible type 1 errors).
Predictors of drop out after 1–2 visits or after 3 or more visits
Because so much drop out occurred very early, analyses were carried out with separate models for overall drop out after one or two visits, or after three or more visits (online Table DS7) (detailed results for each sector are available from the authors on request). In general the patterns were similar in both models. However, human services (OR = 0.3) and CAM (OR = 0.5) had lower drop out early on but similar (OR = 1.4) or slightly higher (OR = 1.9) drop out later. Drop out was higher for patients with substance use disorders only after three or more visits (OR = 2.1). Further analyses fitted the same sets of models within country income groups (detailed results available from the authors on request).
Discussion
Main findings
In this paper, using data from the WHO WMH surveys, the overall percentage who dropped out of treatment for mental health problems in the past 12 months was 31.7%. Even when looked at by treatment sector and by the income group of the country it was never trivial. Over all countries combined, the psychiatric sector had the lowest drop out (21.3%). The drop out from the psychiatric sector was similar across high-income, upper-middle-income and low/lower-middle-income countries but, for any treatment, upper-middle-income countries had higher drop out (45.1%) than high-income (26.3%) and low/lower-middle-income (37.6%) countries.
The results of the WHO WMH surveys differ in important respects from those of previous national surveys from Canada and the USA in which similar analyses were carried out. Reference Wang5,Reference Edlund, Wang, Berglund, Katz, Lin and Kessler7,Reference Olfson, Mojtabai, Sampson, Hwang, Druss and Wang8 The overall drop-out rate in the current study (31.7%) is higher than found in the early 1990s in the Ontario Health Survey (OHS) (17%) and the US National Comorbidity Survey (NCS) (19%) Reference Edlund, Wang, Berglund, Katz, Lin and Kessler7 as well as in the 2003–2004 Canadian Community Health Survey (CCHS) (22.3%). Reference Wang5 Slightly different definitions of drop out were used in these earlier studies Reference Wang5 but these seem unlikely to have produced such large differences. Even the US National Comorbidity Survey Replication (NCS-R), Reference Olfson, Mojtabai, Sampson, Hwang, Druss and Wang8 one of the high-income countries in the WMH surveys, had a somewhat lower level of drop out (22.4%) than that for the high-income countries as a group (26.3%).
In the entire set of WMH surveys included here, drop out in the past 12 months was more likely after only one or two visits, and less likely if there had been prior treatment at any time, and if there were three or more providers. These findings may reflect severity and chronicity whereby patients with more need for services are less likely to drop out. However, the specific disorders experienced by the patients had little relationship to drop out and what associations were seen were inconsistent across sectors and across high-, middle- and low-income groups. Nor was the number of disorder groups associated with drop out. Moreover, analyses of severity indicated that drop out was lower for moderate and severe cases only among those with three or more visits. As drop out can occur because patients think that treatment is ineffective, or conversely, because they think it has been effective even though their provider does not think that they have completed treatment, these two very different reasons for treatment drop out Reference Westmacott and Hunsley14 may explain the failure to find measures of need for treatment to be strong predictors of drop out. An important implication of the findings for drop out by the number of visits is that more attention needs to be paid to the early stages of treatment, as one or two visits are unlikely to provide much benefit to patients.
There were some clear differences in drop out across treatment sectors. In contrast to the results from Canada, Reference Wang5 drop out was less common from the mental health sectors, particularly from psychiatric care. This finding held across high-, higher-middle- and low/lower-middle-income countries. The pattern for other sectors, however, was not consistent across country income groups and is undoubtedly related to what services are provided and how they can be accessed. Results for CAM were the most different.
Insurance was generally not related to drop out in the WMH surveys, in contrast to the OHS, NCS and the NCS-R, in which mental health insurance was associated with lower odds of drop out. The WMH failure to find a similar pattern may arise from significant heterogeneity in the structure and resources of the health systems of the countries surveyed, even within the income-level groups. For instance, the USA and New Zealand are both high-income countries, yet in the USA, for the majority of the population, access to care is dependent on health insurance, whereas in New Zealand most mental healthcare by professionals is accessed through a publically funded system, with very limited private insurance-funded mental healthcare available.
Sociodemographic characteristics are important prediposing factors for mental disorder Reference Demyttenaere, Bruffaerts, Posada-Villa, Gasquet, Kovess and Lepine3 and are associated with access to treatment. Reference Wang, Aguilar-Gaxiola, Alonso, Angermeyer, Borges and Bromet2 Once an individual has accessed treatment, however, sociodemographic characteristics were found here to have little association with drop out. Both the OHS and NCS Reference Edlund, Wang, Berglund, Katz, Lin and Kessler7 found that younger people were more likely to drop out.
Strengths and limitations
The WMH survey results are strengthened by the fact that they are based on large national or regional probability samples and include middle-income and low-income countries, not just the high-income countries previously studied. Standard measures were used across the surveys and there was joint analysis of data. Nonetheless, there are several important limitations. One is that there is heterogeneity across the countries in health system service structure, funding and resourcing 15 and prevalence of disorders. Reference Demyttenaere, Bruffaerts, Posada-Villa, Gasquet, Kovess and Lepine3 This heterogeneity means that caution is needed in interpreting results based on pooled analyses, even though pooling was necessary to avoid sparse data. A second limitation is that all data are based on self-report (as for all the other surveys discussed). Not only are there issues of recall over the past 12 months, Reference Rhodes and Fung16 but the definition of treatment drop out is based on the patient's report that they terminated treatment prematurely, which might not always be the judgement of the provider. Also, analyses are based on visits in the past 12 months and may not correspond to an episode of care. Other limitations are that detailed characteristics of care and the matching of patient and treatment provider could not be considered. Despite these limitations, the findings from this study show that drop out is quite common regardless of the broader economic, health resourcing and health service structure in which the care is being provided, that drop out is most likely to occur early in the treatment process and that drop out is widely distributed in the sense that it is not strongly related either to sociodemographic or to clinical characteristics of patients. Drop out from general medical services is high and requires particular attention.
There have been many clinical studies of drop out from out-patient treatment in a variety of settings such as psychiatric or general mental health services, psychotherapy services and substance use services, mostly in high-income countries. These studies are able to define episodes of care. Many, Reference Wierzbicki and Pekarik17 especially large studies of routinely collected data, Reference Beynon, McMinn and Marr18,Reference Mitchell and Selmes19 have few predictors apart from sociodemographic characteristics. Reference Reneses, Munoz and Lopez-Ibor20 These are useful for indicating which groups of patients are hardest to retain in treatment but have not been particularly consistent across studies. Reference Barrett, Chua, Crits-Christoph, Gibbons and Thompson21 Other smaller clinical studies have a richer set of predictors including more clinical details, Reference Rossi, Amaddeo, Bisoffi, Ruggeri, Thornicroft and Tansella22 views of patients and staff Reference Rossi, Amaddeo, Bisoffi, Ruggeri, Thornicroft and Tansella22–Reference Westmacott, Hunsley, Best, Rumstein-McKean and Schindler24 and measures of the therapeutic alliance. Reference Johansson and Eklund25
Implications
The results reported here, other survey results and clinical studies all show that we have a good deal of work to do to address the important and widespread problem of treatment drop out. Not only is it important to provide access to treatment for mental health problems but it is also necessary to retain patients in treatment long enough for them to benefit.
Strategies for retention in psychotherapy have been reviewed Reference Barrett, Chua, Crits-Christoph, Gibbons and Thompson21,Reference Ogrodniczuk, Joyce and Piper26 with a call for more research, especially into strategies other than pretherapy preparation. Reference Ogrodniczuk, Joyce and Piper26 Barrett et al Reference Barrett, Chua, Crits-Christoph, Gibbons and Thompson21 provide recommendations for role induction, motivational interviewing, therapist feedback and careful attention to the therapuetic alliance to reduce drop out. In an impoverished patient group, drop out was reduced by adding case management to therapy. Reference Miranda, Azocar, Organista, Dwyer and Araene27
Attempts to address drop out have been made in other settings. For example a prompt to encourage first attendance at psychiatric out-patient clinics, Reference Kitcheman, Adams, Pervaiz, Kader, Mohandas and Brookes28 and strategies like this may assist with reducing early drop out. Patient–physician communication has been shown to influence use of antidepressants. Reference Bull, Hu, Lee, Ming, Markson and Fireman29 Strategies to address drop out from general medical services are required and most likely require further education and training, particularly for general practitioners, plus opportunities for them to refer patients on to other services. A salutory tale comes from a study of a change in case management for patients with substance misuse that found that the new centralised system reduced attendance and completion, indicating the need for careful evaluation of new systems. Reference Rohrer, Vaughan, Cadoret, Carswell, Patterson and Zwick30
As we found predictors of drop out to be similar across country income-level groups, these strategies to address drop out may also be applicable regardless of the broader economic and health service structure in which the care is being provided.
Acknowledgements
We thank the staff of the WMH Data Collection and Data Analysis Coordination Centres for assistance with instrumentation, fieldwork and consultation on data analysis. A complete list of all within-country and cross-national WMH publications can be found at http://www.hcp.med.harvard.edu/wmh/.








eLetters
No eLetters have been published for this article.