INTRODUCTION
A cesarean scar ectopic pregnancy is rare but its incidence is increasing. Familiarity with its sonographic findings can prevent the erroneous identification of a cesarean scar ectopic as an intrauterine pregnancy. To our knowledge, there have been no published case reports of an emergency physician using point-of-care transabdominal ultrasound to diagnose a cesarean scar ectopic pregnancy.
CASE PRESENTATION
A 33-year-old gravida 2 para 1 woman presented to the emergency department with 3 days of constant suprapubic pain. She was 7 weeks and 4 days pregnant by her last menstrual period, diagnosed by urine βhCG. She denied vaginal discharge or bleeding. The pregnancy was conceived naturally with no assistive reproductive technologies. She was previously healthy, with a past surgical history notable for cesarean delivery one decade earlier for an atypical fetal heart rate tracing.
The patient's vitals were heart rate 89 beats/min, blood pressure 105/70 mm Hg, respiratory rate 13 breaths/min, oxygen saturation 100% on room air, and temperature 36.6°C (97.9°F). Her abdomen was soft with mild tenderness and fullness over the suprapubic area. There were no signs of peritonitis. A serum βhCG was reported as 92291.
A point-of-care ultrasound examination was performed in the emergency department by the emergency physician. A 6-2 MHz curvilinear probe with the obstetric preset selected was placed in the longitudinal orientation cephalad to the pubic symphysis. The scan revealed a gestational sac with surrounding decidual reaction immediately adjacent to the bladder (Figures 1A and 1B). This was positioned in the lower segment of the uterus without a typical-appearing homogeneous myometrium surrounding all sides. A transverse probe orientation revealed a fetal pole within the gestational sac and again demonstrated an absence of myometrium (Figure 1C). An M-mode tracing revealed a heart rate of 171 beats per minute, signifying a live pregnancy. No free fluid was visualized in the pelvis, nor in the patient's right upper quadrant. These findings were concerning for a live ectopic pregnancy within the anterior wall of the uterus.
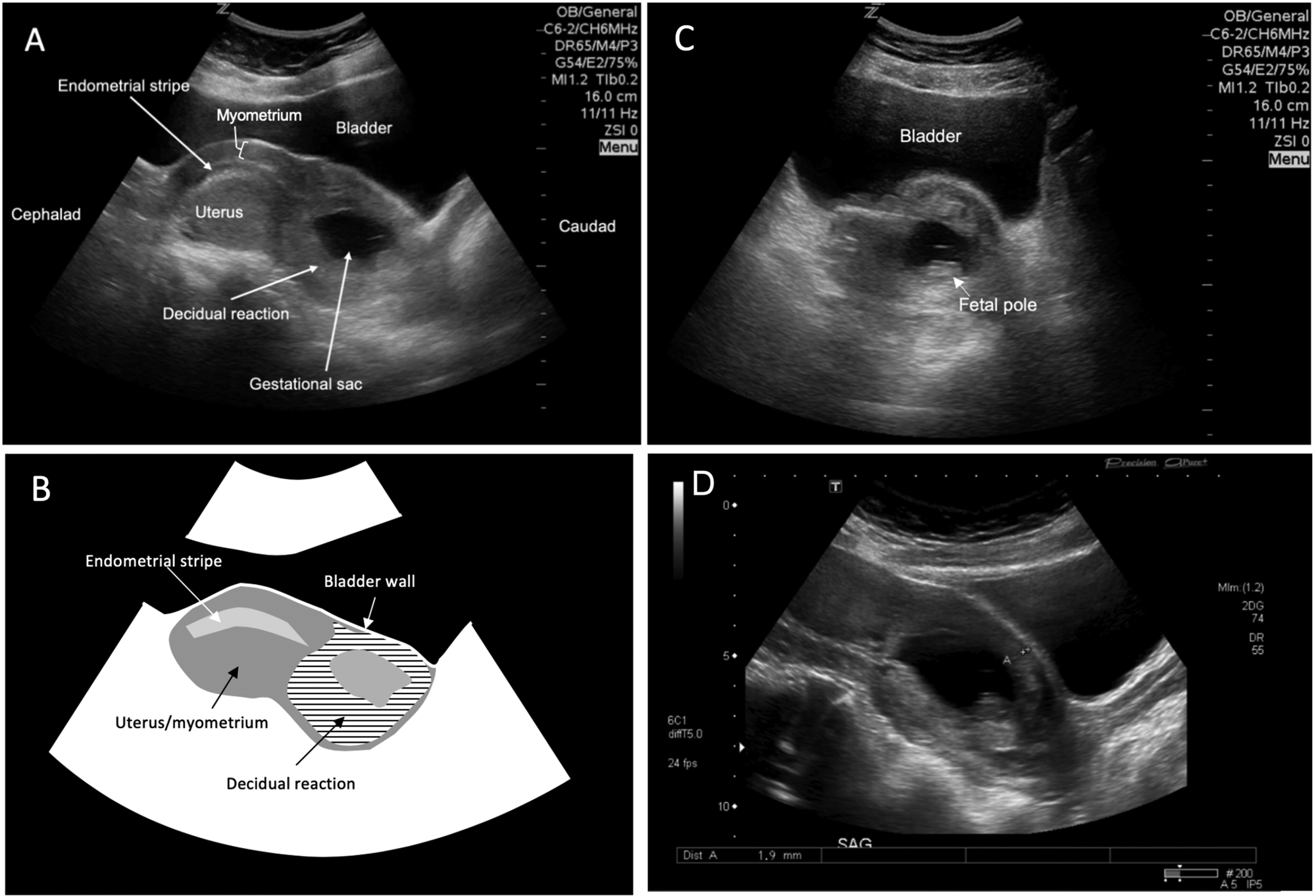
Figure 1. (A) Longitudinal point-of-care ultrasound scan positioned cephalad to the pubis reveals a gestational sac within the lower anterior aspect of the uterus adjacent to the bladder and absence of normal myometrium surrounding the gestational sac. (B) Schematic representation of Figure 1A, denoting the relationship of myometrium, decidual reaction, and bladder wall. (C) Transverse point-of-care ultrasound scan demonstrating a fetal pole within the gestational sac and heterogeneous surrounding tissue. (D) Consultative transabdominal longitudinal ultrasound showing a myometrial thickness of 1.9 mm anterior to the gestational sac.
A consultative ultrasound scan of the pelvis and abdomen was ordered, and obstetrical consultation was requested. The ultrasound confirmed a cesarean scar ectopic, with myometrial thinning of 1–2 millimetres overlying the anterior aspect of the pregnancy (Figure 1D). The patient remained stable and the decision was made by the obstetrical consultant to perform a staged procedure. The patient underwent an ultrasound-guided transvaginal potassium-chloride injection directly into the gestational sac with aspiration of its contents and subsequent laparoscopically guided hysteroscopy with dilatation and curettage. She was discharged in good condition.
DISCUSSION
A cesarean scar ectopic pregnancy is rare, occurring in approximately 1 in 1,800 to 1 in 2,000 pregnancies, and accounting for 6.1% of ectopic pregnancies in patients with previous cesarean deliveries.Reference Seow, Huang and Lin1,Reference Rotas, Haberman and Levgur2 Its incidence is increasing, both due to increased recognition and increased rates of cesarean deliveries being performed worldwide.Reference Rotas, Haberman and Levgur2 A cesarean scar ectopic pregnancy is thought to occur by embryo migration through a microscopic scar defect, enabling the embryo to become completely surrounded by myometrium and scar tissue.Reference Rotas, Haberman and Levgur2 Patients with cesarean scar ectopic pregnancies typically present for assessment in the first trimester with nonspecific symptoms, including lower abdominal or pelvic cramping and vaginal bleeding.Reference Rotas, Haberman and Levgur2 Failure to diagnose a cesarean scar ectopic pregnancy in a timely manner can result in serious morbidity, including uterine rupture, life-threatening hemorrhage, and a hysterectomy.Reference Seow, Huang and Lin1,Reference Rotas, Haberman and Levgur2
Diagnosis is usually made by a combination of consultative transabdominal and transvaginal ultrasonography. Diagnostic criteria vary, however, generally include an empty uterus and cervical canal, gestational sac within the anterior portion of the lower uterus, and thinned or absent myometrium between the bladder and gestational sac.Reference Seow, Huang and Lin1–Reference Osborn, Williams and Craig3
In this report, we present the first case of cesarean scar ectopic pregnancy in the literature diagnosed by a transabdominal point-of-care ultrasound. Point-of-care ultrasound is a common adjunct used in the emergency department for the evaluation of first-trimester, pregnancy-related complaints, including abdominal pain and vaginal bleeding.Reference Murray, Baakdah, Bardell and Tulandi4 Of critical importance in patients with these complaints is to rule out ectopic pregnancy, as it is a potential source of morbidity and mortality. In patients without risk factors for a heterotopic pregnancy, such as the use of fertility treatments, point-of-care ultrasound identification of an intrauterine pregnancy is considered to effectively rule out ectopic pregnancy, as the likelihood of a heterotopic pregnancy in the general population is considered to be extremely low.Reference Murray, Baakdah, Bardell and Tulandi4,Reference Socransky and Wiss5
Criteria for the diagnosis of an intrauterine pregnancy by point-of-care ultrasound include identification of the adjacency of the uterus to the bladder (a typical ectopic pregnancy may appear to be surrounded by uterine-like tissue; however, it will usually not be found immediately adjacent to the bladder); identification of a gestational sac; decidual reaction centred within the endometrial stripe; yolk sac and/or fetal pole; and myometrial thickness > 5–8 mm5. Failure to meet any of these criteria warrants the physician to declare no definitive intrauterine pregnancy and to seek consultative ultrasound.Reference Socransky and Wiss5 In spite of these criteria, a visible ectopic pregnancy on point-of-care ultrasound may mislead the physician into declaring an intrauterine pregnancy. The cesarean scar ectopic pregnancy may be predisposed to this error due to its close approximation to the uterus and bladder. Knowledge of the appearance of a cesarean scar ectopic pregnancy is therefore of particular importance to the emergency physician.
In our case, 4 of 5 criteria for intrauterine pregnancy diagnosis by point-of-care ultrasound diagnosis were met (gestational sac, decidual reaction, yolk sac/heart rate, bladder-uterine adjacency). However, the images reveal a lack of visible myometrium surrounding the gestational sac, particularly on the aspect in contact with the bladder. Further scrutiny also reveals that, unlike a normal intrauterine pregnancy, the cesarean scar ectopic is eccentrically located, being positioned lower in the uterus than the expected site of implantation. In our case, this is the most obviously abnormal feature.
CONCLUSION
A cesarean scar ectopic pregnancy is a rare form of ectopic pregnancy, however, its incidence is increasing. Emergency physicians must maintain a high degree of suspicion for this diagnosis in patients with previous cesarean delivery. Familiarity with the point-of-care ultrasound appearance of a cesarean scar ectopic is necessary to prevent erroneous identification of the pregnancy as intrauterine. In particular, eccentric positioning (anterior/low uterine) and decreased myometrial mantle should alert the physician to this diagnosis. A definitive diagnosis requires a consultative ultrasound and expert obstetrical consultation.
Competing interests
None declared.



