To the Editor—We read with great interest the manuscript emphasizing increasing resistance to colistin and tigecycline in Enterobacteriaceae.Reference Kumar 1 Hence, we present the epidemiology of colistin- and carbapenem-resistant (CoCR) Klebsiella pneumoniae (CoCR-KP) and Escherichia coli (CoCR-E. coli) isolated from various clinical samples from January 1 through July 30, 2015, at a 700-bed tertiary care university hospital. We also report synergy testing results of antibiotic combinations that could be used for the treatment of the infections caused by CoCR isolates.
A total of 19 isolates (6 E. coli, 13 K. pneumoniae) from 17 patients were included in the study. All E. coli and 3 K. pneumoniae isolates were recovered from rectal swab samples collected during a point prevalance program performed for detection of CR-KP colonization in accordance with Centers for Disease Control and Prevention methods. Ten K. pneumoniae isolates were obtained from urine (n=7), blood (n=1), central venous catheter (n=1), and peritoneal fluid (n=1) samples. The identification of the isolates was made by matrix-assisted laser desorption/ionization–time of flight mass spectrometry (VITEK MS; bioMérieux) and by analytical profile index (API20E; bioMérieux). Antimicrobial susceptibility testing against carbapenem, colistin, and tigecycline was performed by Etest (bioMérieux) and against amikacin, gentamicin, cefuroxime, ceftazidime, cefepime, ceftriaxone, piperacillin-tazobactam, amoxicillin-clavulanic acid, aztreonam, chloramphenicol, trimethoprim-sulfamethoxazole, fosfomycin, and tetracycline by disc diffusion method (BBL). The results were interpreted in accordance with European Committee on Antimicrobial Susceptibility Testing breakpoints. 2 Because European Committee on Antimicrobial Susceptibility Testing zone diameter breakpoints are not available for fosfomycin and tetracycline, Clinical and Laboratory Standards Institute breakpoints were used. 3 E. coli ATCC 25922 was included with every batch of susceptibility tests. The isolates were categorized as multidrug resistant, extensively drug resistant, and pandrug resistant in accordance with a recent consensus document.Reference Magiorakos, Srinivasan and Carey 4 The synergy between different antibiotic combinations was tested by using Etest, and the fractional inhibitory concentration index for each double or triple combination was calculated and interpreted as described previously.Reference Sopirala, Mangino and Gebreyes 5
Genetic relatedness of the CoCR isolates was evaluated by pulsed-field gel electrophoresis with XbaI-digested genomic DNA as described previouslyReference Marchaim, Chopra and Pogue 6 and by arbitrarily primed polymerase chain reaction using universal M13 primer.Reference Welsh and McClelland 7 Antimicrobial resistance genes bla OXA-48, bla NDM, bla KPC, bla CTX-M, and bla PER-1 in the DNA genome and plasmid-mediated mcr-1 gene in the plasmid DNA were detected by using polymerase chain reaction.Reference Poirel, Walsh, Cuvillier and Nordmann 8 – Reference Liu, Wang and Walsh 10
All patients infected or colonized with CoCR-KP or CoCR-E. coli had several underlying diseases, received broad-spectrum antibiotics, and had prolonged hospitalization mainly in the intensive care units or oncology wards (Table 1). Thirteen of the 19 isolates were considered as colonization. Antibacterial susceptibility rates of CoCR-KP were as follows: aztreonam, 8% (1/13); fosfomycin, 8% (1/13); tetracycline, 15% (2/13); tigecycline, 15% (2/13); chloramphenicol, 15% (2/13); gentamicin, 23% (3/13); and trimethoprim-sulfamethoxazole, 23% (3/13). Five of 6 E. coli were pandrug resistant and 1 isolate was extensively drug resistant (susceptible only to chloramphenicol). Of the 13 K. pneumoniae isolates, 7 were pandrug resistant, 4 extensively drug resistant, and 2 multidrug resistant. All K. pneumoniae isolates were harboring OXA-48; however, the isolates were negative for K. pneumoniae carbapenemase, New Delhi metallo-beta-lactamase, and PER-1 and mcr-1 genes. CTX-M was detected in 9 K. pneumoniae and 4 E. coli isolates. Meropenem plus colistin and meropenem plus ertapenem exhibited synergism but meropenem plus ertapenem plus colistin had antagonistic effect against all CoCR isolates. Meropenem plus colistin plus tigecycline had an antagonistic effect in 1 isolate but indifferent effect in 18 isolates. Tigecycline plus colistin and tigecycline plus meropenem exhibited synergism in 6 and 5 isolates, respectively. Tigecycline plus meropem were antagonistic in 2 isolates. Tigecycline plus colistin and tigecycline plus meropenem exhibited indifferent effect for the rest of the isolates. Although meropenem plus ertapenem or meropenem plus colistin had synergistic effect, the role of this combination in patients with bacteremia is questionable. Of 19 isolates, 18 had minimal inhibitor concentration of meropenem higher or equal to 32 mg/L, which makes it difficult to achieve adequate serum concentration. On the other hand, 1 of 3 patients with extensively drug-resistant CoCR-KP urinary tract infection was succesfully treated with colistin plus meropenem and 2 patients were successfully treated with gentamicin (which was susceptible in vitro). Although microbiological cure was achieved with gentamicin plus ertapenem in a patient with secondary peritonitis, the patient died with end organ failure 10 days after the treatment was completed. Targeted gentamicin treatment was associated with favorable outcome in CoCR-KP sepsis.Reference Gonzalez-Padilla, Torre-Cisneros and Rivera-Espinar 11
TABLE 1 Demographic and Clinical Characteristics of 17 Patients With Colistin- and Carbapenem-Resistant Klebsiella pneumoniae and Escherichia coli
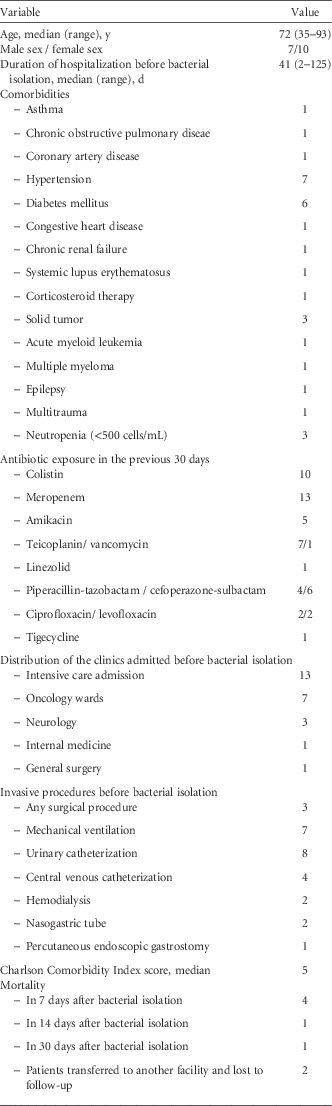
NOTE. Data are no. of patients unless otherwise indicated.
Although all K. pneumoniae isolates were identical and E. coli isolates have 2 pulsotypes according to pulsed-field gel electrophoresis results, it is not easy to define the exact chronological sequence in patients colonized or infected by the CoCR isolates if only simultanous isolation of the organism from culture is considered. In our study, 10 of 17 CoCR-KP and CoCR-E. coli isolated patients were already under contact precautions because of previous multidrug-resistant bacteria colonization but this did not prevent the spread of the CoCR isolates due to poor adherence to infection control precautions. In cases of prolonged hospitalization, transfer of patients between wards and intensive care units, which is a frequent situation in our institute, might result in the transmission of the resistant germs between different hospital units. Marchaim et alReference Marchaim, Chopra and Pogue 6 have presented a similar report in patients infected with the identical CoCR-KP isolates from different wards.
In conclusion, the circulation of the identical strains in such a relatively short period of time (7 months) could indicate an epidemic that requires an urgent intervention to improve the infection control precautions and prevent the spread of the CoCR isolates.
ACKNOWLEDGMENTS
We thank Gülden Kaya for technical asistance in the laboratory work.
Financial support. None reported.
Potential conflicts of interest. Gökhan Metan reports that he has received honaria for speaking at symposia and lectures organized by Gilead and financial compensation from Pfizer for the time and expenses for a meeting organized to discuss the content of a review paper, is a member of the advisory board of Pfizer and Astellas, and has received travel grants from Merck Sharp & Dohme, Pfizer, and Gilead to participate in conferences. Serhat Unal reports that he has received honaria for lectures as well as travel grants to participate in conferences from Pfizer, Merck Sharp & Dohme, and Gilead. All other authors report no conflicts of interest relevant to this article.



